Aortic stenosis echocardiography
|
Aortic Stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Percutaneous Aortic Balloon Valvotomy (PABV) or Aortic Valvuloplasty |
|
Transcatheter Aortic Valve Replacement (TAVR) |
|
Case Studies |
|
Aortic stenosis echocardiography On the Web |
|
American Roentgen Ray Society Images of Aortic stenosis echocardiography |
|
Directions to Hospitals Treating Aortic stenosis echocardiography |
|
Risk calculators and risk factors for Aortic stenosis echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Mohammed A. Sbeih, M.D. [2]; Lakshmi Gopalakrishnan, M.B.B.S. [3]
Overview
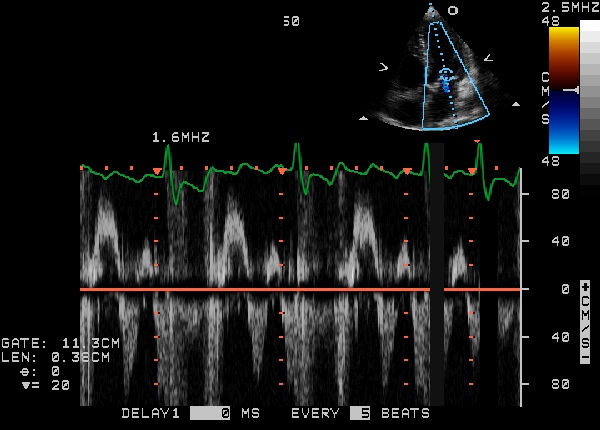
Echocardiography is the best non-invasive test to evaluate the aortic valve anatomy and function. Echocardiography can be used to estimate the gradient across the aortic valve using the modified Bernoulli equation (gradient = 4 X velocity2). The flow must be constant, so as the velocity increases, the valve area decreases proportionally. Echocardiography can also be used to assess the severity of left ventricular hypertrophy.
Optimal Echocardiography Views
Parasternal Long Axis View
The parasternal long axis view visualizes the right and non coronary leaflets.
Parasternal Short Axis View
In the parasternal short axis view, the aortic leaflets open equally and form a circular orifice during systole. During diastole, the normal leaflets form a three pointed star with prominence at the closing point (nodules of Arentius).
Severity of Aortic Stenosis
Aortic stenosis severity can be assessed by estimating both the pressure gradient across the valve and the aortic valve area.
- Using echocardiographic flow velocities, the aortic valve area can be calculated non-invasively to estimate the severity of aortic stenosis.
- Using the velocity of the blood through the valve, the pressure gradient across the valve can be calculated by the equation:
Gradient = 4(velocity)² mmHg
Normal Aortic Valve:
- A normal aortic valve has no gradient, and
- Aortic valve surface area is of 2.5 to 3.5 cms2.
Mild Aortic Stenosis:
- Mean pressure gradient across the valve is less than 25 mm Hg, or
- Valve surface area is between 1.5 and 2.5 cms2, or
- Jet velocity less than 3.0 m per second
Moderate Aortic Stenosis:
- Mean pressure gradient across the valve is between 25 mm Hg and 40 mm Hg, or
- Valve surface area is between 1.0 and 1.5 cms2, or
- Jet velocity 3.0 to 4.0 m per second
Moderate to Severe Aortic Stenosis
- Valve surface area is between 0.7 and 1.0 cms2
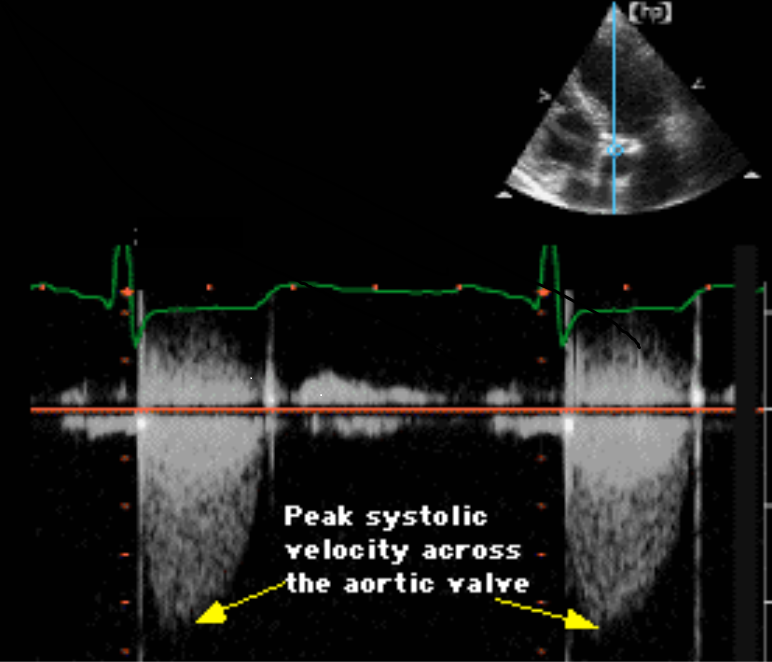
Severe Aortic Stenosis:
- Mean pressure gradient across the valve is more than 40 mm Hg, or
- Valve surface area is less than 0.7 cm2, or
- Jet velocity is greater than 4.0 m per second
| Severity | mild | moderate | severe |
|---|---|---|---|
| Valve Surface Area | 2.5 - 1.5 | 1.5 - 1.0 | <1.0 |
| Jet Velocity (m/s) | 2 - 3 | 3 - 4 | >4 |
| Peak Gradient (mmHg) | <25 | 25 - 40 | >40 |
| Mean Gradient (mmHg) | <20 | 20-40 | >40 |
Examples
Demonstration of Diastolic Mitral Regurgitation due to Severe Aortic Stenosis
Demonstration of Aortic regurgitation combined with Aortic Stenosis
{{#ev:youtube|J-Qs_evodww}}
Demonstration of Calcific Aortic Stenosis with Mitral Annular Calcification and Moderate Mitral Regurgitation
{{#ev:youtube|qjpV19034sk}}
Low flow Aortic Stenosis
{{#ev:youtube|WC3uKS4ShSM&feature=related}}
Severe Aortic Stenosis without Aortic Regurgitation
Cntinuous wave doppler below shows a peak velocity across the aortic valve of a gradient of 85 mmHg, which is compatible with severe aortic stenosis. No aortic regurgitation is present.
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [1]
Echocardiography (DO NOT EDIT) [1]
| Class I |
| "1. Echocardiography is recommended for the diagnosis and assessment of aortic stenosis severity.(Level of Evidence: B) " |
| "2. Echocardiography is recommended in patients with aortic stenosis for the assessment of left ventricular wall thickness, size, and function.(Level of Evidence: B) " |
| "3. Echocardiography is recommended for re-evaluation of patients with known aortic stenosis and changing symptoms or signs.(Level of Evidence: B) " |
| "4. Echocardiography is recommended for the assessment of changes in hemodynamic severity and left ventricular function in patients with known aortic stenosis during pregnancy. (Level of Evidence: B) " |
| "5. Transthoracic echocardiography is recommended for re-evaluation of asymptomatic patients: every year for severe aortic stenosis; every 1 to 2 years for moderate aortic stenosis; and every 3 to 5 years for mild aortic stenosis.(Level of Evidence: B) " |
| Class IIa |
|
"1. Dobutamine stress echocardiography is reasonable to evaluate patients with low-flow/low-gradient AS and LV dysfunction. (Level of Evidence: B)" |
Asymptomatic Adolescents (DO NOT EDIT) [1]
| Class I |
| "1. Doppler echocardiography is recommended yearly in the asymptomatic adolescent or young adult with AS who has a Doppler mean gradient greater than 30 mm Hg or a peak velocity greater than 3.5 m per second (peak gradient greater than 50 mm Hg) and every 2 years if the Doppler gradient is less than or equal to 30 mm Hg or the peak jet velocity is less than or equal to 3.5 m per second (peak gradient less than or equal to 50 mm Hg).(Level of Evidence: C) " |
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [1]
References
- ↑ 1.0 1.1 1.2 1.3 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help)
- Pages with citations using unsupported parameters
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- Disease
- Signs and symptoms
- Physical Examination
- Valvular heart disease
- Cardiology
- Congenital heart disease
- Mature chapter
- Cardiac surgery
- Surgery
- Overview complete
- For review
- Template complete