Alzheimer's disease: Difference between revisions
(Streamlining of pathophysiology section, removing repetition.) |
(Rearranged sections: moved history and epidemiology closer to beginning.) |
||
| Line 176: | Line 176: | ||
}}</ref> | }}</ref> | ||
== | ==History== | ||
[[Image:Auguste D aus Marktbreit.jpg|220px|thumb|[[Auguste D]], first described patient with AD]] | |||
Although the concept of [[dementia]] goes as far back as the ancient Greek and Roman philosophers and [[physician]]s,<ref name="pmid9661992">{{cite journal | |||
|author=Berchtold NC, Cotman CW | |||
|title=Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s | |||
|journal=Neurobiology of Aging | |||
|volume=19 | |||
|issue=3 | |||
|pages=173–189 | |||
|year=1998 | |||
|pmid=9661992 | |||
|doi=10.1016/S0197-4580(98)00052-9 | |||
}}</ref> it was in 1901 when Alöis Alzheimer, a German [[psychiatry|psychiatrist]], identified the first case of what became known as Alzheimer's disease in a fifty-year-old woman he called [[Auguste D]]. Alöis Alzheimer followed her until she died in 1906, when he first reported the case publicly.<ref>Auguste D.: | |||
* {{ | |||
cite journal | |||
| author=Alzheimer Alöis | |||
| title=Uber eine eigenartige Erkrankung der Hirnrinde | |||
| journal= | |||
| volume=64 | |||
| issue=1–2 | |||
| pages=146–148 | |||
| year=1907 | |||
| language={{de icon}} | |||
}} | |||
*{{cite journal | *{{cite journal | ||
|author= | |author=Alöis Alzheimer | ||
|title= | |origdate=1907 | ||
|journal= | |title=About a peculiar disease of the cerebral cortex. (Translated by L. Jarvik and H. Greenson) | ||
|volume= | |journal=Alzheimer Disease and Associated Disorders | ||
|issue= | |volume=1 | ||
|pages= | |issue=1 | ||
|year= | |pages=3–8 | ||
| | |year=1987 | ||
| | |pmid=3331112 | ||
| | |doi= | ||
|issn= | |||
}} | }} | ||
*{{cite | *{{cite book | ||
|author= | |author=Maurer Ulrike, Maurer Konrad | ||
|title= | |title=Alzheimer: the life of a physician and the career of a disease | ||
| | |publisher=Columbia University Press | ||
| | |location=New York | ||
| | |year=2003 | ||
|pages= | |pages=270 | ||
| | |isbn=0-231-11896-1 | ||
| | |oclc= | ||
| | |doi= | ||
}} | }} | ||
*{{cite | *{{cite book | ||
|author= | |author=Hochberg Fred H., Rottenberg David | ||
|title= | |title=Neurological classics in modern translation | ||
| | |publisher=Hafner Press | ||
| | |location=New York | ||
| | |year=1977 | ||
|pages= | |pages=<!-- needed --> | ||
|isbn=0-02-851180-8 | |||
| | |oclc= | ||
| | |doi= | ||
}}</ref> In the following five years, eleven similar cases were reported in the [[medical literature]], some of them already using the term Alzheimer's disease.<ref name="pmid9661992">{{cite journal | |||
|doi= | |author=Berchtold NC, Cotman CW | ||
}}</ref> | |title=Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s | ||
|author= | |journal=Neurobiology of Aging | ||
|title= | |volume=19 | ||
|journal= | |||
|volume= | |||
|issue=3 | |issue=3 | ||
|pages= | |pages=173–189 | ||
|year= | |year=1998 | ||
|pmid= | |pmid=9661992 | ||
|doi=10. | |doi=10.1016/S0197-4580(98)00052-9 | ||
}}</ref> The | }}</ref> The official consideration of the disease as a distinctive entity is attributed to [[Emil Kraepelin]], who included ''Alzheimer’s disease'' or ''presenile'' [[dementia]] as a subtype of ''senile dementia'' in the eighth edition of his ''Textbook of Psychiatry'', published in 1910.<ref name="isbn1-4325-0833-4">{{cite book | ||
|author=Kraepelin Emil, Diefendorf A. Ross (translated by) | |||
|title=Clinical Psychiatry: A Textbook For Students And Physicians (Reprint) | |||
|publisher=Kessinger Publishing | |||
|location= | |||
|date=2007-01-17 | |||
|pages=568 | |||
|isbn=1-4325-0833-4 | |||
|oclc= | |||
|doi= | |||
}}</ref> | |||
|author= | |||
|title= | For most of the twentieth century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45 and 65 who developed symptoms of dementia. The terminology changed after 1977 when a conference concluded that the clinical and [[pathological]] manifestations of presenile and senile dementia were almost identical, although the authors also added that this did not rule out the possibility of different [[etiology|etiologies]]. This eventually led to the use of ''Alzheimer's disease'' independently of onset age of the disease.<ref name="pmid9702682">{{cite journal | ||
| | |author=Boller F, Forbes MM | ||
| | |title=History of dementia and dementia in history: an overview | ||
| | |journal=Journal of Neurological Science | ||
|pages= | |volume=158 | ||
| | |issue=2 | ||
| | |pages=125–133 | ||
|doi= | |year=1998 | ||
|pmid=9702682 | |||
|doi=10.1016/S0022-510X(98)00128-2 }}</ref><ref name="isbn0-89004-225-X">{{cite book | |||
}}</ref> | |author=Katzman Robert, Terry Robert D, Bick Katherine L (editors) | ||
{{cite journal | |title=Alzheimer's disease: senile dementia and related disorders | ||
|author= | |publisher=Raven Press | ||
|title= | |location=New York | ||
|journal= | |year=1978 | ||
|volume= | |pages=595 | ||
|issue=2 | |isbn=0-89004-225-X | ||
|pages= | |oclc= | ||
|year= | |doi= | ||
|pmid= | }}</ref> The term ''senile dementia of the Alzheimer type'' (SDAT) was used for a time to describe the condition in those over 65, with classical Alzheimer's disease being used for those younger. Eventually, the term Alzheimer's disease was formally adopted in medical nomenclature to describe individuals of all ages with a characteristic common symptom pattern, disease course, and [[neuropathology]].<ref name="pmid3531918">{{cite journal | ||
|doi=10. | |author=Amaducci LA, Rocca WA, Schoenberg BS | ||
}} | |title=Origin of the distinction between Alzheimer's disease and senile dementia: how history can clarify nosology | ||
</ref><ref name=" | |journal=Neurology | ||
{{cite | |volume=36 | ||
|author= | |issue=11 | ||
|title=Alzheimer's disease | |pages=1497–1499 | ||
| | |year=1986 | ||
| | |pmid=3531918 | ||
| | |doi= | ||
|pages= | }}</ref> | ||
| | |||
| | |||
}} | ==Epidemiology== | ||
</ref> | {| align="left" border="2"| class="wikitable" style="text-align:center" | ||
|+AD incidence rates<br /> after 65 years of age<ref name="pmid17727890"/> | |||
|author= | |- | ||
|title= | ! Age !! Incidence<br/>(new affected)<br/> per thousand<br /> person–years | ||
|volume= | |- | ||
|issue= | ! 65–69 | ||
|pages= | | 3 | ||
|year= | |- | ||
|pmid= | ! 70–74 | ||
|doi= | | 6 | ||
}}</ref><ref name=" | |- | ||
|author= | ! 75–79 | ||
|title= | | 9 | ||
|journal= | |- | ||
|volume= | ! 80–84 | ||
|issue= | | 23 | ||
|pages= | |- | ||
|year= | ! 85–89 | ||
|pmid= | | 40 | ||
|doi=10. | |- | ||
}}</ref><ref | ! 90– <!-- The digit-width spaces to the left of this comment make the numbers line up properly. --> | ||
| 69 | |||
|} | |||
Alzheimer's disease is the most frequent type of dementia in the elderly and affects almost half of all patients with dementia. Correspondingly, advancing age is the primary risk factor for the disease. <ref>{{cite journal | author = Gorelick P | title = Risk factors for vascular dementia and Alzheimer disease | journal = Stroke | volume = 35 | issue = 11 Suppl 1 | pages = 2620–2622 | year = 2004 | pmid = 15375299 | url = http://stroke.ahajournals.org/cgi/content/full/35/11_suppl_1/2620 | |||
| doi=10.1161/01.STR.0000143318.70292.47 | |||
}} | |||
</ref> <ref> | |||
{{cite journal | {{cite journal | ||
|author= | | author = Hebert L, Scherr P, Bienias J, Bennett D, Evans D | ||
|title= | | title = Alzheimer disease in the U.S. population: prevalence estimates using the 2000 census | ||
|journal=Neurology | | journal = Archives of Neurology | ||
|volume= | | volume = 60 | issue = 8 | pages = 1119–1122 | ||
|issue= | | year = 2003 | pmid = 12925369 | ||
|pages= | | url = http://archneur.ama-assn.org/cgi/content/full/60/8/1119 | ||
|year= | | doi = 10.1001/archneur.60.8.1119 | ||
|pmid= | |||
| | |||
|doi=10. | |||
}}</ref> | }}</ref> | ||
The World Health Organization estimates that globally the total ''[[disability adjusted life years]] (DALY)'' for AD and other dementias exceeded eleven million in 2005, with a projected 3.4% annual increase.<ref> | |||
{{cite web | |||
{{cite journal | |url=http://www.who.int/mental_health/neurology/chapter_2_neuro_disorders_public_h_challenges.pdf | ||
|author= | |title=Neurological disorders: Public health challenges | ||
|title= | |format=PDF | ||
|journal= | |publisher=World Health Organization | ||
|volume= | }}</ref> A study in Denmark found that women aged 65 are at significantly higher risk (22 percent) of developing AD by age 95 than their male counterparts (nine percent), while [[vascular dementia]]s were nearly equal.<ref>{{cite journal | ||
|issue= | |author=Andersen K, Launer LJ, Dewey ME, Letenneur L, Ott A, Copeland JR, Dartigues JF, Kragh-Sorensen P, Baldereschi M, Brayne C, Lobo A, Martinez-Lage JM, Stijnen T, Hofman A | ||
|pages= | |title=Gender differences in the incidence of AD and vascular dementia: The EURODEM Studies. EURODEM Incidence Research Group | ||
|journal=Neurology | |||
|volume=53 | |||
|issue=9 | |||
|pages=1992–1997 | |||
|year=1999 | |year=1999 | ||
|pmid= | |pmid=10599770 | ||
}}</ref> AD | |doi= | ||
{{cite journal | }}</ref> | ||
|author= | |||
|title= | Some studies have shown a relationship between risk of developing AD and lifetime magnetic field exposure, although the mechanism is unknown.<ref>{{cite journal | ||
|journal= | |author=Davanipour Z, Tseng CC, Lee PJ, Sobel E | ||
|volume= | |title=A case-control study of occupational magnetic field exposure and Alzheimer's disease: results from the California Alzheimer's Disease Diagnosis and Treatment Centers | ||
|issue= | |journal=BMC Neurol | ||
|pages= | |volume=7 | ||
|year= | |issue= | ||
| | |pages=13 | ||
| | |year=2007 | ||
}}</ref><ref | |pmid=17559686 | ||
{{cite journal | |doi=10.1186/1471-2377-7-13 | ||
|author= | |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1906833 | ||
|title= | |accessdate=2008-02-26 | ||
|journal= | }}</ref><ref>{{cite journal | ||
|volume= | |author=Qiu C, Fratiglioni L, Karp A, Winblad B, Bellander T | ||
|issue= | |title=Occupational exposure to electromagnetic fields and risk of Alzheimer's disease | ||
|pages= | |journal=Epidemiology | ||
|year= | |volume=15 | ||
|pmid= | |issue=6 | ||
| doi = 10. | |pages=687–694 | ||
}}</ref> | |year=2004 | ||
|author= | |pmid=15475717 | ||
|title= | |doi=10.1097/01.ede.0000142147.49297.9d | ||
|journal= | }}</ref> Other research does not confirm this link.<ref>{{cite journal | ||
|volume= | |author=Seidler A, Geller P, Nienhaus A, Bernhardt T, Ruppe I, Eggert S, Hietanen M, Kauppinen T, Frölich L | ||
|issue= | |title=Occupational exposure to low frequency magnetic fields and dementia: a case-control study | ||
|pages= | |journal=Occup Environ Med | ||
|year= | |volume=64 | ||
| | |issue=2 | ||
| | |pages=108–114 | ||
}}</ref><ref | |year=2007 | ||
|author= | |pmid=17043077 | ||
|title= | |doi=10.1136/oem.2005.024190 | ||
|url=http://oem.bmj.com/cgi/content/full/64/2/108 | |||
|journal= | }}</ref> The role of [[metal]]s in the disease is also controversial.<ref>Role of metals: | ||
|volume= | * {{cite journal | ||
|issue= | |author=Rondeau V, Commenges D, Jacqmin-Gadda H, Dartigues JF |title=Relation between aluminum concentrations in drinking water and Alzheimer's disease: an 8-year follow-up study |journal=American Journal of Epidemiology |volume=152 |issue=1 |pages=59–66 |year=2000 |pmid=10901330 |url=http://aje.oxfordjournals.org/cgi/content/full/152/1/59 |doi=10.1093/aje/152.1.59 }} | ||
|pages= | * {{cite journal |author=Shcherbatykh I, Carpenter DO |title=The role of metals in the etiology of Alzheimer's disease |journal=Journal of Alzheimers Disease |volume=11 |issue=2 |pages=191–205 |year=2007 |pmid=17522444 }} | ||
|year= | * {{cite journal | ||
|pmid= | |author=Santibáñez M, Bolumar F, García AM |title=Occupational risk factors in Alzheimer's disease: a review assessing the quality of published epidemiological studies |journal=Occupational and Environmental Medicine |volume=64 |issue=11 |pages=723–732 |year=2007 |pmid=17525096 |doi=10.1136/oem.2006.028209}} | ||
}} | * {{cite web | ||
|author= | |url=http://www.who.int/water_sanitation_health/dwq/wsh0304_53/en/index8.html | ||
|title= | |publisher=World Health Organization | ||
|journal= | |title=Water sanitation in health: Aluminum in drinking water | ||
|volume= | |year=2003 | ||
|issue= | }}</ref> | ||
|pages= | |||
|year= | Two main measures are used in [[epidemiology|epidemiological]] studies: incidence and prevalence. [[Incidence (epidemiology)|Incidence]] is the number of new cases per unit of person–time at risk (usually number of new cases per thousand person–years); while [[prevalence]] is the total number of cases of the disease in the population at a given time. | ||
|pmid= | |||
}} | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |||
| | |||
| | |||
| | |||
| | |||
}}</ref> | |||
[[ | Regarding incidence, [[cohort study|cohort]] longitudinal studies (studies where a disease-free population is followed over the years) provide rates between 10–15 per thousand person–years for all dementias and 5–8 for AD,<ref name="pmid17727890">{{cite journal | ||
=== | |author=Bermejo-Pareja F, Benito-León J, Vega S, Medrano MJ, Román GC | ||
|title=Incidence and subtypes of dementia in three elderly populations of central Spain | |||
{{cite journal | |journal=J. Neurol. Sci. | ||
|author= | |volume=264 | ||
|title= | |issue=1–2 | ||
|journal= | |pages=63–72 | ||
|volume= | |year=2008 | ||
|month=January | |||
|pmid=17727890 | |||
|doi=10.1016/j.jns.2007.07.021 | |||
}}</ref><ref name="pmid12028245">{{cite journal | |||
|author=Di Carlo A, Baldereschi M, Amaducci L, ''et al'' | |||
|title=Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study | |||
|journal=J Am Geriatr Soc | |||
|volume=50 | |||
|issue=1 | |issue=1 | ||
|pages= | |pages=41–8 | ||
|year= | |year=2002 | ||
|month= | |month=January | ||
|pmid= | |pmid=12028245 | ||
}}</ref> which means that half of new dementia cases each year are AD. Advancing age is a primary risk factor for the disease and incidence rates are not equal for all ages: every five years after the age of 65, the risk of acquiring the disease approximately doubles, increasing from 3 to as much as 69 per thousand person years.<ref name="pmid17727890"/><ref name="pmid12028245"/> There are also sex differences in the incidence rates, women having a higher risk of developing AD particularly in the population older than 85.<ref name="pmid12028245"/><ref>{{cite journal | |||
}}</ref> | |author=Andersen K, Launer LJ, Dewey ME, ''et al'' | ||
{{cite journal | |title=Gender differences in the incidence of AD and vascular dementia: The EURODEM Studies. EURODEM Incidence Research Group | ||
|author= | |journal=Neurology | ||
|title= | |volume=53 | ||
|journal= | |issue=9 | ||
|volume= | |pages=1992–7 | ||
|issue= | |year=1999 | ||
|pages= | |month=December | ||
|year= | |pmid=10599770 | ||
|pmid= | }}</ref> | ||
}}</ref> | |||
{{cite journal | Prevalence of AD in populations is dependent upon different factors including incidence and survival. Since the incidence of AD increases with age, it is particularly important to include the mean age of the population of interest. In the United States, Alzheimer prevalence was estimated to be 1.6% in the year 2000 both overall and in the 65–74 age group, with the rate increasing to 19% in the 75–84 group and to 42% in the greater than 84 group.<ref>2000 U.S. estimates: | ||
|author= | *{{cite journal | ||
|title= | |author=Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA | ||
|journal= | |title=Alzheimer disease in the US population: prevalence estimates using the 2000 census | ||
|volume= | |journal=Arch. Neurol. | ||
|issue= | |volume=60 | ||
|pages= | |issue=8 | ||
|pages=1119–22 | |||
|year=2003 | |||
|month=August | |||
|pmid=12925369 | |||
|doi=10.1001/archneur.60.8.1119 | |||
}} | |||
*{{cite web | |||
|title=Profiles of general demographic characteristics, 2000 census of population and housing, United States | |||
|year=2001 | |||
|publisher=U.S. Census Bureau | |||
|url=http://www.census.gov/prod/cen2000/dp1/2kh00.pdf | |||
|format=PDF | |||
|accessdate=2008-08-27 | |||
}}</ref> Prevalence rates in less developed regions are lower.<ref name="pmid16360788"/> The [[World Health Organization]] estimated that in 2005, 0.379% of people worldwide had dementia, and that the prevalence would increase to 0.441% in 2015 and to 0.556% in 2030.<ref name="isbn9789241563369">{{cite book | |||
| last = World Health Organization | |||
| title = Neurological Disorders: Public Health Challenges | |||
| publisher = World Health Organization | |||
| year = 2006 | |||
| location = Switzerland | |||
| pages = 204–207 | |||
| url = http://www.who.int/mental_health/neurology/neurodiso/en/index.html | |||
| isbn = 978-92-4-156336-9 }}</ref> Other studies have reached similar conclusions.<ref name="pmid16360788">{{cite journal | |||
|author=Ferri CP, Prince M, Brayne C, ''et al'' | |||
|title=Global prevalence of dementia: a Delphi consensus study | |||
|journal=Lancet | |||
|volume=366 | |||
|issue=9503 | |||
|pages=2112–7 | |||
|year=2005 | |year=2005 | ||
|month= | |month=December | ||
|pmid= | |pmid=16360788 | ||
}}</ref> | |doi=10.1016/S0140-6736(05)67889-0 | ||
|author= | |url=http://www.sbgg.org.br/profissional/artigos/pdf/demencia_mundo.pdf | ||
|title= | |accessdate=2008-06-13 | ||
|journal= | |format=PDF}}</ref> Another study estimated that in 2006, 0.40% of the world population (range 0.17–0.89%; absolute number 26.6 million, range 11.4–59.4 million) were afflicted by AD, and that the prevalence rate would triple and the absolute number would quadruple by the year 2050.<ref name="Brookmeyer2007">2006 prevalence estimate: | ||
|volume= | *{{cite journal | ||
|issue= | |author=Brookmeyer R, Johnson E, Ziegler-Graham K, MH Arrighi | ||
|pages= | |title=Forecasting the global burden of Alzheimer’s disease | ||
|year= | |journal=Alzheimer's and Dementia | ||
|month= | |volume=3 | ||
|issue=3 | |||
|doi=10.1016/j. | |pages=186–91 | ||
|year=2007 | |||
|month=July | |||
|doi=10.1016/j.jalz.2007.04.381 | |||
| | |url=http://works.bepress.com/cgi/viewcontent.cgi?article=1022&context=rbrookmeyer | ||
|accessdate=2008-06-18 | |||
}} | |||
*{{cite paper | |||
|url=http://un.org/esa/population/publications/wpp2006/WPP2006_Highlights_rev.pdf | |||
|format=PDF | |||
|url=http:// | |||
|accessdate=2008-08-27 | |accessdate=2008-08-27 | ||
|year=2007 | |year=2007 | ||
| | |title=World population prospects: the 2006 revision, highlights | ||
| | |publisher=Population Division, Department of Economic and Social Affairs, United Nations | ||
| | |version=Working Paper No. ESA/P/WP.202 | ||
}} | }}</ref> | ||
==Characteristics== | |||
The disease course is divided into four stages, with a progressive decline in cognition and functional capabilities. | |||
===Predementia=== | |||
The first symptoms are commonly misattributed to normal [[ageing]] or [[Stress (medicine)|stress]].<ref name="pmid17222085"/> Detailed [[neuropsychology|neuropsychological]] testing can reveal mild cognitive difficulties up to eight years before a person meets the clinical criteria for [[diagnosis]] of AD.<ref>Preclinical: | |||
*{{cite journal | *{{cite journal | ||
|author= | |author=Linn RT, Wolf PA, Bachman DL, ''et al'' | ||
|title= | |title=The 'preclinical phase' of probable Alzheimer's disease. A 13-year prospective study of the Framingham cohort | ||
|journal= | |journal=Arch. Neurol. | ||
|volume= | |volume=52 | ||
|issue=5 | |issue=5 | ||
|pages= | |pages=485–90 | ||
|year= | |year=1995 | ||
|month=May | |month=May | ||
|pmid= | |pmid=7733843 | ||
| | |accessdate=2008-08-04 | ||
}} | }} | ||
*{{cite journal | *{{cite journal | ||
|author= | |author=Saxton J, Lopez OL, Ratcliff G, ''et al'' | ||
|title= | |title=Preclinical Alzheimer disease: neuropsychological test performance 1.5 to 8 years prior to onset | ||
|journal= | |journal=Neurology | ||
|volume= | |volume=63 | ||
|issue= | |issue=12 | ||
|pages= | |pages=2341–7 | ||
|year= | |year=2004 | ||
|month= | |month=December | ||
|pmid= | |pmid=15623697 | ||
}} | |||
}} | *{{cite journal | ||
|author= | |author=Twamley EW, Ropacki SA, Bondi MW | ||
|title= | |title=Neuropsychological and neuroimaging changes in preclinical Alzheimer's disease | ||
|journal= | |journal=J Int Neuropsychol Soc | ||
|volume= | |volume=12 | ||
|issue= | |issue=5 | ||
|pages= | |pages=707–35 | ||
|year= | |year=2006 | ||
|month= | |month=September | ||
|pmid= | |pmid=16961952 | ||
}}</ref> These symptoms | |pmc=1621044 | ||
|author= | |doi=10.1017/S1355617706060863 | ||
|title= | }}</ref> These early symptoms can affect the most complex [[Activities of daily living|daily living activities]].<ref name="pmid16513677">{{cite journal | ||
|journal= | |author=Perneczky R, Pohl C, Sorg C, Hartmann J, Komossa K, Alexopoulos P, Wagenpfeil S, Kurz A | ||
|volume= | |title=Complex activities of daily living in mild cognitive impairment: conceptual and diagnostic issues | ||
|issue= | |journal=Age Ageing | ||
|pages= | |volume=35 | ||
|year= | |issue=3 | ||
| | |pages=240–245 | ||
| | |year=2006 | ||
}}</ref> | |pmid=16513677 | ||
|doi=10.1093/ageing/afj054 | |||
}}</ref> The most noticeable early deficit is memory loss. The patient has difficulty remembering recently learned facts and acquiring new information.<ref name="pmid12603249">{{cite journal | |||
|author=Arnáiz E, Almkvist O | |||
|title=Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease | |||
|author= | |journal=Acta Neurol. Scand., Suppl. | ||
|title= | |volume=179 | ||
|pages=34–41 | |||
|journal= | |||
|volume= | |||
|pages= | |||
|year=2003 | |year=2003 | ||
|pmid=12603249 | |||
|pmid= | |doi=10.1034/j.1600-0404.107.s179.7.x | ||
|doi=10. | |accessdate=2008-06-12 | ||
}}</ref><ref name="pmid15785034">{{cite journal | |||
|author=Kazui H, Matsuda A, Hirono N, ''et al'' | |||
|title=Everyday memory impairment of patients with mild cognitive impairment | |||
|journal=Dement Geriatr Cogn Disord | |||
|volume=19 | |||
|issue=5–6 | |||
|pages=331–7 | |||
|year=2005 | |||
|pmid=15785034 | |||
|doi=10.1159/000084559 | |||
|url=http://content.karger.com/produktedb/produkte.asp?typ=fulltext&file=DEM20050195_6331 | |||
|accessdate=2008-06-12 | |||
}}</ref> Subtle problems with the [[executive functions]] of [[attention|attentiveness]], [[planning]], flexibility, and [[abstraction|abstract thinking]], or impairments in [[semantic memory]] (memory of meanings, and conceptual relationships), can also be symptomatic of the early stages of AD.<ref name="pmid15703322"> | |||
{{cite journal | |||
| | |author=Rapp MA, Reischies FM | ||
|title=Attention and executive control predict Alzheimer disease in late life: results from the Berlin Aging Study (BASE) | |||
|journal=American Journal of Geriatric Psychiatry | |||
|volume=13 | |||
|issue=2 | |||
|pages=134–141 | |||
|year=2005 | |||
|pmid=15703322 | |||
}}</ref> | |doi=10.1176/appi.ajgp.13.2.134 | ||
}} | |||
|author= | </ref><ref name="pmid12754679"> | ||
|title= | {{cite journal | ||
|journal= | |author=Spaan PE, Raaijmakers JG, Jonker C | ||
|volume= | |title=Alzheimer's disease versus normal ageing: a review of the efficiency of clinical and experimental memory measures | ||
|issue= | |journal=Journal of Clinical Experimental Neuropsychology | ||
|pages= | |volume=25 | ||
|year= | |issue=2 | ||
|pmid= | |pages=216–233 | ||
|year=2003 | |||
| | |pmid=12754679 | ||
| | }} | ||
</ref> | |||
[[Apathy]] can be observed at this stage, and remains the most persistent [[neuropsychiatry|neuropsychiatric]] symptom throughout the course of the disease.<ref name="pmid15956265">{{cite journal | |||
|author=Craig D, Mirakhur A, Hart DJ, McIlroy SP, Passmore AP | |||
| | |title=A cross-sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer's disease |journal=American Journal of Geriatric Psychiatry | ||
|volume=13 | |||
|issue=6 | |||
|pages=460–468 | |||
|year=2005 | |||
}}</ref> | |pmid=15956265 | ||
|doi=10.1176/appi.ajgp.13.6.460 | |||
}}</ref><ref name="pmid16567037">{{cite journal | |||
|author=Robert PH, Berr C, Volteau M, Bertogliati C, Benoit M, Sarazin M, Legrain S, Dubois B | |||
|title=Apathy in patients with mild cognitive impairment and the risk of developing dementia of Alzheimer's disease: a one-year follow-up study | |||
|journal=Clin Neurol Neurosurg | |||
|volume=108 | |||
|issue=8 | |||
|pages=733–736 | |||
|year=2006 | |||
|pmid=16567037 | |||
|doi=10.1016/j.clineuro.2006.02.003 | |||
}}</ref><ref name="pmid17485646"> | |||
{{cite journal | |||
|author=Palmer K, Berger AK, Monastero R, Winblad B, Bäckman L, Fratiglioni L | |||
|title=Predictors of progression from mild cognitive impairment to Alzheimer disease | |||
|journal=Neurology | |||
|volume=68 | |||
}}</ref><ref name=" | |issue=19 | ||
|author= | |pages=1596–1602 | ||
|title=Alzheimer's disease | |||
|journal= | |||
|volume=25 | |||
|issue= | |||
|pages= | |||
|year= | |||
|pmid= | |||
}}</ref> | |||
[[ | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2007 | |year=2007 | ||
|pmid= | |pmid=17485646 | ||
|doi=10. | |doi=10.1212/01.wnl.0000260968.92345.3f | ||
}}</ref> | }}</ref> The preclinical stage of the disease has also been termed [[mild cognitive impairment]],<ref name="pmid17408315"> | ||
|author= | {{cite journal | ||
|title= | |author=Small BJ, Gagnon E, Robinson B | ||
|journal= | |title=Early identification of cognitive deficits: preclinical Alzheimer's disease and mild cognitive impairment | ||
|volume= | |journal=Geriatrics | ||
|issue= | |volume=62 | ||
|pages= | |issue=4 | ||
|year= | |pages=19–23 | ||
| | |year=2007 | ||
| | |month=April | ||
}}</ref> | |pmid=17408315 | ||
}}</ref> but there is still debate on whether this term corresponds to a different and separate diagnostic entity or is just a first step of Alzheimer's disease.<ref name="pmid17279076"> | |||
|author= | {{cite journal | ||
|title= | |author=Petersen RC | ||
|journal= | |title=The current status of mild cognitive impairment—what do we tell our patients? | ||
|volume= | |journal=Nat Clin Pract Neurol | ||
|issue= | |volume=3 | ||
|pages= | |issue=2 | ||
|pages=60–1 | |||
|year=2007 | |||
|month=February | |||
|pmid=17279076 | |||
|doi=10.1038/ncpneuro0402 | |||
| | |||
|pmid= | |||
|doi = 10. | |||
}}</ref> | }}</ref> | ||
===Early dementia=== | |||
|author= | In people with AD the increasing impairment of learning and memory eventually leads to a definitive diagnosis. In a small proportion of them, difficulties with language, executive functions, [[perception]] ([[agnosia]]), or execution of movements ([[apraxia]]) are more prominent than memory problems.<ref name="pmid10653284"> | ||
|title= | {{cite journal | ||
|journal= | |author=Förstl H, Kurz A | ||
|volume= | |title=Clinical features of Alzheimer's disease | ||
|issue= | |journal=European Archives of Psychiatry and Clinical Neuroscience | ||
|pages= | |volume=249 | ||
|year= | |issue=6 | ||
|pages=288–290 | |||
|pmid= | |year=1999 | ||
|pmid=10653284 | |||
}}</ref> | }}</ref> AD does not affect all memory capacities equally. [[long-term memory|Older memories]] of the person's life ([[episodic memory]]), facts learned ([[semantic memory]]), and [[implicit memory]] (the memory of the body on how to do things, such as using a fork to eat) are less affected than new facts or memories.<ref name="pmid1300219"> | ||
{{cite journal | |||
|author=Carlesimo GA, Oscar-Berman M | |||
|title=Memory deficits in Alzheimer's patients: a comprehensive review | |||
|journal=Neuropsychol Rev | |||
|volume=3 | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue=2 | |issue=2 | ||
|pages= | |pages=119–69 | ||
|year= | |year=1992 | ||
| | |month=June | ||
| | |pmid=1300219 | ||
}}</ref> | }}</ref><ref name="pmid8821346"> | ||
|author= | {{cite journal | ||
|title= | |author=Jelicic M, Bonebakker AE, Bonke B | ||
|journal= | |title=Implicit memory performance of patients with Alzheimer's disease: a brief review | ||
|volume= | |journal=International Psychogeriatrics | ||
|pages= | |volume=7 | ||
|year= | |issue=3 | ||
|pmid= | |pages=385–392 | ||
}}</ref> | |year=1995 | ||
|pmid=8821346 | |||
| doi = 10.1017/S1041610295002134 | |||
[[ | }}</ref> [[semantic memory|Language problems]] include a shrinking [[vocabulary]] and decreased word [[fluency]], which lead to a general impoverishment of oral and written language. In this stage, the person with Alzheimer's is usually capable of adequately communicating basic ideas.<ref name="pmid7967534">{{cite journal | ||
|author= | |author=Frank EM | ||
|title= | |title=Effect of Alzheimer's disease on communication function | ||
|journal= | |journal=J S C Med Assoc | ||
|volume= | |volume=90 | ||
|issue= | |issue=9 | ||
|pages= | |pages=417–23 | ||
|year= | |year=1994 | ||
|pmid= | |month=September | ||
| | |pmid=7967534 | ||
}}</ref><ref name=" | }}</ref><ref name="pmid12402233">{{cite journal | ||
|author= | |author=Becker JT, Overman AA | ||
|title= | |title=[The semantic memory deficit in Alzheimer's disease] | ||
|journal= | |language=Spanish; Castilian | ||
|volume= | |journal=Rev Neurol | ||
|issue= | |volume=35 | ||
|pages= | |issue=8 | ||
|year= | |pages=777–83 | ||
| | |year=2002 | ||
| | |pmid=12402233 | ||
}}</ref> | }}</ref><ref name="pmid7617154">{{cite journal | ||
{{cite | |author=Hodges JR, Patterson K | ||
| | |title=Is semantic memory consistently impaired early in the course of Alzheimer's disease? Neuroanatomical and diagnostic implications | ||
| | |journal=Neuropsychologia | ||
| | |volume=33 | ||
| | |issue=4 | ||
| | |pages=441–59 | ||
|year = | |year=1995 | ||
| | |month=April | ||
| | |pmid=7617154 | ||
}}</ref> | }}</ref> While performing [[fine motor skill|fine motor tasks]] such as writing, drawing or dressing, difficulty with planning and coordinating certain movements ([[apraxia]]) may be present, making sufferers appear [[clumsiness|clumsy]].<ref name="pmid8124945">{{cite journal | ||
{{cite journal | |author=Benke T | ||
|author= | |title=Two forms of apraxia in Alzheimer's disease | ||
|title= | |journal=Cortex | ||
|journal= | |volume=29 | ||
|volume= | |issue=4 | ||
|pages=715–25 | |||
|year=1993 | |||
|month=December | |||
|pmid=8124945 | |||
}}</ref> As the disease progresses, people with AD can often continue to perform many tasks independently, but may need assistance or supervision with cognitively demanding activities.<ref name="pmid10653284"/> | |||
[[Image:Portion of Reagan's Alzheimer's letter.png|left|thumb|120px|In 1994 United States ex-president R. Reagan informed the country of his AD diagnosis via a hand-written letter.]] | |||
===Moderate dementia=== | |||
Progressive deterioration eventually hinders independence.<ref name="pmid10653284" /> Speech difficulties become more evident, with an inability to recall vocabulary leading to frequent incorrect word substitutions ([[paraphasia]]s). Reading and writing skills are also progressively lost.<ref name="pmid7967534"/><ref name="pmid15121235"> | |||
{{cite journal | |||
|author=Forbes KE, Shanks MF, Venneri A | |||
|title=The evolution of dysgraphia in Alzheimer's disease | |||
|journal=Brain Res. Bull. | |||
|volume=63 | |||
|issue=1 | |issue=1 | ||
|pages= | |pages=19–24 | ||
|year= | |year=2004 | ||
|pmid= | |month=March | ||
|doi=10. | |pmid=15121235 | ||
}}</ref> | |doi=10.1016/j.brainresbull.2003.11.005 | ||
{{ | }}</ref> Complex motor sequences become less coordinated as time passes, reducing the ability to perform most normal daily activities.<ref name="pmid16209425"> | ||
cite journal |author= | {{cite journal | ||
}} | |author=Galasko D, Schmitt F, Thomas R, Jin S, Bennett D | ||
</ref> | |title=Detailed assessment of activities of daily living in moderate to severe Alzheimer's disease | ||
|journal=Journal of the International Neuropsychology Society | |||
|volume=11 | |||
|issue=4 | |||
|author= | |pages=446–453 | ||
|title= | |year=2005 | ||
|journal= | |pmid=16209425 | ||
|volume= | }}</ref> During this phase, memory problems worsen, and the person may fail to recognise close relatives.<ref name="pmid1737981"> | ||
|issue= | {{cite journal | ||
|pages= | |author=Galasko D, Schmitt F, Thomas R, Jin S, Bennett D | ||
|year= | |title=Detailed assessment of activities of daily living in moderate to severe Alzheimer's disease | ||
| | |journal=J Int Neuropsychol Soc | ||
| | |volume=11 | ||
}}</ref> | |issue=4 | ||
{{ | |pages=446–53 | ||
cite journal |author= | |year=2005 | ||
}} | |month=July | ||
</ref> | |pmid=16209425 | ||
}}</ref> [[Long-term memory]], which was previously intact, becomes impaired,<ref name="pmid15288331">{{cite journal | |||
{{ | |author=Sartori G, Snitz BE, Sorcinelli L, Daum I | ||
|title=Remote memory in advanced Alzheimer's disease | |||
|journal=Arch Clin Neuropsychol | |||
|volume=19 | |||
|issue=6 | |||
|pages=779–89 | |||
}} | |year=2004 | ||
</ref> | |month=September | ||
|pmid=15288331 | |||
|doi=10.1016/j.acn.2003.09.007 | |||
[[ | }}</ref> and behavioural changes become more prevalent. Common [[neuropsychiatric]] manifestations are wandering, sundowning,<ref>{{cite journal | ||
|author=Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A | |||
|title=Sundowning and circadian rhythms in Alzheimer's disease | |||
{{ | |journal=Am J Psychiatry | ||
cite journal |author= | |volume=158 | ||
|issue=5 | |||
|pages=704–11 | |||
|year=2001 | |||
|month=May | |||
|pmid=11329390 | |||
|url=http://ajp.psychiatryonline.org/cgi/content/full/158/5/704 | |||
|accessdate=2008-08-27 | |||
}}</ref> [[irritability]] and [[labile affect]], leading to crying, outbursts of unpremeditated [[aggression]], or resistance to caregiving. Approximately 30% of patients also develop [[Delusional misidentification syndrome|illusionary misidentifications]] and other [[delusion]]al symptoms.<ref name="pmid15956265"/><ref>Neuropsychiatric symptoms: | |||
*{{cite journal | |||
|author=Scarmeas N, Brandt J, Blacker D, ''et al'' | |||
|title=Disruptive behavior as a predictor in Alzheimer disease | |||
|journal=Arch. Neurol. | |||
|volume=64 | |||
|issue=12 | |||
|pages=1755–61 | |||
|year=2007 | |||
|month=December | |||
|pmid=18071039 | |||
|doi=10.1001/archneur.64.12.1755 | |||
}} | }} | ||
*{{cite journal | |||
{{ | |author=Tatsch MF, Bottino CM, Azevedo D, ''et al'' | ||
cite journal |author= | |title=Neuropsychiatric symptoms in Alzheimer disease and cognitively impaired, nondemented elderly from a community-based sample in Brazil: prevalence and relationship with dementia severity | ||
|journal=Am J Geriatr Psychiatry | |||
|volume=14 | |||
|issue=5 | |||
|pages=438–45 | |||
|year=2006 | |||
|month=May | |||
|pmid=16670248 | |||
|doi=10.1097/01.JGP.0000218218.47279.db | |||
}} | }} | ||
*{{cite journal | |||
|author= | |author=Volicer L, Bass EA, Luther SL | ||
|title= | |title=Agitation and resistiveness to care are two separate behavioral syndromes of dementia | ||
|journal= | |journal=J Am Med Dir Assoc | ||
|volume= | |volume=8 | ||
|issue= | |issue=8 | ||
|pages= | |pages=527–32 | ||
|year=2007 | |year=2007 | ||
|pmid= | |month=October | ||
|doi=10. | |pmid=17931577 | ||
}}</ref> | |doi=10.1016/j.jamda.2007.05.005 | ||
|author= | }}</ref> [[Urinary incontinence]] can develop.<ref name="pmid11442300">{{cite journal | ||
|title= | |author=Honig LS, Mayeux R | ||
|journal= | |title=Natural history of Alzheimer's disease | ||
|volume= | |journal=Aging (Milano) | ||
|issue= | |volume=13 | ||
|pages= | |issue=3 | ||
|year= | |pages=171–82 | ||
| | |year=2001 | ||
| | |month=June | ||
}}</ref> | |pmid=11442300 | ||
{{ | }}</ref> These symptoms create [[stress (medicine)|stress]] for relatives and caretakers, which can be reduced by moving the person from [[home care]] to a long-term care facility.<ref name="pmid10653284" /><ref name="pmid7806732">{{cite journal | ||
cite journal |author= | |author=Gold DP, Reis MF, Markiewicz D, Andres D | ||
}} | |title=When home caregiving ends: a longitudinal study of outcomes for caregivers of relatives with dementia | ||
</ref | |journal=J Am Geriatr Soc | ||
|volume=43 | |||
|issue=1 | |||
|pages=10–6 | |||
|year=1995 | |||
|month=January | |||
|pmid=7806732 | |||
}}</ref> | |||
|author= | ===Advanced dementia=== | ||
|title= | During this last stage of AD, the patient is completely dependent upon caregivers. Language is reduced to simple phrases or even single words, eventually leading to complete loss of speech.<ref name="pmid7967534"/> | ||
|journal= | Despite the loss of verbal language abilities, patients can often understand and return emotional signals.<ref name="pmid14685735">{{cite journal | ||
|volume= | |author=Bär M, Kruse A, Re S | ||
|issue= | |title=[Situations of emotional significance in residents suffering from dementia] | ||
|pages= | |language=German | ||
|journal=Z Gerontol Geriatr | |||
|volume=36 | |||
|issue=6 | |||
|pages=454–62 | |||
|year=2003 | |year=2003 | ||
|pmid= | |month=December | ||
|doi=10. | |pmid=14685735 | ||
}}</ref> | |doi=10.1007/s00391-003-0191-0 | ||
{{ | }}</ref> | ||
cite journal |author= | Although aggressiveness can still be present, extreme apathy and [[exhaustion]] are much more common.<ref name="pmid10653284" /> | ||
}} | Patients will ultimately not be able to perform even the most simple tasks without assistance. [[musculature|Muscle mass]] and mobility deteriorate to the point where the patient is bedridden,<ref name="pmid7775724">{{cite journal | ||
</ref><ref name=" | |author=Souren LE, Franssen EH, Reisberg B | ||
{{ | |title=Contractures and loss of function in patients with Alzheimer's disease | ||
cite journal |author= | |journal=J Am Geriatr Soc | ||
}} | |volume=43 | ||
</ref> | |issue=6 | ||
|pages=650–5 | |||
|year=1995 | |||
{{ | |month=June | ||
cite journal |author= | |pmid=7775724 | ||
}}</ref> and they lose the ability to feed themselves.<ref name="pmid12675103">{{cite journal | |||
|author=Berkhout AM, Cools HJ, van Houwelingen HC | |||
|title=The relationship between difficulties in feeding oneself and loss of weight in nursing-home patients with dementia | |||
|journal=Age Ageing | |||
|journal= | |volume=27 | ||
|volume= | |issue=5 | ||
|issue= | |pages=637–41 | ||
|pages= | |year=1998 | ||
|year= | |month=September | ||
|pmid= | |pmid=12675103 | ||
}}</ref> | |||
}}</ref> | When death comes, it is usually directly caused by some external factor such as [[bedsore|pressure ulcers]] or [[pneumonia]], rather than the disease itself.<ref name="pmid11490146">{{cite journal | ||
|author= | |author=Wada H, Nakajoh K, Satoh-Nakagawa T, ''et al'' | ||
|title= | |title=Risk factors of aspiration pneumonia in Alzheimer's disease patients | ||
|journal= | |journal=Gerontology | ||
|volume= | |volume=47 | ||
|issue=5 | |||
|pages=271–6 | |||
|year=2001 | |||
|pmid=11490146 | |||
}}</ref><ref name="pmid10369823">{{cite journal | |||
|author=Gambassi G, Landi F, Lapane KL, Sgadari A, Mor V, Bernabei R | |||
|title=Predictors of mortality in patients with Alzheimer's disease living in nursing homes | |||
|journal=J. Neurol. Neurosurg. Psychiatr. | |||
|volume=67 | |||
|issue=1 | |issue=1 | ||
|pages= | |pages=59–65 | ||
|year= | |year=1999 | ||
|pmid= | |month=July | ||
| | |pmid=10369823 | ||
}}</ref><ref> | |pmc=1736445 | ||
{{cite journal | }}</ref> | ||
<br clear="left"/> | |||
==Pathophysiology== | |||
[[Image:Alzheimer's disease - MRI.jpg|thumb|220px|[[MRI]] images of a normal aged brain (right) and an Alzheimer's patient's brain (left). In the Alzheimer brain, atrophy is clearly seen.]] | |||
At a [[macroscopic]] level, AD is characterised by loss of [[neuron]]s and [[synapse]]s in the [[cerebral cortex]] and certain subcortical regions. This results in gross [[atrophy]] of the affected regions, including degeneration in the [[temporal lobe]] and [[parietal lobe]], and parts of the [[frontal cortex]] and [[cingulate gyrus]].<ref name="pmid12934968">{{cite journal |author=Wenk GL |title=Neuropathologic changes in Alzheimer's disease |journal=Journal of Clinical Psychiatry |volume=64 Suppl 9 |issue= |pages=7–10 |year=2003 |pmid=12934968 |doi=}}</ref> | |||
Three major competing hypotheses exist to explain the cause of the disease. The oldest is the ''[[cholinergic]] hypothesis'', which proposes that AD is caused by reduced synthesis of the [[neurotransmitter]] [[acetylcholine]]. Most currently available drug therapies in Alzheimer's are based on this theory, however, the medications that treat acetylcholine deficiency only affect symptoms of the disease and neither halt nor reverse it.<ref name="pmid16644763">{{cite journal |author=Walker LC, Rosen RF |title=Alzheimer therapeutics-what after the cholinesterase inhibitors? |journal=Age Ageing |volume=35 |issue=4 |pages=332–335 |year=2006 |pmid=16644763 |doi=10.1093/ageing/afl009}}</ref> | |||
The cholinergic hypothesis has not maintained widespread support in the face of this evidence, although cholinergic effects have been proposed to initiate large-scale aggregation,<ref name="pmid15236795">{{cite journal |author=Shen ZX |title=Brain cholinesterases: II. The molecular and cellular basis of Alzheimer's disease |journal=Medical Hypotheses |volume=63 |issue=2 |pages=308–321 |year=2004 |pmid=15236795 |doi=10.1016/j.mehy.2004.02.031}}</ref> leading to generalised neuroinflammation.<ref name="pmid12934968">{{cite journal |author=Wenk GL |title=Neuropathologic changes in Alzheimer's disease |journal=Journal of Clinical Psychiatry |volume=64 Suppl 9 |issue= |pages=7–10 |year=2003 |pmid=12934968 |doi=}}</ref> In 1991 the [[amyloid beta|amyloid]] hypothesis was proposed,<ref name="pmid1763432">{{cite journal |author=Hardy J, Allsop D |title=Amyloid deposition as the central event in the aetiology of Alzheimer's disease |journal=Trends Pharmacol. Sci. |volume=12 |issue=10 |pages=383–8 |year=1991 |pmid=1763432 |doi=10.1016/0165-6147(91)90609-V }}</ref> while research after 2000 is also centered on [[tau protein]]s. The two positions differ with one stating that the tau protein abnormalities initiate the disease cascade, while the other states that amyloid beta (Aβ) deposits are the causative factor in the disease.<ref name="pmid11801334">{{cite journal |author=Mudher A, Lovestone S |title=Alzheimer's disease-do tauists and baptists finally shake hands? |journal=Trends in Neuroscience |volume=25 |issue=1 |pages=22–26 |year=2002 |pmid=11801334 | doi=10.1016/S0166-2236(00)02031-2 }}</ref> | |||
The ''[[amyloid beta|amyloid]] hypothesis'' postulates that amyloid beta (Aβ) deposits are the fundamental cause of the disease.<ref name="pmid1763432">{{cite journal | |||
|author= | |author=Hardy J, Allsop D | ||
|title= | |title=Amyloid deposition as the central event in the aetiology of Alzheimer's disease | ||
|journal= | |journal=Trends Pharmacol. Sci. | ||
|volume= | |volume=12 | ||
|issue= | |issue=10 | ||
|pages= | |pages=383–88 | ||
|year= | |year=1991 | ||
| | |month=October | ||
| | |pmid=1763432 | ||
}}</ref> | }}</ref><ref name="pmid11801334">{{cite journal | ||
{{ | |author=Mudher A, Lovestone S | ||
cite journal |author= | |title=Alzheimer's disease-do tauists and baptists finally shake hands? | ||
}} | |journal=Trends Neurosci. | ||
</ref> | |volume=25 | ||
|author= | |issue=1 | ||
|title= | |pages=22–26 | ||
|journal= | |year=2002 | ||
|volume= | |month=January | ||
|issue= | |pmid=11801334 | ||
|pages= | }}</ref> | ||
[[Image:Amyloid-plaque formation-big.jpg|300px|left|thumb|border|Enzymes act on the APP (amyloid precursor protein) and cut it into fragments. The beta-amyloid fragment is crucial in the formation of senile plaques in AD.]] | |||
Alzheimer's disease has been identified as a [[protein folding|protein misfolding]] disease, or [[proteopathy]], due to the accumulation of abnormally folded A-beta and tau proteins in the brains of AD patients.<ref name="pmid14528050">{{cite journal |author=Hashimoto M, Rockenstein E, Crews L, Masliah E |title=Role of protein aggregation in mitochondrial dysfunction and neurodegeneration in Alzheimer's and Parkinson's diseases |journal=Neuromolecular Medicine |volume=4 |issue=1–2 |pages=21–36 |year=2003 |pmid=14528050 |doi=10.1385/NMM:4:1-2:21}}</ref> | |||
Plaques are made of a small [[peptide]] (39 to 43 amino acid residues) called [[beta-amyloid]] (also A-beta or Aβ), a [[protein]] fragment snipped from a larger protein called [[amyloid precursor protein]] (APP). APP is a [[transmembrane protein]]; which means that it sticks through the neuron's membrane; and is believed to help neurons grow, survive and repair themselves after injury.<ref name="pmid16822978">{{cite journal |author=Priller C, Bauer T, Mitteregger G, Krebs B, Kretzschmar HA, Herms J |title=Synapse formation and function is modulated by the amyloid precursor protein |journal=Journal of Neuroscience |volume=26 |issue=27 |pages=7212–7221 |year=2006 |pmid=16822978 |doi=10.1523/JNEUROSCI.1450-06.2006}}</ref><ref name="pmid12927332">{{cite journal |author=Turner PR, O'Connor K, Tate WP, Abraham WC |title=Roles of amyloid precursor protein and its fragments in regulating neural activity, plasticity and memory |journal=Prog. Neurobiology |volume=70 |issue=1 |pages=1–32 |year=2003 |pmid=12927332 |doi=}}</ref> In AD, something causes APP to be divided by [[enzymes]] through a mechanism called [[proteolysis]].<ref name="pmid15787600">{{cite journal |author=Hooper NM |title=Roles of proteolysis and lipid rafts in the processing of the amyloid precursor protein and prion protein |journal=Biochemical Society Transactions |volume=33 |issue=Pt 2 |pages=335–338 |year=2005 |pmid=15787600 |doi=10.1042/BST0330335}}</ref> One of these fragments is [[beta-amyloid]]. Beta-amyloid fragments (amyloid fibrils) outside the cell form clumps that deposit outside neurons in dense formations known as [[senile plaques]].<ref name="pmid15004691">{{cite journal |author=Ohnishi S, Takano K |title=Amyloid fibrils from the viewpoint of protein folding |journal=Cellular Molecular Life Sciences |volume=61 |issue=5 |pages=511–524 |year=2004 |pmid=15004691 |doi=10.1007/s00018-003-3264-8}}</ref><ref name="pmid15184601">{{cite journal |author=Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J |title=The importance of neuritic plaques and tangles to the development and evolution of AD |journal=Neurology |volume=62 |issue=11 |pages=1984–1989 |year=2004 |pmid=15184601 |doi=}}</ref> | |||
The amyloid hypothesis is compelling because the gene for the amyloid beta precursor (APP) is located on [[chromosome 21]], and patients with [[trisomy 21]] (Down Syndrome) who thus have an extra [[gene dosage|gene copy]] almost universally exhibit AD-like disorders by 40 years of age.<ref name="pmid16904243">{{cite journal | |||
|author=Nistor M, Don M, Parekh M, Sarsoza F, Goodus M, Lopez GE, Kawas C, Leverenz J, Doran E, Lott IT, Hill M, Head E | |||
|title=Alpha- and beta-secretase activity as a function of age and beta-amyloid in Down syndrome and normal brain | |||
|journal=Neurobiol. Aging | |||
|volume=28 | |||
|issue=10 | |||
|pages=1493–506 | |||
|year=2007 | |year=2007 | ||
|pmid= | |pmid=16904243 | ||
|doi=10.1016/ | |doi=10.1016/j.neurobiolaging.2006.06.023 | ||
}}</ref><ref name=" | }}</ref><ref name="pmid15639317">{{cite journal |author=Lott IT, Head E |title=Alzheimer disease and Down syndrome: factors in pathogenesis |journal=Neurobiology of Aging |volume=26 |issue=3 |pages=383–389 |year=2005 |pmid=15639317 |doi=10.1016/j.neurobiolaging.2004.08.005}}</ref> It should be noted further that [[ApoE4]], the major genetic risk factor for AD, leads to excess amyloid build-up in the brain before AD symptoms arise. Thus, Aβ deposition precedes clinical AD.<ref name="pmid7566000">{{cite journal | ||
|author= | |author=Polvikoski T, Sulkava R, Haltia M, Kainulainen K, Vuorio A, Verkkoniemi A, Niinistö L, Halonen P, Kontula K | ||
|title= | |title=Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein | ||
|journal= | |journal=New England Journal of Medicine | ||
|volume= | |volume=333 | ||
|issue= | |issue=19 | ||
|pages= | |pages=1242–1247 | ||
|year= | |year=1995 | ||
|pmid= | |pmid=7566000 | ||
|doi=10. | |doi=10.1056/NEJM199511093331902 | ||
}}</ref> It is known that some types of inherited AD involve only mutations in the APP gene (although this is not the most common type—others involve genes for "pre-senilin" proteins which process APP and may also have still-unknown functions).<ref>{{cite web |url=http://ghr.nlm.nih.gov/condition=alzheimerdisease |title=Alzheimer disease |publisher=US National Library of Medicine |date=2008-04-25 |accessdate=2008-05-02}}</ref> However, another strong support for the amyloid hypothesis, which looks at Aβ as the common initiating factor for Alzheimer's disease, is that [[Genetically modified organism|transgenic]] mice solely expressing a mutant human APP gene develop fibrillar amyloid plaques.<ref>Beta-amyloid precursor protein | |||
* {{cite journal | |||
|author=Games D, Adams D, Alessandrini R, Barbour R, Berthelette P, Blackwell C, Carr T, Clemens J, Donaldson T, Gillespie F | |||
|title=Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein | |||
|journal=Nature | |||
|volume=373 | |||
|issue=6514 | |||
|pages=523–527 | |||
|year=1995 | |||
|pmid=7845465 | |||
|doi=10.1038/373523a0 | |||
}} | |||
* {{cite journal |author=Masliah E, Sisk A, Mallory M, Mucke L, Schenk D, Games D |title=Comparison of neurodegenerative pathology in transgenic mice overexpressing V717F beta-amyloid precursor protein and Alzheimer's disease |journal=Journal of Neuroscience |volume=16 |issue=18 |pages=5795–5811 |year=1996 |pmid=8795633 |doi=}} | |||
* {{cite journal | |||
|author=Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S, Yang F, Cole G | |||
|title=Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice | |||
|journal=Science | |||
|volume=274 | |||
|issue=5284 | |||
|pages=99–102 | |||
|year=1996 | |||
|pmid=8810256 | |||
|doi = 10.1126/science.274.5284.99 | |||
}}</ref> | }}</ref> | ||
If damage from Aβ is the primary initiating cause of AD, the exact mechanism has not been elucidated. The traditional formulation of the amyloid hypothesis points to the cytotoxicity of mature aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis and thus inducing [[apoptosis]].<ref name="pmid2218531">{{cite journal |author=Yankner BA, Duffy LK, Kirschner DA |title=Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides |journal=Science |volume=250 |issue=4978 |pages=279–282 |year=1990 |pmid=2218531 |doi=10.1126/science.2218531 }}</ref> It is also known that Aβ selectively builds up in the mitochondria of samples from the brains of humans with AD, and in mitochondria from transgenic mice with APP genes, and in both cases inhibits certain mitochondrial enzyme functions, and a similar decrease in glucose utilization in neurons to the one which is a known characteristic of AD. This process may also lead to the formation of damaging reactive oxygen species, calcium influx, and apoptosis. Mechanisms which involve direct damage from Aβ before it forms fibrils and plaques also address the issue that neuronal damage is not correlated as well with plaques, since in this model it is not the plaques themselves which cause the major damage, but rather the precursor Aβ protein directly, via another mechanism.<ref name="pmid17424907">{{cite journal|author=Chen, X, Yan, SD|title=Mitochondrial Aβ: A Potential Cause of Metabolic Dysfunction in Alzheimer's Disease. |journal=IUBMB Life|volume=58|issue=12|pages=686-694|year=2006|pmid=17424907|doi=10.1080/15216540601047767}}</ref> | |||
Again, deposition of amyloid plaques does not correlate well with neuron loss.<ref name="pmid15039236">{{cite journal | |||
|author=Schmitz C, Rutten BP, Pielen A, ''et al'' | |||
|title=Hippocampal neuron loss exceeds amyloid plaque load in a transgenic mouse model of Alzheimer's disease | |||
|journal=Am. J. Pathol. | |||
|volume=164 | |||
|issue=4 | |||
|pages=1495–1502 | |||
|year=2004 | |||
|month=April | |||
|pmid=15039236 | |||
|pmc=1615337 | |||
}}</ref> | |||
[[Image:TAU HIGH.JPG|thumb|right|Upright| Microscopy image of a neurofibrillary tangle, conformed by hyperphosphorylated tau protein]] | |||
This observation supports the ''tau hypothesis'', the idea that [[tau protein]] abnormalities initiate the disease cascade.<ref name="pmid11801334"/> AD is also considered a [[tauopathy]] due to abnormal aggregation of the [[tau protein]]. Healthy neurons have an internal support structure, or [[cytoskeleton]], partly made up of structures called [[microtubules]]. These microtubules act like tracks, guiding nutrients and molecules from the body of the cell down to the ends of the [[axon]] and back. A special kind of protein, tau, makes the microtubules stable through a process named [[phosphorylation]] and is therefore called a [[microtubule-associated protein]].<ref name="pmid17604998">{{cite journal |author=Hernández F, Avila J |title=Tauopathies |journal=Cellular Molecular Life Sciences |volume=64 |issue=17 |pages=2219–2233 |year=2007 |pmid=17604998 |doi=10.1007/s00018-007-7220-x}}</ref> In AD, tau is changed chemically, becoming [[Hyperphosphorylation|hyperphosphorylated]]. | |||
[[Image:TANGLES HIGH.jpg|left|thumb|left|350px|In Alzheimer's disease, changes in tau protein lead to the disintegration of microtubules in brain cells.]] | |||
In the tau hypothesis, hyperphosphorylated tau begins to pair with other threads of tau and they become tangled up together inside nerve cell bodies in masses known as [[neurofibrillary tangles]].<ref name="pmid1669718">{{cite journal |author=Goedert M, Spillantini MG, Crowther RA |title=Tau proteins and neurofibrillary degeneration |journal=Brain Pathology |volume=1 |issue=4 |pages=279–286 |year=1991 |pmid=1669718 | doi=10.1111/j.1750-3639.1991.tb00671.x }}</ref> When this happens, the microtubules disintegrate, collapsing the neuron's transport system. This may result first in malfunctions in communication between neurons and later in the death of the cells.<ref name="pmid17127334">{{cite journal |author=Chun W, Johnson GV |title=The role of tau phosphorylation and cleavage in neuronal cell death |journal=Frontiers of Bioscience |volume=12 |pages=733–756 |year=2007 |pmid=17127334}}</ref> | |||
Both [[amyloid plaques]] and [[neurofibrillary tangle]]s are clearly visible by [[microscopy]] in AD brains.<ref name="pmid15184601">{{cite journal |author=Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J |title=The importance of neuritic plaques and tangles to the development and evolution of AD |journal=Neurology |volume=62 |issue=11 |pages=1984–1989 |year=2004 |pmid=15184601 |doi=}}</ref> Plaques are dense, mostly [[insoluble]] deposits of amyloid-beta [[protein]] and [[cell]]ular material outside and around neurons. Tangles are insoluble twisted fibers that build up inside the nerve cell. Though many older people develop some plaques and tangles, the brains of AD patients have them to a much greater extent and in different brain locations.<ref name="pmid8038565">{{cite journal |author=Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH |title=Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital |journal=Cerebral Cortex |volume=4 |issue=2 |pages=138–150 |year=1994 |pmid=8038565 |doi =10.1093/cercor/4.2.138 }}</ref> | |||
Recent research supports the previously obscure theory that [[Herpes_simplex#Alzheimer.27s_disease|Herpes simplex]] virus type 1 plays a role as a possible cause of AD in people carrying the susceptible versions of the [[Apolipoprotein E|apoE]] gene.<ref name=Itzhaki2008>{{cite journal |author=Wozniak MA, Mee AP, Itzhaki RF |title=Herpes simplex virus type 1 DNA is located within Alzheimer's disease amyloid plaques |journal=J Pathol. |volume=217 |issue=1 |pages=131–8 |year=2009 |month=January |pmid=18973185 |doi=10.1002/path.2449 |url=http://www3.interscience.wiley.com/journal/121411445/abstract}}</ref> | |||
[[ | As HSV-1 is not a new virus, some additional factor is needed to explain the increase | ||
[http://www.cdc.gov/nchs/pressroom/07newsreleases/lifeexpectancy.htm|increase] in the age adjusted incidence of AD. Various inflammatory processes and inflammatory cytokines may also have a role in the pathology of Alzheimer's disease. However, these are general markers of tissue damage in any disease, and may also be either secondary causes of tissue damage in AD, or else bystander "marker" effects.<ref>{{cite journal |author=Greig NH, Mattson MP, Perry T, Chan SL, Giordano T, Sambamurti K, Rogers JT, Ovadia H, Lahiri DK |title=New therapeutic strategies and drug candidates for neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists. |journal=Ann N Y Acad Sci.|volume=1035 |issue=Dec |pages=290–315 |year=2004 |pmid=15681814 |doi=10.1196/annals.1332.018 }}</ref> Other cholinergic effects have also been proposed, for example, initiation of large-scale aggregation of amyloid,<ref name="pmid15236795">{{cite journal | |||
|author=Shen ZX | |||
|title=Brain cholinesterases: II. The molecular and cellular basis of Alzheimer's disease | |||
|journal=Med. Hypotheses | |||
|volume=63 | |||
</ref> | |issue=2 | ||
|pages=308–21 | |||
{{cite journal | |year=2004 | ||
|author= | |pmid=15236795 | ||
|title= | |doi=10.1016/j.mehy.2004.02.031 | ||
|journal= | }}</ref> leading to generalised neuroinflammation.<ref name="pmid12934968">{{cite journal | ||
|volume= | |author=Wenk GL | ||
|title=Neuropathologic changes in Alzheimer's disease | |||
|pages= | |journal=J Clin Psychiatry | ||
|year= | |volume=64 Suppl 9 | ||
|pmid= | |pages=7–10 | ||
|year=2003 | |||
|pmid=12934968 | |||
}}</ref> | }}</ref> | ||
==Diagnosis== | |||
[[Dementia]] is by definition a clinical condition but not an exact diagnosis. Alzheimer's disease is usually diagnosed clinically from the patient history, collateral history from relatives, and clinical observations, based on the presence of characteristic [[Neurology|neurological]] and [[neuropsychology|neuropsychological]] features and the [[Diagnosis of exclusion|absence of alternative conditions]].<ref name="pmid17407994">{{cite journal | |||
|author=Mendez MF | |||
|title=The accurate diagnosis of early-onset dementia | |||
|journal=International Journal of Psychiatry Medicine | |||
|volume=36 | |||
|issue=4 | |||
|pages=401–412 | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2006 | |year=2006 | ||
|pmid= | |pmid=17407994 | ||
|doi= | |doi= | ||
}} | }}</ref><ref name="pmid17018549">{{cite journal | ||
|author=Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J | |||
|author= | |title=Therapeutic approaches to Alzheimer's disease | ||
|title= | |journal=Brain | ||
|journal= | |volume=129 | ||
|volume= | |issue=Pt 11 | ||
|issue=11 | |pages=2840–2855 | ||
|pages= | |year=2006 | ||
|year= | |pmid=17018549 | ||
|pmid= | |doi=10.1093/brain/awl280 | ||
|doi=10. | }}</ref> Advanced [[medical imaging]] with [[Computed tomography|CT]] or [[Magnetic resonance imaging|MRI]], and with [[SPECT]] or [[PET]] are generally used to help to diagnose the subtype of dementia and exclude other cerebral pathology.<ref> | ||
}} | {{cite web | ||
|url = http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf | |||
|author= | |format = PDF | ||
|title= | |title = Dementia: Quick reference guide | ||
|journal=Neurology | |publisher = [[National Institute for Health and Clinical Excellence]] | ||
|volume= | |month = November | ||
|issue= | |year = 2006 | ||
|pages= | |isbn = 1-84629-312-X | ||
|accessdate = 2008-02-22 | |||
}}</ref> Neuropsychological evaluation including memory testing and assessment of intellectual functioning can further characterize the dementia.<ref name="pmid17222085"> | |||
{{cite journal | |||
|author=Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, Scheltens P, Tariska P, Winblad B | |||
|title=Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline | |||
|journal=European Journal of Neurology | |||
|volume=14 | |||
|issue=1 | |||
|pages=e1–26 | |||
|year=2007 | |year=2007 | ||
|pmid= | |pmid=17222085 | ||
|doi=10. | |doi=10.1111/j.1468-1331.2006.01605.x | ||
}}</ref> Medical organizations have created diagnostic criteria to ease and standardize the process for practicing physicians. Sometimes the diagnosis can be confirmed or made at postmortem when brain material is available and can be examined histologically and histochemically.<ref name="pmid6610841"> | |||
{{ | |||
cite journal |author=McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM |title=Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease |journal=Neurology |volume=34 |issue=7 |pages=939–44 |year=1984 |pmid=6610841 |doi= | |||
}} | }} | ||
</ref> | |||
|author= | |||
|title= | ===Diagnostic criteria=== | ||
|journal= | [[NINCDS-ADRDA Alzheimer's Criteria|The diagnostic criteria for Alzheimer of the NINCDS-ADRDA]] (National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association) are among the most used.<ref name="pmid17616482">{{cite journal | ||
|volume= | |author=Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P | ||
|issue= | |title=Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria | ||
|pages= | |journal=Lancet Neurology | ||
|year= | |volume=6 | ||
|pmid= | |issue=8 | ||
|doi=10.1016/ | |pages=734–746 | ||
|year=2007 | |||
|pmid=17616482 | |||
|doi=10.1016/S1474-4422(07)70178-3 | |||
}}</ref> These criteria require that the presence of cognitive impairment and a suspected dementia syndrome be confirmed by [[Neuropsychological assessment|neuropsychological testing]] for a clinical diagnosis of possible or probable AD while they need [[histopathologic]] confirmation ([[microscopic]] examination of [[brain tissue]]) for the definitive diagnosis. They have shown good [[Reliability (statistics)|reliability]] and [[Validity (statistics)|validity]].<ref name="pmid7986174"> | |||
{{ | |||
cite journal |author=Blacker D, Albert MS, Bassett SS, Go RC, Harrell LE, Folstein MF |title=Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative |journal=Archives of Neurology |volume=51 |issue=12 |pages=1198–1204 |year=1994 |pmid=7986174 |doi= | |||
}} | |||
</ref> They specify as well eight cognitive domains that may be impaired in AD (i.e., [[memory]], [[language]], [[perception|perceptual skills]], [[attention]], constructive abilities, [[orientation (mental)|orientation]], [[problem solving]] and functional abilities). | |||
Similar to the NINCDS-ADRDA Alzheimer's Criteria are the ''[[Diagnostic and Statistical Manual of Mental Disorders]]'' (DSM-IV-TR) criteria published by the [[American Psychiatric Association]].<ref> | |||
{{ | |||
cite book | last=American Psychiatric Association | title=Diagnostic and Statistical Manual of Mental disorders, 4th Edition Text Revision | date=2000 | location=Washington DC | | |||
}} | }} | ||
</ref><ref name="pmid8752526"> | |||
|author= | {{ | ||
|title= | cite journal |author=Ito N |title=Clinical aspects of dementia |language=Japanese |journal=Hokkaido Igaku Zasshi |volume=71 |issue=3 |pages=315–320 |year=1996 |pmid=8752526 |doi= | ||
|journal= | }} | ||
|volume= | </ref> | ||
|issue= | |||
|pages= | ===Diagnostic tools=== | ||
|year= | [[Image:InterlockingPentagons.svg|left|220px|framed|Neuropsychological screening tests can help in the diagnosis of AD. In them patients have to copy drawings similar to the one shown in the picture, remember words, read or sum.]] | ||
|pmid= | |||
|doi= | Neuropsychological [[Screening (medicine)|screening]] tests as the [[Mini mental state examination]] (MMSE) are widely used to evaluate the cognitive impairments needed for diagnosis, but more comprehensive batteries are necessary for high reliability by this method, especially in the earliest stages of the disease.<ref name="pmid1512391"> | ||
}}</ref> | {{ | ||
cite journal |author=Tombaugh TN, McIntyre NJ |title=The mini-mental state examination: a comprehensive review |journal=J Am Geriatr Soc |volume=40 |issue=9 |pages=922–935 |year=1992 |pmid=1512391 |doi= | |||
{{cite journal | }} | ||
</ref><ref name="pmid9987708"> | |||
|author= | {{ | ||
| | cite journal |author=Pasquier F |title=Early diagnosis of dementia: neuropsychology |journal=J. Neurol. |volume=246 |issue=1 |pages=6–15 |year=1999 |pmid=9987708 |doi= | ||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
| | |||
}}</ref> | |||
|author= | |||
|title= | |||
|journal=J. | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year= | |||
|pmid= | |||
|doi= | |||
}} | }} | ||
</ref> On the other hand neurological examination in early AD will usually be normal, independent of cognitive impairment; but for many of the other dementing disorders is key for diagnosis. Therefore, neurological examination is crucial in the [[differential diagnosis]] of Alzheimer and other diseases.<ref name="pmid17222085">{{cite journal | |||
| | |author=Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, Scheltens P, Tariska P, Winblad B | ||
| | |title=Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline | ||
| | |journal=European Journal of Neurology | ||
}} | |volume=14 | ||
|issue=1 | |||
|author= | |pages=e1–26 | ||
|title= | |year=2007 | ||
|pmid=17222085 | |||
|journal= | |doi=10.1111/j.1468-1331.2006.01605.x | ||
|volume= | }}</ref> In addition, interviews with family members are also utilised in the assessment of the disease. Caregivers can supply important information on the daily living abilities, as well as on the decrease over time of the patient's mental function.<ref name="pmid16327345">{{cite journal | ||
|issue= | |author=Harvey PD, Moriarty PJ, Kleinman L, Coyne K, Sadowsky CH, Chen M, Mirski DF | ||
|pages= | |title=The validation of a caregiver assessment of dementia: the Dementia Severity Scale | ||
|year= | |journal=Alzheimer Disease and Associated Disorders | ||
|pmid= | |volume=19 | ||
|issue=4 | |||
|pages=186–194 | |||
|year=2005 | |||
|pmid=16327345 | |||
|doi= | |doi= | ||
}}</ref> This is especially important since a patient with AD is commonly unaware of his or her own deficits ([[anosognosia]]).<ref name="pmid15738860"> | |||
{{ | |||
cite journal |author=Antoine C, Antoine P, Guermonprez P, Frigard B |title=Awareness of deficits and anosognosia in Alzheimer's disease. |language=French |journal=Encephale |volume=30 |issue=6 |pages=570–577 |year=2004 |pmid=15738860 |doi= | |||
}} | }} | ||
</ref> Many times families also have difficulties in the detection of initial dementia symptoms and in adequately communicating them to a physician.<ref name="pmid16197855"> | |||
|author= | {{ | ||
|title= | cite journal |author=Cruz VT, Pais J, Teixeira A, Nunes B |title=The initial symptoms of Alzheimer disease: caregiver perception |language=Portuguese |journal=Acta Med Port |volume=17 |issue=6 |pages=435–444 |year=2004 |pmid=16197855 |doi= | ||
|journal= | }} | ||
|volume= | </ref> Finally, supplemental testing provides extra information on some features of the disease or are used to rule out other diagnoses. Examples are [[blood test]]s, which can identify other causes for dementia different than AD,<ref name="pmid17222085"> | ||
|issue= | {{ | ||
|pages= | cite journal |author=Waldemar G, Dubois B, Emre M, ''et al'' |title=Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline |journal=European Journal of Neurology |volume=14 |issue=1 |pages=e1–26 |year=2007 |pmid=17222085 |doi=10.1111/j.1468-1331.2006.01605.x | ||
|year= | |||
|pmid= | |||
|doi= | |||
}}</ref> | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year= | |||
|pmid= | |||
|doi= | |||
}} | }} | ||
</ref> which rarely may even be reversible;<ref>{{cite journal | |||
|author= | |author=Clarfield AM | ||
|title= | |title=The decreasing prevalence of reversible dementias: an updated meta-analysis | ||
|journal= | |journal=Arch. Intern. Med. | ||
|volume= | |volume=163 | ||
|issue= | |issue=18 | ||
|pages= | |pages=2219–29 | ||
|year=2003 | |year=2003 | ||
|pmid= | |pmid=14557220 | ||
|doi=10. | |doi=10.1001/archinte.163.18.2219 | ||
}}</ref> or [[psychological testing|psychological tests]] for [[clinical depression|depression]], as depression can both co-occur with AD or, on the contrary, be at the origin of the patient's cognitive impairment.<ref name="pmid9153154"> | |||
{{ | |||
cite journal |author=Geldmacher DS, Whitehouse PJ |title=Differential diagnosis of Alzheimer's disease |journal=Neurology |volume=48 |issue=5 Suppl 6 |pages=S2–9 |year=1997 |pmid=9153154 |doi= | |||
}} | }} | ||
</ref><ref name="pmid17495754"> | |||
|author= | {{ | ||
|title= | cite journal |author=Potter GG, Steffens DC |title=Contribution of depression to cognitive impairment and dementia in older adults |journal=Neurologist |volume=13 |issue=3 |pages=105–117 |year=2007 |pmid=17495754 |doi=10.1097/01.nrl.0000252947.15389.a9 | ||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2007 | |||
|pmid= | |||
|doi=10. | |||
}} | }} | ||
</ref> | |||
|author= | |||
|title= | Increasingly, the [[functional neuroimaging]] modalities of [[single photon emission computed tomography]] (SPECT) and [[positron emission tomography]] (PET) are being used to diagnose Alzheimer's, as they have shown similar ability to diagnose Alzheimer's disease as methods involving [[mental status examination]].<ref name="pmid16785801"> | ||
|journal= | {{ | ||
|volume= | cite journal |author=Bonte FJ, Harris TS, Hynan LS, Bigio EH, White CL |title=Tc-99m HMPAO SPECT in the differential diagnosis of the dementias with histopathologic confirmation |journal=Clinical nuclear medicine |volume=31 |issue=7 |pages=376–378 |year=2006 |pmid=16785801 |doi=10.1097/01.rlu.0000222736.81365.63 | ||
|issue= | |||
|pages= | |||
|year= | |||
|pmid= | |||
|doi=10. | |||
}} | }} | ||
</ref> Furthermore, the ability of SPECT to differentiate Alzheimer's disease from other possible causes, in a patient already known to be suffering from dementia, appears to be superior to attempts to differentiate the cause of dementia cause by mental testing and history.<ref name="pmid15545324">{{cite journal | |||
|author= | |author=Dougall NJ, Bruggink S, Ebmeier KP | ||
|title= | |title=Systematic review of the diagnostic accuracy of 99mTc-HMPAO-SPECT in dementia | ||
|journal= | |journal=American Journal of Geriatric Psychiatry | ||
|volume= | |volume=12 | ||
|issue= | |issue=6 | ||
|pages= | |pages=554–570 | ||
|year=2004 | |||
|pmid=15545324 | |||
|doi=10.1176/appi.ajgp.12.6.554 | |||
}}</ref> A new technique known as "PiB [[Positron emission tomography|PET]]" has been developed for directly and clearly imaging beta-amyloid deposits [[in vivo]] using a [[Contrast medium|contrasting]] [[Radioactive tracer|tracer]] that [[Binding (molecular)|binds]] selectively to the Abeta deposits.<ref>{{cite journal | |||
|author=Kemppainen NM, Aalto S, Karrasch M, Någren K, Savisto N, Oikonen V, Viitanen M, Parkkola R, Rinne JO | |||
|title=Cognitive reserve hypothesis: Pittsburgh Compound B and fluorodeoxyglucose positron emission tomography in relation to education in mild Alzheimer's disease | |||
|journal=Ann. Neurol. | |||
|volume=63 | |||
|issue=1 | |||
|pages=112–8 | |||
|year=2008 | |year=2008 | ||
|pmid= | |pmid=18023012 | ||
|doi=10. | |doi=10.1002/ana.21212 | ||
}}</ref> [[ | }}</ref><ref> | ||
{{cite journal | |||
|author= | |author=Ikonomovic MD, Klunk WE, Abrahamson EE, Mathis CA, Price JC, Tsopelas ND, Lopresti BJ, Ziolko S, Bi W, Paljug WR, Debnath ML, Hope CE, Isanski BA, Hamilton RL, Dekosky ST | ||
|title= | |title=Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer’s disease | ||
|journal= | |journal=Brain | ||
|volume= | |url=http://brain.oxfordjournals.org/cgi/reprint/awn016?ijkey=KksjlncuMZm8LuP&keytype=ref | ||
|issue= | |date= March 2008 | ||
|pages= | |doi=doi:10.1093/brain/awn016 | ||
|pmid=18339640 | |||
}}</ref><ref name="pmid18263627">{{cite journal | |||
|author=Jack CR, Lowe VJ, Senjem ML, ''et al'' | |||
|title=11C PiB and structural MRI provide complementary information in imaging of Alzheimer's disease and amnestic mild cognitive impairment | |||
|journal=Brain | |||
|volume=131 | |||
|issue=Pt 3 | |||
|pages=665-80 | |||
|year=2008 | |||
|pmid=18263627 | |||
|doi=10.1093/brain/awm336 | |||
}}</ref> Another recent objective marker of the disease is the analysis of [[cerebrospinal fluid]] for [[amyloid beta]] or [[tau protein]]s.<ref name="pmid17612711"> | |||
{{ | |||
cite journal |author=Marksteiner J, Hinterhuber H, Humpel C |title=Cerebrospinal fluid biomarkers for diagnosis of Alzheimer's disease: beta-amyloid(1-42), tau, phospho-tau-181 and total protein |journal=Drugs Today |volume=43 |issue=6 |pages=423–431 |year=2007 |pmid=17612711 |doi=10.1358/dot.2007.43.6.1067341 | |||
}} | |||
</ref> Both advances (neuroimaging and cerebrospinal fluid analysis) have led to the proposal of new diagnostic criteria.<ref name="pmid17616482">{{cite journal | |||
|author=Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P | |||
|title=Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria | |||
|journal=Lancet Neurology | |||
|volume=6 | |||
|issue=8 | |||
|pages=734–746 | |||
|year=2007 | |year=2007 | ||
|pmid= | |pmid=17616482 | ||
|doi=10. | |doi=10.1016/S1474-4422(07)70178-3 | ||
}} | }}</ref><ref name="pmid17222085">{{cite journal | ||
|author=Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, Scheltens P, Tariska P, Winblad B | |||
|author= | |title=Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline | ||
|title= | |journal=European Journal of Neurology | ||
|journal=Journal of | |volume=14 | ||
|volume= | |issue=1 | ||
|issue= | |pages=e1–26 | ||
|pages= | |year=2007 | ||
|year= | |pmid=17222085 | ||
|pmid= | |doi=10.1111/j.1468-1331.2006.01605.x | ||
|doi= | |||
}}</ref> | }}</ref> | ||
==Prevention== | |||
[[Image:Honoré Daumier 032.jpg|left|thumb|220px|Intellectual activities such as playing chess or regular social interaction have been linked to a reduced risk of AD in epidemiological studies, although no causal relationship has been found.]] | |||
At present contradictory results in global studies, incapacity to prove causal relationships between risk factors and the disease, and possible secondary effects indicate a lack of specific measures to prevent or delay the onset of AD.<ref>Prevention recommendations not supported: | |||
* {{cite journal |author=Kawas CH |title=Medications and diet: protective factors for AD? |journal=Alzheimer Dis Assoc Disord |volume=20 |issue=3 Suppl 2 |pages=S89–96 |year=2006 |pmid=16917203 |doi=}} | |||
* {{cite journal |author=Luchsinger JA, Mayeux R |title=Dietary factors and Alzheimer's disease |journal=Lancet Neurol |volume=3 |issue=10 |pages=579–87 |year=2004 |pmid=15380154 |doi=10.1016/S1474-4422(04)00878-6}} | |||
* {{cite journal |author=Luchsinger JA, Noble JM, Scarmeas N |title=Diet and Alzheimer's disease |journal=Curr Neurol Neurosci Rep |volume=7 |issue=5 |pages=366–72 |year=2007 |pmid=17764625 |doi=10.1007/s11910-007-0057-8 }} | |||
</ref> | |||
Different epidemiological studies have proposed relationships between certain modifiable factors, such as diet, cardiovascular risk, pharmaceutical products, or intellectual activities among others, and a population's likelihood of developing AD. Only further research, including clinical trials, will reveal whether, in fact, these factors can help to prevent AD.<ref> | |||
{{cite journal | {{cite journal | ||
|author=Szekely CA, Breitner JC, Zandi PP | |||
|title=Prevention of Alzheimer's disease | |||
|journal=Int Rev Psychiatry | |||
|volume=19 | |||
|issue=6 | |||
|pages=693–706 | |||
|year=2007 | |||
|pmid=18092245 | |||
|doi=10.1080/09540260701797944 | |||
}}</ref> | |||
}}</ref> | |||
The components of a [[Mediterranean diet]], which include fruit and vegetables, [[bread]], [[wheat]] and other [[cereal]]s, [[olive oil]], [[fish]], and [[red wine]], may all individually or together reduce the risk and course of Alzheimer's disease. There is evidence that frequent and moderate consumption of alcohol (beer, wine or distilled spirits) reduces the risk of the disease,<ref>Alcohol: | |||
|author= | *{{cite journal |author=Mulkamal KJ, et al. |title=Prospective study of alcohol consumption and risk of dementia in older adults. |journal=Journal of the American Medical Association |date=2003-03-19 |volume=289|pages=1405-1413}} | ||
|title= | *{{cite journal |author=Ganguli M, et al. |title=Alcohol consumption and cognitive function in late life: A longitudinal community study. |journal=Neurology |year=2005 |volume=65 |pages=1210-1217}} | ||
|journal= | *{{cite journal |author=Huang W, et al. |title=Alcohol consumption and incidence of dementia in a community sample aged 75 years and older. |journal=Journal of Clinical Epidemiology |year=2002 |volume=55|issue=10 |pages=959-964}} | ||
|volume= | *{{cite journal |author=Rodgers B, et al. |title=Non-linear relationships between cognitive function and alcohol consumption in young, middle-aged and older adults: The PATH Through Life Project. |journal=Addiction |year=2005|volume=100|issue=9 |pages=1280-1290 }} | ||
|issue= | *{{cite journal |author=Anstey KJ, et al. |title=Lower cognitive test scores observed in alcohol are associated with demographic, personality, and biological factors: The PATH Through Life Project. |journal=Addiction |year=2005 |volume=100 |issue=9 |pages=1291-1301; }}{{cite journal|author=Espeland, M., et al. |title=Association between alcohol intake and domain-specific cognitive function in older women. |journal=Neuroepidemiology |year=2006 |volume=1 |issue=27 |pages=1-12 }} | ||
|pages= | *{{cite journal |author=Stampfer MJ, et al. |title=Effects of moderate alcohol consumption on cognitive function in women. |journal=New England Journal of Medicine |year=2005 |volume=352 |pages=245-253}} | ||
| | *{{cite journal |author=Ruitenberg A, et al. |title=Alcohol consumption and risk of dementia: the Rotterdam Study. |journal=Lancet |year=2002 |volume=359 |issue=9303 |pages=281-286}} | ||
| | *{{cite journal |author=Scarmeas N, et al. |title=Mediterranean diet and risk for Alzheimer’s disease. |journal=Annals of Neurology |year=2006 |date=2006-04-18}} | ||
| | </ref> <ref> Mediterranean diet: | ||
| | * {{cite journal | ||
| | |author=Scarmeas N, Stern Y, Mayeux R, Luchsinger JA | ||
}} | |title=Mediterranean diet, Alzheimer disease, and vascular mediation | ||
|journal=Arch. Neurol. | |||
|volume=63 | |||
|author= | |issue=12 | ||
|title= | |pages=1709–1717 | ||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2006 | |year=2006 | ||
|pmid= | |pmid=17030648 | ||
|doi=10. | |doi=10.1001/archneur.63.12.noc60109 | ||
}} | |||
* {{cite journal | |||
|author=Scarmeas N, Luchsinger JA, Mayeux R, Stern Y | |||
|title=Mediterranean diet and Alzheimer disease mortality | |||
|journal=Neurology | |||
|volume=69 | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue=11 | |issue=11 | ||
|pages= | |pages=1084–93 | ||
|year= | |year=2007 | ||
|pmid= | |pmid=17846408 | ||
|doi= | |doi=10.1212/01.wnl.0000277320.50685.7c | ||
}} | |||
* {{cite journal | |||
|author=Barberger-Gateau P, Raffaitin C, Letenneur L, Berr C, Tzourio C, Dartigues JF, Alpérovitch A | |||
|title=Dietary patterns and risk of dementia: the Three-City cohort study | |||
|journal=Neurology | |||
|volume=69 | |||
}} | |issue=20 | ||
| | |pages=1921–1930 | ||
|title= | |year=2007 | ||
|pmid=17998483 | |||
| | |doi=10.1212/01.wnl.0000278116.37320.52 | ||
| | }} | ||
* {{cite journal | |||
| | |author=Dai Q, Borenstein AR, Wu Y, Jackson JC, Larson EB | ||
| | |title=Fruit and vegetable juices and Alzheimer's disease: the Kame Project | ||
| | |journal=American Journal of Medicine | ||
|volume=119 | |||
| | |issue=9 | ||
|pages=751–759 | |||
| | |||
}} | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2006 | |year=2006 | ||
|pmid= | |pmid=16945610 | ||
|doi=10. | |doi=10.1016/j.amjmed.2006.03.045 | ||
}} | |||
* {{cite journal | |||
|author=Savaskan E, Olivieri G, Meier F, Seifritz E, Wirz-Justice A, Müller-Spahn F | |||
|title=Red wine ingredient resveratrol protects from beta-amyloid neurotoxicity | |||
|journal=Gerontology | |||
|volume=49 | |||
|issue=6 | |||
|pages=380–383 | |||
|year=2003 | |||
|pmid=14624067 | |||
}} | |doi=10.1159/000073766 | ||
|author= | }}</ref> but it is still considered premature to make dietary recommendations on this basis.<ref> | ||
|title= | {{cite journal|quote=Available data do not permit definitive conclusions regarding diet and AD or specific recommendations on diet modification for the prevention of AD. ||title=Dietary factors and Alzheimer's disease. |author=Luchsinger JA, Mayeux R |pmid=15380154 |journal=Lancet Neurology |date=2004 Oct |volume=3 |issue=10 |pages=579-587 }}</ref><ref> | ||
|journal= | {{cite journal | ||
|volume= | |title=Medications and diet: protective factors for AD? | ||
|issue= | |author=Kawas CH | ||
|pages= | |pmid=16917203 | ||
|year= | |journal=Alzheimer Dis Assoc Disord | ||
|pmid= | |date=2006 Jul-Sep | ||
|doi=10. | |volume=20 | ||
}}</ref> | |issue=3 Suppl 2 | ||
| | |pages=S89-96 | ||
|title= | |quote=Evidence regarding dietary and supplemental intake of vitamins E, C, and folate, and studies of alcohol and wine intake are also reviewed. At present, there is insufficient evidence to make public health recommendations, but these studies can provide potentially important clues and new avenues for clinical and laboratory research. | ||
| | }}</ref> [[vitamin E|Vitamins E]], [[B-vitamins|B]], and [[vitamin C|C]], or [[folic acid]] have appeared to be related to a reduced risk of AD,<ref>Vitamins: | ||
| | * {{cite journal | ||
| | |author=Morris MC, Schneider JA, Tangney CC | ||
|title=Thoughts on B-vitamins and dementia | |||
| | |journal=J. Alzheimers Dis. | ||
| | |volume=9 | ||
| | |issue=4 | ||
| | |pages=429–33 | ||
}}</ref><ref>{{cite | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
}}</ref> | |||
[[ | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2006 | |year=2006 | ||
|pmid= | |pmid=16917152 | ||
|doi= | |doi= | ||
}} | }} | ||
|url=http://www. | * {{cite web | ||
| | |url=http://www.alz.org/alzheimers_disease_10428.asp | ||
| | |author=Alzheimer's Association | ||
|title=Vitamin E | |||
}} | |||
}} | * {{cite journal | ||
|author= | |author=Landmark K | ||
|title= | |title=[Could intake of vitamins C and E inhibit development of Alzheimer dementia?] | ||
| | |language=Norwegian | ||
| | |journal=Tidsskr. Nor. Laegeforen. | ||
|volume=126 | |||
|issue=2 | |||
|pages=159–61 | |||
|year=2006 | |||
|pmid=16415937 | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year= | |||
|pmid= | |||
|doi= | |doi= | ||
}} | }} | ||
* {{cite journal | |||
|author=Luchsinger JA, Tang MX, Miller J, Green R, Mayeux R | |||
|author= | |title=Relation of higher folate intake to lower risk of Alzheimer disease in the elderly | ||
|title= | |journal=Arch. Neurol. | ||
|journal= | |volume=64 | ||
|volume= | |||
|issue=1 | |issue=1 | ||
|pages= | |pages=86–92 | ||
|year=2007 | |||
|pmid=17210813 | |||
|doi=10.1001/archneur.64.1.86 | |||
}}</ref> | |||
but other studies indicate that they do not have any significant effect on the onset or course of the disease, but may have important secondary effects in conjunction with other therapies.<ref>Vitamins only of secondary benefit: | |||
* {{cite journal | |||
|author=Morris MC, Evans DA, Schneider JA, Tangney CC, Bienias JL, Aggarwal NT | |||
|title=Dietary folate and vitamins B-12 and B-6 not associated with incident Alzheimer's disease | |||
|journal=J. Alzheimers Dis. | |||
|volume=9 | |||
|issue=4 | |||
|pages=435–43 | |||
|year=2006 | |year=2006 | ||
|pmid= | |pmid=16917153 | ||
|doi= | |doi= | ||
}} | }} | ||
|author= | * {{cite journal | ||
|title= | |author=Malouf M, Grimley EJ, Areosa SA | ||
|journal= | |title=Folic acid with or without vitamin B12 for cognition and dementia | ||
|volume= | |journal=Cochrane Database Syst Rev | ||
|volume= | |||
|issue=4 | |issue=4 | ||
|pages= | |pages=CD004514 | ||
|year= | |year=2003 | ||
|pmid= | |pmid=14584018 | ||
|doi=10. | |doi=10.1002/14651858.CD004514 | ||
}} | }} | ||
|author= | * {{cite journal | ||
|title= | |author=Sun Y, Lu CJ, Chien KL, Chen ST, Chen RC | ||
|journal= | |title=Efficacy of multivitamin supplementation containing vitamins B6 and B12 and folic acid as adjunctive treatment with a cholinesterase inhibitor in Alzheimer's disease: a 26-week, randomised, double-blind, placebo-controlled study in Taiwanese patients | ||
|volume= | |journal=Clin Ther | ||
|issue= | |volume=29 | ||
|pages= | |issue=10 | ||
|year= | |pages=2204–14 | ||
|pmid= | |year=2007 | ||
|doi=10. | |pmid=18042476 | ||
|doi=10.1016/j.clinthera.2007.10.012 | |||
}} | |||
* {{cite journal | |||
|author=Boothby LA, Doering PL | |||
|title=Vitamin C and vitamin E for Alzheimer's disease | |||
|journal=Ann Pharmacother | |||
|volume=39 | |||
|issue=12 | |||
|pages=2073–80 | |||
|year=2005 | |||
|pmid=16227450 | |||
|doi=10.1345/aph.1E495 | |||
}} | }} | ||
* {{cite journal | |||
|author=Gray SL, Anderson ML, Crane PK, Breitner JC, McCormick W, Bowen JD, Teri L, Larson E | |||
|author= | |title=Antioxidant vitamin supplement use and risk of dementia or Alzheimer's disease in older adults | ||
|title= | |journal=J Am Geriatr Soc | ||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2005 | |||
|pmid= | |||
|doi=10. | |||
}} | |||
|author= | |||
|title= | |||
|journal= | |||
|volume=56 | |volume=56 | ||
|issue= | |issue=2 | ||
|pages= | |pages=291–295 | ||
|year= | |year=2008 | ||
|pmid= | |pmid=18047492 | ||
|doi= | |doi=10.1111/j.1532-5415.2007.01531.x | ||
}}</ref> | }}</ref> [[Curcumin]] in curry has shown some effectiveness in preventing brain damage in [[mouse model]]s.<ref>Curcumin in diet: | ||
|author= | * {{cite journal | ||
|title= | |author=Garcia-Alloza M, Borrelli LA, Rozkalne A, Hyman BT, Bacskai BJ | ||
|journal= | |title=Curcumin labels amyloid pathology in vivo, disrupts existing plaques, and partially restores distorted neurites in an Alzheimer mouse model | ||
|volume= | |journal=Journal of Neurochemistry | ||
|issue= | |volume=102 | ||
|pages= | |issue=4 | ||
|pages=1095–1104 | |||
|year=2007 | |year=2007 | ||
|pmid= | |pmid=17472706 | ||
|doi=10. | |doi=10.1111/j.1471-4159.2007.04613.x | ||
}} | }} | ||
|author= | * {{cite journal | ||
|title= | |author=Lim GP, Chu T, Yang F, Beech W, Frautschy SA, Cole GM | ||
|journal= | |title=The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse | ||
|volume= | |journal=Journal of Neuroscience | ||
|issue= | |volume=21 | ||
|pages= | |issue=21 | ||
|year= | |pages=8370–8377 | ||
|pmid= | |year=2001 | ||
|doi= | |pmid=11606625 | ||
|doi= | |||
}}</ref> | }}</ref> | ||
Although cardiovascular risk factors, such as [[hypercholesterolemia]], [[hypertension]], [[diabetes]], and smoking, are associated with a higher risk of onset and course of AD,<ref name="pmid17483665">{{cite journal |author=Rosendorff C, Beeri MS, Silverman JM |title=Cardiovascular risk factors for Alzheimer's disease |journal=Am J Geriatr Cardiol |volume=16 |issue=3 |pages=143–9 |year=2007 |pmid=17483665 |doi=10.1111/j.1076-7460.2007.06696.x}}</ref><ref name="obesity">{{cite journal | |||
| | |author=Gustafson D, Rothenberg E, Blennow K, Steen B, Skoog I | ||
| | |title=An 18-year follow-up of overweight and risk of Alzheimer disease | ||
| title = | |journal=Arch. Intern. Med. | ||
| | |volume=163 | ||
| | |issue=13 | ||
| | |pages=1524–1528 | ||
| doi=10. | |year=2003 | ||
}}</ref> | |pmid=12860573 | ||
|doi=10.1001/archinte.163.13.1524 | |||
|author= | }}</ref> [[statins]], which are [[cholesterol]] lowering drugs, have not been effective in preventing or improving the course of the disease.<ref name="pmid17927279">{{cite journal |author=Reiss AB, Wirkowski E |title=Role of HMG-CoA reductase inhibitors in neurological disorders : progress to date |journal=Drugs |volume=67 |issue=15 |pages=2111–2120 |year=2007 |pmid=17927279 |doi=}}</ref><ref name="pmid17877925">{{cite journal |author=Kuller LH |title=Statins and dementia |journal=Current Atherosclerosis Reports |volume=9 |issue=2 |pages=154–161 |year=2007 |pmid=17877925 |doi=10.1007/s11883-007-0012-9 }}</ref> However long-term usage of [[non-steroidal anti-inflammatory drug]] (NSAIDs), is associated with a reduced likelihood of developing AD in some individuals.<ref name="pmid18003940"> | ||
|title= | {{cite journal | ||
|journal= | |author=Szekely CA, Breitner JC, Fitzpatrick AL, Rea TD, Psaty BM, Kuller LH, Zandi PP | ||
|volume= | |title=NSAID use and dementia risk in the Cardiovascular Health Study: role of APOE and NSAID type | ||
|issue= | |journal=Neurology | ||
|pages= | |volume=70 | ||
|year= | |issue=1 | ||
|pmid= | |pages=17–24 | ||
|doi=10. | |year=2008 | ||
}}</ref> | |pmid=18003940 | ||
|doi=10.1212/01.wnl.0000284596.95156.48 | |||
|author= | }}</ref><ref> | ||
|title= | {{cite news | ||
|journal= | |title=Long-term use of ibuprofen may reduce the risk of developing Alzheimer's disease, a large US study reports. | ||
|volume= | |publisher=BBC | ||
|issue= | |date=2008-05-05 | ||
|pages= | |url=http://news.bbc.co.uk/1/hi/health/7380064.stm | ||
|year= | }}</ref><ref> | ||
|pmid= | {{cite news | ||
|doi=10.1080/ | |title=Ibuprofen Linked to Reduced Alzheimer's Risk | ||
}}</ref><ref name=" | |publisher=Washington Post | ||
|author= | |date=2008-05-05 | ||
|title= | |url=http://www.washingtonpost.com/wp-dyn/content/article/2008/05/05/AR2008050501839.html | ||
|journal= | }}</ref> | ||
|volume= | |||
|issue= | Other pharmaceutical therapies such as female [[hormone replacement therapy]] are no longer thought to prevent dementia,<ref name="pmid17882683">{{cite journal |author=Craig MC, Murphy DG |title=Estrogen: effects on normal brain function and neuropsychiatric disorders |journal=Climacteric |volume=10 Suppl 2 |issue= |pages=97–104 |year=2007 |pmid=17882683 |doi=10.1080/13697130701598746}}</ref><ref name="pmid17767023">{{cite journal |author=Mori K, Takeda M |title=Hormone replacement Up-to-date. Hormone replacement therapy and brain function|language=Japanese |journal=Clin Calcium |volume=17 |issue=9 |pages=1349–1354 |year=2007 |pmid=17767023 |doi=CliCa070913491354}}</ref> and a 2007 [[systematic review]] concluded that there was inconsistent and unconvincing evidence that [[Ginkgo Biloba|ginkgo]] has any positive effect on dementia or cognitive impairment.<ref>{{cite journal | ||
|pages= | |author=Birks J, Grimley Evans J | ||
|year= | |title=Ginkgo biloba for cognitive impairment and dementia | ||
|pmid= | |||
|doi= | |||
}}</ref> | |||
|author= | |||
|title= | |||
|journal=Cochrane Database Syst Rev | |journal=Cochrane Database Syst Rev | ||
|volume= | |volume= | ||
|issue= | |issue=2 | ||
|pages= | |pages=CD003120 | ||
|year= | |year=2007 | ||
|pmid= | |pmid=17443523 | ||
|doi=10.1002/14651858. | |doi=10.1002/14651858.CD003120.pub2 | ||
}}</ref><ref name=" | |url= http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD003120/frame.html | ||
|author= | |accessdate=2008-02-22 | ||
|title= | }}</ref> | ||
|journal= | |||
|volume= | Intellectual activities such as playing chess, completing crossword puzzles or regular social interaction, may also delay the onset or reduce the severity of Alzheimer's disease.<ref>{{cite journal | author=Verghese J, Lipton R, Katz M, Hall C, Derby C, Kuslansky G, Ambrose A, Sliwinski M, Buschke H | title=Leisure activities and the risk of dementia in the elderly. |journal=N Engl J Med | volume=348 | issue=25 | pages=2508–2516 | year=2003 | pmid=12815136 |doi=10.1056/NEJMoa022252 }}</ref><ref name="pmid16632311">{{cite journal | ||
|issue= | |author=Bennett DA, Schneider JA, Tang Y, Arnold SE, Wilson RS | ||
|pages= | |title=The effect of social networks on the relation between Alzheimer's disease pathology and level of cognitive function in old people: a longitudinal cohort study | ||
|year= | |journal=Lancet Neurol | ||
|pmid= | |volume=5 | ||
|doi=10. | |issue=5 | ||
}}</ref> | |pages=406–412 | ||
|year=2006 | |||
|pmid=16632311 | |||
|doi=10.1016/S1474-4422(06)70417-3 | |||
}}</ref> Bilingualism is also related to a later onset of Alzheimer.<ref>{{cite journal | author=Bialystok E, Craik FIM, Freedman M |title=Bilingualism as a protection against the onset of symptoms of dementia|journal=Neuropsychologia |volume=42 |issue=2 |pages=459-464 |year=2007 |pmid= |doi=10.1016/j.neuropsychologia.2006.10.009}}</ref> | |||
==Management== | |||
There is no known cure for Alzheimer's disease. Available treatments offer relatively small symptomatic benefit but remain [[palliative care|palliative]] in nature. Current treatments can be divided into pharmaceutical, psychosocial and caregiving. | |||
===Pharmaceutical=== | |||
| | [[Image:Donepezil3d.png|right|thumb|220px|3d molecular spacefill of [[donepezil]], an [[acetylcholinesterase inhibitor]] used in the treatment of AD symptoms]] | ||
[[Image:Memantine.png|right|thumb|220px|Molecular structure of [[memantine]], a medication approved for advanced AD symptoms]] | |||
Four medications, to treat the cognitive manifestations of AD, are currently approved by regulatory agencies, including the U.S. [[Food and Drug Administration]] (FDA) and the [[European Medicines Agency]] (EMEA). Three are [[acetylcholinesterase inhibitor]]s and the other is [[memantine]], an [[NMDA receptor]] [[receptor antagonist|antagonist]]. No drug has an indication for delaying or halting the progression of the disease. | |||
Because reduction in the activity of the [[cholinergic]] neurons in the disease is well known,<ref name="pmid8534419">{{cite journal | |||
|author=Geula C, Mesulam MM | |||
|title=Cholinesterases and the pathology of Alzheimer disease | |||
|journal=Alzheimer Dis Assoc Disord | |||
|volume=9 Suppl 2 | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |issue= | ||
|pages= | |pages=23–8 | ||
|year= | |year=1995 | ||
|pmid= | |pmid=8534419 | ||
|doi= | |doi= | ||
}}</ref> | }}</ref> [[acetylcholinesterase inhibitor]]s are employed to reduce the rate at which [[acetylcholine]] (ACh) is broken down and so to increase the concentration of ACh in the brain, thereby combatting the loss of ACh caused by the death of the cholinergin neurons.<ref name="pmid11105732">{{cite journal | ||
| | |author=Stahl SM | ||
|title=The new cholinesterase inhibitors for Alzheimer's disease, Part 2: illustrating their mechanisms of action | |||
| title= | |journal=J Clin Psychiatry | ||
| | |volume=61 | ||
| | |issue=11 | ||
| | |pages=813-814 | ||
| doi= | |year=2000 | ||
}}</ref> | |pmid=11105732 | ||
|doi= | |||
}}</ref> Cholinesterase inhibitors currently approved include [[donepezil]] (brand name ''Aricept''),<ref>{{cite web | |||
| url=http://www. | |url=http://www.nlm.nih.gov/medlineplus/druginfo/medmaster/a697032.html | ||
|title=Donepezil | |||
| title = | |accessdate=2008-03-20 | ||
| | |date=2007-01-08 | ||
| date | |publisher= US National Library of Medicine (Medline) | ||
}}</ref> [[galantamine]] (''Razadyne''),<ref>{{cite web | |||
| | |url=http://www.nlm.nih.gov/medlineplus/druginfo/medmaster/a699058.html | ||
}}</ref> | |title=Galantamine | ||
|accessdate=2008-03-20 | |||
|date=2007-01-08 | |||
|publisher= US National Library of Medicine (Medline) | |||
}}</ref> and [[rivastigmine]] (branded as ''Exelon'',<ref>{{cite web | |||
|url=http://www.nlm.nih.gov/medlineplus/druginfo/medmaster/a602009.html | |||
| | |title=Rivastigmine | ||
|title= | |accessdate=2008-03-20 | ||
| | |date=2007-01-08 | ||
| | |publisher= US National Library of Medicine (Medline) | ||
| | }}</ref> and ''Exelon Patch''<ref>{{cite web | ||
| | |url=http://www.nlm.nih.gov/medlineplus/druginfo/medmaster/a607078.html | ||
| | |title=Rivastigmine Transdermal | ||
| | |accessdate=2008-03-20 | ||
| | |date=2007-01-08 | ||
| | |publisher= US National Library of Medicine (Medline) | ||
|url=http:// | }}</ref>). There is also evidence for the efficacy of these medications in mild to moderate Alzheimer’s disease,<ref name="pmid16437532">{{cite journal | ||
|accessdate=2008- | |author=Birks J | ||
}}</ref> | |title=Cholinesterase inhibitors for Alzheimer's disease | ||
{{cite | |journal=Cochrane Database Syst Rev | ||
| | |volume= | ||
|issue=1 | |||
| title = | |pages=CD005593 | ||
| | |year=2006 | ||
| | |pmid=16437532 | ||
| | |doi=10.1002/14651858.CD005593 | ||
| doi=10. | }}</ref> and some evidence for their use in the advanced stage. Only donepezil is approved for treatment of advanced AD dementia.<ref name="pmid16437430">{{cite journal | ||
}}</ref> | |author=Birks J, Harvey RJ | ||
|title=Donepezil for dementia due to Alzheimer's disease | |||
|journal=Cochrane Database Syst Rev | |||
{{cite | |volume= | ||
| | |issue=1 | ||
|title= | |pages=CD001190 | ||
| | |year=2006 | ||
| | |pmid=16437430 | ||
| | |doi=10.1002/14651858.CD001190.pub2 | ||
}}</ref><ref>{{cite journal | }}</ref> The use of these drugs in [[mild cognitive impairment]] has not shown any effect in a delay of the onset of AD.<ref name="pmid18044984">{{cite journal | ||
|author= | |author=Raschetti R, Albanese E, Vanacore N, Maggini M | ||
|title= | |title=Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials | ||
|journal= | |journal=PLoS Med | ||
|volume=4 | |volume=4 | ||
|issue= | |issue=11 | ||
|pages= | |pages=e338 | ||
|year= | |year=2007 | ||
|pmid= | |pmid=18044984 | ||
|doi=10. | |doi=10.1371/journal.pmed.0040338 | ||
}}</ref> | }}</ref> Most common [[side effect]]s include [[nausea]] and [[vomiting]], both of which are linked to cholinergic excess. These side effects arise in approximately ten to twenty percent of users and are mild to moderate in severity. Less common secondary effects include [[muscle cramp]]s; decreased [[heart rate]] ([[bradycardia]]), decreased [[appetite]] and weight, and increased [[gastric acid]].<ref>{{cite web | ||
{{cite | |url=http://www.aricept.com/content/pi.pdf | ||
|title=Aricept and Aricept ODT Product Insert | |||
|accessdate=2008-01-30 | |||
|format= PDF | |||
|publisher= Eisai and Pfizer | |||
}}</ref><ref>{{cite web | |||
|url=http://razadyneer.com/razadyneer/pages/pdf/razadyne_er.pdf | |||
|title=Razadyne ER U.S. Full Prescribing Information | |||
|accessdate=2008-02-19 | |||
|format=PDF | |||
}}</ref> | |publisher=Ortho-McNeil Neurologics | ||
}}</ref><ref>{{cite web | |||
|url=http://www.pharma.us.novartis.com/product/pi/pdf/exelonpatch.pdf | |||
|title=Exelon ER U.S. Prescribing Information | |||
|accessdate=2008-02-19 | |||
|format=PDF | |||
|publisher=Novartis Pharmaceuticals | |||
}}</ref><ref>{{cite web | |||
|url=http://www.fda.gov/cder/foi/label/2006/020823s016,021025s008lbl.pdf | |||
|title=Exelon U.S. Prescribing Information | |||
|accessdate=2008-02-21 | |||
|format= PDF | |||
|publisher=Novartis Pharmaceuticals | |||
}}</ref> | |||
[[Glutamate]] is a useful excitatory [[neurotransmitter]] of the nervous system, although excessive amounts in the [[brain]] can lead to [[cell]] death through a process called [[excitotoxicity]] which consists of the overstimulation of glutamate [[Receptor (biochemistry)|receptors]]. Excitotoxicity occurs not only in Alzheimer's disease, but also in other neurological diseases such as [[Parkinson's disease]] and [[multiple sclerosis]].<ref name="pmid16424917">{{cite journal | |||
|author=Lipton SA | |||
|title=Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond | |||
|journal=Nat Rev Drug Discov | |||
|volume=5 | |||
|issue=2 | |||
|pages=160–170 | |||
|year=2006 | |||
|pmid=16424917 | |||
|doi=10.1038/nrd1958 | |||
}}</ref> [[Memantine]] (brand names ''Akatinol'', ''Axura'', ''Ebixa''/''Abixa'', ''Memox'' and ''Namenda''),<ref>{{cite web | |||
|url=http://www.nlm.nih.gov/medlineplus/druginfo/medmaster/a604006.html | |||
|title=Memantine | |||
|accessdate=2008-03-22 | |||
|date=2004-01-04 | |||
|publisher= US National Library of Medicine (Medline) | |||
}}</ref> is a noncompetitive [[NMDA receptor]] [[Receptor antagonist|antagonist]] first used as an anti-[[influenza]] agent. It acts on the [[glutamatergic system]] by blocking NMDA glutamate receptors and inhibits their overstimulation by glutamate.<ref name="pmid16424917" /> Memantine has been shown to be moderately efficacious in the treatment of moderate to severe Alzheimer’s disease. Its effects in the initial stages are unknown.<ref name="pmid15495043">{{cite journal | |||
}}</ref> | |author=Areosa Sastre A, McShane R, Sherriff F | ||
|title=Memantine for dementia | |||
|journal=Cochrane Database Syst Rev | |||
|url=http:// | |volume= | ||
|title= | |issue=4 | ||
| | |pages=CD003154 | ||
| | |year=2004 | ||
|publisher= US National | |pmid=15495043 | ||
|doi=10.1002/14651858.CD003154.pub2 | |||
}}</ref> | }}</ref> Reported adverse events with memantine are infrequent and mild, including [[hallucination]]s, [[confusion]], [[dizziness]], [[headache]] and [[fatigue (medical)|fatigue]].<ref>{{cite web | ||
| | |url=http://www.frx.com/pi/namenda_pi.pdf | ||
|title= | |title=Namenda Prescribing Information | ||
| | |accessdate=2008-02-19 | ||
| | |format=PDF | ||
| | |publisher=Forest Pharmaceuticals | ||
| | }}</ref> Memantine used in combination with donepezil has been shown to be "of statistically significant but clinically marginal effectiveness".<ref name="pmid18316756">{{cite journal | ||
|author=Raina P, Santaguida P, Ismaila A, ''et al'' | |||
| | |title=Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline | ||
| | |journal=Annals of Internal Medicine | ||
| | |volume=148 | ||
|issue=5 | |||
|pages=379-397 | |||
|year=2008 | |||
}}</ref> | |pmid=18316756 | ||
|url = http:// | |||
|title = | |||
|accessdate=2008- | |||
| | |||
| | |||
}}</ref> | |||
{{cite journal | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year= | |||
|pmid= | |||
|doi= | |doi= | ||
}}</ref><ref>{{cite journal | }}</ref> | ||
|author= | |||
|title= | [[Neuroleptic]] [[anti-psychotic]] drugs commonly given to Alzheimer's patients with behavioural problems are modestly useful in reducing [[aggression]] and [[psychosis]], but are associated with serious adverse effects, such as [[cerebrovascular]] events, [[extra-pyramidal|movement difficulties]] or cognitive decline, that do not permit their routine use.<ref name="pmid16437455">{{cite journal | ||
|journal= | |author=Ballard C, Waite J | ||
|title=The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease | |||
|journal=Cochrane Database Syst Rev | |||
|volume= | |||
|issue=1 | |||
|pages=CD003476 | |||
|year=2006 | |||
|pmid=16437455 | |||
|doi=10.1002/14651858.CD003476.pub2 | |||
}}</ref><ref name="pmid18384230">{{cite journal | |||
|author=Ballard C, Lana MM, Theodoulou M, ''et al'' | |||
|title=A Randomised, Blinded, Placebo-Controlled Trial in Dementia Patients Continuing or Stopping Neuroleptics (The DART-AD Trial) | |||
|journal=PLoS Med. | |||
|volume=5 | |volume=5 | ||
|issue= | |issue=4 | ||
|pages= | |pages=e76 | ||
|year=2008 | |year=2008 | ||
|pmid= | |pmid=18384230 | ||
|doi=10. | |doi=10.1371/journal.pmed.0050076 | ||
}}</ref><ref>{{cite journal | }}</ref><ref name="pmid15687315">{{cite journal | ||
|author= | |author=Sink KM, Holden KF, Yaffe K | ||
|title= | |title=Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence | ||
|journal= | |journal=JAMA | ||
|volume= | |volume=293 | ||
|issue=5 | |issue=5 | ||
|pages= | |pages=596-608 | ||
|year= | |year=2005 | ||
|pmid= | |pmid=15687315 | ||
|doi=10. | |doi=10.1001/jama.293.5.596 | ||
}}</ref> | }}</ref> | ||
== | ===Psychosocial intervention=== | ||
[[Image:Snoezelruimte.JPG|righ|220px|thumb|A specifically designed room for sensory integration therapy, or snoezelen; an emotion-oriented psychosocial intervention for people with dementia]] | |||
[[Psychosocial]] interventions are used as an adjunct to pharmaceutical treatment and can be classified within behavior, emotion, cognition or stimulation oriented approaches. Research on efficacy is unavailable and rarely specific to the disease, focusing instead on dementia.<ref name="pracGuideAPA">{{cite web | |||
| url=http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=AlzPG101007 | |||
| format=PDF | |||
| title =Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias | |||
| publisher =[[American Psychiatric Association]] | |||
| date=October 2007 | |||
| accessdate=2007-12-28 | |||
| doi=10.1176/appi.books.9780890423967.152139 | |||
}}</ref> | |||
[[Behavior modification|Behavioral interventions]] attempt to identify and reduce the antecedents and consequences of problem behaviors. This approach has not shown success in the overall functioning of patients,<ref name="pmid16323385">{{cite journal | |||
|author=Bottino CM, Carvalho IA, Alvarez AM, ''et al'' | |||
|title=Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study | |||
|author= | |journal=Clin Rehabil | ||
|title= | |volume=19 | ||
|issue=8 | |||
|pages=861–869 | |||
|year=2005 | |||
|pmid=16323385 | |||
|doi=10.1191/0269215505cr911oa | |||
}}</ref> | |||
but can help to reduce some specific problem behaviors, such as [[Urinary incontinence|incontinence]].<ref name="pmid11342679">{{cite journal | |||
|author=Doody RS, Stevens JC, Beck C, ''et al'' | |||
|title=Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology | |||
|journal=Neurology | |journal=Neurology | ||
|volume= | |volume=56 | ||
|issue= | |issue=9 | ||
|pages= | |pages=1154–1166 | ||
|year= | |year=2001 | ||
|pmid=11342679 | |||
|pmid= | |doi= | ||
}}</ref> There is still a lack of high quality data on the effectiveness of these techniques in other behavior problems such as wandering.<ref name="pmid17253573">{{cite journal | |||
| | |author=Hermans DG, Htay UH, McShane R | ||
|title=Non-pharmacological interventions for wandering of people with dementia in the domestic setting | |||
|journal=Cochrane Database Syst Rev | |||
|volume= | |||
}}</ref> | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue=1 | |issue=1 | ||
|pages= | |pages=CD005994 | ||
|year= | |year=2007 | ||
| | |pmid=17253573 | ||
| | |doi=10.1002/14651858.CD005994.pub2 | ||
}}</ref> | }}</ref><ref name="pmid17096455">{{cite journal | ||
|author= | |author=Robinson L, Hutchings D, Dickinson HO, ''et al'' | ||
|title= | |title=Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review | ||
|journal= | |journal=Int J Geriatr Psychiatry | ||
|volume= | |volume=22 | ||
|issue= | |issue=1 | ||
|pages= | |pages=9–22 | ||
|year= | |year=2007 | ||
|pmid=17096455 | |||
|pmid= | |doi=10.1002/gps.1643 | ||
|doi=10. | |||
}}</ref> | }}</ref> | ||
Emotion-oriented interventions include [[reminiscence therapy]], [[validation therapy]], supportive [[psychotherapy]], sensory integration or [[snoezelen]], and [[simulated presence therapy]]. Supportive psychotherapy has received little or no formal scientific study, but some clinicians find it useful in helping mildly impaired patients adjust to their illness.<ref name="pracGuideAPA">{{{{cite web | |||
| url=http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=AlzPG101007 | |||
| format=PDF | |||
| title =Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias | |||
| publisher =[[American Psychiatric Association]] | |||
| date=October 2007 | |||
| accessdate=2007-12-28 | |||
| | | doi=10.1176/appi.books.9780890423967.152139 | ||
}}</ref> | |||
| | Reminiscence therapy (RT) involves the discussion of past experiences individually or in group, many times with the aid of photographs, household items, music and sound recordings, or other familiar items from the past. Although there are few quality studies on the effectiveness of RT it may be beneficial for [[cognition]] and [[Mood (psychology)|mood]].<ref name="pmid15846613">{{cite journal | ||
|author=Woods B, Spector A, Jones C, Orrell M, Davies S | |||
|title=Reminiscence therapy for dementia | |||
|journal=Cochrane Database Syst Rev | |||
|volume= | |||
|issue=2 | |||
|pages=CD001120 | |||
|year=2005 | |||
|pmid=15846613 | |||
|doi=10.1002/14651858.CD001120.pub2 | |||
Alzheimer's disease | |||
}} | |||
</ref> <ref> | |||
{{cite journal | |||
}}</ref> | }}</ref> | ||
Simulated presence therapy (SPT) is based on [[Attachment theory|attachment theories]] and is normally carried out playing a recording with voices of the closest relatives of the patient. There is preliminary evidence indicating that SPT may reduce [[anxiety]] and [[Challenging behaviour|challenging behaviors]].<ref name="pmid11827626">{{cite journal | |||
|author=Peak JS, Cheston RI | |||
{{cite | |title=Using simulated presence therapy with people with dementia | ||
|journal=Aging Ment Health | |||
|volume=6 | |||
|issue=1 | |||
|pages=77–81 | |||
}}</ref> | |year=2002 | ||
|author= | |pmid=11827626 | ||
|title= | |doi=10.1080/13607860120101095 | ||
|journal= | }}</ref><ref name="pmid10203120">{{cite journal | ||
|volume= | |author=Camberg L, Woods P, Ooi WL, ''et al'' | ||
|issue= | |title=Evaluation of Simulated Presence: a personalised approach to enhance well-being in persons with Alzheimer's disease | ||
|pages= | |journal=J Am Geriatr Soc | ||
|volume=47 | |||
|issue=4 | |||
|pages=446-452 | |||
|year=1999 | |year=1999 | ||
|pmid= | |pmid=10203120 | ||
|doi= | |doi= | ||
}}</ref> | |||
Finally, validation therapy is based on acceptance of the reality and personal truth of another's experience, while sensory integration is based on exercises aimed to stimulate [[sense]]s. There is little evidence to support the usefulness of these therapies.<ref name="pmid12917907">{{cite journal | |||
|author=Neal M, Briggs M | |||
|title=Validation therapy for dementia | |||
|journal=Cochrane Database Syst Rev | |||
|volume= | |||
|issue=3 | |||
|pages=CD001394 | |||
|year=2003 | |||
|pmid=12917907 | |||
|doi=10.1002/14651858.CD001394 | |||
}}</ref><ref name="pmid12519587">{{cite journal | |||
|author=Chung JC, Lai CK, Chung PM, French HP | |||
|title=Snoezelen for dementia | |||
|journal=Cochrane Database Syst Rev | |||
|volume= | |||
|issue=4 | |||
|pages=CD003152 | |||
|year=2002 | |||
|pmid=12519587 | |||
|doi=10.1002/14651858.CD003152 | |||
}}</ref> | }}</ref> | ||
The aim of cognition-oriented treatments, which include reality orientation and [[Rehabilitation (neuropsychology)|cognitive retraining]] is the restoration of [[cognitive deficit]]s. Reality orientation consists in the presentation of information about time, place or person in order to ease the understanding of the person about its surroundings and his place in them. On the other hand cognitive retraining tries to improve impaired capacities by exercitation of mental abilities. Both have shown some efficacy improving cognitive capacities,<ref name="pmid17636652">{{cite journal | |||
|author=Spector A, Orrell M, Davies S, Woods B | |||
|title=WITHDRAWN: Reality orientation for dementia | |||
|journal=Cochrane Database Syst Rev | |||
|volume= | |||
|issue=3 | |||
|pages=CD001119 | |||
|year=2000 | |||
|pmid=17636652 | |||
|doi=10.1002/14651858.CD001119.pub2 | |||
}}</ref><ref name="pmid12948999">{{cite journal | |||
|author=Spector A, Thorgrimsen L, Woods B, ''et al'' | |||
}}</ref><ref>{{cite journal | |title=Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial | ||
|journal=Br J Psychiatry | |||
|volume=183 | |||
|issue= | |||
|pages=248–254 | |||
|year=2003 | |||
|pmid=12948999 | |||
|doi=10.1192/bjp.183.3.248 | |||
}}</ref> although in some works these effects were transient and negative effects, such as frustration, have also been reported.<ref name="pracGuideAPA">{{{{cite web | |||
| url=http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=AlzPG101007 | |||
}}</ref> | | format=PDF | ||
| title=Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias | |||
| publisher=[[American Psychiatric Association]] | |||
| date=October 2007 | |||
| accessdate=2007-12-28 | |||
| doi=10.1176/appi.books.9780890423967.152139 | |||
}}</ref> | |||
Stimulation-oriented treatments include [[Art therapy|art]], [[Music therapy|music]] and [[Animal-assisted therapy|pet]] therapies, [[Physical therapy|exercise]], and any other kind of [[Recreational therapy|recreational activities]] for patients. Stimulation has modest support for improving behavior, mood, and, to a lesser extent, function. Nevertheless, as important as these effects are, the main support for the use of stimulation therapies is the improvement in the patient daily life routine they suppose.<ref name="pracGuideAPA">{{cite web | |||
| url=http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=AlzPG101007 | |||
| format=PDF | |||
}}</ref> | | title =Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias | ||
| publisher =[[American Psychiatric Association]] | |||
| date=October 2007 | |||
| accessdate=2007-12-28 | |||
| doi=10.1176/appi.books.9780890423967.152139 | |||
}}</ref> | }}</ref> | ||
===Caregiving=== | |||
{{Further|[[Caregiving and dementia]]}} | |||
Since there is no cure for Alzheimer's, caregiving is an essential part of the treatment. Due to the eventual inability for the sufferer to self-care, Alzheimer's has to be carefully care-managed. Home care in the familiar surroundings of home may delay onset of some symptoms and delay or eliminate the need for more professional and costly levels of care.<ref>{{cite journal | |||
|author= | |author=Gaugler JE, Kane RL, Kane RA, Newcomer R | ||
|title= | |title=Early community-based service utilization and its effects on institutionalization in dementia caregiving | ||
|journal= | |journal=Gerontologist | ||
|volume= | |volume=45 | ||
|issue= | |issue=2 | ||
|pages= | |pages=177–85 | ||
|year= | |year=2005 | ||
|month= | |month=April | ||
|pmid= | |pmid=15799982 | ||
|doi= | |doi= | ||
|url=http://gerontologist.gerontologyjournals.org/cgi/pmidlookup?view=long&pmid=15799982 | |||
|accessdate=2008-05-30 | |||
| | }}</ref> Many family members choose to look after their relative,<ref name="burden1"/> but two-thirds of nursing home residents have dementias.<ref> | ||
{{cite web | |||
| url=http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=AlzPG101007 | |||
| format=PDF | |||
| title =Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias | |||
| publisher =[[American Psychiatric Association]] | |||
| date=October 2007 | |||
| accessdate=2007-12-28 | |||
}}</ref> | | doi=10.1176/appi.books.9780890423967.152139 | ||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
}}</ref> | }}</ref> | ||
Modifications to the living environment and lifestyle of the Alzheimer's patient can improve functional performance and ease caretaker burden. Assessment by an [[occupational therapist]] is often indicated. Adherence to simplified routines and labeling of household items to cue the patient can aid with [[activities of daily living]], while placing safety locks on cabinets, doors, and gates and securing hazardous chemicals can prevent accidents and wandering. Changes in routine or environment can trigger or exacerbate agitation, whereas well-lit rooms, adequate rest, and avoidance of excess stimulation all help prevent such episodes.<ref> | |||
{{cite web | |||
| | |url=http://web.archive.org/web/20060925112503/http://www.alz.org/Health/Treating/agitation.asp | ||
|title= Treating behavioral and psychiatric symptoms | |||
|date=2006 | |||
|accessdate=2006-09-25 | |||
|publisher = Alzheimer's Association | |||
}}</ref><ref>{{cite journal | |||
|author=Wenger GC, Burholt V, Scott A | |||
|title=Dementia and help with household tasks: a comparison of cases and non-cases | |||
|journal=Health Place | |||
|volume=4 | |||
|issue=1 | |||
|pages=33–44 | |||
|year=1998 | |||
|pmid=10671009 | |||
|doi=10.1016/S1353-8292(97)00024-5 | |||
}}</ref> Appropriate social and visual stimulation can improve function by increasing awareness and orientation. For instance, boldly colored tableware aids those with severe AD, helping people overcome a diminished sensitivity to visual contrast to increase food and beverage intake.<ref name="pmid15297089"> | |||
| | {{cite journal | ||
|accessdate= | | author = Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A | ||
}}</ref> | | title = Visual contrast enhances food and liquid intake in advanced Alzheimer's disease | ||
| | | journal = Clinical Nutrition | ||
| title = | | volume = 23 | ||
| | | issue = 4 | ||
| | | pages = 533–538 | ||
| | | year = 2004 | ||
| pages = | | pmid = 15297089 | ||
| | | doi = 10.1016/j.clnu.2003.09.015 | ||
| | }}</ref> | ||
|author= | |||
|title= | == Clinical research == | ||
|journal= | |||
|volume= | {{Main|Alzheimer's disease clinical research}} | ||
|issue= | |||
|pages= | As of 2008, the safety and efficacy of more than 400 pharmaceutical treatments are being investigated in [[clinical trial]]s worldwide, and approximately one-fourth of these compounds are in [[Phase III]] trials, which is the last step prior to review by regulatory agencies.<ref>{{cite web | ||
|year= | |url=http://www.clinicaltrials.gov/ct2/results?term=alzheimer | ||
|title= Clinical Trials. Found 459 studies with search of: alzheimer | |||
|pmid= | |accessdate= 2008-03-23 | ||
|doi=10.1016/ | |publisher= US National Institutes of Health | ||
|url=http://www. | }}</ref> It is unknown as to whether any of these trials will ultimately prove successful in treating the disease. | ||
|accessdate=2008- | |||
| | A critical area of clinical research is focused on treating the underlying disease pathology. Reduction of [[amyloid beta]] levels is a common target of compounds under investigation. [[Immunotherapy]] or [[vaccination]] for the amyloid protein is one treatment modality under study. Unlike vaccines which seek to prevent disease, this therapy would be used to treat diagnosed patients, and is based upon the concept of training the immune system to recognize, attack, and reverse deposition of amyloid, thereby altering the course of the disease.<ref>Vaccination: | ||
*{{cite journal | * {{cite journal |author=Hawkes CA, McLaurin J |title=Immunotherapy as treatment for Alzheimer's disease |journal=Expert Reviews of Neurotherapy |volume=7 |issue=11 |pages=1535–1548 |year=2007 |pmid=17997702 |doi=10.1586/14737175.7.11.1535 | ||
|author= | }} | ||
|title= | * {{cite journal |author=Solomon B |title=Clinical immunologic approaches for the treatment of Alzheimer's disease |journal=Expert Opin Investig Drugs |volume=16 |issue=6 |pages=819–828 |year=2007 |pmid=17501694 |doi=10.1517/13543784.16.6.819 | ||
|journal= | |||
|volume= | |||
|issue= | |||
|pages= | |||
|year=2007 | |||
| | |||
|doi=10. | |||
| | |||
}} | }} | ||
*{{cite | * {{cite journal |author=Woodhouse A, Dickson TC, Vickers JC |title=Vaccination strategies for Alzheimer's disease: A new hope? |journal=Drugs Aging |volume=24 |issue=2 |pages=107–119 |year=2007 |pmid=17313199 |doi=10.2165/00002512-200724020-00003 | ||
|url=http:// | }}</ref> An example of such a vaccine under investigation is ACC-001.<ref>{{cite web |url=http://www.clinicaltrials.gov/ct/show/NCT00498602 |title = Study Evaluating ACC-001 in Mild to Moderate Alzheimers Disease Subjects |work = Clinical Trial |publisher = [FDA clinicaltrials.gov] |date = 2008-03-11}}</ref><ref>{{cite web | ||
| | |url=http://clinicaltrials.gov/ct2/show/NCT00479557 |title=Study Evaluating Safety, Tolerability, and Immunogenicity of ACC-001 in Subjects With Alzheimer's Disease | ||
| | }}</ref> Similar agents are [[bapineuzumab]], an antibody designed as identical to the naturally-induced anti-amyloid antibody,<ref>{{cite web | ||
| | |url=http://clinicaltrials.gov/ct2/show/NCT00574132 | ||
|title= | |title= Bapineuzumab in Patients With Mild to Moderate Alzheimer's Disease/ Apo_e4 non-carriers | ||
|work = Clinical Trial | |||
| | |accessdate=2008-03-23 | ||
|publisher= US National Institutes of Health | |||
|date= 2008-02-29 | |||
== | }}</ref> and [[Tarenflurbil|MPC-7869]], a selective amyloid beta-42 lowering agent.<ref>{{cite web | ||
|url = http://clinicaltrials.gov/ct2/show/NCT00105547 | |||
|title= Efficacy Study of MPC-7869 to Treat Patients With Alzheimer's | |||
| | |work = Clinical Trial | ||
|title= | |accessdate=2008-03-23 | ||
| | |publisher= US National Institutes of Health | ||
| | |date = 2007-12-11 | ||
| | }}</ref> Other approaches are neuroprotective agents, such as AL-108,<ref>{{cite web | ||
| | |url = http://clinicaltrials.gov/ct2/show/NCT00422981 | ||
| | |title = Safety, Tolerability and Efficacy Study to Evaluate Subjects With Mild Cognitive Impairment | ||
| | |work = Clinical Trial | ||
| | |accessdate=2008-03-23 | ||
}}</ref> | |publisher= US National Institutes of Health | ||
|date = 2008-03-11 | |||
cite | }}</ref> metal-protein interaction attenuation agents, such as PBT2,<ref>{{cite web | ||
| | |url = http://clinicaltrials.gov/ct2/show/NCT00471211 | ||
| title= | |title = Study Evaluating the Safety, Tolerability and Efficacy of PBT2 in Patients With Early Alzheimer's Disease | ||
| | |work = Clinical Trial | ||
| | |accessdate=2008-03-23 | ||
| | |publisher= US National Institutes of Health | ||
| | |date = 2008-01-13 | ||
}}</ref> or [[tumor necrosis factor-alpha]] [[receptor]] fusion proteins, such as [[etanercept]].<ref name="pmid16926764"> | |||
{{cite journal | |||
}} | |author=Tobinick E, Gross H, Weinberger A, Cohen H | ||
|title=TNF-alpha modulation for treatment of Alzheimer's disease: a 6-month pilot study | |||
|author= | |journal=MedGenMed | ||
|volume=8 | |||
|title= | |issue=2 | ||
|journal= | |pages=25 | ||
|volume= | |year=2006 | ||
|issue= | |pmid=16926764 | ||
|pages= | |||
|year= | |||
|pmid= | |||
|doi= | |doi= | ||
}}</ref><ref>{{cite journal | |||
}} | |author=Griffin WS | ||
|title=Perispinal etanercept: potential as an Alzheimer therapeutic | |||
|author= | |journal=J Neuroinflammation | ||
|title=Alzheimer | |volume=5 | ||
| | |issue= | ||
| | |pages=3 | ||
| | |year=2008 | ||
|pages= | |pmid=18186919 | ||
| | |doi=10.1186/1742-2094-5-3 | ||
| | }}</ref><ref>{{cite journal | ||
|doi= | |author=Tobinick E | ||
|title=Perispinal etanercept for treatment of Alzheimer's disease | |||
|journal=Curr Alzheimer Res | |||
|volume=4 | |||
|issue=5 | |||
|pages=550-552 | |||
|year=2007 | |||
|pmid=18220520 | |||
|doi=10.2174/156720507783018217 | |||
}}</ref> There are also many basic investigations attempting to increase the knowledge on the origin and mechanisms of the disease that may lead to new treatments. | |||
==Prognosis== | |||
}}</ref> | |||
|author= | The early stages of Alzheimer's disease are difficult to diagnose. A definitive diagnosis is usually made once cognitive impairment compromises daily living activities, although the person may still be living independently. He will progress from mild cognitive problems, such as memory loss through increasing stages of cognitive and non-cognitive disturbances, eliminating any possibility of independent living.<ref name="pmid10653284" /> | ||
|title= | |||
|journal= | [[Life expectancy]] of the population with the disease is reduced.<ref name="pmid3776457"/><ref name="pmid8757016">{{cite journal | ||
|volume= | |author=Bowen JD, Malter AD, Sheppard L, ''et al'' | ||
|issue= | |title=Predictors of mortality in patients diagnosed with probable Alzheimer's disease | ||
|pages= | |journal=Neurology | ||
|year= | |volume=47 | ||
|pmid= | |issue=2 | ||
|doi=10. | |pages=433–9 | ||
}}</ref> | |year=1996 | ||
|author= | |month=August | ||
|title= | |pmid=8757016 | ||
| | }}</ref><ref name="pmid12580712">{{cite journal | ||
| | |author=Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M | ||
| | |title=Functional transitions and active life expectancy associated with Alzheimer disease | ||
|pages= | |journal=Arch. Neurol. | ||
| | |volume=60 | ||
| | |||
| | |||
}}</ref> | |||
|author= | |||
|title= | |||
|journal= | |||
|volume= | |||
|issue=2 | |issue=2 | ||
|pages= | |pages=253–9 | ||
|year= | |year=2003 | ||
|pmid= | |month=February | ||
| | |pmid=12580712 | ||
|author= | }}</ref> The mean life expectancy following diagnosis is approximately seven years.<ref name="pmid3776457"/> Fewer than 3% of patients live more than fourteen years.<ref name="pmid7793228"/> Disease features significantly associated with reduced survival are an increased severity of cognitive impairment, decreased functional level, history of falls, and disturbances in the neurological examination. Other coincident diseases such as [[Heart disease|heart problems]], [[Diabetes mellitus|diabetes]] or history of [[alcohol abuse]] are also related with shortened survival.<ref name="pmid8757016"/><ref name="pmid15068977">{{cite journal | ||
|title=Alzheimer's disease: | |author=Larson EB, Shadlen MF, Wang L, ''et al'' | ||
| | |title=Survival after initial diagnosis of Alzheimer disease | ||
| | |journal=Ann. Intern. Med. | ||
| | |volume=140 | ||
|pages= | |issue=7 | ||
| | |pages=501–9 | ||
| | |year=2004 | ||
| | |month=April | ||
}}</ref> | |pmid=15068977 | ||
|author= | }}</ref><ref name="pmid7792352">{{cite journal | ||
|title= | |author=Jagger C, Clarke M, Stone A | ||
|journal= | |title=Predictors of survival with Alzheimer's disease: a community-based study | ||
|volume= | |journal=Psychol Med | ||
|issue= | |volume=25 | ||
|pages= | |issue=1 | ||
|year= | |pages=171–7 | ||
|pmid= | |year=1995 | ||
|doi= | |month=January | ||
|pmid=7792352 | |||
}}</ref> While the earlier the age at onset the higher the total survival years, life expectancy is particularly reduced when compared to the healthy population among those who are younger.<ref name="pmid12580712"/> Men have a less favourable survival prognosis than women.<ref name="pmid7793228"/><ref name="pmid15883266">{{cite journal | |||
|author=Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST | |||
|title=Alzheimer disease and mortality: a 15-year epidemiological study | |||
|journal=Arch. Neurol. | |||
|volume=62 | |||
|issue=5 | |||
|pages=779–84 | |||
|year=2005 | |||
|month=May | |||
|pmid=15883266 | |||
|doi=10.1001/archneur.62.5.779 | |||
}}</ref> | }}</ref> | ||
The disease is the underlying cause of death in 70% of all cases.<ref name="pmid3776457"/> [[Pneumonia]] and [[dehydration]] are the most frequent immediate causes of death, while [[cancer]] is a less frequent cause of death than in the general population.<ref name="pmid3776457"/><ref name="pmid15883266"/> | |||
==Society and culture== | ==Society and culture== | ||
===Social costs=== | ===Social costs=== | ||
Revision as of 01:29, 2 December 2009
Template:DiseaseDisorder infobox
Editor-in-Chief: Peter Pressman, M.D. [1], Northwestern Memorial Hospital, Department of Neurology
Dr. Pressman has nothing to disclose.
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Alzheimer's disease (AD), also called Alzheimer disease, Senile Dementia of the Alzheimer Type (SDAT) or simply Alzheimer's, is the most common form of dementia. This incurable, degenerative, and terminal disease was first described by German psychiatrist Alois Alzheimer in 1906. Generally it is diagnosed in people over 65 years of age,[1] although the less-prevalent early-onset Alzheimer's can occur much earlier. An estimated 26.6 million people worldwide had Alzheimer's in 2006; this number may quadruple by 2050.[2]
Although each sufferer experiences Alzheimer's in a unique way, there are many common symptoms.[3] The earliest observable symptoms are often mistakenly thought to be 'age-related' changes, or manifestations of stress.[4] The most commonly recognised symptom of early Alzheimer's disease is memory loss, usually the forgetting of recently learned facts. As the disease advances, symptoms include confusion, irritability and aggression, mood swings, language breakdown, long-term memory loss, and the general withdrawal of the sufferer as their senses decline.[4][5] Gradually, bodily functions are lost, ultimately leading to death.[6] When a doctor or physician has been notified, and AD is suspected, the diagnosis is usually confirmed with behavioural assessments and cognitive tests, often followed by a brain scan if available.[7] Individual prognosis is difficult to assess, as the duration of the disease varies. AD develops for an indeterminate period of time before becoming fully apparent, and it can progress undiagnosed for years. The mean life expectancy following diagnosis is approximately seven years.[8] Fewer than three percent of individuals live more than fourteen years after diagnosis.[9]
The cause of Alzheimer's disease is poorly understood. Research indicates that the disease is associated with plaques and tangles in the brain.[10] Currently-used treatments offer a small symptomatic benefit. No treatments to halt the progression of the disease are yet available. As of 2008, more than 500 clinical trials were investigating possible treatments for AD, but it is unknown if any of them will prove successful.[11] Many measures have been suggested for the prevention of Alzheimer's disease, but the value of these measures is unproven in slowing the course and reducing the severity of the disease. Mental stimulation, exercise, and a balanced diet are often recommended as both a possible prevention and a sensible way of managing the disease.[12]
Because AD cannot be cured, management of patients is essential as the disease progresses. The role of the main caregiver is often taken by a spouse or a close relative.[13] Alzheimer's disease is known for placing a great burden on caregivers; the pressures can be wide-ranging, affecting social, psychological, physical, and economic components of the caregiver's life.[14][15][16] In developed countries, AD is one of the most economically costly diseases to society.[17][18]
History
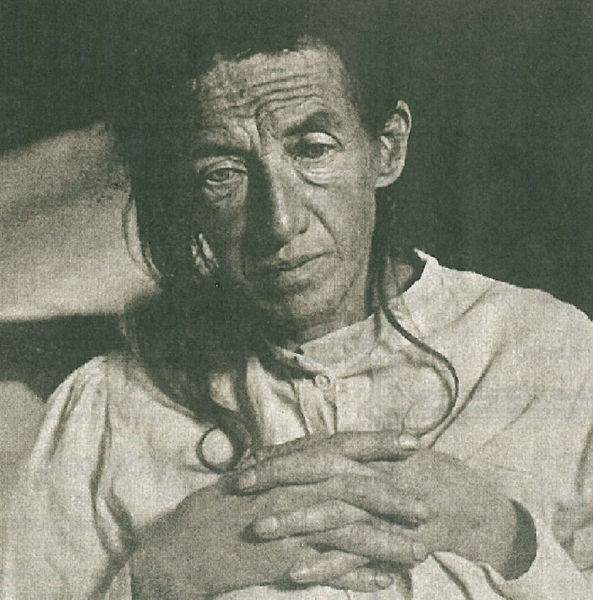
Although the concept of dementia goes as far back as the ancient Greek and Roman philosophers and physicians,[19] it was in 1901 when Alöis Alzheimer, a German psychiatrist, identified the first case of what became known as Alzheimer's disease in a fifty-year-old woman he called Auguste D. Alöis Alzheimer followed her until she died in 1906, when he first reported the case publicly.[20] In the following five years, eleven similar cases were reported in the medical literature, some of them already using the term Alzheimer's disease.[19] The official consideration of the disease as a distinctive entity is attributed to Emil Kraepelin, who included Alzheimer’s disease or presenile dementia as a subtype of senile dementia in the eighth edition of his Textbook of Psychiatry, published in 1910.[21]
For most of the twentieth century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45 and 65 who developed symptoms of dementia. The terminology changed after 1977 when a conference concluded that the clinical and pathological manifestations of presenile and senile dementia were almost identical, although the authors also added that this did not rule out the possibility of different etiologies. This eventually led to the use of Alzheimer's disease independently of onset age of the disease.[22][23] The term senile dementia of the Alzheimer type (SDAT) was used for a time to describe the condition in those over 65, with classical Alzheimer's disease being used for those younger. Eventually, the term Alzheimer's disease was formally adopted in medical nomenclature to describe individuals of all ages with a characteristic common symptom pattern, disease course, and neuropathology.[24]
Epidemiology
| Age | Incidence (new affected) per thousand person–years |
|---|---|
| 65–69 | 3 |
| 70–74 | 6 |
| 75–79 | 9 |
| 80–84 | 23 |
| 85–89 | 40 |
| 90– | 69 |
Alzheimer's disease is the most frequent type of dementia in the elderly and affects almost half of all patients with dementia. Correspondingly, advancing age is the primary risk factor for the disease. [26] [27]
The World Health Organization estimates that globally the total disability adjusted life years (DALY) for AD and other dementias exceeded eleven million in 2005, with a projected 3.4% annual increase.[28] A study in Denmark found that women aged 65 are at significantly higher risk (22 percent) of developing AD by age 95 than their male counterparts (nine percent), while vascular dementias were nearly equal.[29]
Some studies have shown a relationship between risk of developing AD and lifetime magnetic field exposure, although the mechanism is unknown.[30][31] Other research does not confirm this link.[32] The role of metals in the disease is also controversial.[33]
Two main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person–time at risk (usually number of new cases per thousand person–years); while prevalence is the total number of cases of the disease in the population at a given time.
Regarding incidence, cohort longitudinal studies (studies where a disease-free population is followed over the years) provide rates between 10–15 per thousand person–years for all dementias and 5–8 for AD,[25][34] which means that half of new dementia cases each year are AD. Advancing age is a primary risk factor for the disease and incidence rates are not equal for all ages: every five years after the age of 65, the risk of acquiring the disease approximately doubles, increasing from 3 to as much as 69 per thousand person years.[25][34] There are also sex differences in the incidence rates, women having a higher risk of developing AD particularly in the population older than 85.[34][35]
Prevalence of AD in populations is dependent upon different factors including incidence and survival. Since the incidence of AD increases with age, it is particularly important to include the mean age of the population of interest. In the United States, Alzheimer prevalence was estimated to be 1.6% in the year 2000 both overall and in the 65–74 age group, with the rate increasing to 19% in the 75–84 group and to 42% in the greater than 84 group.[36] Prevalence rates in less developed regions are lower.[37] The World Health Organization estimated that in 2005, 0.379% of people worldwide had dementia, and that the prevalence would increase to 0.441% in 2015 and to 0.556% in 2030.[38] Other studies have reached similar conclusions.[37] Another study estimated that in 2006, 0.40% of the world population (range 0.17–0.89%; absolute number 26.6 million, range 11.4–59.4 million) were afflicted by AD, and that the prevalence rate would triple and the absolute number would quadruple by the year 2050.[2]
Characteristics
The disease course is divided into four stages, with a progressive decline in cognition and functional capabilities.
Predementia
The first symptoms are commonly misattributed to normal ageing or stress.[4] Detailed neuropsychological testing can reveal mild cognitive difficulties up to eight years before a person meets the clinical criteria for diagnosis of AD.[39] These early symptoms can affect the most complex daily living activities.[40] The most noticeable early deficit is memory loss. The patient has difficulty remembering recently learned facts and acquiring new information.[41][42] Subtle problems with the executive functions of attentiveness, planning, flexibility, and abstract thinking, or impairments in semantic memory (memory of meanings, and conceptual relationships), can also be symptomatic of the early stages of AD.[43][44] Apathy can be observed at this stage, and remains the most persistent neuropsychiatric symptom throughout the course of the disease.[45][46][47] The preclinical stage of the disease has also been termed mild cognitive impairment,[48] but there is still debate on whether this term corresponds to a different and separate diagnostic entity or is just a first step of Alzheimer's disease.[49]
Early dementia
In people with AD the increasing impairment of learning and memory eventually leads to a definitive diagnosis. In a small proportion of them, difficulties with language, executive functions, perception (agnosia), or execution of movements (apraxia) are more prominent than memory problems.[50] AD does not affect all memory capacities equally. Older memories of the person's life (episodic memory), facts learned (semantic memory), and implicit memory (the memory of the body on how to do things, such as using a fork to eat) are less affected than new facts or memories.[51][52] Language problems include a shrinking vocabulary and decreased word fluency, which lead to a general impoverishment of oral and written language. In this stage, the person with Alzheimer's is usually capable of adequately communicating basic ideas.[53][54][55] While performing fine motor tasks such as writing, drawing or dressing, difficulty with planning and coordinating certain movements (apraxia) may be present, making sufferers appear clumsy.[56] As the disease progresses, people with AD can often continue to perform many tasks independently, but may need assistance or supervision with cognitively demanding activities.[50]
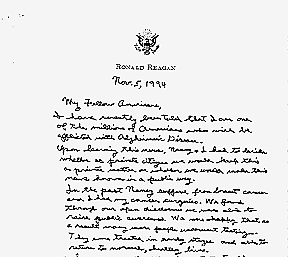
Moderate dementia
Progressive deterioration eventually hinders independence.[50] Speech difficulties become more evident, with an inability to recall vocabulary leading to frequent incorrect word substitutions (paraphasias). Reading and writing skills are also progressively lost.[53][57] Complex motor sequences become less coordinated as time passes, reducing the ability to perform most normal daily activities.[58] During this phase, memory problems worsen, and the person may fail to recognise close relatives.[59] Long-term memory, which was previously intact, becomes impaired,[60] and behavioural changes become more prevalent. Common neuropsychiatric manifestations are wandering, sundowning,[61] irritability and labile affect, leading to crying, outbursts of unpremeditated aggression, or resistance to caregiving. Approximately 30% of patients also develop illusionary misidentifications and other delusional symptoms.[45][62] Urinary incontinence can develop.[63] These symptoms create stress for relatives and caretakers, which can be reduced by moving the person from home care to a long-term care facility.[50][64]
Advanced dementia
During this last stage of AD, the patient is completely dependent upon caregivers. Language is reduced to simple phrases or even single words, eventually leading to complete loss of speech.[53]
Despite the loss of verbal language abilities, patients can often understand and return emotional signals.[65]
Although aggressiveness can still be present, extreme apathy and exhaustion are much more common.[50]
Patients will ultimately not be able to perform even the most simple tasks without assistance. Muscle mass and mobility deteriorate to the point where the patient is bedridden,[66] and they lose the ability to feed themselves.[67]
When death comes, it is usually directly caused by some external factor such as pressure ulcers or pneumonia, rather than the disease itself.[68][69]
Pathophysiology

At a macroscopic level, AD is characterised by loss of neurons and synapses in the cerebral cortex and certain subcortical regions. This results in gross atrophy of the affected regions, including degeneration in the temporal lobe and parietal lobe, and parts of the frontal cortex and cingulate gyrus.[70] Three major competing hypotheses exist to explain the cause of the disease. The oldest is the cholinergic hypothesis, which proposes that AD is caused by reduced synthesis of the neurotransmitter acetylcholine. Most currently available drug therapies in Alzheimer's are based on this theory, however, the medications that treat acetylcholine deficiency only affect symptoms of the disease and neither halt nor reverse it.[71] The cholinergic hypothesis has not maintained widespread support in the face of this evidence, although cholinergic effects have been proposed to initiate large-scale aggregation,[72] leading to generalised neuroinflammation.[70] In 1991 the amyloid hypothesis was proposed,[73] while research after 2000 is also centered on tau proteins. The two positions differ with one stating that the tau protein abnormalities initiate the disease cascade, while the other states that amyloid beta (Aβ) deposits are the causative factor in the disease.[74] The amyloid hypothesis postulates that amyloid beta (Aβ) deposits are the fundamental cause of the disease.[73][74]
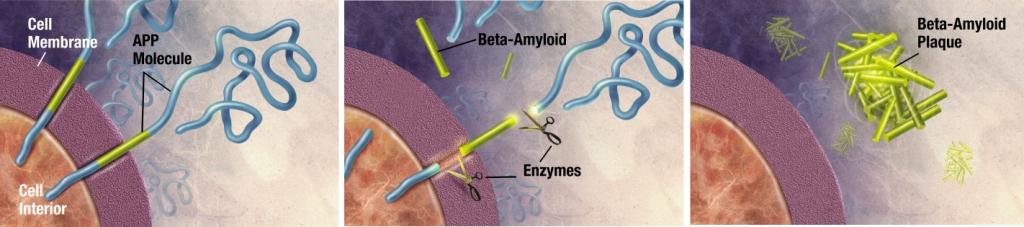
Alzheimer's disease has been identified as a protein misfolding disease, or proteopathy, due to the accumulation of abnormally folded A-beta and tau proteins in the brains of AD patients.[75] Plaques are made of a small peptide (39 to 43 amino acid residues) called beta-amyloid (also A-beta or Aβ), a protein fragment snipped from a larger protein called amyloid precursor protein (APP). APP is a transmembrane protein; which means that it sticks through the neuron's membrane; and is believed to help neurons grow, survive and repair themselves after injury.[76][77] In AD, something causes APP to be divided by enzymes through a mechanism called proteolysis.[78] One of these fragments is beta-amyloid. Beta-amyloid fragments (amyloid fibrils) outside the cell form clumps that deposit outside neurons in dense formations known as senile plaques.[79][10] The amyloid hypothesis is compelling because the gene for the amyloid beta precursor (APP) is located on chromosome 21, and patients with trisomy 21 (Down Syndrome) who thus have an extra gene copy almost universally exhibit AD-like disorders by 40 years of age.[80][81] It should be noted further that ApoE4, the major genetic risk factor for AD, leads to excess amyloid build-up in the brain before AD symptoms arise. Thus, Aβ deposition precedes clinical AD.[82] It is known that some types of inherited AD involve only mutations in the APP gene (although this is not the most common type—others involve genes for "pre-senilin" proteins which process APP and may also have still-unknown functions).[83] However, another strong support for the amyloid hypothesis, which looks at Aβ as the common initiating factor for Alzheimer's disease, is that transgenic mice solely expressing a mutant human APP gene develop fibrillar amyloid plaques.[84] If damage from Aβ is the primary initiating cause of AD, the exact mechanism has not been elucidated. The traditional formulation of the amyloid hypothesis points to the cytotoxicity of mature aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis and thus inducing apoptosis.[85] It is also known that Aβ selectively builds up in the mitochondria of samples from the brains of humans with AD, and in mitochondria from transgenic mice with APP genes, and in both cases inhibits certain mitochondrial enzyme functions, and a similar decrease in glucose utilization in neurons to the one which is a known characteristic of AD. This process may also lead to the formation of damaging reactive oxygen species, calcium influx, and apoptosis. Mechanisms which involve direct damage from Aβ before it forms fibrils and plaques also address the issue that neuronal damage is not correlated as well with plaques, since in this model it is not the plaques themselves which cause the major damage, but rather the precursor Aβ protein directly, via another mechanism.[86] Again, deposition of amyloid plaques does not correlate well with neuron loss.[87]
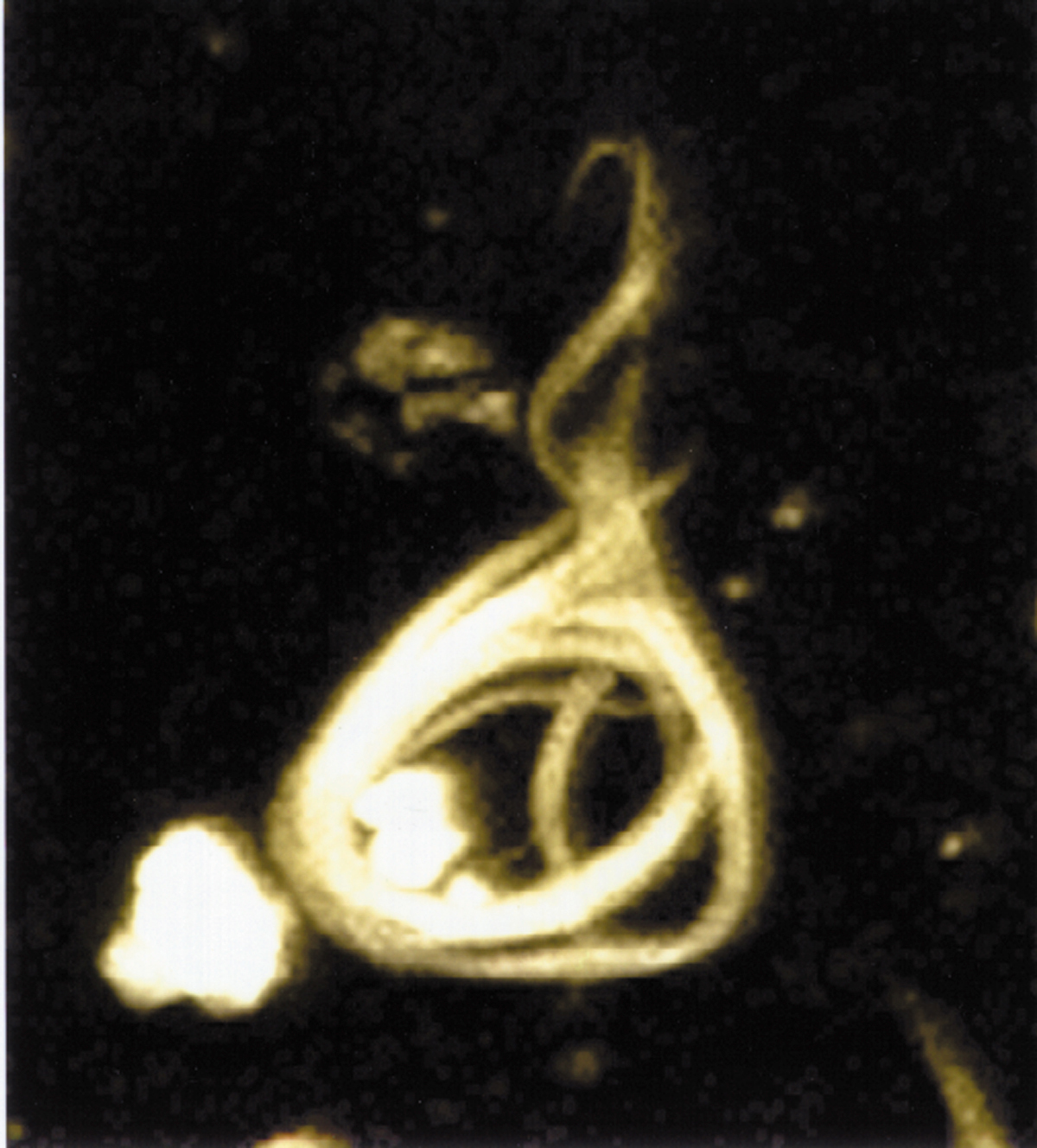
This observation supports the tau hypothesis, the idea that tau protein abnormalities initiate the disease cascade.[74] AD is also considered a tauopathy due to abnormal aggregation of the tau protein. Healthy neurons have an internal support structure, or cytoskeleton, partly made up of structures called microtubules. These microtubules act like tracks, guiding nutrients and molecules from the body of the cell down to the ends of the axon and back. A special kind of protein, tau, makes the microtubules stable through a process named phosphorylation and is therefore called a microtubule-associated protein.[88] In AD, tau is changed chemically, becoming hyperphosphorylated.
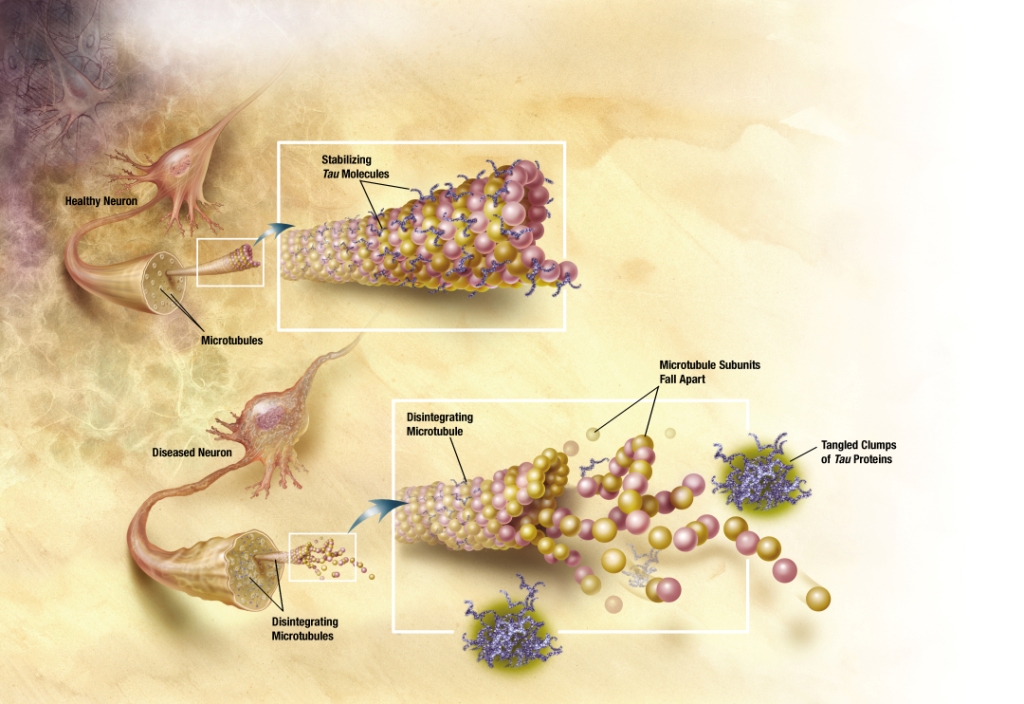
In the tau hypothesis, hyperphosphorylated tau begins to pair with other threads of tau and they become tangled up together inside nerve cell bodies in masses known as neurofibrillary tangles.[89] When this happens, the microtubules disintegrate, collapsing the neuron's transport system. This may result first in malfunctions in communication between neurons and later in the death of the cells.[90] Both amyloid plaques and neurofibrillary tangles are clearly visible by microscopy in AD brains.[10] Plaques are dense, mostly insoluble deposits of amyloid-beta protein and cellular material outside and around neurons. Tangles are insoluble twisted fibers that build up inside the nerve cell. Though many older people develop some plaques and tangles, the brains of AD patients have them to a much greater extent and in different brain locations.[91]
Recent research supports the previously obscure theory that Herpes simplex virus type 1 plays a role as a possible cause of AD in people carrying the susceptible versions of the apoE gene.[92] As HSV-1 is not a new virus, some additional factor is needed to explain the increase [3] in the age adjusted incidence of AD. Various inflammatory processes and inflammatory cytokines may also have a role in the pathology of Alzheimer's disease. However, these are general markers of tissue damage in any disease, and may also be either secondary causes of tissue damage in AD, or else bystander "marker" effects.[93] Other cholinergic effects have also been proposed, for example, initiation of large-scale aggregation of amyloid,[72] leading to generalised neuroinflammation.[70]
Diagnosis
Dementia is by definition a clinical condition but not an exact diagnosis. Alzheimer's disease is usually diagnosed clinically from the patient history, collateral history from relatives, and clinical observations, based on the presence of characteristic neurological and neuropsychological features and the absence of alternative conditions.[94][95] Advanced medical imaging with CT or MRI, and with SPECT or PET are generally used to help to diagnose the subtype of dementia and exclude other cerebral pathology.[96] Neuropsychological evaluation including memory testing and assessment of intellectual functioning can further characterize the dementia.[4] Medical organizations have created diagnostic criteria to ease and standardize the process for practicing physicians. Sometimes the diagnosis can be confirmed or made at postmortem when brain material is available and can be examined histologically and histochemically.[97]
Diagnostic criteria
The diagnostic criteria for Alzheimer of the NINCDS-ADRDA (National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association) are among the most used.[98] These criteria require that the presence of cognitive impairment and a suspected dementia syndrome be confirmed by neuropsychological testing for a clinical diagnosis of possible or probable AD while they need histopathologic confirmation (microscopic examination of brain tissue) for the definitive diagnosis. They have shown good reliability and validity.[99] They specify as well eight cognitive domains that may be impaired in AD (i.e., memory, language, perceptual skills, attention, constructive abilities, orientation, problem solving and functional abilities). Similar to the NINCDS-ADRDA Alzheimer's Criteria are the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria published by the American Psychiatric Association.[100][101]
Diagnostic tools
Neuropsychological screening tests as the Mini mental state examination (MMSE) are widely used to evaluate the cognitive impairments needed for diagnosis, but more comprehensive batteries are necessary for high reliability by this method, especially in the earliest stages of the disease.[102][103] On the other hand neurological examination in early AD will usually be normal, independent of cognitive impairment; but for many of the other dementing disorders is key for diagnosis. Therefore, neurological examination is crucial in the differential diagnosis of Alzheimer and other diseases.[4] In addition, interviews with family members are also utilised in the assessment of the disease. Caregivers can supply important information on the daily living abilities, as well as on the decrease over time of the patient's mental function.[104] This is especially important since a patient with AD is commonly unaware of his or her own deficits (anosognosia).[105] Many times families also have difficulties in the detection of initial dementia symptoms and in adequately communicating them to a physician.[106] Finally, supplemental testing provides extra information on some features of the disease or are used to rule out other diagnoses. Examples are blood tests, which can identify other causes for dementia different than AD,[4] which rarely may even be reversible;[107] or psychological tests for depression, as depression can both co-occur with AD or, on the contrary, be at the origin of the patient's cognitive impairment.[108][109]
Increasingly, the functional neuroimaging modalities of single photon emission computed tomography (SPECT) and positron emission tomography (PET) are being used to diagnose Alzheimer's, as they have shown similar ability to diagnose Alzheimer's disease as methods involving mental status examination.[110] Furthermore, the ability of SPECT to differentiate Alzheimer's disease from other possible causes, in a patient already known to be suffering from dementia, appears to be superior to attempts to differentiate the cause of dementia cause by mental testing and history.[111] A new technique known as "PiB PET" has been developed for directly and clearly imaging beta-amyloid deposits in vivo using a contrasting tracer that binds selectively to the Abeta deposits.[112][113][114] Another recent objective marker of the disease is the analysis of cerebrospinal fluid for amyloid beta or tau proteins.[115] Both advances (neuroimaging and cerebrospinal fluid analysis) have led to the proposal of new diagnostic criteria.[98][4]
Prevention

At present contradictory results in global studies, incapacity to prove causal relationships between risk factors and the disease, and possible secondary effects indicate a lack of specific measures to prevent or delay the onset of AD.[116] Different epidemiological studies have proposed relationships between certain modifiable factors, such as diet, cardiovascular risk, pharmaceutical products, or intellectual activities among others, and a population's likelihood of developing AD. Only further research, including clinical trials, will reveal whether, in fact, these factors can help to prevent AD.[117]
The components of a Mediterranean diet, which include fruit and vegetables, bread, wheat and other cereals, olive oil, fish, and red wine, may all individually or together reduce the risk and course of Alzheimer's disease. There is evidence that frequent and moderate consumption of alcohol (beer, wine or distilled spirits) reduces the risk of the disease,[118] [119] but it is still considered premature to make dietary recommendations on this basis.[120][121] Vitamins E, B, and C, or folic acid have appeared to be related to a reduced risk of AD,[122] but other studies indicate that they do not have any significant effect on the onset or course of the disease, but may have important secondary effects in conjunction with other therapies.[123] Curcumin in curry has shown some effectiveness in preventing brain damage in mouse models.[124]
Although cardiovascular risk factors, such as hypercholesterolemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and course of AD,[125][126] statins, which are cholesterol lowering drugs, have not been effective in preventing or improving the course of the disease.[127][128] However long-term usage of non-steroidal anti-inflammatory drug (NSAIDs), is associated with a reduced likelihood of developing AD in some individuals.[129][130][131]
Other pharmaceutical therapies such as female hormone replacement therapy are no longer thought to prevent dementia,[132][133] and a 2007 systematic review concluded that there was inconsistent and unconvincing evidence that ginkgo has any positive effect on dementia or cognitive impairment.[134]
Intellectual activities such as playing chess, completing crossword puzzles or regular social interaction, may also delay the onset or reduce the severity of Alzheimer's disease.[135][136] Bilingualism is also related to a later onset of Alzheimer.[137]
Management
There is no known cure for Alzheimer's disease. Available treatments offer relatively small symptomatic benefit but remain palliative in nature. Current treatments can be divided into pharmaceutical, psychosocial and caregiving.
Pharmaceutical
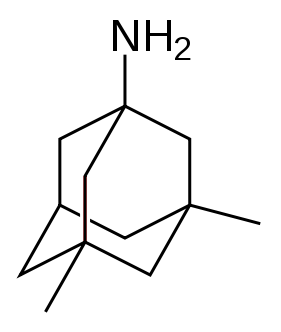
Four medications, to treat the cognitive manifestations of AD, are currently approved by regulatory agencies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMEA). Three are acetylcholinesterase inhibitors and the other is memantine, an NMDA receptor antagonist. No drug has an indication for delaying or halting the progression of the disease.
Because reduction in the activity of the cholinergic neurons in the disease is well known,[138] acetylcholinesterase inhibitors are employed to reduce the rate at which acetylcholine (ACh) is broken down and so to increase the concentration of ACh in the brain, thereby combatting the loss of ACh caused by the death of the cholinergin neurons.[139] Cholinesterase inhibitors currently approved include donepezil (brand name Aricept),[140] galantamine (Razadyne),[141] and rivastigmine (branded as Exelon,[142] and Exelon Patch[143]). There is also evidence for the efficacy of these medications in mild to moderate Alzheimer’s disease,[144] and some evidence for their use in the advanced stage. Only donepezil is approved for treatment of advanced AD dementia.[145] The use of these drugs in mild cognitive impairment has not shown any effect in a delay of the onset of AD.[146] Most common side effects include nausea and vomiting, both of which are linked to cholinergic excess. These side effects arise in approximately ten to twenty percent of users and are mild to moderate in severity. Less common secondary effects include muscle cramps; decreased heart rate (bradycardia), decreased appetite and weight, and increased gastric acid.[147][148][149][150]
Glutamate is a useful excitatory neurotransmitter of the nervous system, although excessive amounts in the brain can lead to cell death through a process called excitotoxicity which consists of the overstimulation of glutamate receptors. Excitotoxicity occurs not only in Alzheimer's disease, but also in other neurological diseases such as Parkinson's disease and multiple sclerosis.[151] Memantine (brand names Akatinol, Axura, Ebixa/Abixa, Memox and Namenda),[152] is a noncompetitive NMDA receptor antagonist first used as an anti-influenza agent. It acts on the glutamatergic system by blocking NMDA glutamate receptors and inhibits their overstimulation by glutamate.[151] Memantine has been shown to be moderately efficacious in the treatment of moderate to severe Alzheimer’s disease. Its effects in the initial stages are unknown.[153] Reported adverse events with memantine are infrequent and mild, including hallucinations, confusion, dizziness, headache and fatigue.[154] Memantine used in combination with donepezil has been shown to be "of statistically significant but clinically marginal effectiveness".[155]
Neuroleptic anti-psychotic drugs commonly given to Alzheimer's patients with behavioural problems are modestly useful in reducing aggression and psychosis, but are associated with serious adverse effects, such as cerebrovascular events, movement difficulties or cognitive decline, that do not permit their routine use.[156][157][158]
Psychosocial intervention

Psychosocial interventions are used as an adjunct to pharmaceutical treatment and can be classified within behavior, emotion, cognition or stimulation oriented approaches. Research on efficacy is unavailable and rarely specific to the disease, focusing instead on dementia.[159]
Behavioral interventions attempt to identify and reduce the antecedents and consequences of problem behaviors. This approach has not shown success in the overall functioning of patients,[160] but can help to reduce some specific problem behaviors, such as incontinence.[161] There is still a lack of high quality data on the effectiveness of these techniques in other behavior problems such as wandering.[162][163]
Emotion-oriented interventions include reminiscence therapy, validation therapy, supportive psychotherapy, sensory integration or snoezelen, and simulated presence therapy. Supportive psychotherapy has received little or no formal scientific study, but some clinicians find it useful in helping mildly impaired patients adjust to their illness.[159] Reminiscence therapy (RT) involves the discussion of past experiences individually or in group, many times with the aid of photographs, household items, music and sound recordings, or other familiar items from the past. Although there are few quality studies on the effectiveness of RT it may be beneficial for cognition and mood.[164] Simulated presence therapy (SPT) is based on attachment theories and is normally carried out playing a recording with voices of the closest relatives of the patient. There is preliminary evidence indicating that SPT may reduce anxiety and challenging behaviors.[165][166] Finally, validation therapy is based on acceptance of the reality and personal truth of another's experience, while sensory integration is based on exercises aimed to stimulate senses. There is little evidence to support the usefulness of these therapies.[167][168]
The aim of cognition-oriented treatments, which include reality orientation and cognitive retraining is the restoration of cognitive deficits. Reality orientation consists in the presentation of information about time, place or person in order to ease the understanding of the person about its surroundings and his place in them. On the other hand cognitive retraining tries to improve impaired capacities by exercitation of mental abilities. Both have shown some efficacy improving cognitive capacities,[169][170] although in some works these effects were transient and negative effects, such as frustration, have also been reported.[159]
Stimulation-oriented treatments include art, music and pet therapies, exercise, and any other kind of recreational activities for patients. Stimulation has modest support for improving behavior, mood, and, to a lesser extent, function. Nevertheless, as important as these effects are, the main support for the use of stimulation therapies is the improvement in the patient daily life routine they suppose.[159]
Caregiving
Since there is no cure for Alzheimer's, caregiving is an essential part of the treatment. Due to the eventual inability for the sufferer to self-care, Alzheimer's has to be carefully care-managed. Home care in the familiar surroundings of home may delay onset of some symptoms and delay or eliminate the need for more professional and costly levels of care.[171] Many family members choose to look after their relative,[172] but two-thirds of nursing home residents have dementias.[173]
Modifications to the living environment and lifestyle of the Alzheimer's patient can improve functional performance and ease caretaker burden. Assessment by an occupational therapist is often indicated. Adherence to simplified routines and labeling of household items to cue the patient can aid with activities of daily living, while placing safety locks on cabinets, doors, and gates and securing hazardous chemicals can prevent accidents and wandering. Changes in routine or environment can trigger or exacerbate agitation, whereas well-lit rooms, adequate rest, and avoidance of excess stimulation all help prevent such episodes.[174][175] Appropriate social and visual stimulation can improve function by increasing awareness and orientation. For instance, boldly colored tableware aids those with severe AD, helping people overcome a diminished sensitivity to visual contrast to increase food and beverage intake.[176]
Clinical research
As of 2008, the safety and efficacy of more than 400 pharmaceutical treatments are being investigated in clinical trials worldwide, and approximately one-fourth of these compounds are in Phase III trials, which is the last step prior to review by regulatory agencies.[177] It is unknown as to whether any of these trials will ultimately prove successful in treating the disease.
A critical area of clinical research is focused on treating the underlying disease pathology. Reduction of amyloid beta levels is a common target of compounds under investigation. Immunotherapy or vaccination for the amyloid protein is one treatment modality under study. Unlike vaccines which seek to prevent disease, this therapy would be used to treat diagnosed patients, and is based upon the concept of training the immune system to recognize, attack, and reverse deposition of amyloid, thereby altering the course of the disease.[178] An example of such a vaccine under investigation is ACC-001.[179][180] Similar agents are bapineuzumab, an antibody designed as identical to the naturally-induced anti-amyloid antibody,[181] and MPC-7869, a selective amyloid beta-42 lowering agent.[182] Other approaches are neuroprotective agents, such as AL-108,[183] metal-protein interaction attenuation agents, such as PBT2,[184] or tumor necrosis factor-alpha receptor fusion proteins, such as etanercept.[185][186][187] There are also many basic investigations attempting to increase the knowledge on the origin and mechanisms of the disease that may lead to new treatments.
Prognosis
The early stages of Alzheimer's disease are difficult to diagnose. A definitive diagnosis is usually made once cognitive impairment compromises daily living activities, although the person may still be living independently. He will progress from mild cognitive problems, such as memory loss through increasing stages of cognitive and non-cognitive disturbances, eliminating any possibility of independent living.[50]
Life expectancy of the population with the disease is reduced.[8][188][189] The mean life expectancy following diagnosis is approximately seven years.[8] Fewer than 3% of patients live more than fourteen years.[9] Disease features significantly associated with reduced survival are an increased severity of cognitive impairment, decreased functional level, history of falls, and disturbances in the neurological examination. Other coincident diseases such as heart problems, diabetes or history of alcohol abuse are also related with shortened survival.[188][190][191] While the earlier the age at onset the higher the total survival years, life expectancy is particularly reduced when compared to the healthy population among those who are younger.[189] Men have a less favourable survival prognosis than women.[9][192]
The disease is the underlying cause of death in 70% of all cases.[8] Pneumonia and dehydration are the most frequent immediate causes of death, while cancer is a less frequent cause of death than in the general population.[8][192]
Society and culture
Social costs
Because the median age of the industrialised world's population is gradually increasing, Alzheimer's is a major public health challenge. Much of the concern about the solvency of governmental social safety nets is founded on estimates of the costs of caring for baby boomers, assuming that they develop Alzheimer's in the same proportions as earlier generations. For this reason, money spent informing the public of available effective prevention methods may yield disproportionate benefits.[193]
Caregiving burden
The role of family caregivers has become more prominent in both reducing the social cost of care and improving the quality of life of the patient. Home-based care also can have economic, emotional, and psychological costs to the patient's family. Although family members in particular often express the desire to care for the sufferer to the end,[194] Alzheimer's disease is known for effecting a high burden on caregivers.[172]
Alzheimer's disease can incur a variety of stresses on the caregivers: typical complaints are stress, depression, and an inability to cope. Reasons for these complaints can include: high-demands on the caregiver's concentration, as Alzheimer's sufferers have a decreasing regard for their own safety (and can wander when unattended, for example); the lack of gratitude received when the sufferer is unaware of the help being given; and the lack of satisfaction when the sufferer's condition does not abate. Alzheimer's sufferers can be verbally and physically aggressive, and can stubbornly refuse to be helped. Aggression in particular can lead to a temptation to retaliate, which can put both the sufferer and carer at risk. It is additionally stressful for caregivers who are friends and family to witness a sufferer lose his or her identity, and eventually be unable to recognise them.[172]
Family caregivers often give up time from work and forego pay to spend 47 hours per week on average with the person with AD. From a 2006 survey of US patients with long term care insurance, direct and indirect costs of caring for an Alzheimer's patient average $77,500 per year.[195]
References
- ↑ Brookmeyer R, Gray S, Kawas C (1998). "Projections of Alzheimer's disease in the United States and the public health impact of delaying disease onset". Am J Public Health. 88 (9): 1337–42. PMC 1509089. PMID 9736873. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 2006 prevalence estimate:
- Brookmeyer R, Johnson E, Ziegler-Graham K, MH Arrighi (2007). "Forecasting the global burden of Alzheimer's disease". Alzheimer's and Dementia. 3 (3): 186–91. doi:10.1016/j.jalz.2007.04.381. Retrieved 2008-06-18. Unknown parameter
|month=ignored (help) - Template:Cite paper
- Brookmeyer R, Johnson E, Ziegler-Graham K, MH Arrighi (2007). "Forecasting the global burden of Alzheimer's disease". Alzheimer's and Dementia. 3 (3): 186–91. doi:10.1016/j.jalz.2007.04.381. Retrieved 2008-06-18. Unknown parameter
- ↑
"What is Alzheimer's disease?". Alzheimers.org.uk. 2007. Retrieved 2008-02-21. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Waldemar G, Dubois B, Emre M; et al. (2007). "Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline". Eur. J. Neurol. 14 (1): e1–26. doi:10.1111/j.1468-1331.2006.01605.x. PMID 17222085. Unknown parameter
|month=ignored (help) - ↑ Tabert MH, Liu X, Doty RL, Serby M, Zamora D, Pelton GH, Marder K, Albers MW, Stern Y, Devanand DP (2005). "A 10-item smell identification scale related to risk for Alzheimer's disease". Ann. Neurol. 58 (1): 155–160. doi:10.1002/ana.20533. PMID 15984022.
- ↑ "Understanding stages and symptoms of Alzheimer's disease". National Institute on Aging. 2007-10-26. Retrieved 2008-02-21.
- ↑ "Alzheimer's diagnosis of AD". Alzheimer's Research Trust. Retrieved 2008-02-29.
- ↑ 8.0 8.1 8.2 8.3 8.4 Mölsä PK, Marttila RJ, Rinne UK (1986). "Survival and cause of death in Alzheimer's disease and multi-infarct dementia". Acta Neurol. Scand. 74 (2): 103–7. PMID 3776457. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ 9.0 9.1 9.2 Mölsä PK, Marttila RJ, Rinne UK (1995). "Long-term survival and predictors of mortality in Alzheimer's disease and multi-infarct dementia". Acta Neurol. Scand. 91 (3): 159–64. PMID 7793228. Unknown parameter
|month=ignored (help) - ↑ 10.0 10.1 10.2 Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J (2004). "The importance of neuritic plaques and tangles to the development and evolution of AD". Neurology. 62 (11): 1984–1989. PMID 15184601.
- ↑ "Alzheimer's Disease Clinical Trials". US National Institutes of Health. Retrieved 2008-08-18.
- ↑ "Can Alzheimer's disease be prevented" (pdf). National Institute on Aging. 2006-08-29. Retrieved 2008-02-29.
- ↑ "The MetLife study of Alzheimer's disease: The caregiving experience" (PDF). MetLife Mature Market Institute. 2006. Retrieved 2008-02-12. Unknown parameter
|month=ignored (help) - ↑ Thompson CA, Spilsbury K, Hall J, Birks Y, Barnes C, Adamson J (2007). "Systematic review of information and support interventions for caregivers of people with dementia". BMC Geriatr. 7: 18. doi:10.1186/1471-2318-7-18. PMC 1951962. PMID 17662119.
- ↑ Schneider J, Murray J, Banerjee S, Mann A (1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: I—Factors associated with carer burden". International Journal of Geriatric Psychiatry. 14 (8): 651–661. doi:10.1002/(SICI)1099-1166(199908)14:8<651::AID-GPS992>3.0.CO;2-B. PMID 10489656. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Murray J, Schneider J, Banerjee S, Mann A (1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: II--A qualitative analysis of the experience of caregiving". International Journal of Geriatric Psychiatry. 14 (8): 662–667. doi:10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4. PMID 10489657. Unknown parameter
|month=ignored (help) - ↑ Bonin-Guillaume S, Zekry D, Giacobini E, Gold G, Michel JP (2005). "Impact économique de la démence (English: The economical impact of dementia)". Presse Med (in French). 34 (1): 35–41. ISSN 0755-4982. PMID 15685097. Unknown parameter
|month=ignored (help) - ↑ Meek PD, McKeithan K, Schumock GT (1998). "Economic considerations in Alzheimer's disease". Pharmacotherapy. 18 (2 Pt 2): 68–73, discussion 79–82. PMID 9543467.
- ↑ 19.0 19.1 Berchtold NC, Cotman CW (1998). "Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s". Neurobiology of Aging. 19 (3): 173–189. doi:10.1016/S0197-4580(98)00052-9. PMID 9661992.
- ↑ Auguste D.:
- Alzheimer Alöis (1907). "Uber eine eigenartige Erkrankung der Hirnrinde" (in Template:De icon). 64 (1–2): 146–148.
- Alöis Alzheimer (1987). "About a peculiar disease of the cerebral cortex. (Translated by L. Jarvik and H. Greenson)". Alzheimer Disease and Associated Disorders. 1 (1): 3–8. PMID 3331112. Unknown parameter
|origdate=ignored (|orig-year=suggested) (help) - Maurer Ulrike, Maurer Konrad (2003). Alzheimer: the life of a physician and the career of a disease. New York: Columbia University Press. p. 270. ISBN 0-231-11896-1.
- Hochberg Fred H., Rottenberg David (1977). Neurological classics in modern translation. New York: Hafner Press. ISBN 0-02-851180-8.
- ↑ Kraepelin Emil, Diefendorf A. Ross (translated by) (2007-01-17). Clinical Psychiatry: A Textbook For Students And Physicians (Reprint). Kessinger Publishing. p. 568. ISBN 1-4325-0833-4.
- ↑ Boller F, Forbes MM (1998). "History of dementia and dementia in history: an overview". Journal of Neurological Science. 158 (2): 125–133. doi:10.1016/S0022-510X(98)00128-2. PMID 9702682.
- ↑ Katzman Robert, Terry Robert D, Bick Katherine L (editors) (1978). Alzheimer's disease: senile dementia and related disorders. New York: Raven Press. p. 595. ISBN 0-89004-225-X.
- ↑ Amaducci LA, Rocca WA, Schoenberg BS (1986). "Origin of the distinction between Alzheimer's disease and senile dementia: how history can clarify nosology". Neurology. 36 (11): 1497–1499. PMID 3531918.
- ↑ 25.0 25.1 25.2 Bermejo-Pareja F, Benito-León J, Vega S, Medrano MJ, Román GC (2008). "Incidence and subtypes of dementia in three elderly populations of central Spain". J. Neurol. Sci. 264 (1–2): 63–72. doi:10.1016/j.jns.2007.07.021. PMID 17727890. Unknown parameter
|month=ignored (help) - ↑ Gorelick P (2004). "Risk factors for vascular dementia and Alzheimer disease". Stroke. 35 (11 Suppl 1): 2620–2622. doi:10.1161/01.STR.0000143318.70292.47. PMID 15375299.
- ↑ Hebert L, Scherr P, Bienias J, Bennett D, Evans D (2003). "Alzheimer disease in the U.S. population: prevalence estimates using the 2000 census". Archives of Neurology. 60 (8): 1119–1122. doi:10.1001/archneur.60.8.1119. PMID 12925369.
- ↑ "Neurological disorders: Public health challenges" (PDF). World Health Organization.
- ↑ Andersen K, Launer LJ, Dewey ME, Letenneur L, Ott A, Copeland JR, Dartigues JF, Kragh-Sorensen P, Baldereschi M, Brayne C, Lobo A, Martinez-Lage JM, Stijnen T, Hofman A (1999). "Gender differences in the incidence of AD and vascular dementia: The EURODEM Studies. EURODEM Incidence Research Group". Neurology. 53 (9): 1992–1997. PMID 10599770.
- ↑ Davanipour Z, Tseng CC, Lee PJ, Sobel E (2007). "A case-control study of occupational magnetic field exposure and Alzheimer's disease: results from the California Alzheimer's Disease Diagnosis and Treatment Centers". BMC Neurol. 7: 13. doi:10.1186/1471-2377-7-13. PMID 17559686. Retrieved 2008-02-26.
- ↑ Qiu C, Fratiglioni L, Karp A, Winblad B, Bellander T (2004). "Occupational exposure to electromagnetic fields and risk of Alzheimer's disease". Epidemiology. 15 (6): 687–694. doi:10.1097/01.ede.0000142147.49297.9d. PMID 15475717.
- ↑ Seidler A, Geller P, Nienhaus A, Bernhardt T, Ruppe I, Eggert S, Hietanen M, Kauppinen T, Frölich L (2007). "Occupational exposure to low frequency magnetic fields and dementia: a case-control study". Occup Environ Med. 64 (2): 108–114. doi:10.1136/oem.2005.024190. PMID 17043077.
- ↑ Role of metals:
- Rondeau V, Commenges D, Jacqmin-Gadda H, Dartigues JF (2000). "Relation between aluminum concentrations in drinking water and Alzheimer's disease: an 8-year follow-up study". American Journal of Epidemiology. 152 (1): 59–66. doi:10.1093/aje/152.1.59. PMID 10901330.
- Shcherbatykh I, Carpenter DO (2007). "The role of metals in the etiology of Alzheimer's disease". Journal of Alzheimers Disease. 11 (2): 191–205. PMID 17522444.
- Santibáñez M, Bolumar F, García AM (2007). "Occupational risk factors in Alzheimer's disease: a review assessing the quality of published epidemiological studies". Occupational and Environmental Medicine. 64 (11): 723–732. doi:10.1136/oem.2006.028209. PMID 17525096.
- "Water sanitation in health: Aluminum in drinking water". World Health Organization. 2003.
- ↑ 34.0 34.1 34.2 Di Carlo A, Baldereschi M, Amaducci L; et al. (2002). "Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study". J Am Geriatr Soc. 50 (1): 41–8. PMID 12028245. Unknown parameter
|month=ignored (help) - ↑ Andersen K, Launer LJ, Dewey ME; et al. (1999). "Gender differences in the incidence of AD and vascular dementia: The EURODEM Studies. EURODEM Incidence Research Group". Neurology. 53 (9): 1992–7. PMID 10599770. Unknown parameter
|month=ignored (help) - ↑ 2000 U.S. estimates:
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA (2003). "Alzheimer disease in the US population: prevalence estimates using the 2000 census". Arch. Neurol. 60 (8): 1119–22. doi:10.1001/archneur.60.8.1119. PMID 12925369. Unknown parameter
|month=ignored (help) - "Profiles of general demographic characteristics, 2000 census of population and housing, United States" (PDF). U.S. Census Bureau. 2001. Retrieved 2008-08-27.
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA (2003). "Alzheimer disease in the US population: prevalence estimates using the 2000 census". Arch. Neurol. 60 (8): 1119–22. doi:10.1001/archneur.60.8.1119. PMID 12925369. Unknown parameter
- ↑ 37.0 37.1 Ferri CP, Prince M, Brayne C; et al. (2005). "Global prevalence of dementia: a Delphi consensus study" (PDF). Lancet. 366 (9503): 2112–7. doi:10.1016/S0140-6736(05)67889-0. PMID 16360788. Retrieved 2008-06-13. Unknown parameter
|month=ignored (help) - ↑ World Health Organization (2006). Neurological Disorders: Public Health Challenges. Switzerland: World Health Organization. pp. 204–207. ISBN 978-92-4-156336-9.
- ↑ Preclinical:
- Linn RT, Wolf PA, Bachman DL; et al. (1995). "The 'preclinical phase' of probable Alzheimer's disease. A 13-year prospective study of the Framingham cohort". Arch. Neurol. 52 (5): 485–90. PMID 7733843. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - Saxton J, Lopez OL, Ratcliff G; et al. (2004). "Preclinical Alzheimer disease: neuropsychological test performance 1.5 to 8 years prior to onset". Neurology. 63 (12): 2341–7. PMID 15623697. Unknown parameter
|month=ignored (help) - Twamley EW, Ropacki SA, Bondi MW (2006). "Neuropsychological and neuroimaging changes in preclinical Alzheimer's disease". J Int Neuropsychol Soc. 12 (5): 707–35. doi:10.1017/S1355617706060863. PMC 1621044. PMID 16961952. Unknown parameter
|month=ignored (help)
- Linn RT, Wolf PA, Bachman DL; et al. (1995). "The 'preclinical phase' of probable Alzheimer's disease. A 13-year prospective study of the Framingham cohort". Arch. Neurol. 52 (5): 485–90. PMID 7733843. Unknown parameter
- ↑ Perneczky R, Pohl C, Sorg C, Hartmann J, Komossa K, Alexopoulos P, Wagenpfeil S, Kurz A (2006). "Complex activities of daily living in mild cognitive impairment: conceptual and diagnostic issues". Age Ageing. 35 (3): 240–245. doi:10.1093/ageing/afj054. PMID 16513677.
- ↑ Arnáiz E, Almkvist O (2003). "Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease". Acta Neurol. Scand., Suppl. 179: 34–41. doi:10.1034/j.1600-0404.107.s179.7.x. PMID 12603249.
|access-date=requires|url=(help) - ↑ Kazui H, Matsuda A, Hirono N; et al. (2005). "Everyday memory impairment of patients with mild cognitive impairment". Dement Geriatr Cogn Disord. 19 (5–6): 331–7. doi:10.1159/000084559. PMID 15785034. Retrieved 2008-06-12.
- ↑ Rapp MA, Reischies FM (2005). "Attention and executive control predict Alzheimer disease in late life: results from the Berlin Aging Study (BASE)". American Journal of Geriatric Psychiatry. 13 (2): 134–141. doi:10.1176/appi.ajgp.13.2.134. PMID 15703322.
- ↑ Spaan PE, Raaijmakers JG, Jonker C (2003). "Alzheimer's disease versus normal ageing: a review of the efficiency of clinical and experimental memory measures". Journal of Clinical Experimental Neuropsychology. 25 (2): 216–233. PMID 12754679.
- ↑ 45.0 45.1 Craig D, Mirakhur A, Hart DJ, McIlroy SP, Passmore AP (2005). "A cross-sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer's disease". American Journal of Geriatric Psychiatry. 13 (6): 460–468. doi:10.1176/appi.ajgp.13.6.460. PMID 15956265.
- ↑ Robert PH, Berr C, Volteau M, Bertogliati C, Benoit M, Sarazin M, Legrain S, Dubois B (2006). "Apathy in patients with mild cognitive impairment and the risk of developing dementia of Alzheimer's disease: a one-year follow-up study". Clin Neurol Neurosurg. 108 (8): 733–736. doi:10.1016/j.clineuro.2006.02.003. PMID 16567037.
- ↑ Palmer K, Berger AK, Monastero R, Winblad B, Bäckman L, Fratiglioni L (2007). "Predictors of progression from mild cognitive impairment to Alzheimer disease". Neurology. 68 (19): 1596–1602. doi:10.1212/01.wnl.0000260968.92345.3f. PMID 17485646.
- ↑
Small BJ, Gagnon E, Robinson B (2007). "Early identification of cognitive deficits: preclinical Alzheimer's disease and mild cognitive impairment". Geriatrics. 62 (4): 19–23. PMID 17408315. Unknown parameter
|month=ignored (help) - ↑
Petersen RC (2007). "The current status of mild cognitive impairment—what do we tell our patients?". Nat Clin Pract Neurol. 3 (2): 60–1. doi:10.1038/ncpneuro0402. PMID 17279076. Unknown parameter
|month=ignored (help) - ↑ 50.0 50.1 50.2 50.3 50.4 50.5 Förstl H, Kurz A (1999). "Clinical features of Alzheimer's disease". European Archives of Psychiatry and Clinical Neuroscience. 249 (6): 288–290. PMID 10653284.
- ↑
Carlesimo GA, Oscar-Berman M (1992). "Memory deficits in Alzheimer's patients: a comprehensive review". Neuropsychol Rev. 3 (2): 119–69. PMID 1300219. Unknown parameter
|month=ignored (help) - ↑ Jelicic M, Bonebakker AE, Bonke B (1995). "Implicit memory performance of patients with Alzheimer's disease: a brief review". International Psychogeriatrics. 7 (3): 385–392. doi:10.1017/S1041610295002134. PMID 8821346.
- ↑ 53.0 53.1 53.2 Frank EM (1994). "Effect of Alzheimer's disease on communication function". J S C Med Assoc. 90 (9): 417–23. PMID 7967534. Unknown parameter
|month=ignored (help) - ↑ Becker JT, Overman AA (2002). "[The semantic memory deficit in Alzheimer's disease]". Rev Neurol (in Spanish; Castilian). 35 (8): 777–83. PMID 12402233.
- ↑ Hodges JR, Patterson K (1995). "Is semantic memory consistently impaired early in the course of Alzheimer's disease? Neuroanatomical and diagnostic implications". Neuropsychologia. 33 (4): 441–59. PMID 7617154. Unknown parameter
|month=ignored (help) - ↑ Benke T (1993). "Two forms of apraxia in Alzheimer's disease". Cortex. 29 (4): 715–25. PMID 8124945. Unknown parameter
|month=ignored (help) - ↑
Forbes KE, Shanks MF, Venneri A (2004). "The evolution of dysgraphia in Alzheimer's disease". Brain Res. Bull. 63 (1): 19–24. doi:10.1016/j.brainresbull.2003.11.005. PMID 15121235. Unknown parameter
|month=ignored (help) - ↑ Galasko D, Schmitt F, Thomas R, Jin S, Bennett D (2005). "Detailed assessment of activities of daily living in moderate to severe Alzheimer's disease". Journal of the International Neuropsychology Society. 11 (4): 446–453. PMID 16209425.
- ↑
Galasko D, Schmitt F, Thomas R, Jin S, Bennett D (2005). "Detailed assessment of activities of daily living in moderate to severe Alzheimer's disease". J Int Neuropsychol Soc. 11 (4): 446–53. PMID 16209425. Unknown parameter
|month=ignored (help) - ↑ Sartori G, Snitz BE, Sorcinelli L, Daum I (2004). "Remote memory in advanced Alzheimer's disease". Arch Clin Neuropsychol. 19 (6): 779–89. doi:10.1016/j.acn.2003.09.007. PMID 15288331. Unknown parameter
|month=ignored (help) - ↑ Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A (2001). "Sundowning and circadian rhythms in Alzheimer's disease". Am J Psychiatry. 158 (5): 704–11. PMID 11329390. Retrieved 2008-08-27. Unknown parameter
|month=ignored (help) - ↑ Neuropsychiatric symptoms:
- Scarmeas N, Brandt J, Blacker D; et al. (2007). "Disruptive behavior as a predictor in Alzheimer disease". Arch. Neurol. 64 (12): 1755–61. doi:10.1001/archneur.64.12.1755. PMID 18071039. Unknown parameter
|month=ignored (help) - Tatsch MF, Bottino CM, Azevedo D; et al. (2006). "Neuropsychiatric symptoms in Alzheimer disease and cognitively impaired, nondemented elderly from a community-based sample in Brazil: prevalence and relationship with dementia severity". Am J Geriatr Psychiatry. 14 (5): 438–45. doi:10.1097/01.JGP.0000218218.47279.db. PMID 16670248. Unknown parameter
|month=ignored (help) - Volicer L, Bass EA, Luther SL (2007). "Agitation and resistiveness to care are two separate behavioral syndromes of dementia". J Am Med Dir Assoc. 8 (8): 527–32. doi:10.1016/j.jamda.2007.05.005. PMID 17931577. Unknown parameter
|month=ignored (help)
- Scarmeas N, Brandt J, Blacker D; et al. (2007). "Disruptive behavior as a predictor in Alzheimer disease". Arch. Neurol. 64 (12): 1755–61. doi:10.1001/archneur.64.12.1755. PMID 18071039. Unknown parameter
- ↑ Honig LS, Mayeux R (2001). "Natural history of Alzheimer's disease". Aging (Milano). 13 (3): 171–82. PMID 11442300. Unknown parameter
|month=ignored (help) - ↑ Gold DP, Reis MF, Markiewicz D, Andres D (1995). "When home caregiving ends: a longitudinal study of outcomes for caregivers of relatives with dementia". J Am Geriatr Soc. 43 (1): 10–6. PMID 7806732. Unknown parameter
|month=ignored (help) - ↑ Bär M, Kruse A, Re S (2003). "[Situations of emotional significance in residents suffering from dementia]". Z Gerontol Geriatr (in German). 36 (6): 454–62. doi:10.1007/s00391-003-0191-0. PMID 14685735. Unknown parameter
|month=ignored (help) - ↑ Souren LE, Franssen EH, Reisberg B (1995). "Contractures and loss of function in patients with Alzheimer's disease". J Am Geriatr Soc. 43 (6): 650–5. PMID 7775724. Unknown parameter
|month=ignored (help) - ↑ Berkhout AM, Cools HJ, van Houwelingen HC (1998). "The relationship between difficulties in feeding oneself and loss of weight in nursing-home patients with dementia". Age Ageing. 27 (5): 637–41. PMID 12675103. Unknown parameter
|month=ignored (help) - ↑ Wada H, Nakajoh K, Satoh-Nakagawa T; et al. (2001). "Risk factors of aspiration pneumonia in Alzheimer's disease patients". Gerontology. 47 (5): 271–6. PMID 11490146.
- ↑ Gambassi G, Landi F, Lapane KL, Sgadari A, Mor V, Bernabei R (1999). "Predictors of mortality in patients with Alzheimer's disease living in nursing homes". J. Neurol. Neurosurg. Psychiatr. 67 (1): 59–65. PMC 1736445. PMID 10369823. Unknown parameter
|month=ignored (help) - ↑ 70.0 70.1 70.2 Wenk GL (2003). "Neuropathologic changes in Alzheimer's disease". Journal of Clinical Psychiatry. 64 Suppl 9: 7–10. PMID 12934968.
- ↑ Walker LC, Rosen RF (2006). "Alzheimer therapeutics-what after the cholinesterase inhibitors?". Age Ageing. 35 (4): 332–335. doi:10.1093/ageing/afl009. PMID 16644763.
- ↑ 72.0 72.1 Shen ZX (2004). "Brain cholinesterases: II. The molecular and cellular basis of Alzheimer's disease". Medical Hypotheses. 63 (2): 308–321. doi:10.1016/j.mehy.2004.02.031. PMID 15236795.
- ↑ 73.0 73.1 Hardy J, Allsop D (1991). "Amyloid deposition as the central event in the aetiology of Alzheimer's disease". Trends Pharmacol. Sci. 12 (10): 383–8. doi:10.1016/0165-6147(91)90609-V. PMID 1763432.
- ↑ 74.0 74.1 74.2 Mudher A, Lovestone S (2002). "Alzheimer's disease-do tauists and baptists finally shake hands?". Trends in Neuroscience. 25 (1): 22–26. doi:10.1016/S0166-2236(00)02031-2. PMID 11801334.
- ↑ Hashimoto M, Rockenstein E, Crews L, Masliah E (2003). "Role of protein aggregation in mitochondrial dysfunction and neurodegeneration in Alzheimer's and Parkinson's diseases". Neuromolecular Medicine. 4 (1–2): 21–36. doi:10.1385/NMM:4:1-2:21. PMID 14528050.
- ↑ Priller C, Bauer T, Mitteregger G, Krebs B, Kretzschmar HA, Herms J (2006). "Synapse formation and function is modulated by the amyloid precursor protein". Journal of Neuroscience. 26 (27): 7212–7221. doi:10.1523/JNEUROSCI.1450-06.2006. PMID 16822978.
- ↑ Turner PR, O'Connor K, Tate WP, Abraham WC (2003). "Roles of amyloid precursor protein and its fragments in regulating neural activity, plasticity and memory". Prog. Neurobiology. 70 (1): 1–32. PMID 12927332.
- ↑ Hooper NM (2005). "Roles of proteolysis and lipid rafts in the processing of the amyloid precursor protein and prion protein". Biochemical Society Transactions. 33 (Pt 2): 335–338. doi:10.1042/BST0330335. PMID 15787600.
- ↑ Ohnishi S, Takano K (2004). "Amyloid fibrils from the viewpoint of protein folding". Cellular Molecular Life Sciences. 61 (5): 511–524. doi:10.1007/s00018-003-3264-8. PMID 15004691.
- ↑ Nistor M, Don M, Parekh M, Sarsoza F, Goodus M, Lopez GE, Kawas C, Leverenz J, Doran E, Lott IT, Hill M, Head E (2007). "Alpha- and beta-secretase activity as a function of age and beta-amyloid in Down syndrome and normal brain". Neurobiol. Aging. 28 (10): 1493–506. doi:10.1016/j.neurobiolaging.2006.06.023. PMID 16904243.
- ↑ Lott IT, Head E (2005). "Alzheimer disease and Down syndrome: factors in pathogenesis". Neurobiology of Aging. 26 (3): 383–389. doi:10.1016/j.neurobiolaging.2004.08.005. PMID 15639317.
- ↑ Polvikoski T, Sulkava R, Haltia M, Kainulainen K, Vuorio A, Verkkoniemi A, Niinistö L, Halonen P, Kontula K (1995). "Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein". New England Journal of Medicine. 333 (19): 1242–1247. doi:10.1056/NEJM199511093331902. PMID 7566000.
- ↑ "Alzheimer disease". US National Library of Medicine. 2008-04-25. Retrieved 2008-05-02.
- ↑ Beta-amyloid precursor protein
- Games D, Adams D, Alessandrini R, Barbour R, Berthelette P, Blackwell C, Carr T, Clemens J, Donaldson T, Gillespie F (1995). "Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein". Nature. 373 (6514): 523–527. doi:10.1038/373523a0. PMID 7845465.
- Masliah E, Sisk A, Mallory M, Mucke L, Schenk D, Games D (1996). "Comparison of neurodegenerative pathology in transgenic mice overexpressing V717F beta-amyloid precursor protein and Alzheimer's disease". Journal of Neuroscience. 16 (18): 5795–5811. PMID 8795633.
- Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S, Yang F, Cole G (1996). "Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice". Science. 274 (5284): 99–102. doi:10.1126/science.274.5284.99. PMID 8810256.
- ↑ Yankner BA, Duffy LK, Kirschner DA (1990). "Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides". Science. 250 (4978): 279–282. doi:10.1126/science.2218531. PMID 2218531.
- ↑ Chen, X, Yan, SD (2006). "Mitochondrial Aβ: A Potential Cause of Metabolic Dysfunction in Alzheimer's Disease". IUBMB Life. 58 (12): 686–694. doi:10.1080/15216540601047767. PMID 17424907.
- ↑ Schmitz C, Rutten BP, Pielen A; et al. (2004). "Hippocampal neuron loss exceeds amyloid plaque load in a transgenic mouse model of Alzheimer's disease". Am. J. Pathol. 164 (4): 1495–1502. PMC 1615337. PMID 15039236. Unknown parameter
|month=ignored (help) - ↑ Hernández F, Avila J (2007). "Tauopathies". Cellular Molecular Life Sciences. 64 (17): 2219–2233. doi:10.1007/s00018-007-7220-x. PMID 17604998.
- ↑ Goedert M, Spillantini MG, Crowther RA (1991). "Tau proteins and neurofibrillary degeneration". Brain Pathology. 1 (4): 279–286. doi:10.1111/j.1750-3639.1991.tb00671.x. PMID 1669718.
- ↑ Chun W, Johnson GV (2007). "The role of tau phosphorylation and cleavage in neuronal cell death". Frontiers of Bioscience. 12: 733–756. PMID 17127334.
- ↑ Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH (1994). "Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital". Cerebral Cortex. 4 (2): 138–150. doi:10.1093/cercor/4.2.138. PMID 8038565.
- ↑ Wozniak MA, Mee AP, Itzhaki RF (2009). "Herpes simplex virus type 1 DNA is located within Alzheimer's disease amyloid plaques". J Pathol. 217 (1): 131–8. doi:10.1002/path.2449. PMID 18973185. Unknown parameter
|month=ignored (help) - ↑ Greig NH, Mattson MP, Perry T, Chan SL, Giordano T, Sambamurti K, Rogers JT, Ovadia H, Lahiri DK (2004). "New therapeutic strategies and drug candidates for neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists". Ann N Y Acad Sci. 1035 (Dec): 290–315. doi:10.1196/annals.1332.018. PMID 15681814.
- ↑ Mendez MF (2006). "The accurate diagnosis of early-onset dementia". International Journal of Psychiatry Medicine. 36 (4): 401–412. PMID 17407994.
- ↑ Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J (2006). "Therapeutic approaches to Alzheimer's disease". Brain. 129 (Pt 11): 2840–2855. doi:10.1093/brain/awl280. PMID 17018549.
- ↑
"Dementia: Quick reference guide" (PDF). National Institute for Health and Clinical Excellence. 2006. ISBN 1-84629-312-X. Retrieved 2008-02-22. Unknown parameter
|month=ignored (help) - ↑ McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984). "Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease". Neurology. 34 (7): 939–44. PMID 6610841.
- ↑ 98.0 98.1 Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P (2007). "Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria". Lancet Neurology. 6 (8): 734–746. doi:10.1016/S1474-4422(07)70178-3. PMID 17616482.
- ↑ Blacker D, Albert MS, Bassett SS, Go RC, Harrell LE, Folstein MF (1994). "Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative". Archives of Neurology. 51 (12): 1198–1204. PMID 7986174.
- ↑ American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental disorders, 4th Edition Text Revision. Washington DC.
- ↑ Ito N (1996). "Clinical aspects of dementia". Hokkaido Igaku Zasshi (in Japanese). 71 (3): 315–320. PMID 8752526.
- ↑ Tombaugh TN, McIntyre NJ (1992). "The mini-mental state examination: a comprehensive review". J Am Geriatr Soc. 40 (9): 922–935. PMID 1512391.
- ↑ Pasquier F (1999). "Early diagnosis of dementia: neuropsychology". J. Neurol. 246 (1): 6–15. PMID 9987708.
- ↑ Harvey PD, Moriarty PJ, Kleinman L, Coyne K, Sadowsky CH, Chen M, Mirski DF (2005). "The validation of a caregiver assessment of dementia: the Dementia Severity Scale". Alzheimer Disease and Associated Disorders. 19 (4): 186–194. PMID 16327345.
- ↑ Antoine C, Antoine P, Guermonprez P, Frigard B (2004). "Awareness of deficits and anosognosia in Alzheimer's disease". Encephale (in French). 30 (6): 570–577. PMID 15738860.
- ↑ Cruz VT, Pais J, Teixeira A, Nunes B (2004). "The initial symptoms of Alzheimer disease: caregiver perception". Acta Med Port (in Portuguese). 17 (6): 435–444. PMID 16197855.
- ↑ Clarfield AM (2003). "The decreasing prevalence of reversible dementias: an updated meta-analysis". Arch. Intern. Med. 163 (18): 2219–29. doi:10.1001/archinte.163.18.2219. PMID 14557220.
- ↑ Geldmacher DS, Whitehouse PJ (1997). "Differential diagnosis of Alzheimer's disease". Neurology. 48 (5 Suppl 6): S2–9. PMID 9153154.
- ↑ Potter GG, Steffens DC (2007). "Contribution of depression to cognitive impairment and dementia in older adults". Neurologist. 13 (3): 105–117. doi:10.1097/01.nrl.0000252947.15389.a9. PMID 17495754.
- ↑ Bonte FJ, Harris TS, Hynan LS, Bigio EH, White CL (2006). "Tc-99m HMPAO SPECT in the differential diagnosis of the dementias with histopathologic confirmation". Clinical nuclear medicine. 31 (7): 376–378. doi:10.1097/01.rlu.0000222736.81365.63. PMID 16785801.
- ↑ Dougall NJ, Bruggink S, Ebmeier KP (2004). "Systematic review of the diagnostic accuracy of 99mTc-HMPAO-SPECT in dementia". American Journal of Geriatric Psychiatry. 12 (6): 554–570. doi:10.1176/appi.ajgp.12.6.554. PMID 15545324.
- ↑ Kemppainen NM, Aalto S, Karrasch M, Någren K, Savisto N, Oikonen V, Viitanen M, Parkkola R, Rinne JO (2008). "Cognitive reserve hypothesis: Pittsburgh Compound B and fluorodeoxyglucose positron emission tomography in relation to education in mild Alzheimer's disease". Ann. Neurol. 63 (1): 112–8. doi:10.1002/ana.21212. PMID 18023012.
- ↑
Ikonomovic MD, Klunk WE, Abrahamson EE, Mathis CA, Price JC, Tsopelas ND, Lopresti BJ, Ziolko S, Bi W, Paljug WR, Debnath ML, Hope CE, Isanski BA, Hamilton RL, Dekosky ST (March 2008). "Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer's disease". Brain. doi:doi:10.1093/brain/awn016 Check
|doi=value (help). PMID 18339640. - ↑ Jack CR, Lowe VJ, Senjem ML; et al. (2008). "11C PiB and structural MRI provide complementary information in imaging of Alzheimer's disease and amnestic mild cognitive impairment". Brain. 131 (Pt 3): 665–80. doi:10.1093/brain/awm336. PMID 18263627.
- ↑ Marksteiner J, Hinterhuber H, Humpel C (2007). "Cerebrospinal fluid biomarkers for diagnosis of Alzheimer's disease: beta-amyloid(1-42), tau, phospho-tau-181 and total protein". Drugs Today. 43 (6): 423–431. doi:10.1358/dot.2007.43.6.1067341. PMID 17612711.
- ↑ Prevention recommendations not supported:
- Kawas CH (2006). "Medications and diet: protective factors for AD?". Alzheimer Dis Assoc Disord. 20 (3 Suppl 2): S89–96. PMID 16917203.
- Luchsinger JA, Mayeux R (2004). "Dietary factors and Alzheimer's disease". Lancet Neurol. 3 (10): 579–87. doi:10.1016/S1474-4422(04)00878-6. PMID 15380154.
- Luchsinger JA, Noble JM, Scarmeas N (2007). "Diet and Alzheimer's disease". Curr Neurol Neurosci Rep. 7 (5): 366–72. doi:10.1007/s11910-007-0057-8. PMID 17764625.
- ↑ Szekely CA, Breitner JC, Zandi PP (2007). "Prevention of Alzheimer's disease". Int Rev Psychiatry. 19 (6): 693–706. doi:10.1080/09540260701797944. PMID 18092245.
- ↑ Alcohol:
- Mulkamal KJ; et al. (2003-03-19). "Prospective study of alcohol consumption and risk of dementia in older adults". Journal of the American Medical Association. 289: 1405–1413.
- Ganguli M; et al. (2005). "Alcohol consumption and cognitive function in late life: A longitudinal community study". Neurology. 65: 1210–1217.
- Huang W; et al. (2002). "Alcohol consumption and incidence of dementia in a community sample aged 75 years and older". Journal of Clinical Epidemiology. 55 (10): 959–964.
- Rodgers B; et al. (2005). "Non-linear relationships between cognitive function and alcohol consumption in young, middle-aged and older adults: The PATH Through Life Project". Addiction. 100 (9): 1280–1290.
- Anstey KJ; et al. (2005). "Lower cognitive test scores observed in alcohol are associated with demographic, personality, and biological factors: The PATH Through Life Project". Addiction. 100 (9): 1291–1301, .Espeland, M.; et al. (2006). "Association between alcohol intake and domain-specific cognitive function in older women". Neuroepidemiology. 1 (27): 1–12.
- Stampfer MJ; et al. (2005). "Effects of moderate alcohol consumption on cognitive function in women". New England Journal of Medicine. 352: 245–253.
- Ruitenberg A; et al. (2002). "Alcohol consumption and risk of dementia: the Rotterdam Study". Lancet. 359 (9303): 281–286.
- Scarmeas N; et al. (2006-04-18). "Mediterranean diet and risk for Alzheimer's disease". Annals of Neurology.
- ↑ Mediterranean diet:
- Scarmeas N, Stern Y, Mayeux R, Luchsinger JA (2006). "Mediterranean diet, Alzheimer disease, and vascular mediation". Arch. Neurol. 63 (12): 1709–1717. doi:10.1001/archneur.63.12.noc60109. PMID 17030648.
- Scarmeas N, Luchsinger JA, Mayeux R, Stern Y (2007). "Mediterranean diet and Alzheimer disease mortality". Neurology. 69 (11): 1084–93. doi:10.1212/01.wnl.0000277320.50685.7c. PMID 17846408.
- Barberger-Gateau P, Raffaitin C, Letenneur L, Berr C, Tzourio C, Dartigues JF, Alpérovitch A (2007). "Dietary patterns and risk of dementia: the Three-City cohort study". Neurology. 69 (20): 1921–1930. doi:10.1212/01.wnl.0000278116.37320.52. PMID 17998483.
- Dai Q, Borenstein AR, Wu Y, Jackson JC, Larson EB (2006). "Fruit and vegetable juices and Alzheimer's disease: the Kame Project". American Journal of Medicine. 119 (9): 751–759. doi:10.1016/j.amjmed.2006.03.045. PMID 16945610.
- Savaskan E, Olivieri G, Meier F, Seifritz E, Wirz-Justice A, Müller-Spahn F (2003). "Red wine ingredient resveratrol protects from beta-amyloid neurotoxicity". Gerontology. 49 (6): 380–383. doi:10.1159/000073766. PMID 14624067.
- ↑
Luchsinger JA, Mayeux R (2004 Oct). "Dietary factors and Alzheimer's disease". Lancet Neurology. 3 (10): 579–587. PMID 15380154.
Available data do not permit definitive conclusions regarding diet and AD or specific recommendations on diet modification for the prevention of AD.
Check date values in:|date=(help) - ↑
Kawas CH (2006 Jul-Sep). "Medications and diet: protective factors for AD?". Alzheimer Dis Assoc Disord. 20 (3 Suppl 2): S89–96. PMID 16917203.
Evidence regarding dietary and supplemental intake of vitamins E, C, and folate, and studies of alcohol and wine intake are also reviewed. At present, there is insufficient evidence to make public health recommendations, but these studies can provide potentially important clues and new avenues for clinical and laboratory research.
Check date values in:|date=(help) - ↑ Vitamins:
- Morris MC, Schneider JA, Tangney CC (2006). "Thoughts on B-vitamins and dementia". J. Alzheimers Dis. 9 (4): 429–33. PMID 16917152.
- Alzheimer's Association. "Vitamin E".
- Landmark K (2006). "[Could intake of vitamins C and E inhibit development of Alzheimer dementia?]". Tidsskr. Nor. Laegeforen. (in Norwegian). 126 (2): 159–61. PMID 16415937.
- Luchsinger JA, Tang MX, Miller J, Green R, Mayeux R (2007). "Relation of higher folate intake to lower risk of Alzheimer disease in the elderly". Arch. Neurol. 64 (1): 86–92. doi:10.1001/archneur.64.1.86. PMID 17210813.
- ↑ Vitamins only of secondary benefit:
- Morris MC, Evans DA, Schneider JA, Tangney CC, Bienias JL, Aggarwal NT (2006). "Dietary folate and vitamins B-12 and B-6 not associated with incident Alzheimer's disease". J. Alzheimers Dis. 9 (4): 435–43. PMID 16917153.
- Malouf M, Grimley EJ, Areosa SA (2003). "Folic acid with or without vitamin B12 for cognition and dementia". Cochrane Database Syst Rev (4): CD004514. doi:10.1002/14651858.CD004514. PMID 14584018.
- Sun Y, Lu CJ, Chien KL, Chen ST, Chen RC (2007). "Efficacy of multivitamin supplementation containing vitamins B6 and B12 and folic acid as adjunctive treatment with a cholinesterase inhibitor in Alzheimer's disease: a 26-week, randomised, double-blind, placebo-controlled study in Taiwanese patients". Clin Ther. 29 (10): 2204–14. doi:10.1016/j.clinthera.2007.10.012. PMID 18042476.
- Boothby LA, Doering PL (2005). "Vitamin C and vitamin E for Alzheimer's disease". Ann Pharmacother. 39 (12): 2073–80. doi:10.1345/aph.1E495. PMID 16227450.
- Gray SL, Anderson ML, Crane PK, Breitner JC, McCormick W, Bowen JD, Teri L, Larson E (2008). "Antioxidant vitamin supplement use and risk of dementia or Alzheimer's disease in older adults". J Am Geriatr Soc. 56 (2): 291–295. doi:10.1111/j.1532-5415.2007.01531.x. PMID 18047492.
- ↑ Curcumin in diet:
- Garcia-Alloza M, Borrelli LA, Rozkalne A, Hyman BT, Bacskai BJ (2007). "Curcumin labels amyloid pathology in vivo, disrupts existing plaques, and partially restores distorted neurites in an Alzheimer mouse model". Journal of Neurochemistry. 102 (4): 1095–1104. doi:10.1111/j.1471-4159.2007.04613.x. PMID 17472706.
- Lim GP, Chu T, Yang F, Beech W, Frautschy SA, Cole GM (2001). "The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse". Journal of Neuroscience. 21 (21): 8370–8377. PMID 11606625.
- ↑ Rosendorff C, Beeri MS, Silverman JM (2007). "Cardiovascular risk factors for Alzheimer's disease". Am J Geriatr Cardiol. 16 (3): 143–9. doi:10.1111/j.1076-7460.2007.06696.x. PMID 17483665.
- ↑ Gustafson D, Rothenberg E, Blennow K, Steen B, Skoog I (2003). "An 18-year follow-up of overweight and risk of Alzheimer disease". Arch. Intern. Med. 163 (13): 1524–1528. doi:10.1001/archinte.163.13.1524. PMID 12860573.
- ↑ Reiss AB, Wirkowski E (2007). "Role of HMG-CoA reductase inhibitors in neurological disorders : progress to date". Drugs. 67 (15): 2111–2120. PMID 17927279.
- ↑ Kuller LH (2007). "Statins and dementia". Current Atherosclerosis Reports. 9 (2): 154–161. doi:10.1007/s11883-007-0012-9. PMID 17877925.
- ↑ Szekely CA, Breitner JC, Fitzpatrick AL, Rea TD, Psaty BM, Kuller LH, Zandi PP (2008). "NSAID use and dementia risk in the Cardiovascular Health Study: role of APOE and NSAID type". Neurology. 70 (1): 17–24. doi:10.1212/01.wnl.0000284596.95156.48. PMID 18003940.
- ↑ "Long-term use of ibuprofen may reduce the risk of developing Alzheimer's disease, a large US study reports". BBC. 2008-05-05.
- ↑ "Ibuprofen Linked to Reduced Alzheimer's Risk". Washington Post. 2008-05-05.
- ↑ Craig MC, Murphy DG (2007). "Estrogen: effects on normal brain function and neuropsychiatric disorders". Climacteric. 10 Suppl 2: 97–104. doi:10.1080/13697130701598746. PMID 17882683.
- ↑ Mori K, Takeda M (2007). "Hormone replacement Up-to-date. Hormone replacement therapy and brain function". Clin Calcium (in Japanese). 17 (9): 1349–1354. doi:CliCa070913491354 Check
|doi=value (help). PMID 17767023. - ↑ Birks J, Grimley Evans J (2007). "Ginkgo biloba for cognitive impairment and dementia". Cochrane Database Syst Rev (2): CD003120. doi:10.1002/14651858.CD003120.pub2. PMID 17443523. Retrieved 2008-02-22.
- ↑ Verghese J, Lipton R, Katz M, Hall C, Derby C, Kuslansky G, Ambrose A, Sliwinski M, Buschke H (2003). "Leisure activities and the risk of dementia in the elderly". N Engl J Med. 348 (25): 2508–2516. doi:10.1056/NEJMoa022252. PMID 12815136.
- ↑ Bennett DA, Schneider JA, Tang Y, Arnold SE, Wilson RS (2006). "The effect of social networks on the relation between Alzheimer's disease pathology and level of cognitive function in old people: a longitudinal cohort study". Lancet Neurol. 5 (5): 406–412. doi:10.1016/S1474-4422(06)70417-3. PMID 16632311.
- ↑ Bialystok E, Craik FIM, Freedman M (2007). "Bilingualism as a protection against the onset of symptoms of dementia". Neuropsychologia. 42 (2): 459–464. doi:10.1016/j.neuropsychologia.2006.10.009.
- ↑ Geula C, Mesulam MM (1995). "Cholinesterases and the pathology of Alzheimer disease". Alzheimer Dis Assoc Disord. 9 Suppl 2: 23–8. PMID 8534419.
- ↑ Stahl SM (2000). "The new cholinesterase inhibitors for Alzheimer's disease, Part 2: illustrating their mechanisms of action". J Clin Psychiatry. 61 (11): 813–814. PMID 11105732.
- ↑ "Donepezil". US National Library of Medicine (Medline). 2007-01-08. Retrieved 2008-03-20.
- ↑ "Galantamine". US National Library of Medicine (Medline). 2007-01-08. Retrieved 2008-03-20.
- ↑ "Rivastigmine". US National Library of Medicine (Medline). 2007-01-08. Retrieved 2008-03-20.
- ↑ "Rivastigmine Transdermal". US National Library of Medicine (Medline). 2007-01-08. Retrieved 2008-03-20.
- ↑ Birks J (2006). "Cholinesterase inhibitors for Alzheimer's disease". Cochrane Database Syst Rev (1): CD005593. doi:10.1002/14651858.CD005593. PMID 16437532.
- ↑ Birks J, Harvey RJ (2006). "Donepezil for dementia due to Alzheimer's disease". Cochrane Database Syst Rev (1): CD001190. doi:10.1002/14651858.CD001190.pub2. PMID 16437430.
- ↑ Raschetti R, Albanese E, Vanacore N, Maggini M (2007). "Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials". PLoS Med. 4 (11): e338. doi:10.1371/journal.pmed.0040338. PMID 18044984.
- ↑ "Aricept and Aricept ODT Product Insert" (PDF). Eisai and Pfizer. Retrieved 2008-01-30.
- ↑ "Razadyne ER U.S. Full Prescribing Information" (PDF). Ortho-McNeil Neurologics. Retrieved 2008-02-19.
- ↑ "Exelon ER U.S. Prescribing Information" (PDF). Novartis Pharmaceuticals. Retrieved 2008-02-19.
- ↑ "Exelon U.S. Prescribing Information" (PDF). Novartis Pharmaceuticals. Retrieved 2008-02-21.
- ↑ 151.0 151.1 Lipton SA (2006). "Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond". Nat Rev Drug Discov. 5 (2): 160–170. doi:10.1038/nrd1958. PMID 16424917.
- ↑ "Memantine". US National Library of Medicine (Medline). 2004-01-04. Retrieved 2008-03-22.
- ↑ Areosa Sastre A, McShane R, Sherriff F (2004). "Memantine for dementia". Cochrane Database Syst Rev (4): CD003154. doi:10.1002/14651858.CD003154.pub2. PMID 15495043.
- ↑ "Namenda Prescribing Information" (PDF). Forest Pharmaceuticals. Retrieved 2008-02-19.
- ↑ Raina P, Santaguida P, Ismaila A; et al. (2008). "Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline". Annals of Internal Medicine. 148 (5): 379–397. PMID 18316756.
- ↑ Ballard C, Waite J (2006). "The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease". Cochrane Database Syst Rev (1): CD003476. doi:10.1002/14651858.CD003476.pub2. PMID 16437455.
- ↑ Ballard C, Lana MM, Theodoulou M; et al. (2008). "A Randomised, Blinded, Placebo-Controlled Trial in Dementia Patients Continuing or Stopping Neuroleptics (The DART-AD Trial)". PLoS Med. 5 (4): e76. doi:10.1371/journal.pmed.0050076. PMID 18384230.
- ↑ Sink KM, Holden KF, Yaffe K (2005). "Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence". JAMA. 293 (5): 596–608. doi:10.1001/jama.293.5.596. PMID 15687315.
- ↑ 159.0 159.1 159.2 159.3 "Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias" (PDF). American Psychiatric Association. October 2007. doi:10.1176/appi.books.9780890423967.152139. Retrieved 2007-12-28.
- ↑ Bottino CM, Carvalho IA, Alvarez AM; et al. (2005). "Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study". Clin Rehabil. 19 (8): 861–869. doi:10.1191/0269215505cr911oa. PMID 16323385.
- ↑ Doody RS, Stevens JC, Beck C; et al. (2001). "Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 56 (9): 1154–1166. PMID 11342679.
- ↑ Hermans DG, Htay UH, McShane R (2007). "Non-pharmacological interventions for wandering of people with dementia in the domestic setting". Cochrane Database Syst Rev (1): CD005994. doi:10.1002/14651858.CD005994.pub2. PMID 17253573.
- ↑ Robinson L, Hutchings D, Dickinson HO; et al. (2007). "Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review". Int J Geriatr Psychiatry. 22 (1): 9–22. doi:10.1002/gps.1643. PMID 17096455.
- ↑ Woods B, Spector A, Jones C, Orrell M, Davies S (2005). "Reminiscence therapy for dementia". Cochrane Database Syst Rev (2): CD001120. doi:10.1002/14651858.CD001120.pub2. PMID 15846613.
- ↑ Peak JS, Cheston RI (2002). "Using simulated presence therapy with people with dementia". Aging Ment Health. 6 (1): 77–81. doi:10.1080/13607860120101095. PMID 11827626.
- ↑ Camberg L, Woods P, Ooi WL; et al. (1999). "Evaluation of Simulated Presence: a personalised approach to enhance well-being in persons with Alzheimer's disease". J Am Geriatr Soc. 47 (4): 446–452. PMID 10203120.
- ↑ Neal M, Briggs M (2003). "Validation therapy for dementia". Cochrane Database Syst Rev (3): CD001394. doi:10.1002/14651858.CD001394. PMID 12917907.
- ↑ Chung JC, Lai CK, Chung PM, French HP (2002). "Snoezelen for dementia". Cochrane Database Syst Rev (4): CD003152. doi:10.1002/14651858.CD003152. PMID 12519587.
- ↑ Spector A, Orrell M, Davies S, Woods B (2000). "WITHDRAWN: Reality orientation for dementia". Cochrane Database Syst Rev (3): CD001119. doi:10.1002/14651858.CD001119.pub2. PMID 17636652.
- ↑ Spector A, Thorgrimsen L, Woods B; et al. (2003). "Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial". Br J Psychiatry. 183: 248–254. doi:10.1192/bjp.183.3.248. PMID 12948999.
- ↑ Gaugler JE, Kane RL, Kane RA, Newcomer R (2005). "Early community-based service utilization and its effects on institutionalization in dementia caregiving". Gerontologist. 45 (2): 177–85. PMID 15799982. Retrieved 2008-05-30. Unknown parameter
|month=ignored (help) - ↑ 172.0 172.1 172.2 Selwood A, Johnston K, Katona C, Lyketsos C, Livingston G (2007). "Systematic review of the effect of psychological interventions on family caregivers of people with dementia". Journal of Affective Disorders. 101 (1–3): 75–89. doi:10.1016/j.jad.2006.10.025. PMID 17173977.
- ↑ "Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias" (PDF). American Psychiatric Association. October 2007. doi:10.1176/appi.books.9780890423967.152139. Retrieved 2007-12-28.
- ↑ "Treating behavioral and psychiatric symptoms". Alzheimer's Association. 2006. Retrieved 2006-09-25.
- ↑ Wenger GC, Burholt V, Scott A (1998). "Dementia and help with household tasks: a comparison of cases and non-cases". Health Place. 4 (1): 33–44. doi:10.1016/S1353-8292(97)00024-5. PMID 10671009.
- ↑ Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A (2004). "Visual contrast enhances food and liquid intake in advanced Alzheimer's disease". Clinical Nutrition. 23 (4): 533–538. doi:10.1016/j.clnu.2003.09.015. PMID 15297089.
- ↑ "Clinical Trials. Found 459 studies with search of: alzheimer". US National Institutes of Health. Retrieved 2008-03-23.
- ↑ Vaccination:
- Hawkes CA, McLaurin J (2007). "Immunotherapy as treatment for Alzheimer's disease". Expert Reviews of Neurotherapy. 7 (11): 1535–1548. doi:10.1586/14737175.7.11.1535. PMID 17997702.
- Solomon B (2007). "Clinical immunologic approaches for the treatment of Alzheimer's disease". Expert Opin Investig Drugs. 16 (6): 819–828. doi:10.1517/13543784.16.6.819. PMID 17501694.
- Woodhouse A, Dickson TC, Vickers JC (2007). "Vaccination strategies for Alzheimer's disease: A new hope?". Drugs Aging. 24 (2): 107–119. doi:10.2165/00002512-200724020-00003. PMID 17313199.
- ↑ "Study Evaluating ACC-001 in Mild to Moderate Alzheimers Disease Subjects". Clinical Trial. [FDA clinicaltrials.gov]. 2008-03-11.
- ↑ "Study Evaluating Safety, Tolerability, and Immunogenicity of ACC-001 in Subjects With Alzheimer's Disease".
- ↑ "Bapineuzumab in Patients With Mild to Moderate Alzheimer's Disease/ Apo_e4 non-carriers". Clinical Trial. US National Institutes of Health. 2008-02-29. Retrieved 2008-03-23.
- ↑ "Efficacy Study of MPC-7869 to Treat Patients With Alzheimer's". Clinical Trial. US National Institutes of Health. 2007-12-11. Retrieved 2008-03-23.
- ↑ "Safety, Tolerability and Efficacy Study to Evaluate Subjects With Mild Cognitive Impairment". Clinical Trial. US National Institutes of Health. 2008-03-11. Retrieved 2008-03-23.
- ↑ "Study Evaluating the Safety, Tolerability and Efficacy of PBT2 in Patients With Early Alzheimer's Disease". Clinical Trial. US National Institutes of Health. 2008-01-13. Retrieved 2008-03-23.
- ↑ Tobinick E, Gross H, Weinberger A, Cohen H (2006). "TNF-alpha modulation for treatment of Alzheimer's disease: a 6-month pilot study". MedGenMed. 8 (2): 25. PMID 16926764.
- ↑ Griffin WS (2008). "Perispinal etanercept: potential as an Alzheimer therapeutic". J Neuroinflammation. 5: 3. doi:10.1186/1742-2094-5-3. PMID 18186919.
- ↑ Tobinick E (2007). "Perispinal etanercept for treatment of Alzheimer's disease". Curr Alzheimer Res. 4 (5): 550–552. doi:10.2174/156720507783018217. PMID 18220520.
- ↑ 188.0 188.1 Bowen JD, Malter AD, Sheppard L; et al. (1996). "Predictors of mortality in patients diagnosed with probable Alzheimer's disease". Neurology. 47 (2): 433–9. PMID 8757016. Unknown parameter
|month=ignored (help) - ↑ 189.0 189.1 Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M (2003). "Functional transitions and active life expectancy associated with Alzheimer disease". Arch. Neurol. 60 (2): 253–9. PMID 12580712. Unknown parameter
|month=ignored (help) - ↑ Larson EB, Shadlen MF, Wang L; et al. (2004). "Survival after initial diagnosis of Alzheimer disease". Ann. Intern. Med. 140 (7): 501–9. PMID 15068977. Unknown parameter
|month=ignored (help) - ↑ Jagger C, Clarke M, Stone A (1995). "Predictors of survival with Alzheimer's disease: a community-based study". Psychol Med. 25 (1): 171–7. PMID 7792352. Unknown parameter
|month=ignored (help) - ↑ 192.0 192.1 Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST (2005). "Alzheimer disease and mortality: a 15-year epidemiological study". Arch. Neurol. 62 (5): 779–84. doi:10.1001/archneur.62.5.779. PMID 15883266. Unknown parameter
|month=ignored (help) - ↑ Sloane PD, Zimmerman S, Suchindran C, Reed P, Wang L, Boustani M, Sudha S (2002). "The public health impact of Alzheimer's disease, 2000–2050: potential implication of treatment advances". Annual Review of Public Health. 23: 213–231. doi:10.1146/annurev.publhealth.23.100901.140525. PMID 11910061.
- ↑ O’Donovan ST. "Dementia caregiving burden and breakdown" (PDF). Forum of Consultant Nurses, Midwives and Allied Health Professionals. Retrieved 2008-02-29.
- ↑ "The MetLife Study of Alzheimer's Disease: The Caregiving Experience" (PDF). MetLife Mature Market Institute. August 2006. Retrieved 2008-02-12.
Further reading
- Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, Mittman B (2002). "Guidelines for managing Alzheimer's disease: Part I. Assessment". American Family Physician. 65 (11): 2263–2272. PMID 12074525.
- Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, Mittman B (2002). "Guidelines for managing Alzheimer's disease: Part II. Treatment". American Family Physician. 65 (12): 2525–2534. PMID 12086242.
- "Genes, lifestyles, and crossword puzzles: Can Alzheimer's disease be prevented" (PDF). US Department of Health and Human Services, National Institute of Aging. Retrieved 2008-02-29.
- Russell D, Barston S, White M (2007-12-19). "Alzheimer's Behavior Management: Learn to manage common behavior problems". helpguide.org. Retrieved 2008-02-29.
Template:Diseases of the nervous system
af:Alzheimer se siekte
ar:ألزهايمر
ast:Alzheimer
bg:Болест на Алцхаймер
ca:Malaltia d'Alzheimer
cs:Alzheimerova choroba
da:Alzheimers sygdom
de:Alzheimer-Krankheit
eo:Alchajmero
eu:Alzheimer
fa:آلزایمر
gl:Alzheimer
ko:알츠하이머병
hy:Ալցհայմերի հիվանդություն
hr:Alzheimerova bolest
id:Alzheimer
is:Alsheimer
it:Morbo di Alzheimer
he:אלצהיימר
lb:Alzheimer
lt:Alzheimerio liga
hu:Alzheimer-kór
ms:Alzheimer
nl:Ziekte van Alzheimer
no:Alzheimers sykdom
simple:Alzheimer's disease
sk:Alzheimerova choroba
sr:Алцхајмерова болест
su:Panyakit Alzheimer
fi:Alzheimerin tauti
sv:Alzheimers sjukdom
uk:Хвороба Альцгеймера
yi:אלצהיימערס קרענק
- Pages with reference errors
- Pages with citations using unsupported parameters
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- Pages using citations with accessdate and no URL
- CS1 maint: Unrecognized language
- CS1 maint: Extra text: authors list
- CS1 errors: DOI
- CS1 maint: Date and year
- CS1 errors: dates
- Alzheimer's disease
- Aging-associated diseases
- Neurological disorders
- Unsolved problems in neuroscience
- Eponyms
- Ailments of unknown etiology
- Geriatrics