Chronic pancreatitis pathophysiology: Difference between revisions
Iqra Qamar (talk | contribs) |
|||
| (33 intermediate revisions by 3 users not shown) | |||
| Line 7: | Line 7: | ||
__NOTOC__ | __NOTOC__ | ||
{{Chronic pancreatitis}} | {{Chronic pancreatitis}} | ||
{{CMG}} | {{CMG}}; {{AE}} {{IQ}} | ||
==Overview== | ==Overview== | ||
Chronic pancreatitis is a progressive [[inflammatory]] process leading to irreversible structural damage to the [[pancreas]] resulting in [[exocrine]] and [[endocrine]] dysfunction. The [[pathogenesis]] is still unclear and multifactorial. Decreased [[bicarbonate]] secretion and intrapancreatic activation of [[digestive enzymes]] is thought to play an important role in the [[pathogenesis]] of chronic pancreatitis. Other factors that are thought to play an important role in the [[pathogenesis]] of chronic pancreatitis may include intraductal plugging and obstruction, direct injury to [[pancreatic]] [[cells]] induced by toxins and toxic metabolites, [[antioxidants]], [[ischemia]], [[autoimmune disorders]], the sentinal [[acute pancreatitis]] event (SAPE), [[necrosis]] and [[fibrosis]]. [[Genes]] involved in the [[pathogenesis]] of chronic pancreatitis include [[Cystic fibrosis transmembrane conductance regulator|CFTR-]]<nowiki/>[[cystic fibrosis]] [[gene mutation]], SPINK-1 [[mutation]], which encodes for [[trypsin inhibitor]], PRSS-1 [[gene mutation]] linked to [[hereditary pancreatitis]], claudin-2 ([[CLDN2]]), and [[carboxypeptidase A1]] ([[Carboxypeptidase A|CPA1]]) [[Gene mutation|gene mutations]]. Associated conditions may include [[autoimmune]] conditions, [[primary biliary cirrhosis]], [[primary sclerosing cholangitis]], [[Sjögren's syndrome|Sjögren syndrome]], and [[renal tubular acidosis]]. [[Gross pathology]] may include enlarged or [[atrophic]] [[pancreas]], [[cysts]], [[Calcification|calcifications]], [[fibrosis]] and patchy focal [[necrosis]]. [[Microscopic]] [[histopathological]] analysis may show patchy focal disease characterized by a [[Mononuclear cells|mononuclear]] infiltrate. | |||
==Pathophysiology== | ==Pathophysiology== | ||
Chronic pancreatitis is a progressive [[inflammatory]] process leading to irreversible structural damage to the pancreas resulting in [[exocrine]] and [[endocrine]] dysfunction.<ref name="pmid7739686">{{cite journal |vauthors=Steer ML, Waxman I, Freedman S |title=Chronic pancreatitis |journal=N. Engl. J. Med. |volume=332 |issue=22 |pages=1482–90 |year=1995 |pmid=7739686 |doi=10.1056/NEJM199506013322206 |url=}}</ref> The [[pathogenesis]] is still unclear and multifactorial; but two mechanisms that play an important role in the [[pathogenesis]] of chronic pancreatitis, which are as follows: | |||
=== Decreased | === Decreased bicarbonate secretion: === | ||
A decrease in [[bicarbonate]] secretion may be due to any of the following causes: | |||
* | * [[Genetic]] causes leading to functional abnormalities of ductal cells | ||
* Obstructive causes such as: | |||
** [[Stricture]] | |||
** [[Malignancy]] | |||
** [[Tumor]] | |||
* Protein hypersecretion resulting in proteinaceous ductal plugs leading to ductal blockage and obstruction<ref name="pmid510088">{{cite journal |vauthors=Sahel J, Sarles H |title=Modifications of pure human pancreatic juice induced by chronic alcohol consumption |journal=Dig. Dis. Sci. |volume=24 |issue=12 |pages=897–905 |year=1979 |pmid=510088 |doi= |url=}}</ref> | * [[Protein]] hypersecretion resulting in proteinaceous ductal plugs leading to ductal blockage and obstruction<ref name="pmid510088">{{cite journal |vauthors=Sahel J, Sarles H |title=Modifications of pure human pancreatic juice induced by chronic alcohol consumption |journal=Dig. Dis. Sci. |volume=24 |issue=12 |pages=897–905 |year=1979 |pmid=510088 |doi= |url=}}</ref> | ||
=== Intrapancreatic activation of digestive enzymes: === | === Intrapancreatic activation of digestive enzymes: === | ||
* Usually results from genetic causes leading to | * Usually results from [[genetic]] causes leading to: | ||
** Impaired enzyme activation and regulation | ** Impaired [[enzyme]] activation and regulation | ||
** Predisposition to injury from toxic environmental stimuli such as alcohol or cigarette smoking | ** Predisposition to injury from toxic environmental stimuli such as [[alcohol]] or [[cigarette smoking]] | ||
[[Image:1024px-Pancreatic stellate cell activation in chronic pancreatitis and pancreatic cancer.jpg|500 px|thumb|center|By Robert Jaster [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons]] | |||
Other factors that are thought to play an important role in the [[pathogenesis]] of chronic pancreatitis include: | |||
==== (a) Intraductal plugging and obstruction ==== | ==== (a) Intraductal plugging and obstruction ==== | ||
===== 1) Proteinaceous ductal plugs ===== | ===== 1) Proteinaceous ductal plugs ===== | ||
* Interlobular and intralobular duct blockage due to abnormal secretion of pancreatic proteins in the pancreatic juice<ref name="pmid510088">{{cite journal |vauthors=Sahel J, Sarles H |title=Modifications of pure human pancreatic juice induced by chronic alcohol consumption |journal=Dig. Dis. Sci. |volume=24 |issue=12 |pages=897–905 |year=1979 |pmid=510088 |doi= |url=}}</ref> | * [[Interlobular duct|Interlobular]] and [[intralobular duct]] blockage due to abnormal secretion of pancreatic [[proteins]] in the [[pancreatic juice]].<ref name="pmid510088">{{cite journal |vauthors=Sahel J, Sarles H |title=Modifications of pure human pancreatic juice induced by chronic alcohol consumption |journal=Dig. Dis. Sci. |volume=24 |issue=12 |pages=897–905 |year=1979 |pmid=510088 |doi= |url=}}</ref> | ||
** GP2, a glycosyl phosphatidylinositol anchored protein is found to be a major component of | ** GP2, a glycosyl phosphatidylinositol anchored [[protein]] is found to be a major component of plugs.<ref name="pmid8326020">{{cite journal |vauthors=Freedman SD, Sakamoto K, Venu RP |title=GP2, the homologue to the renal cast protein uromodulin, is a major component of intraductal plugs in chronic pancreatitis |journal=J. Clin. Invest. |volume=92 |issue=1 |pages=83–90 |year=1993 |pmid=8326020 |pmc=293537 |doi=10.1172/JCI116602 |url=}}</ref> | ||
** Low levels of lithostathine in alcoholics, a | ** Low levels of lithostathine in [[Alcoholic|alcoholics]], a protective [[protein]] secreted by [[pancreatic]] [[acinar cells]] that prevent stone ([[calcium carbonate]]) formation.<ref name="pmid6401181">{{cite journal |vauthors=Guy O, Robles-Diaz G, Adrich Z, Sahel J, Sarles H |title=Protein content of precipitates present in pancreatic juice of alcoholic subjects and patients with chronic calcifying pancreatitis |journal=Gastroenterology |volume=84 |issue=1 |pages=102–7 |year=1983 |pmid=6401181 |doi= |url=}}</ref> | ||
* These proteinaceous plugs are the major sites for calcification and stone formation leading to: | * These proteinaceous plugs are the major sites for [[calcification]] and stone formation leading to: | ||
** Ductal epithelial lesions and inflammatory changes | ** Ductal [[epithelial]] [[lesions]] and [[inflammatory]] changes | ||
** Scarring | ** [[Scarring]] | ||
** Obstruction | ** Obstruction | ||
===== 2) Intraductal obstruction due to other causes ===== | ===== 2) Intraductal obstruction due to other causes ===== | ||
* | * Chronic exposure to stones results in damage to ductal [[epithelial cells]] and [[Acinar gland|acinar glands]] via: | ||
* | ** [[Ulceration]] | ||
* Ethanol abuse | ** [[Scarring]] | ||
** Obstruction | |||
* Biliaropancreatic [[tumors]] ([[pancreatic]] [[adenocarcinoma]], [[neuroendocrine tumors]], and intrapapillary [[mucinous]] [[tumors]]) | |||
* [[Ethanol]] abuse | |||
** [[Alcohol]] may increase the lithogenecity of [[pancreatic juice]] resulting in increased stone formation | |||
==== (b) Direct injury to pancreatic cells induced by toxins and toxic metabolites ==== | ==== (b) Direct injury to pancreatic cells induced by toxins and toxic metabolites ==== | ||
* Alcohol is proposed to have a direct toxic effect on the [[pancreas]]. | * [[Alcohol]] is proposed to have a direct toxic effect on the [[pancreas]] and damage the [[acinar cells]] via a change in [[intracellular]] [[metabolism]] ([[mitochondrial]] damage). | ||
* It is metabolized by the [[pancreas]] and may result in [[oxidative stress]] and induce the release of pancreatic enzymes. This excessive release may result in autodigestion of the gland. | * It is metabolized by the [[pancreas]] and may result in [[oxidative stress]] and induce the release of pancreatic enzymes. This excessive release may result in autodigestion of the [[gland]]. | ||
* Additionally, alcohol may result in activation of pancreatic [[Stellate cell|stellate cells]] which are primarily responsible for [[fibrosis]] of the gland and weakening of the intracellular membranes, which results in anatomical changes in the pancreas, further predisposing to pathological autodigestion.<ref name="pmid21091991">{{cite journal| author=Apte MV, Pirola RC, Wilson JS| title=Mechanisms of alcoholic pancreatitis. | journal=J Gastroenterol Hepatol | year= 2010 | volume= 25 | issue= 12 | pages= 1816-26 | pmid=21091991 | doi=10.1111/j.1440-1746.2010.06445.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21091991 }}</ref><ref name="acutepancreatitis">{{cite journal | * Additionally, [[alcohol]] may result in activation of [[pancreatic]] [[Stellate cell|stellate cells]] which are primarily responsible for [[fibrosis]] of the [[gland]] and weakening of the [[intracellular]] [[membranes]], which results in [[anatomical]] changes in the [[pancreas]], further predisposing to pathological autodigestion.<ref name="pmid21091991">{{cite journal| author=Apte MV, Pirola RC, Wilson JS| title=Mechanisms of alcoholic pancreatitis. | journal=J Gastroenterol Hepatol | year= 2010 | volume= 25 | issue= 12 | pages= 1816-26 | pmid=21091991 | doi=10.1111/j.1440-1746.2010.06445.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21091991 }}</ref><ref name="acutepancreatitis">{{cite journal | ||
| last = Forsmark | | last = Forsmark | ||
| first = Chris E. | | first = Chris E. | ||
| Line 70: | Line 78: | ||
| name-list-format = vanc | | name-list-format = vanc | ||
}}</ref> | }}</ref> | ||
* [[Smoking]] may exacerbate [[pancreatitis]] in alcoholics. | |||
* [[Smoking]] is also found as an independent [[risk factor]] in the development and progression of [[pancreatitis]] as: | |||
** It may affect [[pancreatic]] [[bicarbonate]] and water secretion | |||
** It may predispose to [[oxidative stress]] | |||
** It may also increases the rate of [[pancreatic]] [[calcification]] | |||
==== (c) Antioxidants ==== | ==== (c) Antioxidants ==== | ||
* Steatorrhea in chronic pancreatitis may lead to nutritional deficiencies and decreased levels of antioxidants such as<ref name="pmid3957720">{{cite journal |vauthors=Rose P, Fraine E, Hunt LP, Acheson DW, Braganza JM |title=Dietary antioxidants and chronic pancreatitis |journal=Hum Nutr Clin Nutr |volume=40 |issue=2 |pages=151–64 |year=1986 |pmid=3957720 |doi= |url=}}</ref><ref name="pmid3224602">{{cite journal |vauthors=Uden S, Acheson DW, Reeves J, Worthington HV, Hunt LP, Brown S, Braganza JM |title=Antioxidants, enzyme induction, and chronic pancreatitis: a reappraisal following studies in patients on anticonvulsants |journal=Eur J Clin Nutr |volume=42 |issue=7 |pages=561–9 |year=1988 |pmid=3224602 |doi= |url=}}</ref> | * [[Steatorrhea]] in chronic pancreatitis may lead to [[nutritional deficiencies]] and decreased levels of [[antioxidants]] such as:<ref name="pmid3957720">{{cite journal |vauthors=Rose P, Fraine E, Hunt LP, Acheson DW, Braganza JM |title=Dietary antioxidants and chronic pancreatitis |journal=Hum Nutr Clin Nutr |volume=40 |issue=2 |pages=151–64 |year=1986 |pmid=3957720 |doi= |url=}}</ref><ref name="pmid3224602">{{cite journal |vauthors=Uden S, Acheson DW, Reeves J, Worthington HV, Hunt LP, Brown S, Braganza JM |title=Antioxidants, enzyme induction, and chronic pancreatitis: a reappraisal following studies in patients on anticonvulsants |journal=Eur J Clin Nutr |volume=42 |issue=7 |pages=561–9 |year=1988 |pmid=3224602 |doi= |url=}}</ref> | ||
** Selenium | ** [[Selenium]] | ||
** Vitamin C and E | ** [[Vitamin C]] and [[Vitamin E|E]] | ||
** Methionine | ** [[Methionine]] | ||
* Decreased antioxidant levels may result in:<ref name="pmid3361161">{{cite journal |vauthors=Braganza JM, Thomas A, Robinson A |title=Antioxidants to treat chronic pancreatitis in childhood? Case report and possible implications for pathogenesis |journal=Int. J. Pancreatol. |volume=3 |issue=2-3 |pages=209–16 |year=1988 |pmid=3361161 |doi=10.1007/BF02798933 |url=}}</ref><ref name="pmid18952082">{{cite journal |vauthors=Bhardwaj P, Garg PK, Maulik SK, Saraya A, Tandon RK, Acharya SK |title=A randomized controlled trial of antioxidant supplementation for pain relief in patients with chronic pancreatitis |journal=Gastroenterology |volume=136 |issue=1 |pages=149–159.e2 |year=2009 |pmid=18952082 |doi=10.1053/j.gastro.2008.09.028 |url=}}</ref><ref name="pmid21083584">{{cite journal |vauthors=Burton F, Alkaade S, Collins D, Muddana V, Slivka A, Brand RE, Gelrud A, Banks PA, Sherman S, Anderson MA, Romagnuolo J, Lawrence C, Baillie J, Gardner TB, Lewis MD, Amann ST, Lieb JG, O'Connell M, Kennard ED, Yadav D, Whitcomb DC, Forsmark CE |title=Use and perceived effectiveness of non-analgesic medical therapies for chronic pancreatitis in the United States |journal=Aliment. Pharmacol. Ther. |volume=33 |issue=1 |pages=149–59 |year=2011 |pmid=21083584 |pmc=3142582 |doi=10.1111/j.1365-2036.2010.04491.x |url=}}</ref> | * Decreased [[antioxidant]] levels may result in:<ref name="pmid3361161">{{cite journal |vauthors=Braganza JM, Thomas A, Robinson A |title=Antioxidants to treat chronic pancreatitis in childhood? Case report and possible implications for pathogenesis |journal=Int. J. Pancreatol. |volume=3 |issue=2-3 |pages=209–16 |year=1988 |pmid=3361161 |doi=10.1007/BF02798933 |url=}}</ref><ref name="pmid18952082">{{cite journal |vauthors=Bhardwaj P, Garg PK, Maulik SK, Saraya A, Tandon RK, Acharya SK |title=A randomized controlled trial of antioxidant supplementation for pain relief in patients with chronic pancreatitis |journal=Gastroenterology |volume=136 |issue=1 |pages=149–159.e2 |year=2009 |pmid=18952082 |doi=10.1053/j.gastro.2008.09.028 |url=}}</ref><ref name="pmid21083584">{{cite journal |vauthors=Burton F, Alkaade S, Collins D, Muddana V, Slivka A, Brand RE, Gelrud A, Banks PA, Sherman S, Anderson MA, Romagnuolo J, Lawrence C, Baillie J, Gardner TB, Lewis MD, Amann ST, Lieb JG, O'Connell M, Kennard ED, Yadav D, Whitcomb DC, Forsmark CE |title=Use and perceived effectiveness of non-analgesic medical therapies for chronic pancreatitis in the United States |journal=Aliment. Pharmacol. Ther. |volume=33 |issue=1 |pages=149–59 |year=2011 |pmid=21083584 |pmc=3142582 |doi=10.1111/j.1365-2036.2010.04491.x |url=}}</ref> | ||
** Increased free radical formation | ** Increased [[free radical]] formation | ||
** Lipid peroxidation | ** [[Lipid peroxidation]] | ||
** Cellular damage | ** [[Cellular]] damage | ||
==== (d) Ischemia ==== | ==== (d) Ischemia ==== | ||
* Ischemia is an important precipitating factor in the pathogenesis of chronic pancreatitis | * [[Ischemia]] is an important precipitating factor in the [[pathogenesis]] of chronic pancreatitis. | ||
* Fibrosis and inelasticity of pancreatic tissue seen in chronic pancreatitis may lead to: | * [[Fibrosis]] and inelasticity of [[pancreatic]] [[Tissue (biology)|tissue]] seen in chronic pancreatitis may lead to: | ||
**Increased pancreatic interstitial pressure | **Increased [[pancreatic]] [[interstitial]] pressure | ||
**Increased intraductal pressure and ductal hypertension<ref name="pmid1735346">{{cite journal |vauthors=Karanjia ND, Singh SM, Widdison AL, Lutrin FJ, Reber HA |title=Pancreatic ductal and interstitial pressures in cats with chronic pancreatitis |journal=Dig. Dis. Sci. |volume=37 |issue=2 |pages=268–73 |year=1992 |pmid=1735346 |doi= |url=}}</ref> | **Increased intraductal pressure and ductal hypertension<ref name="pmid1735346">{{cite journal |vauthors=Karanjia ND, Singh SM, Widdison AL, Lutrin FJ, Reber HA |title=Pancreatic ductal and interstitial pressures in cats with chronic pancreatitis |journal=Dig. Dis. Sci. |volume=37 |issue=2 |pages=268–73 |year=1992 |pmid=1735346 |doi= |url=}}</ref> | ||
**Chronic ischemia and necrosis of pancreatic gland<ref name="pmid7514552">{{cite journal |vauthors=Tanaka T, Ichiba Y, Miura Y, Ito H, Dohi K |title=Canine model of chronic pancreatitis due to chronic ischemia |journal=Digestion |volume=55 |issue=2 |pages=86–9 |year=1994 |pmid=7514552 |doi= |url=}}</ref> | **Chronic [[ischemia]] and [[necrosis]] of [[Pancreas|pancreatic gland]]<ref name="pmid7514552">{{cite journal |vauthors=Tanaka T, Ichiba Y, Miura Y, Ito H, Dohi K |title=Canine model of chronic pancreatitis due to chronic ischemia |journal=Digestion |volume=55 |issue=2 |pages=86–9 |year=1994 |pmid=7514552 |doi= |url=}}</ref> | ||
==== (e) Autoimmune disorders ==== | ==== (e) Autoimmune disorders ==== | ||
*Chronic pancreatitis | *Chronic pancreatitis has been found to be associated with [[autoimmune]] conditions such as:<ref name="pmid7129026">{{cite journal |vauthors=Epstein O, Chapman RW, Lake-Bakaar G, Foo AY, Rosalki SB, Sherlock S |title=The pancreas in primary biliary cirrhosis and primary sclerosing cholangitis |journal=Gastroenterology |volume=83 |issue=6 |pages=1177–82 |year=1982 |pmid=7129026 |doi= |url=}}</ref><ref name="pmid8022761">{{cite journal |vauthors=Nishimori I, Yamamoto Y, Okazaki K, Morita M, Onodera M, Kino J, Tamura S, Yamamoto Y |title=Identification of autoantibodies to a pancreatic antigen in patients with idiopathic chronic pancreatitis and Sjögren's syndrome |journal=Pancreas |volume=9 |issue=3 |pages=374–81 |year=1994 |pmid=8022761 |doi= |url=}}</ref> | ||
**Sjögren's syndrome | **[[Sjögren's syndrome]] | ||
**Primary biliary cirrhosis | **[[Primary biliary cirrhosis]] | ||
**Renal tubular | **[[Renal tubular acidosis]] | ||
*HLA-DR antigen expression with T-cell inflammatory infiltrate is seen on | *[[HLA-DR]] [[antigen]] expression with [[T-cell]] [[inflammatory]] infiltrate is seen on ductal cells in some cases of [[idiopathic]] chronic pancreatitis.<ref name="pmid3498162">{{cite journal |vauthors=Bovo P, Mirakian R, Merigo F, Angelini G, Cavallini G, Rizzini P, Bottazzo GF, Scuro LA |title=HLA molecule expression on chronic pancreatitis specimens: is there a role for autoimmunity? A preliminary study |journal=Pancreas |volume=2 |issue=3 |pages=350–6 |year=1987 |pmid=3498162 |doi= |url=}}</ref> | ||
==== (f) Necrosis and fibrosis ==== | ==== (f) Necrosis and fibrosis ==== | ||
* Recurrent attacks of acute pancreatitis may lead to chronic pancreatitis due to | * Recurrent attacks of [[acute pancreatitis]] may lead to chronic pancreatitis due to:<ref name="pmid12079262">{{cite journal |vauthors=Schneider A, Whitcomb DC |title=Hereditary pancreatitis: a model for inflammatory diseases of the pancreas |journal=Best Pract Res Clin Gastroenterol |volume=16 |issue=3 |pages=347–63 |year=2002 |pmid=12079262 |doi=10.1053/bega.2002.0311 |url=}}</ref><ref name="pmid19603011">{{cite journal |vauthors=Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB, Maisonneuve P |title=Natural history of acute pancreatitis: a long-term population-based study |journal=Am. J. Gastroenterol. |volume=104 |issue=11 |pages=2797–805; quiz 2806 |year=2009 |pmid=19603011 |doi=10.1038/ajg.2009.405 |url=}}</ref> | ||
** Necrosis | ** [[Necrosis]] | ||
** Fibrosis | ** [[Fibrosis]] | ||
** Scarring of pancreatic gland | ** [[Scarring]] of [[Pancreas|pancreatic gland]] | ||
** Intrinsic compression of the [[pancreatic]] ductules | |||
*Progression from acute to chronic pancreatitis is dependent upon the number and severity of acute attacks<ref name="pmid8174996">{{cite journal |vauthors=Ammann RW, Muellhaupt B |title=Progression of alcoholic acute to chronic pancreatitis |journal=Gut |volume=35 |issue=4 |pages=552–6 |year=1994 |pmid=8174996 |pmc=1374808 |doi= |url=}}</ref> | |||
==== (g) The sentinal acute pancreatitis event (SAPE) hypothesis: ==== | |||
* SAPE hypothesis explains the role of [[pancreatic]] stellate cells in chronic pancreatitis<ref name="pmid12079262">{{cite journal |vauthors=Schneider A, Whitcomb DC |title=Hereditary pancreatitis: a model for inflammatory diseases of the pancreas |journal=Best Pract Res Clin Gastroenterol |volume=16 |issue=3 |pages=347–63 |year=2002 |pmid=12079262 |doi=10.1053/bega.2002.0311 |url=}}</ref><ref name="pmid20125091">{{cite journal |vauthors=Yadav D, Whitcomb DC |title=The role of alcohol and smoking in pancreatitis |journal=Nat Rev Gastroenterol Hepatol |volume=7 |issue=3 |pages=131–45 |year=2010 |pmid=20125091 |doi=10.1038/nrgastro.2010.6 |url=}}</ref> | |||
* It explains the [[pathogenesis]] of chronic pancreatitis as a continuum of 3 sequential changes: | |||
** Pre-[[acute pancreatitis]] | |||
*** Based on the assumption that chronic pancreatitis occurs in [[genetically]] or environmentally susceptible people or who are at increased risk | |||
** The sentinel attack of [[acute pancreatitis]], which involves: | |||
*** Triggering of [[chronic]] [[inflammation]] in the predisposed patients | |||
*** Activation and recruitment of [[Stellate cell|stellate cells]] | |||
** Progression phase, with [[immune system]] activation that ultimately resulting in: | |||
*** Progression of [[inflammation]] | |||
*** Irreversible changes | |||
[[Image:PMC3274456 1755-1536-4-26-1.png|500 px|thumb|center|Source: nih.gov]] | |||
==Genetics== | ==Genetics== | ||
Genes involved in the pathogenesis of chronic pancreatitis include: | Genes involved in the pathogenesis of chronic pancreatitis include: | ||
* CFTR-Cystic fibrosis gene mutation<ref name="pmid16193325">{{cite journal |vauthors=Bishop MD, Freedman SD, Zielenski J, Ahmed N, Dupuis A, Martin S, Ellis L, Shea J, Hopper I, Corey M, Kortan P, Haber G, Ross C, Tzountzouris J, Steele L, Ray PN, Tsui LC, Durie PR |title=The cystic fibrosis transmembrane conductance regulator gene and ion channel function in patients with idiopathic pancreatitis |journal=Hum. Genet. |volume=118 |issue=3-4 |pages=372–81 |year=2005 |pmid=16193325 |doi=10.1007/s00439-005-0059-z |url=}}</ref><ref name="pmid20416310">{{cite journal |vauthors=Ooi CY, Gonska T, Durie PR, Freedman SD |title=Genetic testing in pancreatitis |journal=Gastroenterology |volume=138 |issue=7 |pages=2202–6, 2206.e1 |year=2010 |pmid=20416310 |doi=10.1053/j.gastro.2010.04.022 |url=}}</ref> | * [https://en.wikipedia.org/wiki/Cystic_fibrosis CFTR-Cystic fibrosis gene mutation]<ref name="pmid16193325">{{cite journal |vauthors=Bishop MD, Freedman SD, Zielenski J, Ahmed N, Dupuis A, Martin S, Ellis L, Shea J, Hopper I, Corey M, Kortan P, Haber G, Ross C, Tzountzouris J, Steele L, Ray PN, Tsui LC, Durie PR |title=The cystic fibrosis transmembrane conductance regulator gene and ion channel function in patients with idiopathic pancreatitis |journal=Hum. Genet. |volume=118 |issue=3-4 |pages=372–81 |year=2005 |pmid=16193325 |doi=10.1007/s00439-005-0059-z |url=}}</ref><ref name="pmid20416310">{{cite journal |vauthors=Ooi CY, Gonska T, Durie PR, Freedman SD |title=Genetic testing in pancreatitis |journal=Gastroenterology |volume=138 |issue=7 |pages=2202–6, 2206.e1 |year=2010 |pmid=20416310 |doi=10.1053/j.gastro.2010.04.022 |url=}}</ref> | ||
* SPINK-1, which encodes for trypsin inhibitor<ref name="pmid10835640">{{cite journal |vauthors=Witt H, Luck W, Hennies HC, Classen M, Kage A, Lass U, Landt O, Becker M |title=Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis |journal=Nat. Genet. |volume=25 |issue=2 |pages=213–6 |year=2000 |pmid=10835640 |doi=10.1038/76088 |url=}}</ref> | * [[SPINK1|SPINK-1]], which encodes for trypsin inhibitor<ref name="pmid10835640">{{cite journal |vauthors=Witt H, Luck W, Hennies HC, Classen M, Kage A, Lass U, Landt O, Becker M |title=Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis |journal=Nat. Genet. |volume=25 |issue=2 |pages=213–6 |year=2000 |pmid=10835640 |doi=10.1038/76088 |url=}}</ref> | ||
* PRSS-1 gene linked to hereditary pancreatitis | * [https://www.wikigenes.org/e/gene/e/5644.html PRSS-1 gene] linked to hereditary pancreatitis | ||
* Claudin-2 (CLDN2)<ref name="pmid23143602">{{cite journal |vauthors=Whitcomb DC, LaRusch J, Krasinskas AM, Klei L, Smith JP, Brand RE, Neoptolemos JP, Lerch MM, Tector M, Sandhu BS, Guda NM, Orlichenko L, Alkaade S, Amann ST, Anderson MA, Baillie J, Banks PA, Conwell D, Coté GA, Cotton PB, DiSario J, Farrer LA, Forsmark CE, Johnstone M, Gardner TB, Gelrud A, Greenhalf W, Haines JL, Hartman DJ, Hawes RA, Lawrence C, Lewis M, Mayerle J, Mayeux R, Melhem NM, Money ME, Muniraj T, Papachristou GI, Pericak-Vance MA, Romagnuolo J, Schellenberg GD, Sherman S, Simon P, Singh VP, Slivka A, Stolz D, Sutton R, Weiss FU, Wilcox CM, Zarnescu NO, Wisniewski SR, O'Connell MR, Kienholz ML, Roeder K, Barmada MM, Yadav D, Devlin B |title=Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis |journal=Nat. Genet. |volume=44 |issue=12 |pages=1349–54 |year=2012 |pmid=23143602 |pmc=3510344 |doi=10.1038/ng.2466 |url=}}</ref> | * Claudin-2 ([[CLDN2]])<ref name="pmid23143602">{{cite journal |vauthors=Whitcomb DC, LaRusch J, Krasinskas AM, Klei L, Smith JP, Brand RE, Neoptolemos JP, Lerch MM, Tector M, Sandhu BS, Guda NM, Orlichenko L, Alkaade S, Amann ST, Anderson MA, Baillie J, Banks PA, Conwell D, Coté GA, Cotton PB, DiSario J, Farrer LA, Forsmark CE, Johnstone M, Gardner TB, Gelrud A, Greenhalf W, Haines JL, Hartman DJ, Hawes RA, Lawrence C, Lewis M, Mayerle J, Mayeux R, Melhem NM, Money ME, Muniraj T, Papachristou GI, Pericak-Vance MA, Romagnuolo J, Schellenberg GD, Sherman S, Simon P, Singh VP, Slivka A, Stolz D, Sutton R, Weiss FU, Wilcox CM, Zarnescu NO, Wisniewski SR, O'Connell MR, Kienholz ML, Roeder K, Barmada MM, Yadav D, Devlin B |title=Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis |journal=Nat. Genet. |volume=44 |issue=12 |pages=1349–54 |year=2012 |pmid=23143602 |pmc=3510344 |doi=10.1038/ng.2466 |url=}}</ref> | ||
* Carboxypeptidase A1 (CPA1) genes<ref name="pmid23955596">{{cite journal |vauthors=Witt H, Beer S, Rosendahl J, Chen JM, Chandak GR, Masamune A, Bence M, Szmola R, Oracz G, Macek M, Bhatia E, Steigenberger S, Lasher D, Bühler F, Delaporte C, Tebbing J, Ludwig M, Pilsak C, Saum K, Bugert P, Masson E, Paliwal S, Bhaskar S, Sobczynska-Tomaszewska A, Bak D, Balascak I, Choudhuri G, Nageshwar Reddy D, Rao GV, Thomas V, Kume K, Nakano E, Kakuta Y, Shimosegawa T, Durko L, Szabó A, Schnúr A, Hegyi P, Rakonczay Z, Pfützer R, Schneider A, Groneberg DA, Braun M, Schmidt H, Witt U, Friess H, Algül H, Landt O, Schuelke M, Krüger R, Wiedenmann B, Schmidt F, Zimmer KP, Kovacs P, Stumvoll M, Blüher M, Müller T, Janecke A, Teich N, Grützmann R, Schulz HU, Mössner J, Keim V, Löhr M, Férec C, Sahin-Tóth M |title=Variants in CPA1 are strongly associated with early onset chronic pancreatitis |journal=Nat. Genet. |volume=45 |issue=10 |pages=1216–20 |year=2013 |pmid=23955596 |pmc=3909499 |doi=10.1038/ng.2730 |url=}}</ref> | * [[Carboxypeptidase A1]] ([[Carboxypeptidase A1|CPA1]]) [[genes]]<ref name="pmid23955596">{{cite journal |vauthors=Witt H, Beer S, Rosendahl J, Chen JM, Chandak GR, Masamune A, Bence M, Szmola R, Oracz G, Macek M, Bhatia E, Steigenberger S, Lasher D, Bühler F, Delaporte C, Tebbing J, Ludwig M, Pilsak C, Saum K, Bugert P, Masson E, Paliwal S, Bhaskar S, Sobczynska-Tomaszewska A, Bak D, Balascak I, Choudhuri G, Nageshwar Reddy D, Rao GV, Thomas V, Kume K, Nakano E, Kakuta Y, Shimosegawa T, Durko L, Szabó A, Schnúr A, Hegyi P, Rakonczay Z, Pfützer R, Schneider A, Groneberg DA, Braun M, Schmidt H, Witt U, Friess H, Algül H, Landt O, Schuelke M, Krüger R, Wiedenmann B, Schmidt F, Zimmer KP, Kovacs P, Stumvoll M, Blüher M, Müller T, Janecke A, Teich N, Grützmann R, Schulz HU, Mössner J, Keim V, Löhr M, Férec C, Sahin-Tóth M |title=Variants in CPA1 are strongly associated with early onset chronic pancreatitis |journal=Nat. Genet. |volume=45 |issue=10 |pages=1216–20 |year=2013 |pmid=23955596 |pmc=3909499 |doi=10.1038/ng.2730 |url=}}</ref> | ||
==Associated Conditions== | ==Associated Conditions== | ||
* Autoimmune conditions | * [[Autoimmune]] conditions: | ||
** | ** [[Primary biliary cirrhosis]] | ||
** Primary sclerosing cholangitis | ** [[Primary sclerosing cholangitis]] | ||
** Sjögren syndrome | ** [[Sjogren syndrome|Sjögren syndrome]] | ||
* | |||
* [[Renal tubular acidosis]] | |||
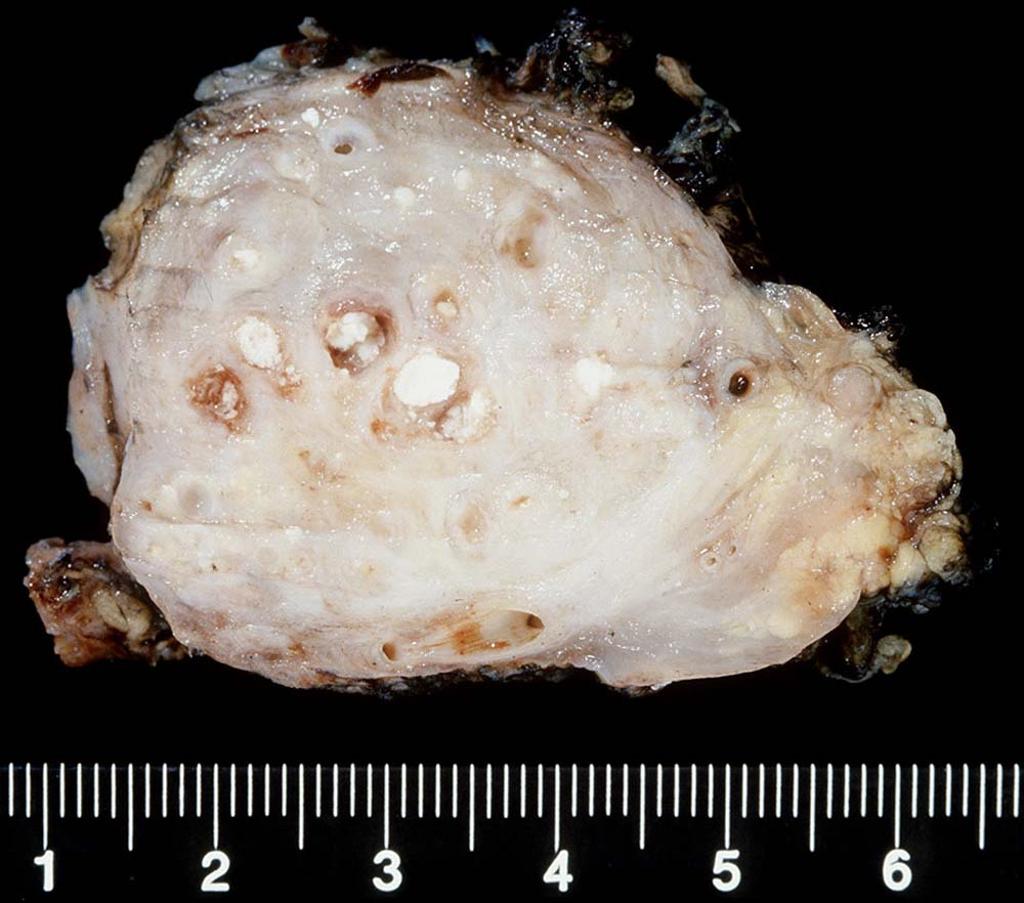
==Gross Pathology== | ==Gross Pathology== | ||
* | *On [[gross examination]], following findings may be observed: | ||
*Fibrosis | **Enlarged or [[atrophic]] [[pancreas]] | ||
* | **[[Cysts]] | ||
[[Image: Xanthogranulomatous pancreatitis.jpg| | **[[Calcification|Calcifications]] | ||
**[[Fibrosis]] | |||
**Patchy focal [[necrosis]] | |||
[[Image: Xanthogranulomatous pancreatitis.jpg|600 px|center|right|By Dr. Roshan Nasimudeen [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons]] | |||
[[Image: Chronic-pancreatitis-gross-pathology-1.jpeg|700 px|center|left|Case courtesy of Dr Henry Knipe, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/27870">rID: 27870</a>]] | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
*On microscopic histopathological analysis: | *On [[microscopic]] [[histopathological]] analysis: | ||
**Patchy focal disease characterized by a mononuclear infiltrate | **Patchy focal disease characterized by a [[Mononuclear cells|mononuclear]] infiltrate | ||
* Early phase findings: | * Early phase findings: | ||
** Increased amount of peri-ductal and inter-lobular connective tissue | ** Increased amount of peri-ductal and inter-lobular [[connective tissue]] | ||
** Minimal to moderate degree of inflammation (mostly T lymphocyte) | ** Minimal to moderate degree of [[inflammation]] (mostly [[T lymphocyte]]) | ||
** The islets of Langerhans are relatively spared | ** The [[islets of Langerhans]] are relatively spared | ||
* Late phase findings: | * Late phase findings: | ||
** Increased amount of connective tissue between the acini causing their distortion and disappearance | ** Increased amount of [[connective tissue]] between the [[acini]] causing their distortion and disappearance | ||
** Connective tissue is replaced by fibrous tissue | ** [[Connective tissue]] is replaced by [[fibrous tissue]] | ||
** Involvement of the islets of Langerhans | ** Involvement of the [[islets of Langerhans]] | ||
* [[Pancreatic]] [[lipomatosis]] may also be seen. It can be: | |||
** Even | |||
** Uneven | |||
{| class="wikitable" | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Type | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Uneven pancreatic lipomatosis | |||
|- | |||
|Type 1a | |||
|Preferential fatty replacement of head | |||
|- | |||
|Type 1b | |||
|Preferential fatty replacement of head, neck and body | |||
|- | |||
|Type 2a | |||
|Preferential fatty replacement of head and [[uncinate process]] | |||
|- | |||
|Type 2b | |||
|Fatty replacement of most of pancreas except peribiliary region | |||
|} | |||
[[Image:Tryptic fat tissue necrosis in severe pancreatitis, HE 1.jpg|500 px|thumb|center|By Patho - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=29668664]] | [[Image:Tryptic fat tissue necrosis in severe pancreatitis, HE 1.jpg|500 px|thumb|center|By Patho - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=29668664]] | ||
[[Image:Tryptic fat tissue necrosis in severe pancreatitis, HE 2.jpg|500 px|thumb|center|By Patho - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=29668789]] | [[Image:Tryptic fat tissue necrosis in severe pancreatitis, HE 2.jpg|500 px|thumb|center|By Patho - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=29668789]] | ||
=== Staging according to pancreatic physiology: === | |||
{| class="wikitable" | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Stage | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Pancreatic physiology | |||
|- | |||
|A | |||
|Normal secretory, exocrine, and endocrine function | |||
|- | |||
|B | |||
|Secretory dysfunction (abnormal secretin stimulation test) | |||
|- | |||
|C | |||
|Exocrine insufficiency (abnormal fecal elastase, steatorrhea, low serum trypsin) | |||
|- | |||
|D | |||
|Endocrine insufficiency (abnormal fasting glucose, glycohemoglobin, glucose tolerance test) | |||
|- | |||
|E | |||
|Both C & D | |||
|- | |||
|X | |||
|Not classified/ unknown | |||
|} | |||
==References== | ==References== | ||
Latest revision as of 19:44, 30 January 2018
| https://https://www.youtube.com/watch?v=met9SntRZe8%7C350}} |
|
Chronic pancreatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
American Pancreatic Association Practice Guidelines |
|
Chronic pancreatitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Chronic pancreatitis pathophysiology |
|
Risk calculators and risk factors for Chronic pancreatitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Iqra Qamar M.D.[2]
Overview
Chronic pancreatitis is a progressive inflammatory process leading to irreversible structural damage to the pancreas resulting in exocrine and endocrine dysfunction. The pathogenesis is still unclear and multifactorial. Decreased bicarbonate secretion and intrapancreatic activation of digestive enzymes is thought to play an important role in the pathogenesis of chronic pancreatitis. Other factors that are thought to play an important role in the pathogenesis of chronic pancreatitis may include intraductal plugging and obstruction, direct injury to pancreatic cells induced by toxins and toxic metabolites, antioxidants, ischemia, autoimmune disorders, the sentinal acute pancreatitis event (SAPE), necrosis and fibrosis. Genes involved in the pathogenesis of chronic pancreatitis include CFTR-cystic fibrosis gene mutation, SPINK-1 mutation, which encodes for trypsin inhibitor, PRSS-1 gene mutation linked to hereditary pancreatitis, claudin-2 (CLDN2), and carboxypeptidase A1 (CPA1) gene mutations. Associated conditions may include autoimmune conditions, primary biliary cirrhosis, primary sclerosing cholangitis, Sjögren syndrome, and renal tubular acidosis. Gross pathology may include enlarged or atrophic pancreas, cysts, calcifications, fibrosis and patchy focal necrosis. Microscopic histopathological analysis may show patchy focal disease characterized by a mononuclear infiltrate.
Pathophysiology
Chronic pancreatitis is a progressive inflammatory process leading to irreversible structural damage to the pancreas resulting in exocrine and endocrine dysfunction.[1] The pathogenesis is still unclear and multifactorial; but two mechanisms that play an important role in the pathogenesis of chronic pancreatitis, which are as follows:
Decreased bicarbonate secretion:
A decrease in bicarbonate secretion may be due to any of the following causes:
- Genetic causes leading to functional abnormalities of ductal cells
- Obstructive causes such as:
- Protein hypersecretion resulting in proteinaceous ductal plugs leading to ductal blockage and obstruction[2]
Intrapancreatic activation of digestive enzymes:
- Usually results from genetic causes leading to:
- Impaired enzyme activation and regulation
- Predisposition to injury from toxic environmental stimuli such as alcohol or cigarette smoking

Other factors that are thought to play an important role in the pathogenesis of chronic pancreatitis include:
(a) Intraductal plugging and obstruction
1) Proteinaceous ductal plugs
- Interlobular and intralobular duct blockage due to abnormal secretion of pancreatic proteins in the pancreatic juice.[2]
- GP2, a glycosyl phosphatidylinositol anchored protein is found to be a major component of plugs.[3]
- Low levels of lithostathine in alcoholics, a protective protein secreted by pancreatic acinar cells that prevent stone (calcium carbonate) formation.[4]
- These proteinaceous plugs are the major sites for calcification and stone formation leading to:
- Ductal epithelial lesions and inflammatory changes
- Scarring
- Obstruction
2) Intraductal obstruction due to other causes
- Chronic exposure to stones results in damage to ductal epithelial cells and acinar glands via:
- Ulceration
- Scarring
- Obstruction
- Biliaropancreatic tumors (pancreatic adenocarcinoma, neuroendocrine tumors, and intrapapillary mucinous tumors)
- Ethanol abuse
- Alcohol may increase the lithogenecity of pancreatic juice resulting in increased stone formation
(b) Direct injury to pancreatic cells induced by toxins and toxic metabolites
- Alcohol is proposed to have a direct toxic effect on the pancreas and damage the acinar cells via a change in intracellular metabolism (mitochondrial damage).
- It is metabolized by the pancreas and may result in oxidative stress and induce the release of pancreatic enzymes. This excessive release may result in autodigestion of the gland.
- Additionally, alcohol may result in activation of pancreatic stellate cells which are primarily responsible for fibrosis of the gland and weakening of the intracellular membranes, which results in anatomical changes in the pancreas, further predisposing to pathological autodigestion.[5][6]
- Smoking may exacerbate pancreatitis in alcoholics.
- Smoking is also found as an independent risk factor in the development and progression of pancreatitis as:
- It may affect pancreatic bicarbonate and water secretion
- It may predispose to oxidative stress
- It may also increases the rate of pancreatic calcification
(c) Antioxidants
- Steatorrhea in chronic pancreatitis may lead to nutritional deficiencies and decreased levels of antioxidants such as:[7][8]
- Selenium
- Vitamin C and E
- Methionine
- Decreased antioxidant levels may result in:[9][10][11]
- Increased free radical formation
- Lipid peroxidation
- Cellular damage
(d) Ischemia
- Ischemia is an important precipitating factor in the pathogenesis of chronic pancreatitis.
- Fibrosis and inelasticity of pancreatic tissue seen in chronic pancreatitis may lead to:
- Increased pancreatic interstitial pressure
- Increased intraductal pressure and ductal hypertension[12]
- Chronic ischemia and necrosis of pancreatic gland[13]
(e) Autoimmune disorders
- Chronic pancreatitis has been found to be associated with autoimmune conditions such as:[14][15]
- HLA-DR antigen expression with T-cell inflammatory infiltrate is seen on ductal cells in some cases of idiopathic chronic pancreatitis.[16]
(f) Necrosis and fibrosis
- Recurrent attacks of acute pancreatitis may lead to chronic pancreatitis due to:[17][18]
- Necrosis
- Fibrosis
- Scarring of pancreatic gland
- Intrinsic compression of the pancreatic ductules
- Progression from acute to chronic pancreatitis is dependent upon the number and severity of acute attacks[19]
(g) The sentinal acute pancreatitis event (SAPE) hypothesis:
- SAPE hypothesis explains the role of pancreatic stellate cells in chronic pancreatitis[17][20]
- It explains the pathogenesis of chronic pancreatitis as a continuum of 3 sequential changes:
- Pre-acute pancreatitis
- Based on the assumption that chronic pancreatitis occurs in genetically or environmentally susceptible people or who are at increased risk
- The sentinel attack of acute pancreatitis, which involves:
- Triggering of chronic inflammation in the predisposed patients
- Activation and recruitment of stellate cells
- Progression phase, with immune system activation that ultimately resulting in:
- Progression of inflammation
- Irreversible changes
- Pre-acute pancreatitis

Genetics
Genes involved in the pathogenesis of chronic pancreatitis include:
- CFTR-Cystic fibrosis gene mutation[21][22]
- SPINK-1, which encodes for trypsin inhibitor[23]
- PRSS-1 gene linked to hereditary pancreatitis
- Claudin-2 (CLDN2)[24]
- Carboxypeptidase A1 (CPA1) genes[25]
Associated Conditions
Gross Pathology
- On gross examination, following findings may be observed:
![By Dr. Roshan Nasimudeen [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons](/images/1/1f/Xanthogranulomatous_pancreatitis.jpg)
Microscopic Pathology
- On microscopic histopathological analysis:
- Patchy focal disease characterized by a mononuclear infiltrate
- Early phase findings:
- Increased amount of peri-ductal and inter-lobular connective tissue
- Minimal to moderate degree of inflammation (mostly T lymphocyte)
- The islets of Langerhans are relatively spared
- Late phase findings:
- Increased amount of connective tissue between the acini causing their distortion and disappearance
- Connective tissue is replaced by fibrous tissue
- Involvement of the islets of Langerhans
- Pancreatic lipomatosis may also be seen. It can be:
- Even
- Uneven
| Type | Uneven pancreatic lipomatosis |
|---|---|
| Type 1a | Preferential fatty replacement of head |
| Type 1b | Preferential fatty replacement of head, neck and body |
| Type 2a | Preferential fatty replacement of head and uncinate process |
| Type 2b | Fatty replacement of most of pancreas except peribiliary region |


Staging according to pancreatic physiology:
| Stage | Pancreatic physiology |
|---|---|
| A | Normal secretory, exocrine, and endocrine function |
| B | Secretory dysfunction (abnormal secretin stimulation test) |
| C | Exocrine insufficiency (abnormal fecal elastase, steatorrhea, low serum trypsin) |
| D | Endocrine insufficiency (abnormal fasting glucose, glycohemoglobin, glucose tolerance test) |
| E | Both C & D |
| X | Not classified/ unknown |
References
- ↑ Steer ML, Waxman I, Freedman S (1995). "Chronic pancreatitis". N. Engl. J. Med. 332 (22): 1482–90. doi:10.1056/NEJM199506013322206. PMID 7739686.
- ↑ 2.0 2.1 Sahel J, Sarles H (1979). "Modifications of pure human pancreatic juice induced by chronic alcohol consumption". Dig. Dis. Sci. 24 (12): 897–905. PMID 510088.
- ↑ Freedman SD, Sakamoto K, Venu RP (1993). "GP2, the homologue to the renal cast protein uromodulin, is a major component of intraductal plugs in chronic pancreatitis". J. Clin. Invest. 92 (1): 83–90. doi:10.1172/JCI116602. PMC 293537. PMID 8326020.
- ↑ Guy O, Robles-Diaz G, Adrich Z, Sahel J, Sarles H (1983). "Protein content of precipitates present in pancreatic juice of alcoholic subjects and patients with chronic calcifying pancreatitis". Gastroenterology. 84 (1): 102–7. PMID 6401181.
- ↑ Apte MV, Pirola RC, Wilson JS (2010). "Mechanisms of alcoholic pancreatitis". J Gastroenterol Hepatol. 25 (12): 1816–26. doi:10.1111/j.1440-1746.2010.06445.x. PMID 21091991.
- ↑ Forsmark CE, Vege SS, Wilcox M (November 17,2016). "Acute Pancreatitis". The New England Journal of Medicine: 1972–1981. doi:10.1056/NEJMra1505202. Retrieved November 25,2016. Check date values in:
|access-date=, |date=(help) - ↑ Rose P, Fraine E, Hunt LP, Acheson DW, Braganza JM (1986). "Dietary antioxidants and chronic pancreatitis". Hum Nutr Clin Nutr. 40 (2): 151–64. PMID 3957720.
- ↑ Uden S, Acheson DW, Reeves J, Worthington HV, Hunt LP, Brown S, Braganza JM (1988). "Antioxidants, enzyme induction, and chronic pancreatitis: a reappraisal following studies in patients on anticonvulsants". Eur J Clin Nutr. 42 (7): 561–9. PMID 3224602.
- ↑ Braganza JM, Thomas A, Robinson A (1988). "Antioxidants to treat chronic pancreatitis in childhood? Case report and possible implications for pathogenesis". Int. J. Pancreatol. 3 (2–3): 209–16. doi:10.1007/BF02798933. PMID 3361161.
- ↑ Bhardwaj P, Garg PK, Maulik SK, Saraya A, Tandon RK, Acharya SK (2009). "A randomized controlled trial of antioxidant supplementation for pain relief in patients with chronic pancreatitis". Gastroenterology. 136 (1): 149–159.e2. doi:10.1053/j.gastro.2008.09.028. PMID 18952082.
- ↑ Burton F, Alkaade S, Collins D, Muddana V, Slivka A, Brand RE, Gelrud A, Banks PA, Sherman S, Anderson MA, Romagnuolo J, Lawrence C, Baillie J, Gardner TB, Lewis MD, Amann ST, Lieb JG, O'Connell M, Kennard ED, Yadav D, Whitcomb DC, Forsmark CE (2011). "Use and perceived effectiveness of non-analgesic medical therapies for chronic pancreatitis in the United States". Aliment. Pharmacol. Ther. 33 (1): 149–59. doi:10.1111/j.1365-2036.2010.04491.x. PMC 3142582. PMID 21083584.
- ↑ Karanjia ND, Singh SM, Widdison AL, Lutrin FJ, Reber HA (1992). "Pancreatic ductal and interstitial pressures in cats with chronic pancreatitis". Dig. Dis. Sci. 37 (2): 268–73. PMID 1735346.
- ↑ Tanaka T, Ichiba Y, Miura Y, Ito H, Dohi K (1994). "Canine model of chronic pancreatitis due to chronic ischemia". Digestion. 55 (2): 86–9. PMID 7514552.
- ↑ Epstein O, Chapman RW, Lake-Bakaar G, Foo AY, Rosalki SB, Sherlock S (1982). "The pancreas in primary biliary cirrhosis and primary sclerosing cholangitis". Gastroenterology. 83 (6): 1177–82. PMID 7129026.
- ↑ Nishimori I, Yamamoto Y, Okazaki K, Morita M, Onodera M, Kino J, Tamura S, Yamamoto Y (1994). "Identification of autoantibodies to a pancreatic antigen in patients with idiopathic chronic pancreatitis and Sjögren's syndrome". Pancreas. 9 (3): 374–81. PMID 8022761.
- ↑ Bovo P, Mirakian R, Merigo F, Angelini G, Cavallini G, Rizzini P, Bottazzo GF, Scuro LA (1987). "HLA molecule expression on chronic pancreatitis specimens: is there a role for autoimmunity? A preliminary study". Pancreas. 2 (3): 350–6. PMID 3498162.
- ↑ 17.0 17.1 Schneider A, Whitcomb DC (2002). "Hereditary pancreatitis: a model for inflammatory diseases of the pancreas". Best Pract Res Clin Gastroenterol. 16 (3): 347–63. doi:10.1053/bega.2002.0311. PMID 12079262.
- ↑ Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB, Maisonneuve P (2009). "Natural history of acute pancreatitis: a long-term population-based study". Am. J. Gastroenterol. 104 (11): 2797–805, quiz 2806. doi:10.1038/ajg.2009.405. PMID 19603011.
- ↑ Ammann RW, Muellhaupt B (1994). "Progression of alcoholic acute to chronic pancreatitis". Gut. 35 (4): 552–6. PMC 1374808. PMID 8174996.
- ↑ Yadav D, Whitcomb DC (2010). "The role of alcohol and smoking in pancreatitis". Nat Rev Gastroenterol Hepatol. 7 (3): 131–45. doi:10.1038/nrgastro.2010.6. PMID 20125091.
- ↑ Bishop MD, Freedman SD, Zielenski J, Ahmed N, Dupuis A, Martin S, Ellis L, Shea J, Hopper I, Corey M, Kortan P, Haber G, Ross C, Tzountzouris J, Steele L, Ray PN, Tsui LC, Durie PR (2005). "The cystic fibrosis transmembrane conductance regulator gene and ion channel function in patients with idiopathic pancreatitis". Hum. Genet. 118 (3–4): 372–81. doi:10.1007/s00439-005-0059-z. PMID 16193325.
- ↑ Ooi CY, Gonska T, Durie PR, Freedman SD (2010). "Genetic testing in pancreatitis". Gastroenterology. 138 (7): 2202–6, 2206.e1. doi:10.1053/j.gastro.2010.04.022. PMID 20416310.
- ↑ Witt H, Luck W, Hennies HC, Classen M, Kage A, Lass U, Landt O, Becker M (2000). "Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis". Nat. Genet. 25 (2): 213–6. doi:10.1038/76088. PMID 10835640.
- ↑ Whitcomb DC, LaRusch J, Krasinskas AM, Klei L, Smith JP, Brand RE, Neoptolemos JP, Lerch MM, Tector M, Sandhu BS, Guda NM, Orlichenko L, Alkaade S, Amann ST, Anderson MA, Baillie J, Banks PA, Conwell D, Coté GA, Cotton PB, DiSario J, Farrer LA, Forsmark CE, Johnstone M, Gardner TB, Gelrud A, Greenhalf W, Haines JL, Hartman DJ, Hawes RA, Lawrence C, Lewis M, Mayerle J, Mayeux R, Melhem NM, Money ME, Muniraj T, Papachristou GI, Pericak-Vance MA, Romagnuolo J, Schellenberg GD, Sherman S, Simon P, Singh VP, Slivka A, Stolz D, Sutton R, Weiss FU, Wilcox CM, Zarnescu NO, Wisniewski SR, O'Connell MR, Kienholz ML, Roeder K, Barmada MM, Yadav D, Devlin B (2012). "Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis". Nat. Genet. 44 (12): 1349–54. doi:10.1038/ng.2466. PMC 3510344. PMID 23143602.
- ↑ Witt H, Beer S, Rosendahl J, Chen JM, Chandak GR, Masamune A, Bence M, Szmola R, Oracz G, Macek M, Bhatia E, Steigenberger S, Lasher D, Bühler F, Delaporte C, Tebbing J, Ludwig M, Pilsak C, Saum K, Bugert P, Masson E, Paliwal S, Bhaskar S, Sobczynska-Tomaszewska A, Bak D, Balascak I, Choudhuri G, Nageshwar Reddy D, Rao GV, Thomas V, Kume K, Nakano E, Kakuta Y, Shimosegawa T, Durko L, Szabó A, Schnúr A, Hegyi P, Rakonczay Z, Pfützer R, Schneider A, Groneberg DA, Braun M, Schmidt H, Witt U, Friess H, Algül H, Landt O, Schuelke M, Krüger R, Wiedenmann B, Schmidt F, Zimmer KP, Kovacs P, Stumvoll M, Blüher M, Müller T, Janecke A, Teich N, Grützmann R, Schulz HU, Mössner J, Keim V, Löhr M, Férec C, Sahin-Tóth M (2013). "Variants in CPA1 are strongly associated with early onset chronic pancreatitis". Nat. Genet. 45 (10): 1216–20. doi:10.1038/ng.2730. PMC 3909499. PMID 23955596.