Lymphadenopathy
| Lymphadenopathy | |
 | |
|---|---|
| Lymphadenopathy | |
| ICD-10 | I88, L04, R59.1 |
| ICD-9 | 289.1-289.3, 683, 785.6 |
| DiseasesDB | 22225 |
| MeSH | D008206 |
|
WikiDoc Resources for Lymphadenopathy |
|
Articles |
|---|
|
Most recent articles on Lymphadenopathy Most cited articles on Lymphadenopathy |
|
Media |
|
Powerpoint slides on Lymphadenopathy |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Lymphadenopathy at Clinical Trials.gov Trial results on Lymphadenopathy Clinical Trials on Lymphadenopathy at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Lymphadenopathy NICE Guidance on Lymphadenopathy
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Lymphadenopathy Discussion groups on Lymphadenopathy Patient Handouts on Lymphadenopathy Directions to Hospitals Treating Lymphadenopathy Risk calculators and risk factors for Lymphadenopathy
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Lymphadenopathy |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information on this page, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Synonyms and keywords: Lymph nodes enlarged, enlarged lymph nodes, lymphadenitis, swollen/enlarged lymph nodes
Overview
Lymphadenopathy is a term meaning "disease of the lymph nodes." It is, however, almost synonymously used with "swollen/enlarged lymph nodes". When the infection is of the lymph nodes themselves, it is called lymphadenitis, but when the infection is of the lymph channels, it is called lymphangitis.
Classification
Depending upon the involvement of the lymph nodes, lymphadenopathy is classified as 3 types.
- Localized lymphadenopathy : due to localized spot of infection e.g. an infected spot on the scalp will cause lymph nodes in the neck on that same side to swell up
- Generalized lymphadenopathy : due to generalized infection all over the body e.g. influenza
- Persistent generalized lymphadenopathy (PGL) : persisting for a long time, possibly without an apparent cause
- Dermatopathic lymphadenopathy : lymphadenopathy associated with skin disease.Tangier disease (ABCA1 deficiency) may also cause this.
Pathophysiology
- If an infection remains untreated, the center of the node may become necrotic, resulting in the accumulation of fluid and debris within the structure. This is known as an abscess and feels a bit like a tensely filled balloon or grape (a.k.a. fluctuance). Knowledge of which nodes drain specific areas will help search efficiently. Following infection, lymph nodes occasionally remain permanently enlarged, though they should be non-tender, small (less the 1 cm), have a rubbery consistency. It is common, for example, to find small, palpable nodes in the submandibular/tonsilar region of otherwise healthy individuals. This likely represents sequelae of past pharyngitis or dental infections.
- Malignancies may also involve the lymph nodes, either primarily (e.g. lymphoma) or as a site of metastasis. In either case, these nodes are generally firm, non-tender, matted (i.e. stuck to each other), fixed (i.e. not freely mobile but rather stuck down to underlying tissue), and increase in size over time. The location of the lymph node may help to determine the site of malignancy. Diffuse, bilateral involvement suggests a systemic malignancy (e.g. lymphoma) while those limited to a specific anatomic region are more likely associated with a local problem. Enlargement of nodes located only on the right side of the neck in the anterior cervical chain, for example, would be consistent with a squamous cell carcinoma, frequently associated with an intra-oral primary cancer.
- Diffuse upper airway infections (e.g. mononucleosis), systemic infections (e.g. tuberculosis) and inflammatory processes (e.g. sarcoidosis) can also cause lymphadenopathy (i.e. lymph node enlargement). This can be either symmetric or asymmetric.
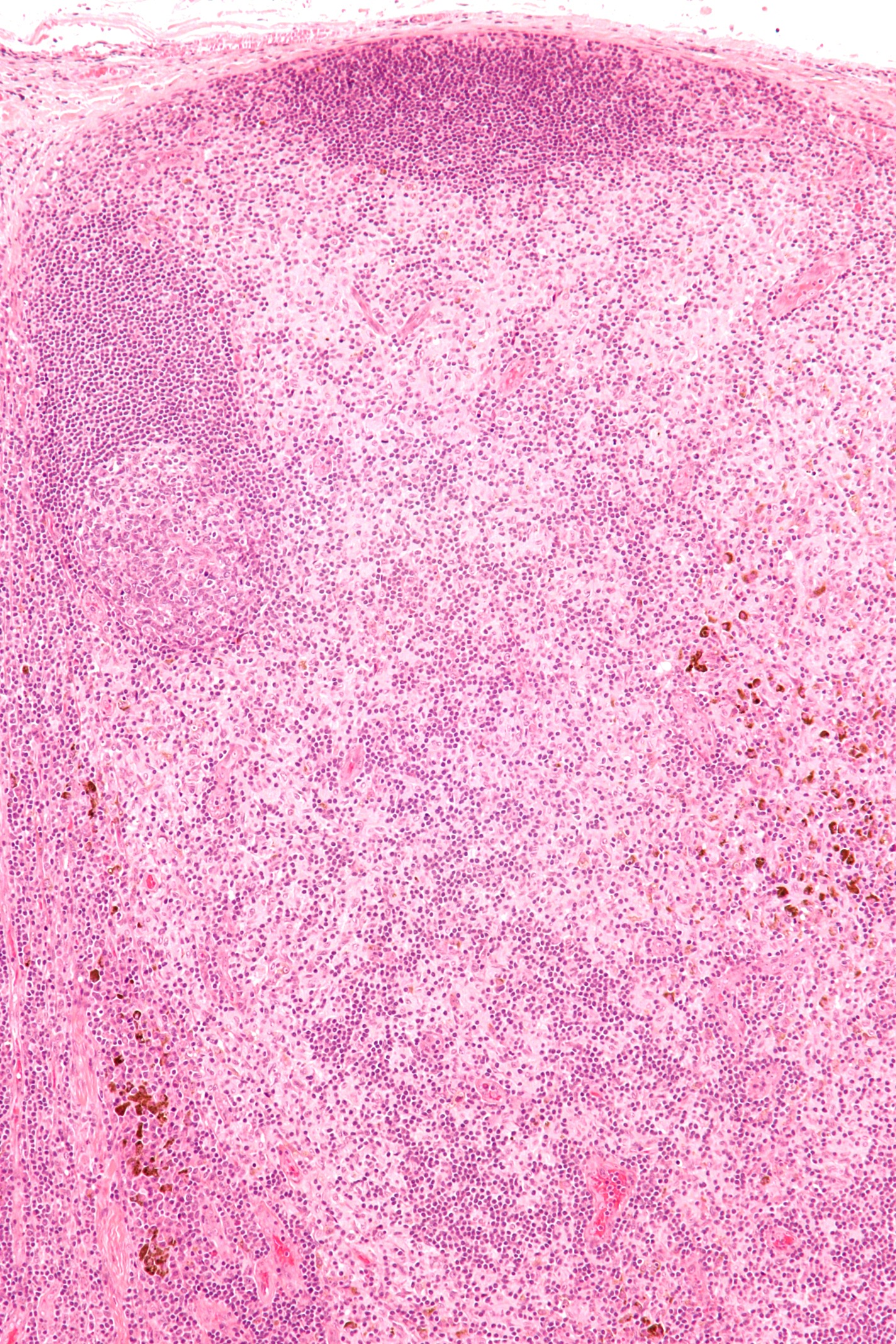
Microscopic pathology
Patterns of Benign (Reactive) Lymphadenopathy
There are three distinct patterns of benign lymphadenopathy:
- Follicular hyperplasia. Seen in infections, autoimmune disorders, and nonspecific reactions.
- Paracortical hyperplasia. Seen in viral infections, skin diseases, and nonspecific reactions.
- Sinus histiocytosis. Seen in lymph nodes draining limbs, inflammatory lesions, and malignancies.
Causes
Common Causes
- Acute infections (e.g. bacterial, or viral)
- Chronic infections (e.g tuberculous lymphadenitis, cat-scratch disease). Infectious mononucleosis is an acute viral infection, the hallmark of which is marked enlargement of the cervical lymph nodes.
- Toxoplasmosis, a parasitic disease, gives a generalized lymphadenopathy[1]
- Hodgkin lymphoma, non-Hodgkin lymphoma, hairy cell leukemia, give lymphadenopathy in all or a few lymph nodes [1]
- Metastasis
- Sarcoidosis
- Systemic lupus erythematosus (SLE)
- Rheumatoid arthritis
- AIDS - generalized lymphadenopathy is an early sign of infection with human immunodeficiency virus (HIV), the virus that causes acquired immunodeficiency syndrome (AIDS). "Lymphadenopathy syndrome" has been used to describe the first symptomatic stage of HIV progression, preceding AIDS-related complex and full-blown AIDS.[2]
Causes by Organ System
Causes in Alphabetical Order[3] [4]
|
|
Bihilar lymphadenopathy
The causes can divide into the four commonest:
- Tuberculosis
- Sarcoidosis
- Lymphoma
- Other malignancies
Less common causes include:
Differentiating from other diseases
Epidemiology and Demogaphics
The estimated incidence of lymphadenopathy in children in the United States ranges from 35% - 45%.
It is more common in the pediatric population.
Race and gender have no predilection in lymphadenopathy incidence.
Risk factors
Natural History, Complications and Prognosis
Natural History
The natural course of lymphadenopathy depends on the underlying cause. Lymphadenopathy due to infectious causes subsides once the infection is controlled.
Complications
- Mediastinal lymphadenopathy causes pressure symptoms like:
- Superior vena cava syndrome
- Tracheal and bronchial obstruction
- Dysphagia
- Hemoptysis
- Uric acid nephropathy
- Hyperkalemia
- Hypercalcemia
- Hypocalcemia
- Hyperphosphatemia
- Renal failure
Prognosis
Prognosis of lymphadenopathy depends entirely on the underlying etiology. Cancerous causes of lymphadenopathy have a poor prognosis compared to the infectious causes.
Diagnosis
Symptoms
Lymphadenopathy can present as
- Lump in the neck (e.g in tumors, sarcoidosis).
- Red, tender skin over lymph node.
- Swollen, tender, or hard lymph nodes.
Physical Examination
The major lymph node groups are located along the anterior and posterior aspects of the neck and on the underside of the jaw. If the nodes are quite big, you may be able to see them bulging under the skin, particularly if the enlargement is asymmetric (i.e. it will be more obvious if one side is larger then the other). To palpate, use the pads of all four fingertips as these are the most sensitive parts of your hands. Examine both sides of the head simultaneously, walking your fingers down the area in question while applying steady, gentle pressure. The major groups of lymph nodes as well as the structures that they drain, are listed below. The description of drainage pathways are rough approximations as there is frequently a fair amount of variability and overlap.
Palpating Anterior Cervical Lymph Nodes
Nodes are generally examined in the following order:
- Anterior Cervical (both superficial and deep): Nodes that lie both on top of and beneath the sternocleidomastoid muscles (SCM) on either side of the neck, from the angle of the jaw to the top of the clavicle. This muscle allows the head to turn to the right and left. The right SCM turns the head to the left and vice versa. They can be easily identified by asking the patient to turn their head into your hand while you provide resistance. Drainage: The internal structures of the throat as well as part of the posterior pharynx, tonsils, and thyroid gland.
- Posterior Cervical: Extend in a line posterior to the SCMs but in front of the trapezius, from the level of the mastoid bone to the clavicle. Drainage: The skin on the back of the head. Also frequently enlarged during upper respiratory infections (e.g. mononucleosis).
- Tonsillar: Located just below the angle of the mandible. Drainage: The tonsilar and posterior pharyngeal regions.
- Sub-Mandibular: Along the underside of the jaw on either side. Drainage: The structures in the floor of the mouth.
- Sub-Mental: Just below the chin. Drainage: The teeth and intra-oral cavity.
- Supra-clavicular: In the hollow above the clavicle, just lateral to where it joins the sternum. Drainage: Part of the throacic cavity, abdomen.
A number of other lymph node groups exist. However, palpation of these areas is limited to those situations when a problem is identified in that specific region (e.g. the pre-auricular nodes, located in front of the ears, may become inflamed during infections of the external canal of the ear).
Lymph nodes are part of the immune system. As such, they are most readily palpable when fighting infections. Infections can either originate from the organs that they drain or primarily within the lymph node itself, referred to as lymphadenitis. Infected lymph nodes tend to be:
- Firm, tender, enlarged and warm. Inflammation can spread to the overlying skin, causing it to appear reddened.
Malignancies may also involve the lymph nodes, either primarily (e.g. lymphoma) or as a site of metastasis. In either case, these nodes are generally:
- Firm, non-tender, matted (i.e. stuck to each other), fixed (i.e. not freely mobile but rather stuck down to underlying tissue), and increase in size over time.
Case Studies in Physical Examination
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
-
Cervical Adenopathy: Massive right side cervical adenopathy and facial assymetry due to metastatic, intraoral squamous cell cancer.
-
Cervical Adenopathy: Massive right side cervical adenopathy and facial assymetry due to metastatic, intraoral squamous cell cancer.
-
Cervical Adenopathy: Large right anterior cervical lymph node.
-
Cervical Adenopathy: Multiple right sided cervical lymph nodes.
Laboratory Findings
Imaging
Chest X Ray
Bihilar lymphadenopathy is a radiographic term that describes the enlargement of mediastinal lymph nodes. It is easily and most commonly identified by a chest x-ray.
-
Sarcoidosis bilateral hilar lymphadenopathy, non-caseating granulomas[14]
CT

Biopsy
The test is used to diagnose cancer or an infection:
- When the doctor feels swollen glands and they do not go away
- When lymph nodes are present on a CT or MRI scan
- For some patients with breast cancer or melanoma, to see if the cancer has spread (sentinel lymph node biopsy)
References
- ↑ 1.0 1.1 Status and anamnesis, Anders Albinsson. Page 12
- ↑ Chris Jennings (1993). "Understanding and Preventing AIDS: A Book for Everyone".
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Blum JA, Neumayr AL, Hatz CF (2012). "Human African trypanosomiasis in endemic populations and travellers". Eur. J. Clin. Microbiol. Infect. Dis. 31 (6): 905–13. doi:10.1007/s10096-011-1403-y. PMID 21901632. Unknown parameter
|month=ignored (help) - ↑ Beukes CA, Thiart J (2012). "The incidence of human herpes virus-8 expression in lymph node biopsies from human immunodeficiency virus-positive patients". Histopathology. doi:10.1111/j.1365-2559.2012.04291.x. PMID 22716315. Unknown parameter
|month=ignored (help) - ↑ Mitsuhashi K, Shiseki M, Ishiyama M; et al. (2011). "[Angioimmunoblastic T-cell lymphoma with marked polyclonal plasmacytosis in peripheral blood and bone marrow mimicking plasma cell leukemia]". Rinsho Ketsueki (in Japanese). 52 (7): 563–9. PMID 21821991. Unknown parameter
|month=ignored (help) - ↑ Simonelli S, Gianazza E, Mombelli G; et al. (2012). "Severe high-density lipoprotein deficiency associated with autoantibodies against lecithin:cholesterol acyltransferase in non-Hodgkin lymphoma". Arch. Intern. Med. 172 (2): 179–81. doi:10.1001/archinternmed.2011.661. PMID 22271127. Unknown parameter
|month=ignored (help) - ↑ Simesen de Bielke MG, Yancoski J, Rocco C; et al. (2012). "A Missense Mutation in the Extracellular Domain of Fas: The Most Common Change in Argentinean Patients with Autoimmune Lymphoproliferative Syndrome Represents a Founder Effect". J Clin Immunol. doi:10.1007/s10875-012-9731-y. PMID 22752343. Unknown parameter
|month=ignored (help) - ↑ Schleenvoigt BT, Keller P, Stallmach A, Pletz MW (2012). "[African tick bite fever--rickettsiosis after holiday in South Africa]". Dtsch. Med. Wochenschr. (in German). 137 (17): 891–3. doi:10.1055/s-0032-1304902. PMID 22511280. Unknown parameter
|month=ignored (help) - ↑ Roushan MR, Amiri MJ (2012). "Update on Childhood Brucellosis". Recent Pat Antiinfect Drug Discov. PMID 22812616. Unknown parameter
|month=ignored (help) - ↑ Dispenzieri A, Armitage JO, Loe MJ; et al. (2012). "The clinical spectrum of Castleman's disease". Am J Hematol. doi:10.1002/ajh.23291. PMID 22791417. Unknown parameter
|month=ignored (help) - ↑ Chondrogiannis K, Vezakis A, Derpapas M, Melemeni A, Fragulidis G (2012). "Seronegative cat-scratch disease diagnosed by PCR detection of Bartonella henselae DNA in lymph node samples". Braz J Infect Dis. 16 (1): 96–9. PMID 22358366.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
de:Lymphadenopathie
he:לימפדנופתיה
id:Limfadenopati
lt:Limfadenitas




![Sarcoidosis bilateral hilar lymphadenopathy, non-caseating granulomas[14]](/images/3/3c/Sarcoidosis_Lymphadenopathy.jpg)