Cysticercosis differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Ahmed Younes (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (23 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | [[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Cysticercosis]] | ||
{{CMG}};{{AE}}{{AY}} | |||
==Overview== | ==Overview== | ||
Cysticercosis must be differentiated from other diseases that cause | Cysticercosis must be differentiated from other diseases that cause brain cystic lesions (as brain abscess and brain tumors) or ocular lesions (as retinal detachment and coats disease). | ||
==Differentiating cysticercosis from other diseases== | |||
{| class="wikitable" | {| class="wikitable" | ||
|+Differentiating neurocysticercosis from other brain cyst lesions | |+Differentiating neurocysticercosis from other brain cyst lesions | ||
| Line 12: | Line 17: | ||
|Neurocysticercosis | |Neurocysticercosis | ||
| | | | ||
* [[Parenchymal]] | * Presenting symptoms differ according to the site of the cysticerci. | ||
* [[Parenchymal]] neurocysticercosis causes all the symptoms and signs of [[Space occupying lesion|space occupying lesions]]. | |||
* Extraparenchymal neurocysticercosis causes manifestations of [[increased intracranial pressure]] if cysts are present in the [[subarachnoid space]] or in the [[ventricles]], manifestations of [[spinal cord compression]] if present in the spinal cord or causes eye disease if cysts are present in the [[orbit]]. | |||
| | | | ||
* [[Immunoblot|CDC's immunoblot]] is based on detection of [[antibody]] to one or more of [[Glycoprotein|7 lentil-lectin purified structural glycoprotein]] [[antigens]] from the larval cysts. | |||
* It is 100% [[Specificity (tests)|specific]] and has a [[sensitivity]] superior to that of any other test yet evaluated | |||
| | |||
* [[Computed tomography|Computerized tomography (CT)]] is superior to [[magnetic resonance imaging|magnetic resonance imaging (MRI)]] for demonstrating small [[calcification]]s. | |||
* However, [[MRI]] shows [[cysts]] in some locations (cerebral convexity, [[Ependyma|ventricular ependyma]]) better than [[CT]], is more [[Sensitivity|sensitive]] than CT to demonstrate surrounding [[cerebral edema|edema]], and may show internal changes indicating the death of cysticerci. | |||
|- | |- | ||
|[[Brain abscess]] | |[[Brain abscess]] | ||
| Line 42: | Line 52: | ||
* [[MRI]]: [[MRI|Gadolinium-enhanced MRI]] is the preferred imaging modality for assessing the extension of the tumor and its exact location.<ref name="urlPrimary Brain Tumors in Adults - American Family Physician">{{cite web |url=http://www.aafp.org/afp/2008/0515/p1423.html |title=Primary Brain Tumors in Adults - American Family Physician |format= |work= |accessdate=}}</ref> | * [[MRI]]: [[MRI|Gadolinium-enhanced MRI]] is the preferred imaging modality for assessing the extension of the tumor and its exact location.<ref name="urlPrimary Brain Tumors in Adults - American Family Physician">{{cite web |url=http://www.aafp.org/afp/2008/0515/p1423.html |title=Primary Brain Tumors in Adults - American Family Physician |format= |work= |accessdate=}}</ref> | ||
|- | |- | ||
|Brain tuberculoma | |[[Tuberculoma|Brain tuberculoma]] | ||
| | | | ||
* Brain tuberculomas has insidious onset of symptoms as compared to tuberculous meningitis. | * [[Tuberculoma|Brain tuberculomas]] has insidious onset of symptoms as compared to [[tuberculous meningitis]]. | ||
* Presentations are usually due to the pressure effect, not the T.B. bacilli. | * Presentations are usually due to the pressure effect, not the [[Bacilli|T.B. bacilli]]. | ||
* Presenting symptoms and signs in order of occurrence:<ref name="urlThe Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF">{{cite web |url=http://www.jacpjournal.org/downloadpdf.asp?issn=2320-8775;year=2015;volume=3;issue=1;spage=3;epage=8;aulast=Mukherjee;type=2 |title=The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF |format= |work= |accessdate=}}</ref> | * Presenting symptoms and signs in order of occurrence:<ref name="urlThe Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF">{{cite web |url=http://www.jacpjournal.org/downloadpdf.asp?issn=2320-8775;year=2015;volume=3;issue=1;spage=3;epage=8;aulast=Mukherjee;type=2 |title=The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF |format= |work= |accessdate=}}</ref> | ||
# Episodes of focal seizures | # Episodes of [[focal seizures]] | ||
# Signs of increased intracranial pressure | # Signs of [[increased intracranial pressure]] | ||
# Focal neurologic deficits. | # [[Focal neurologic signs|Focal neurologic deficits]]. | ||
| | | | ||
* CT: Contrast-enhanced CT scan shows a ring enhancing lesion surrounded by an area of hypodensity (cerebritis) and the resulting mass effect. | * [[TB|T.B.]] should be investigated everywhere else in the body (e.g. [[Lymphadenopathy|peripheral lymphadenopathy]], [[Sputum culture|sputum]] and [[blood culture]]) | ||
* MRI: Better than CT scan in assessing the site and size of the tuberculoma. Gadolinium-enhanced MRI shows a ring enhancing | | | ||
* [[CT]]: [[Contrast enhanced CT|Contrast-enhanced CT]] scan shows a ring enhancing lesion surrounded by an area of hypodensity ([[cerebritis]]) and the resulting [[mass effect]]. | |||
* [[MRI]]: Better than [[CT]] scan in assessing the site and size of the [[tuberculoma]]. Gadolinium-enhanced MRI shows a ring enhancing lesion between 1-5 cm in size (In NCC, the wall is thicker, [[Calcification|calcifications]] are eccentric and the diameter is less than 2 cm) | |||
|- | |- | ||
|Neurosarcoidosis | |Neurosarcoidosis | ||
|70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations are:<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | | | ||
* 70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations are:<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | |||
# Cranial neuropathies: Facial palsy is the most common presentation. | # Cranial nerve neuropathies: [[Facial palsy]] is the most common presentation. | ||
# Meningeal involvement: diffuse meningeal inflammation can cause diffuse basilar polyneuropathy in 40% of the patients. with neurosarcoidosis. | # [[Meningeal]] involvement: diffuse [[Meningitis|meningeal inflammation]] can cause diffuse [[Polyneuropathy|basilar polyneuropathy]] in 40% of the patients. with [[neurosarcoidosis]]. | ||
# Inflammatory spinal cord disease: Inflammatory span usually more than 3 spinal cord segments which helps to differentiate it from Multiple sclerosis. | # Inflammatory [[spinal cord]] disease: Inflammatory span usually more than 3 spinal cord segments which helps to differentiate it from [[Multiple sclerosis|Multiple Sclerosis]]. | ||
# Peripheral neuropathy: Asymmetric polyneuropathy or mononeuritis multiplex. It may also manifest as GBS like presentation. | # [[Peripheral neuropathy]]: [[Polyneuropathy|Asymmetric polyneuropathy]] or [[mononeuritis multiplex]]. It may also manifest as [[Guillain-Barré syndrome|Guillain-Barré syndrome (GBS)]] like presentation. | ||
# HPO axis involvement: may present as diabetes | # [[Hypothalamic pituitary adrenal axis|HPO axis]] involvement: may present as [[diabetes insipidus]]. More than 50% of the cases have no radiological signs. | ||
| | | | ||
* Noninvasive tests have low sensitivity and specificity. | * [[Noninvasive test|Noninvasive tests]] have low [[sensitivity]] and [[specificity]]. | ||
* Serum ACE levels are elevated in 25% of the cases | * Serum [[ACE|ACE levels]] are elevated in 25% of the cases | ||
* Lumbar puncture shows elevated | * [[Lumbar puncture]] shows elevated [[CSF]] proteins together with mild-moderate [[pleocytosis]]. It is usually accompanied by [[oligoclonal bands]].<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | ||
|MRI with contrast shows enhancement of the inflamed areas (i.e. cranial nerves, meninges or HPO axis) | | | ||
* [[Magnetic resonance imaging|MRI]] with [[contrast]] shows enhancement of the inflamed areas (i.e. [[cranial nerves]], [[meninges]] or [[Hypothalamic pituitary adrenal axis|HPO axis]]) | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
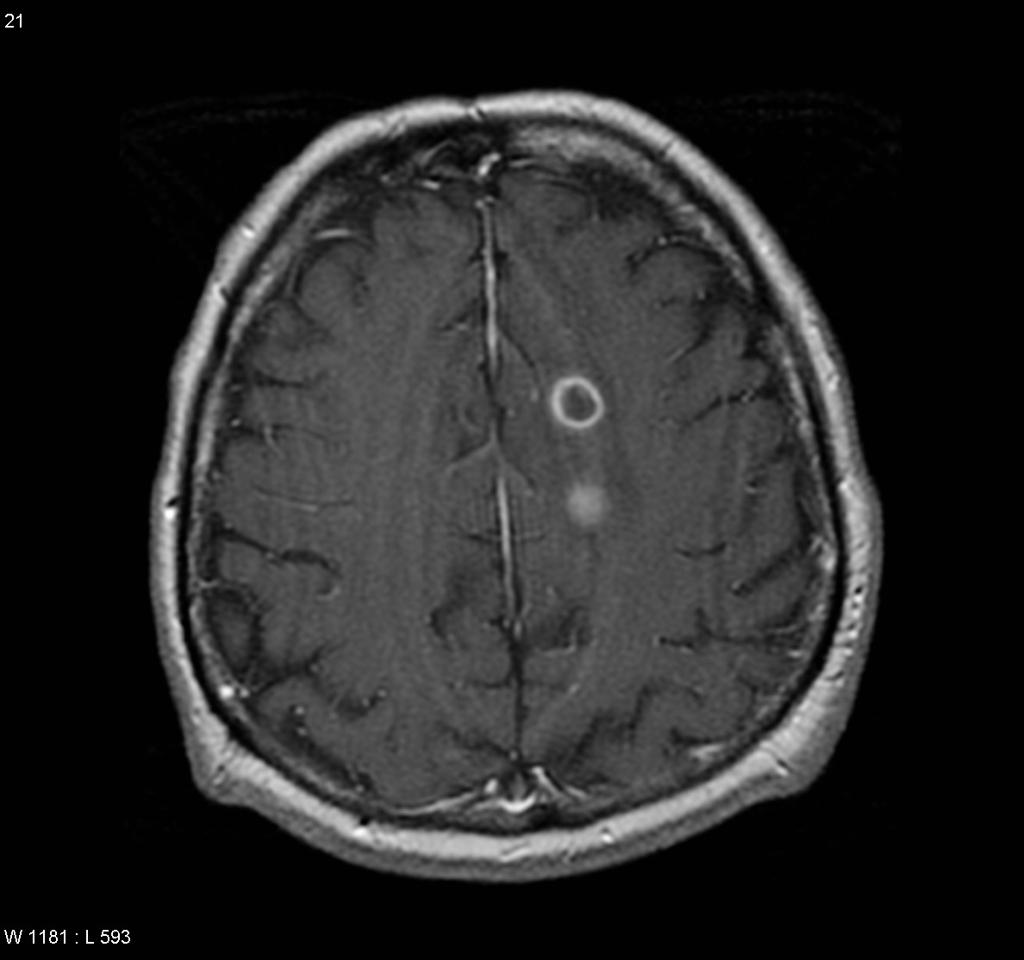
! | ![[Image:cerebral-absceses.jpg|center|300px|thumb|MRI brain showing brain abscess - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/ From the case https://radiopaedia.org/cases/4933"]] | ||
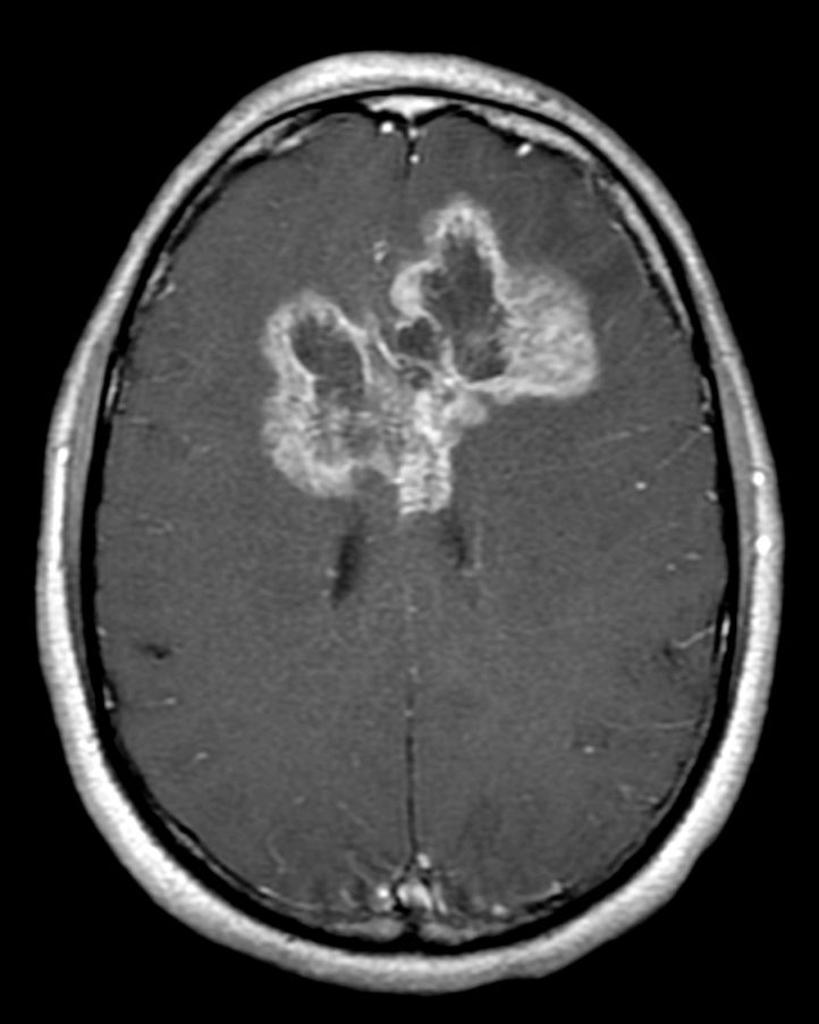
![[Image:butterfly1802.jpg|center|300px|thumb|MRI brain showing Glioblastoma multiforme - Case courtesy of A.Prof Frank Gaillard, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/28272">rID: 28272</a> ]] | |||
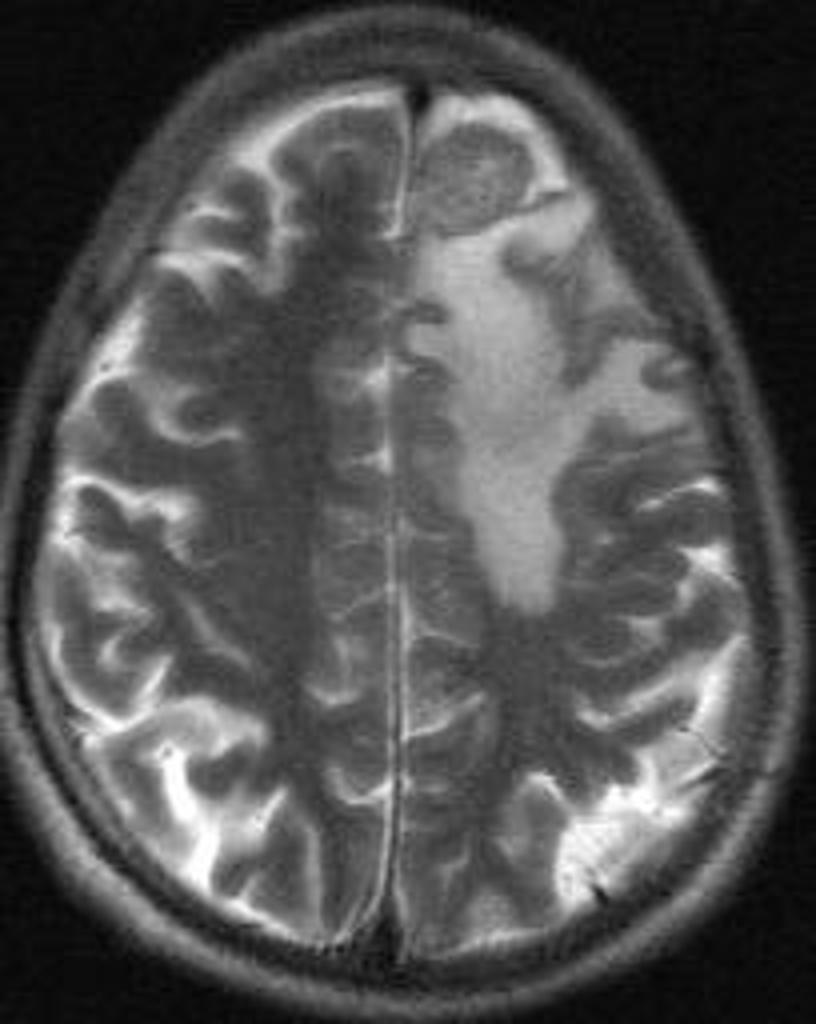
|- | ![[Image:intracranial-tuberculoma-mri-brain.jpg|center|300px|thumb|MRI brain showing tuberculoma - Case courtesy of Dr G Balachandran, https://radiopaedia.org/ From the case https://radiopaedia.org/cases/5489"]] | ||
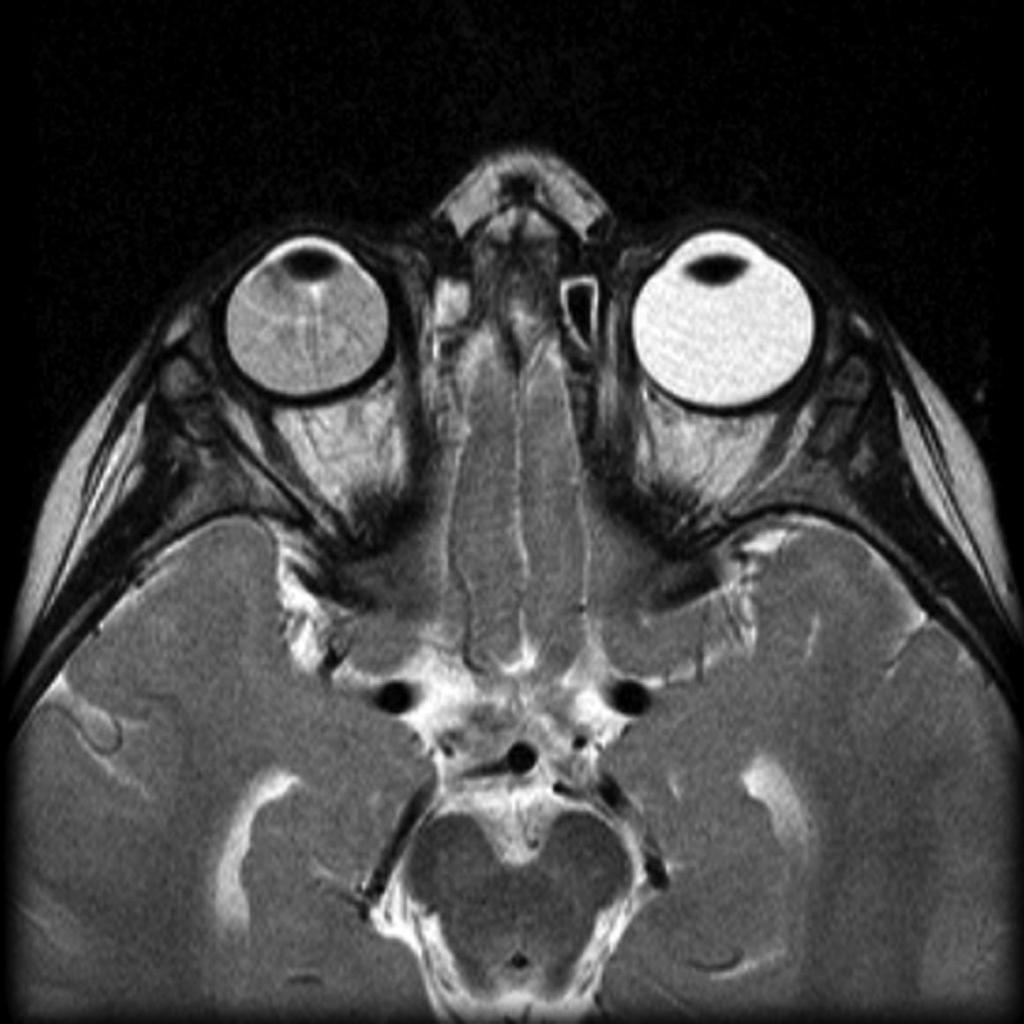
| | ![[Image:neurosarcoidosis-and-chiari-i-malformation.jpg|center|300px|thumb|MRI brain showing Neurosarcoidosis - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/ From the case https://radiopaedia.org/cases/4364S]] | ||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 101: | Line 102: | ||
!Radiological findings | !Radiological findings | ||
|- | |- | ||
| | |[[Coats disease]] | ||
| | | | ||
* Diagnosis made usually between 8-16 years (rarely in adulthood) | |||
* Wide range of symptoms from being [[asymptomatic]] to [[Decreased visual acuity|decreased vision]] and [[strabismus]]. | |||
* [[Decreased visual acuity]] at initial presentation has a poor prognosis. <ref name="urlHow to Diagnose and Manage Coats’ Disease">{{cite web |url=https://www.reviewofophthalmology.com/article/how-to-diagnose-and-manage-coatsand8217-disease-42782 |title=How to Diagnose and Manage Coats’ Disease |format= |work= |accessdate=}}</ref> | |||
| | | | ||
* [[Fundus (eye)|Fundus examination]] reveals vascular lesions and [[Exudate|exudates]]. | |||
* [[Fluorescein angiography]] is the best method to visualize the lesions. | |||
* [[CT]] and [[MRI]] are reserved for atypical cases.<ref name="urlHow to Diagnose and Manage Coats’ Disease">{{cite web |url=https://www.reviewofophthalmology.com/article/how-to-diagnose-and-manage-coatsand8217-disease-42782 |title=How to Diagnose and Manage Coats’ Disease |format= |work= |accessdate=}}</ref> | |||
|- | |- | ||
| | |[[Retinal detachment]] | ||
| | | | ||
* | * Most common presenting symptoms are [[photophobia]] and [[floaters]] | ||
* | * [[Visual field defect|Visual field defects]] (described as curtain falling from periphery to the center)<ref name="urlManagement of retinal detachment: a guide for non-ophthalmologists">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2405853/ |title=Management of retinal detachment: a guide for non-ophthalmologists |format= |work= |accessdate=}}</ref> | ||
| | | | ||
* | * [[Ophthalmoscope]] is not reliable in detecting retinal detachment as there might be associated [[hemorrhage]] | ||
* | * [[Ultrasound]] can be used to identify and localize the detachment.<ref name="urlManagement of retinal detachment: a guide for non-ophthalmologists">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2405853/ |title=Management of retinal detachment: a guide for non-ophthalmologists |format= |work= |accessdate=}}</ref> | ||
|- | |- | ||
| | |Hyperthyroid Ophthalmopathy | ||
| | | | ||
* | * The hallmark is [[Exophthalmos|Eye protrusion]], [[photophobia]], [[lacrimation]] and later in the disease, diminished eye motility.<ref name="urlThyroid Ophthalmopathy - EyeWiki">{{cite web |url=http://eyewiki.aao.org/Thyroid_Ophthalmopathy |title=Thyroid Ophthalmopathy - EyeWiki |format= |work= |accessdate=}}</ref> | ||
| | | | ||
* | * [[Ultrasonography]]: inflamed thickened [[extraocular muscles]]. | ||
* | * [[CT]]: shows [[inflamed]] muscle and free tendon from [[inflammation]] | ||
* [[MRI]]: shows periorbital fat expansion, increased water content of the muscles as a result of the [[inflammation]].<ref name="urlThyroid Ophthalmopathy - EyeWiki">{{cite web |url=http://eyewiki.aao.org/Thyroid_Ophthalmopathy |title=Thyroid Ophthalmopathy - EyeWiki |format= |work= |accessdate=}}</ref> | |||
|- | |- | ||
| | |[[Retinoblastoma]] | ||
|The | | | ||
* The most prominent sign is [[leukocoria]], followed by [[strabismus]] | |||
* The patient also may present with [[buphthalmos]], [[Cloudy cornea (patient information)|corneal clouding]] and eye tearing.<ref name="urlc.ymcdn.com">{{cite web |url=https://c.ymcdn.com/sites/www.covd.org/resource/resmgr/VDR_1-1/VDR1-1_article_Kollodge_Web.pdf+ |title=c.ymcdn.com |format= |work= |accessdate=}}</ref> | |||
| | | | ||
* [[Ultrasound]]: can detect the [[tumor]] as a result of the [[Calcification|calcifications]] inside. | |||
* [[MRI|MRI:]] assess [[Sella turcica|sellar]] and [[Parasellar and suprasellar disorders|parasellar]] regions .. it can also detect extraocular spread of the [[tumor]].<ref name="urlc.ymcdn.com">{{cite web |url=https://c.ymcdn.com/sites/www.covd.org/resource/resmgr/VDR_1-1/VDR1-1_article_Kollodge_Web.pdf+ |title=c.ymcdn.com |format= |work= |accessdate=}}</ref> | |||
|} | |||
{| class="wikitable" | |||
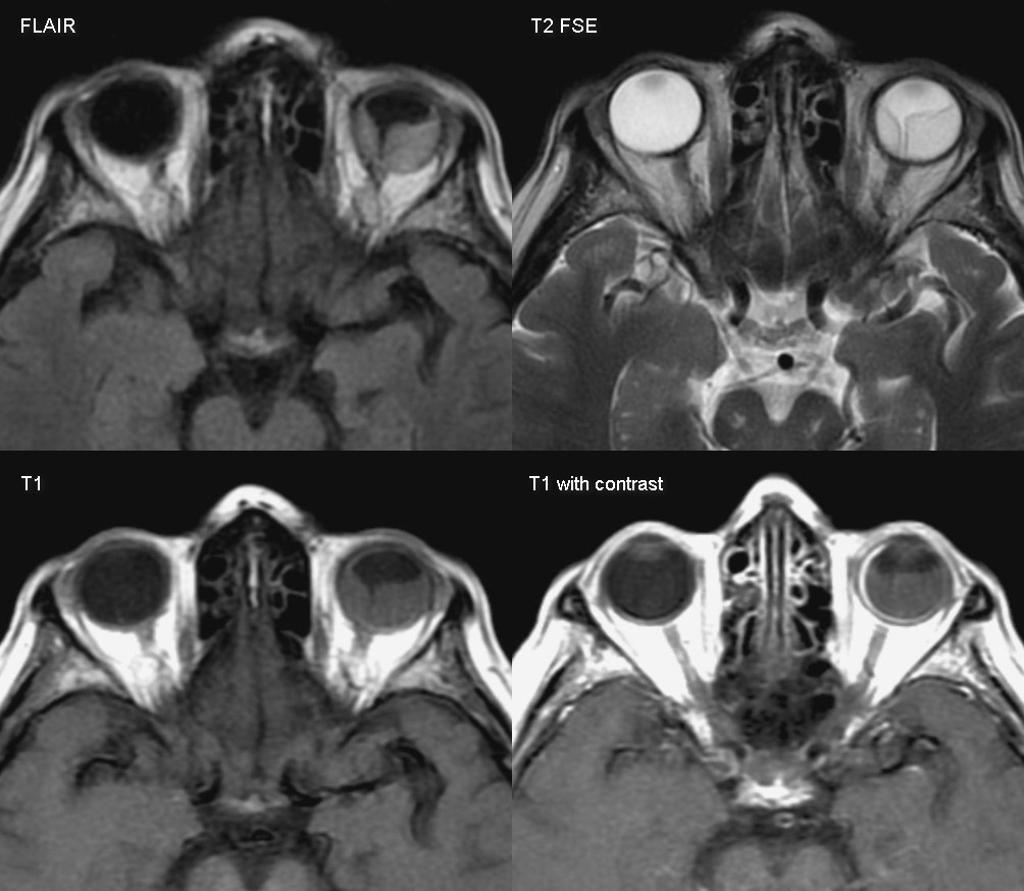
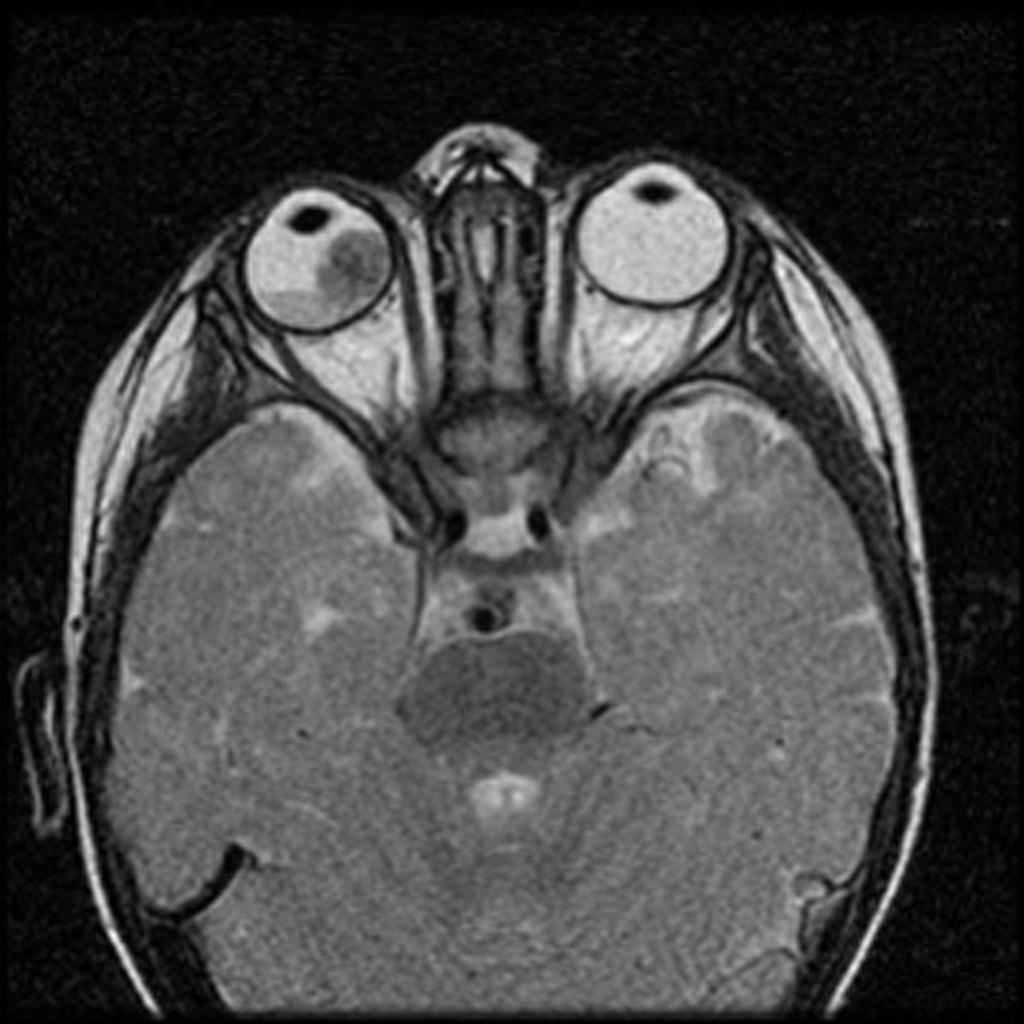
![[Image:Coats-disease-of-the-eye.jpg|center|300px|thumb|MRI of the orbit showing Coats disease - Case courtesy of Dr Michael Sargent, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/6089]] | |||
![[Image:Retinal-detachment-1.jpg|center|300px|thumb|MRI of the orbit showing retinal detachment - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/3134]] | |||
MRI | |||
![[Image:Retinoblastoma-3.jpg|center|300px|thumb|MRI of the orbit showing retinoblastoma - Case courtesy of https://radiopaedia.org/. From the case https://radiopaedia.org/cases/11877]] | |||
![[Image:Thyroid-orbitopathy-severe-2.jpg|center|300px|thumb|CT head showing hyperthyroid-induced orbitopathy - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/4854]] | |||
|} | |} | ||
| Line 167: | Line 151: | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | [[Category:Emergency medicine]] | ||
[[Category: | [[Category:Disease]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
[[Category: | [[Category:Neurology]] | ||
[[Category:Dermatology]] | |||
Latest revision as of 21:11, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Cysticercosis must be differentiated from other diseases that cause brain cystic lesions (as brain abscess and brain tumors) or ocular lesions (as retinal detachment and coats disease).
Differentiating cysticercosis from other diseases
| Disease | Prominent clinical features | Lab findings | Radiological findings |
|---|---|---|---|
| Neurocysticercosis |
|
|
|
| Brain abscess |
|
|
|
| Brain tumors |
|
| |
| Brain tuberculoma |
|
|
|
| Neurosarcoidosis |
|
|
|
 |
 |
 |
 |
|---|
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Coats disease |
|
|
| Retinal detachment |
|
|
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
 |
 |
 |
 |
|---|
References
- ↑ Brouwer MC, Tunkel AR, McKhann GM, van de Beek D (2014). "Brain abscess". N. Engl. J. Med. 371 (5): 447–56. doi:10.1056/NEJMra1301635. PMID 25075836.
- ↑ "Brain Abscess — NEJM".
- ↑ 3.0 3.1 "Primary Brain Tumors in Adults - American Family Physician".
- ↑ "The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF".
- ↑ 5.0 5.1 "Neurosarcoidosis".
- ↑ 6.0 6.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 7.0 7.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 8.0 8.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 9.0 9.1 "c.ymcdn.com".