Cholangitis: Difference between revisions
| Line 46: | Line 46: | ||
== Diagnosis == | == Diagnosis == | ||
=== Other Imaging Findings === | === Other Imaging Findings === | ||
Revision as of 16:19, 27 January 2012
| Cholangitis | |
 | |
|---|---|
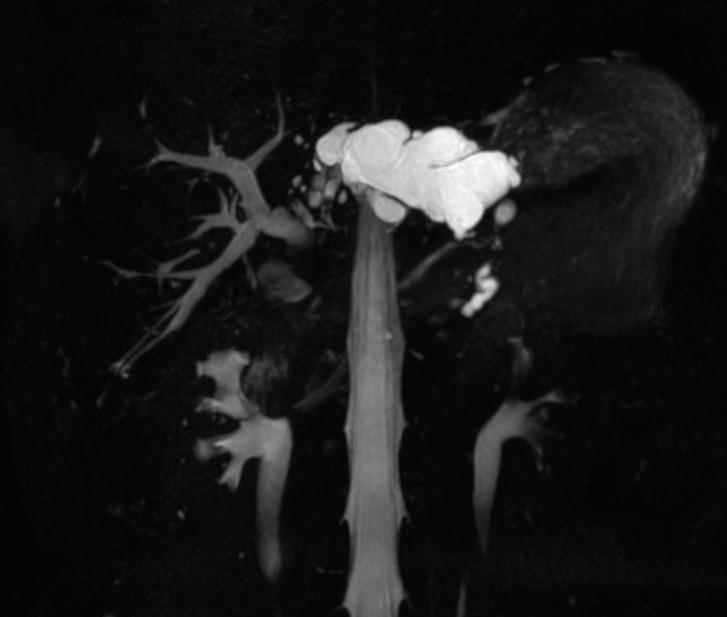
| Recurrent pyogenic cholangitis. (Image courtesy of RadsWiki) | |
| ICD-10 | K83.0 |
| ICD-9 | 576.1 |
| DiseasesDB | 2514 |
| eMedicine | med/2665 emerg/96 |
| MeSH | D002761 |
|
Cholangitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cholangitis On the Web |
|
American Roentgen Ray Society Images of Cholangitis |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Historical Perspective
Pathophysiology
Epidemiology & Demographics
Risk Factors
Screening
Causes
Differentiating Cholangitis
Complications & Prognosis
Diagnosis
History and Symptoms | Physical Examination | Staging | Laboratory tests | Electrocardiogram | X Rays | CT | MRI Echocardiography or Ultrasound | Other images | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Primary prevention | Secondary prevention | Financial costs | Future therapies
Diagnosis
Other Imaging Findings
- Ultrasound: Diagnostic evaluation should proceed first with ultrasound which has an 55-85% sensitivity. Small stones in the common bile duct may be missed. The CBD may not be enlarged early or if the stones has passed. The ducts may be totally normal in PSC.
Treatment
80% of patients with acute cholangitis will respond to conservative therapy and elective drainage. In 15-20%, the cholangitis will progress requiring emergent drainage. Markers for these people are persistent abdominal pain, hypotensive, fever >102, and confusion.
Patients should be kept NPO, given IVF, broad spectrum ABX, Vitamin K and be drained. Choices for drainage are ERCP with stone removal and sphincterotomy/stent placement, surgically drainage or percutaneous drainage. Intrahepatic stones cannot be removed via ERCP and should be drained percutaneously. Randomized trials comparing ERCP and surgery showed morbidity and mortality benefit for ERCP (4.7-10% versus 10-50%). A nasobiliary catheter can be placed if ERCP is impossible (<5%) either because of coagulopathy precluding sphincterotomy, too large a stone (>2cm) etc. Next step should be percutaneous drainage as a bridge to elective surgery since emergent surgery has an up to 40% mortality.