Cardiomyopathy: Difference between revisions
Lina Yaqoub (talk | contribs) |
No edit summary |
||
| Line 27: | Line 27: | ||
[[Cardiomyopathy medical therapy|Medical Therapy]] | [[Cardiomyopathy surgery|Surgery]] | [[Cardiomyopathy primary prevention|Primary Prevention]] | [[Cardiomyopathy secondary prevention|Secondary Prevention]] | [[Cardiomyopathy cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Cardiomyopathy future or investigational therapies|Future or Investigational Therapies]] | [[Cardiomyopathy medical therapy|Medical Therapy]] | [[Cardiomyopathy surgery|Surgery]] | [[Cardiomyopathy primary prevention|Primary Prevention]] | [[Cardiomyopathy secondary prevention|Secondary Prevention]] | [[Cardiomyopathy cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Cardiomyopathy future or investigational therapies|Future or Investigational Therapies]] | ||
== Case Studies == | == Case Studies == | ||
Revision as of 18:43, 15 April 2019
For patient information click here
| Cardiomyopathy | |
 | |
|---|---|
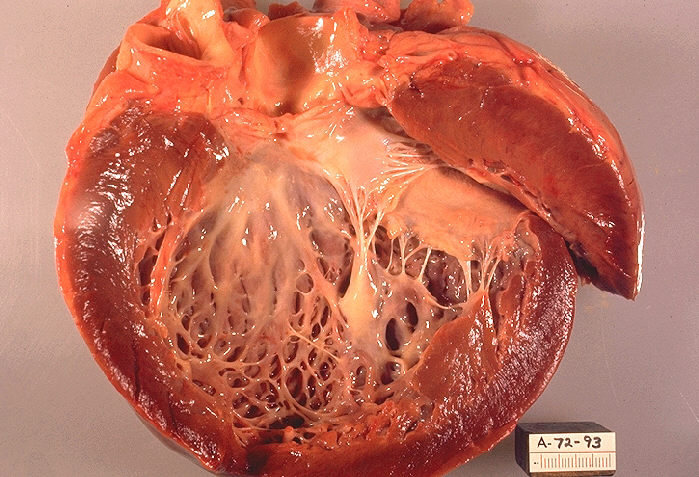
| Opened left ventricle of heart shows a thickened, dilated left ventricle with subendocardial fibrosis manifested as increased whiteness of endocardium {Autopsy findings}. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
|
Cardiomyopathy Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Guidelines |
|
2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy |
|
Case Studies |
|
Cardiomyopathy On the Web |
|
American Roentgen Ray Society Images of Cardiomyopathy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2], Raviteja Guddeti, M.B.B.S. [3]
Synonyms and keywords: Myocardiopathy; cardiac muscle disease; heart muscle disease.
Overview
Historical Perspective
Epidemiology and Demographics
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory Findings | Electrocardiogram | Chest X Ray | CT | MRI | Echocardiography | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies
de:Kardiomyopathie nl:Cardiomyopathie no:Kardiomyopati simple:Cardiomyopathy sr:Кардиомиопатија sv:Hjärtmuskelsjukdom