Aortic stenosis cardiac catheterization
|
Aortic Stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Percutaneous Aortic Balloon Valvotomy (PABV) or Aortic Valvuloplasty |
|
Transcatheter Aortic Valve Replacement (TAVR) |
|
Case Studies |
|
Aortic stenosis cardiac catheterization On the Web |
|
American Roentgen Ray Society Images of Aortic stenosis cardiac catheterization |
|
Directions to Hospitals Treating Aortic stenosis cardiac catheterization |
|
Risk calculators and risk factors for Aortic stenosis cardiac catheterization |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Mohammed A. Sbeih, M.D. [2]; Assistant Editor-In-Chief: Kristin Feeney, B.S. [3]
Overview
Left and right heart catheterization as well as angiography may be useful in the assessment of the patient prior to aortic valve replacement surgery.
Cardiac Catheterization
Assessment of the Gradient Across the Aortic Valve
- Left heart catheterization is performed to simultaneously assess left ventricular and aortic pressures. A catheter is placed inside the left ventricle, and pressure is simultaneously recorded in the femoral artery. The difference in pressures is the pressure gradient across the aortic valve.
- The femoral pressure is usually measured off of the sidearm of the femoral sheath. The sheath size of the femoral sheath should be at least on French size larger than the catheter so that the catheter does not induce dampening of the pressure waveform in the femoral sheath.
- It is assumed that the femoral blood pressure is equal to the blood pressure in the aorta just distal to the aortic valve. This assumption is often wrong. Prior to crossing the aortic valve, the blood pressure should be compared in the proximal aorta and the femoral sheath. As a result of the reflection of the waveforms in stiff atherosclerotic blood vessel, there may be a higher pressure in the femoral sheath. This is termed femoral augmentation. The augmentation of the femoral blood pressure must be subtracted from the peak gradient in calculating the aortic valve area. On the other hand, the pressure in the femoral artery may be lower than that of the central aorta due to peripheral arterial disease. In this scenario, the femoral pressure must be upwardly adjusted to account for this.
Crossing the Stenosed Aortic Valve
- In patients with moderate to severe aortic stenosis, the pigtail catheter will generally not cross the aortic valve in the traditional fashion.
- A straight tipped wire is placed in the catheter.
- In the 30 degree left anterior oblique projection, the wire is then extruded from the pigtail catheter.
- Multiple attempts are made to advance the straight tipped wire across the aortic valve.
- The odds of crossing the valve are improved if you can identify the central jet of blood coming out of the aortic valve. This can be identified by the wire vibrating or shuddering when it is in the jet. The wire should then be advanced in the central region of shuddering or rapid aortic velocity.
- Should the pigtail catheter not provide the appropriate angulation, it can be replaced with a Judkins right 4 catheter (JR4). If this catheter does not work, it can be replaced with an Amplatz right 1 or 2 catheter (AR1 or AR2).
- Care must be taken to heparinize the patient so that a clot does not form on the wire. Alternatively, the wire must be periodically removed and cleared of any clot.
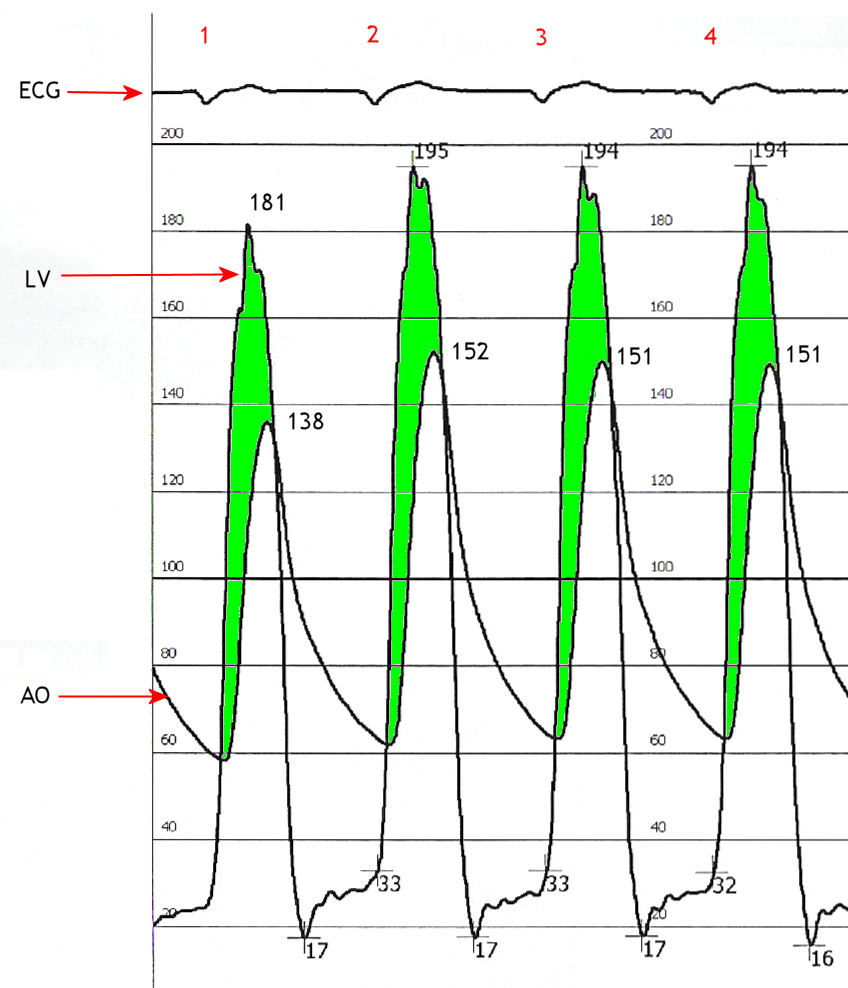 Simultaneous left ventricular and aortic pressure tracings demonstrate a pressure gradient between the left ventricle and aorta, suggesting aortic stenosis. The left ventricle generates higher pressures than what is transmitted to the aorta. The pressure gradient, caused by aortic stenosis, is represented by the green shaded area. (AO = ascending aorta; LV = left ventricle; ECG = electrocardiogram.) The heart may be catheterized to directly measure the pressure on both sides of the aortic valve.
Simultaneous left ventricular and aortic pressure tracings demonstrate a pressure gradient between the left ventricle and aorta, suggesting aortic stenosis. The left ventricle generates higher pressures than what is transmitted to the aorta. The pressure gradient, caused by aortic stenosis, is represented by the green shaded area. (AO = ascending aorta; LV = left ventricle; ECG = electrocardiogram.) The heart may be catheterized to directly measure the pressure on both sides of the aortic valve.
Coronary Angiography
Coronary angiography is performed in elderly patients who are undergoing aortic vavle replacement to ascertain whether obstructive epicardial coronary artery disease is present that would warrant coronary artery bypass graft surgery.
ACC/AHA 2008 Guidelines for the Management of Patients with Valvular Heart Disease - Indications for Cardiac Catheterization (DO NOT EDIT) [1]
| Class I |
| "1.Coronary angiography is recommended before AVR in patients with AS at risk for CAD.(Level of Evidence: B) " |
| "2.Cardiac catheterization for hemodynamic measurements is recommended for assessment of severity of AS in symptomatic patients when noninvasive tests are inconclusive or when there is a discrepancy between noninvasive tests and clinical findings regarding severity of AS. (Level of Evidence: C) " |
| "3.Coronary angiography is recommended before AVR in patients with AS for whom a pulmonary autograft (Ross procedure) is contemplated and if the origin of the coronary arteries was not identified by noninvasive technique.(Level of Evidence: C) " |
| Class III |
| "1.Cardiac catheterization for hemodynamic measurements is not recommended for the assessment of severity of AS before AVR when noninvasive tests are adequate and concordant with clinical findings.(Level of Evidence: C) " |
| "2.Cardiac catheterization for hemodynamic measurements is not recommended for the assessment of LV function and severity of AS in asymptomatic patients. (Level of Evidence: C) " |
| Class IIa |
|
"1. Cardiac catheterization for hemodynamic measurements with infusion of dobutamine can be useful for evaluation of patients with low-flow/low-gradient AS and LV dysfunction. (Level: C)" |
References
- ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.