Cholangitis: Difference between revisions
No edit summary |
m (Robot: Changing Category:DiseaseState to Category:Disease) |
||
| Line 84: | Line 84: | ||
{{SIB}} | {{SIB}} | ||
{{Gastroenterology}} | {{Gastroenterology}} | ||
---- | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category: | [[Category:Disease]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
Revision as of 17:42, 12 December 2011
| Cholangitis | |
 | |
|---|---|
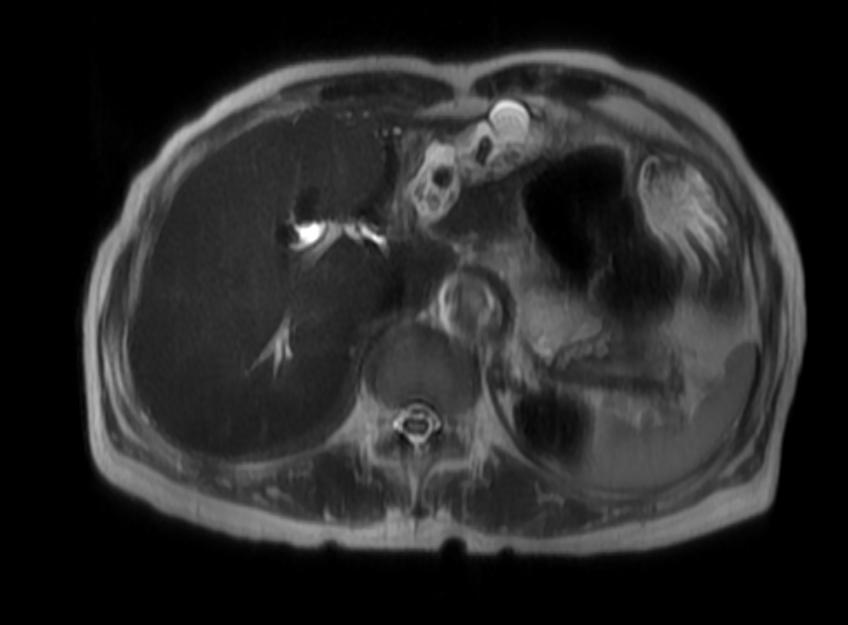
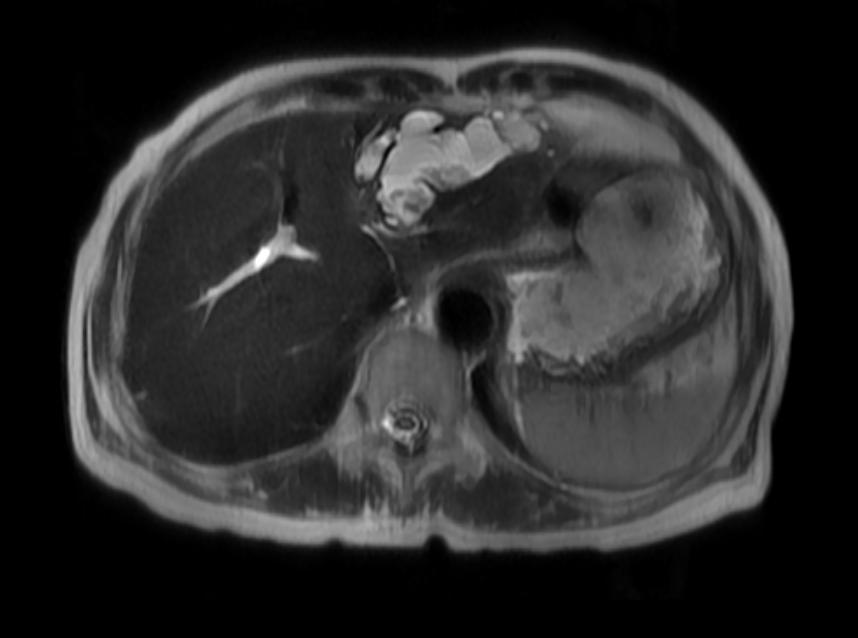
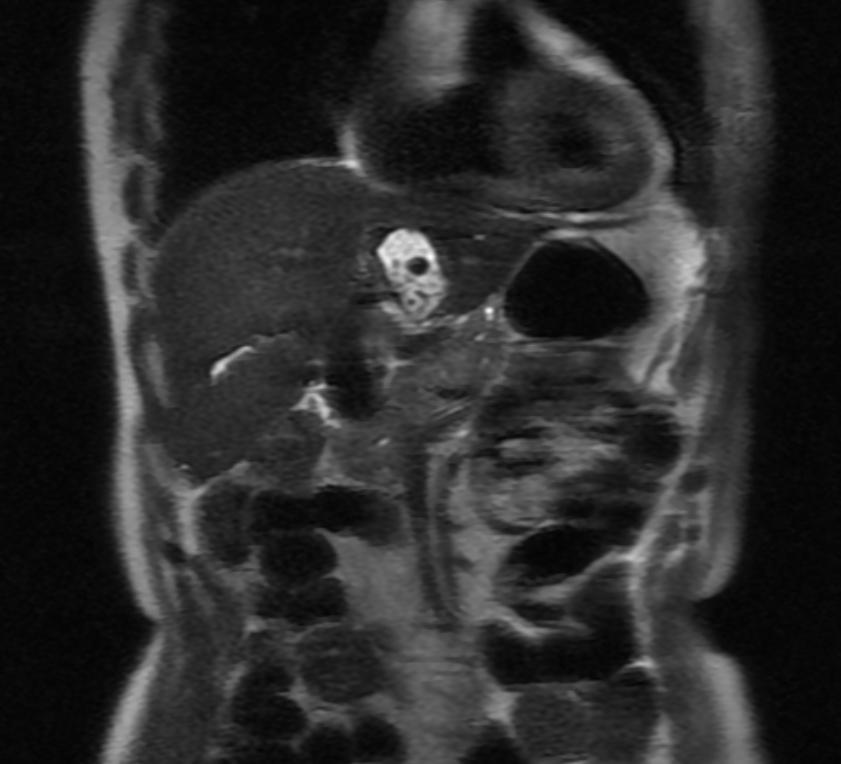
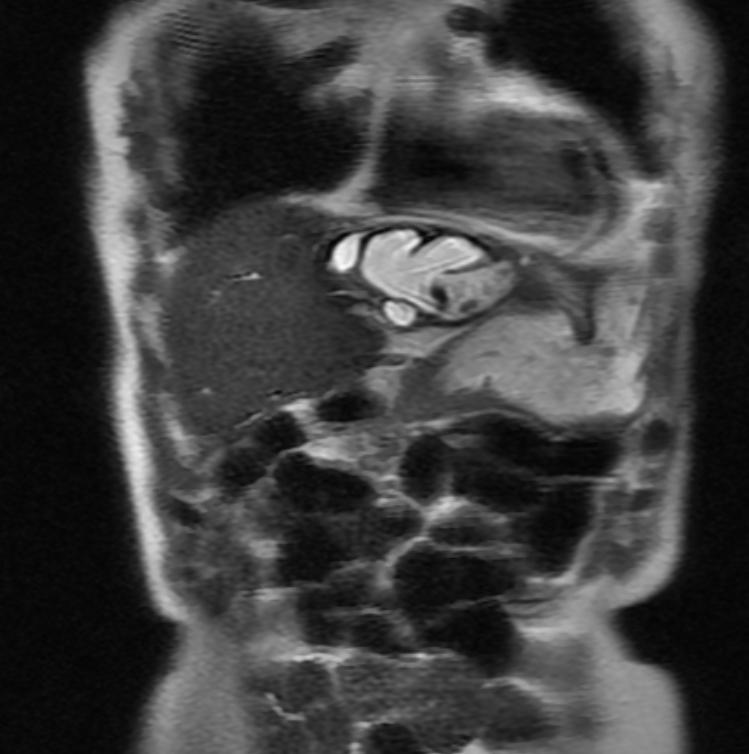
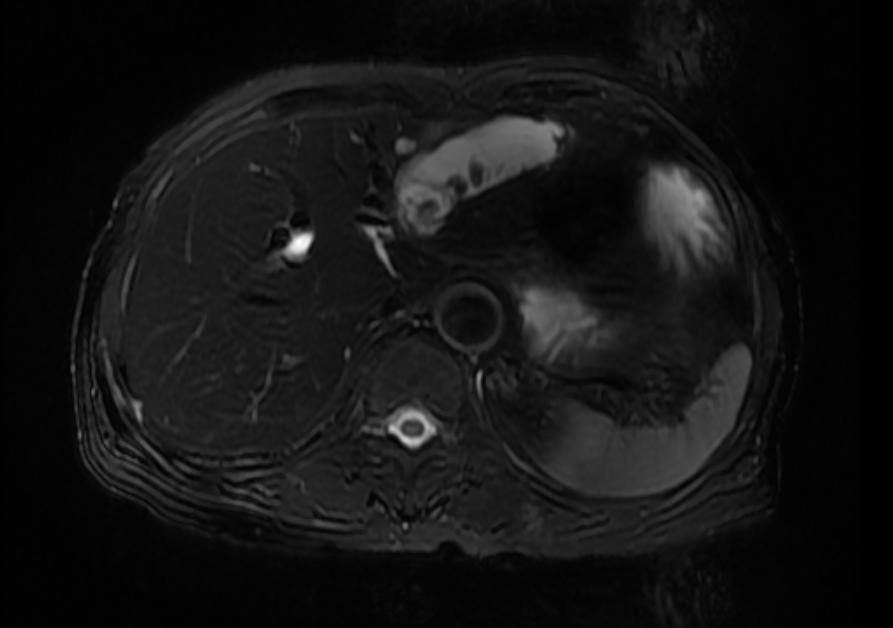
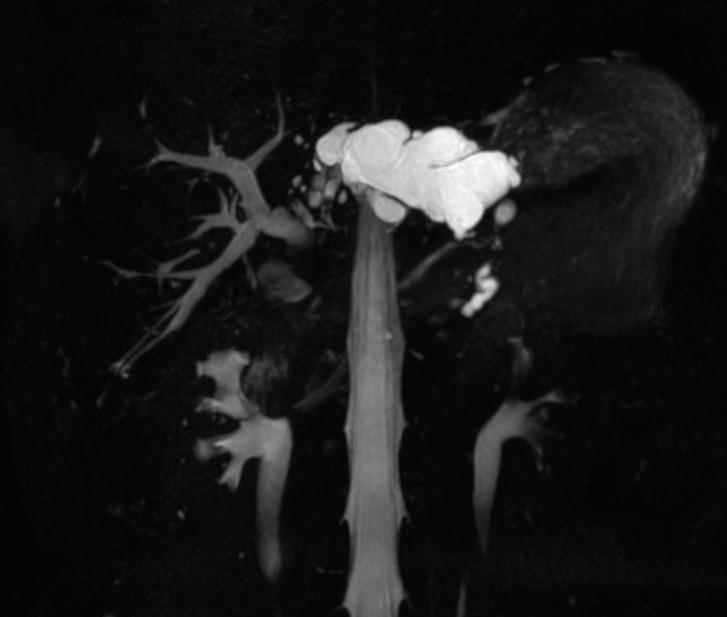
| Recurrent pyogenic cholangitis. (Image courtesy of RadsWiki) | |
| ICD-10 | K83.0 |
| ICD-9 | 576.1 |
| DiseasesDB | 2514 |
| eMedicine | med/2665 emerg/96 |
| MeSH | D002761 |
|
WikiDoc Resources for Cholangitis |
|
Articles |
|---|
|
Most recent articles on Cholangitis Most cited articles on Cholangitis |
|
Media |
|
Powerpoint slides on Cholangitis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cholangitis at Clinical Trials.gov Clinical Trials on Cholangitis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cholangitis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cholangitis Discussion groups on Cholangitis Patient Handouts on Cholangitis Directions to Hospitals Treating Cholangitis Risk calculators and risk factors for Cholangitis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cholangitis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Cholangitis is a clinically defined syndrome of fever, right upper quadrant pain and jaundice caused by infection of bile and inflammation of the biliary tree, usually due to obstruction and stasis. Cholangitis was first described as a life-threatening disorder in 1877 by Charcot. In 1955, Reynolds and Dargan recognized that septic shock and mental status changes portended a poor outcome. (Reynolds’s Pentad). [1] [2] [3] [4]
Epidemiology and Demographics
Parasites are commonly associated with cholangitis outside of the United States. Parasites associated with cholangitis include the Ascaris, Opisthorchis, Clonorchis, Fasciola and Echinococcus. Ascaris is thought to be the etiologic agent of recurrent pyogenic cholangitis (Oriental cholangiohepatitis) found in Hong Kong, Southeast Asia, Columbia, Italy and South Africa. As they migrate to the biliary tree, they bring gut flora with them predisposing to bacterial infection. Dying worms lead to inflammation, granulomatous scarring and fibrosis which may lead to biliary cirrhosis. Opisthorchis and Clonorchis are transmitted by raw fish in Asia, Europe and Siberia and “frequently” lead to the development of cholangiocarcinoma. Fascioloa is transmitted by colonized watercress and does not predispose to cholangiocarcinoma.
Pathophysiology
The presence of gallstones alone predisposes to bacterial colonization. 70% of patients with gallstones will have bacteria in the bile while normal bile is usually sterile. CBD have a higher probability of infection. 80% of stones can be culture positive.
The source of biliary infection is usually ascending from the duodenum or jejunum and less commonly direct hematogenous seeding of the portal system. In the presence of obstruction, the small bowel becomes colonized with colonic flora. The common organisms are E.coli, Klebsiella, Enterococcus, Enterobacter, Proteus. Anaerobes (Strep, Bacteroides, Clostridia) can be found particularly in the elderly. Higher incidence of Pseudomonas in those who have been instrumented. Broad spectrum antibiotics to cover Gram negatives including Pseudomonas, Enterococcus and anaerobes are needed up front. Cephalosporins should not be used as monotherapy. Cipro has been shown in one study to be as effective as monotherapy despite poor coverage for anaerobes and EC.
The most common causes of biliary obstruction are biliary calculi, benign stricture or malignant neoplasms. Benign strictures are caused by primary sclerosing cholangitis, ischemic cholangitis, iatrogenic biliary tract injury, congenital disease and infection. Chronic inflammation predisposed to the development of cholangiocarcinoma. Extraluminal obstruction can occur from pancreatic cancer or pseudocyst, lymphoma, hepatoma, metastatic disease or ampullary cancer.
Biliary obstruction leads to elevated biliary pressures, favoring migration of bacteria into the portal circulation and bile. As pressures increase hepatocyte secretion is impaired and bacteria move into the lymphatics and systemic circulation.
Diagnosis
50-60% of patients will have all three of Charcot’s triad. 95% will have fever, 66% abdominal pain, jaundice is noted in 80% (When bilirubin >2.5). Nonobstructive stones are more likely to present without pain or fever. Elderly patients may present only with hypotension. Dark urine is noted and acholia can be seen.
The combination of hyperbilirubinemia, elevated white blood cell (WBC) count with bandemia, aspartate aminotransferase (AST), alanine aminotransferase (ALT) and alkaline phosphatase elevations all suggest the diagnosis. Alkaline phosphatase and bilirubin are significantly higher inpatients with malignant rather than benign obstruction. In benign obstruction, the bilirubin rarely exceeds 12. Gamma-glutamyltransferase (GGT) and 5’-nucleotidase confirm a biliary origin of the alkaline phosphatase. The prothrombin time is often elevated. AST and ALT may be as high as 1000, especially if microabcesses form.
MRI and CT
CT has a higher sensitivity (63%) and is better to localize the site of obstruction.
MRI
-
Recurrent pyogenic cholangitis
-
Recurrent pyogenic cholangitis
-
Recurrent pyogenic cholangitis
-
Recurrent pyogenic cholangitis
-
Recurrent pyogenic cholangitis
-
Recurrent pyogenic cholangitis
Other Imaging Findings
- Ultrasound: Diagnostic evaluation should proceed first with ultrasound which has an 55-85% sensitivity. Small stones in the common bile duct may be missed. The CBD may not be enlarged early or if the stones has passed. The ducts may be totally normal in PSC.
Treatment
80% of patients with acute cholangitis will respond to conservative therapy and elective drainage. In 15-20%, the cholangitis will progress requiring emergent drainage. Markers for these people are persistent abdominal pain, hypotensive, fever >102, and confusion.
Patients should be kept NPO, given IVF, broad spectrum ABX, Vitamin K and be drained. Choices for drainage are ERCP with stone removal and sphincterotomy/stent placement, surgically drainage or percutaneous drainage. Intrahepatic stones cannot be removed via ERCP and should be drained percutaneously. Randomized trials comparing ERCP and surgery showed morbidity and mortality benefit for ERCP (4.7-10% versus 10-50%). A nasobiliary catheter can be placed if ERCP is impossible (<5%) either because of coagulopathy precluding sphincterotomy, too large a stone (>2cm) etc. Next step should be percutaneous drainage as a bridge to elective surgery since emergent surgery has an up to 40% mortality.
References
- ↑ Kadakia S. Biliary Tract Emergencies. Med Clin North Amer. 1993, 77(5) 1015-1036. PMID 8371614
- ↑ Carpenter H. Bacterial and Parasitic Cholangitis. May Clin Proc. 1998, 73:473-478. PMID 9581592
- ↑ Leese T, Neoptolemos JP, Baker AR. Management of acute cholangitis and the impact of endoscopic sphincterotomy. Br J Surg. 1986, 73:988. PMID 3790964
- ↑ Lai ECS, Mok FPT, Tan ESY. Endoscopic biliary drainage for severe acute cholangitis. NEJM 1992, 326:1582-6. PMID 1584258
Template:SIB
Template:Gastroenterology