Leptospirosis differential diagnosis

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Venkata Sivakrishna Kumar Pulivarthi M.B.B.S [2]
Overview
Leptospirosis must be differentiated from other diseases that cause fever, diarrhea, nausea and vomiting, such as ebola, typhoid fever, malaria, yellow fever, and other enteric bacterial infections. Moderate to severe leptospirosis must be differentiated from dengue fever.
Differential diagnosis
Differential diagnosis list for leptospirosis is very large due to diverse symptomatics. For forms with middle to high severity, the list includes dengue fever and other hemorrhagic fevers, hepatitis of various etiologies, viral meningitis, malaria and typhoid fever. Light forms should be distinguished from influenza and other related viral diseases. Specific tests are a must for proper diagnosis of leptospirosis. Under circumstances of limited access (e.g., developing countries) to specific diagnostic means, close attention must be paid to anamnesis of the patient. Factors like certain dwelling areas, seasonality, contact with stagnant water (swimming, working on flooded meadows, etc) and/or rodents in the medical history support the leptospirosis hypothesis and serve as indications for specific tests (if available).
Differential Diagnosis for Hemorrhagic fever
| Disease | Incubation period | Vector | Symptoms | Physical signs | Lab findings | Other findings | Treatment | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Cough | Rash | Joint pain | Myalgia | Diarrhea | Common hemorrhagic symptoms | Characterestic physical finding | Icterus | Plasma Creatine kinase | Confirmatory test | |||||
| Leptospirosis | 2 to 30 days | Rodents
Domestic animals |
Fever last for 4-7 days, remission for 1-2 days and then relapse | + | Present over legs Hemorrhagic rash | + | +
(Severe myalgia is characteristic of leptospirosis typically localized to the calf and lumbar areas) |
+ | Conjunctival hemorrhage, | Conjunctival suffusion | + | Elevated | Microscopic agglutination test of urine | History of exposure to soil or water
contaminated by infected rodents Recent history travel to tropical, sub tropical areas or humid areas |
NSAIDs |
| Dengue | 4 to 10 days | Aedes mosquito | Fever last for 1-2 days,
remission for 1-2 days and then relapse for 1-2 days (Biphasic fever pattern) |
- | Over legs and trunk
pruritic rash May be hemorrhagic |
+ | + | - | Upper gastrointestinal bleeding | Painful lymphadenopathy | - | Normal | Serology showing positive IgM or IgG | Recent travel to South America, Africa, Southeast Asia | Supportive care
Avoid aspirin and other NSAIDs |
| Malaria |
|
Female Anopheles | Fever present daily or on alternate day or every 3 days depending on Plasmodium sps. | - | No rash | - | + | - | Bloody urine | Hepatosplenomegaly | + | Normal | Giemsa stained thick and thin blood smears | Recent travel to South America, Africa, Southeast Asia | Anti malarial regimen |
| Ebola | 2 to 21 days. | No vector
Human to human transmission |
+ | + | Maculopapular
non-pruritic rash with erythema Centripetal distribution |
+ | + | +
May be bloody in the early phase |
Epistaxis | Sudden onset of high fever with conjunctival injection and early gastrointestinal symptoms | - | Normal | RT-PCR | Recent visit to endemic area especially African countries | Isolation of the patient,
supportive therapy |
| Influenza | 1-4 days | No vector | + | + | +/- | + | + | + | - | Fever and upper respiratory symptoms | - | Normal | Viral culture or PCR | Health care workers
Patients with co-morbid conditions |
Symptomatic treatment |
| Yellow fever | 3 to 6 days | Aedes or Haemagogus species mosquitoes | + | + | - | - | + | - | Conjunctival hemorrhage, | Relative bradycardia | + | Normal | RT-PCR, | Recent travel to Africa, South and Central America, and the Caribbean.
Tropical rain forests of south America |
Symptomatic treatment, |
| Typhoid fever | 6 to 30 days | No vector | + | - | Blanching erythematous
maculopapularlesions on the lower chest and abdomen |
+ | + | + | Intestinal bleeding | Rose spots | - | Normal | Blood or stool culture showing salmonella typhi sps. | Residence in endemic area
Recent travel to endemic area |
Fluoroquinolones, |
Differentiating psittacosis from other diseases
| Clinical feature | Cough | Sputum | Dyspnea | Sore throat | Headache | Confusion | Diarrhea | Chest radiograph changes | Hyponatremia | Leukopenia | Abnormal Liver function tests | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psittacosis | ++ | - | + | - | +++ | + | Minimal |
|
- | + | - | Doxycycline |
| C.pneumoniae pneumonia | + | + | + | +++ | ++ | + | - |
|
- | - | - | Doxycycline, Azithromycin |
| M. pneumoniae pneumonia | ++ | ++ | ++ | - | - | - | - |
|
- | - | + | Doxycycline |
| L. Pneumophila infection | + | +++ | +++ | - | + | ++ | + | Often Multifocal | ++ | + | ++ | Doxycycline |
| Influenza | ++ | ++ | ++ | ++ | ++ | +/- | +/- |
|
- | - | - | zanamivir, oseltamivir, |
| Endocarditis | ++ | ++ | + | - | - | - | - |
bases bilaterally |
- | +/- | +/- | Vancomycin |
| Coxiella burnetii infection | ++ | - | + | +/- | - | +/- | Minimal |
|
- | +/- | =/- | Doxycycline |
| Leptospirosis | ++ | + | ++ | + | + | ++ | - |
|
+++ | Doxycycline, azithromycin, amoxicillin | ||
| Brucellosis | ++ | - | + | - | ++ | + | - |
|
-/+ | +/- | +/- | Doxycycline, rifampin |
Key;
+, occurs in some cases
++, occurs in many cases,
+++, occurs frequently
Leptospirosis must be differentiated from other diseases that cause atypical pneumonia such as Q fever and legionella pneumonia:
| Disease | Prominent clinical features | Lab findings | Chest X-ray |
|---|---|---|---|
| Q fever |
|
 | |
| Mycoplasma pneumonia |
|
|
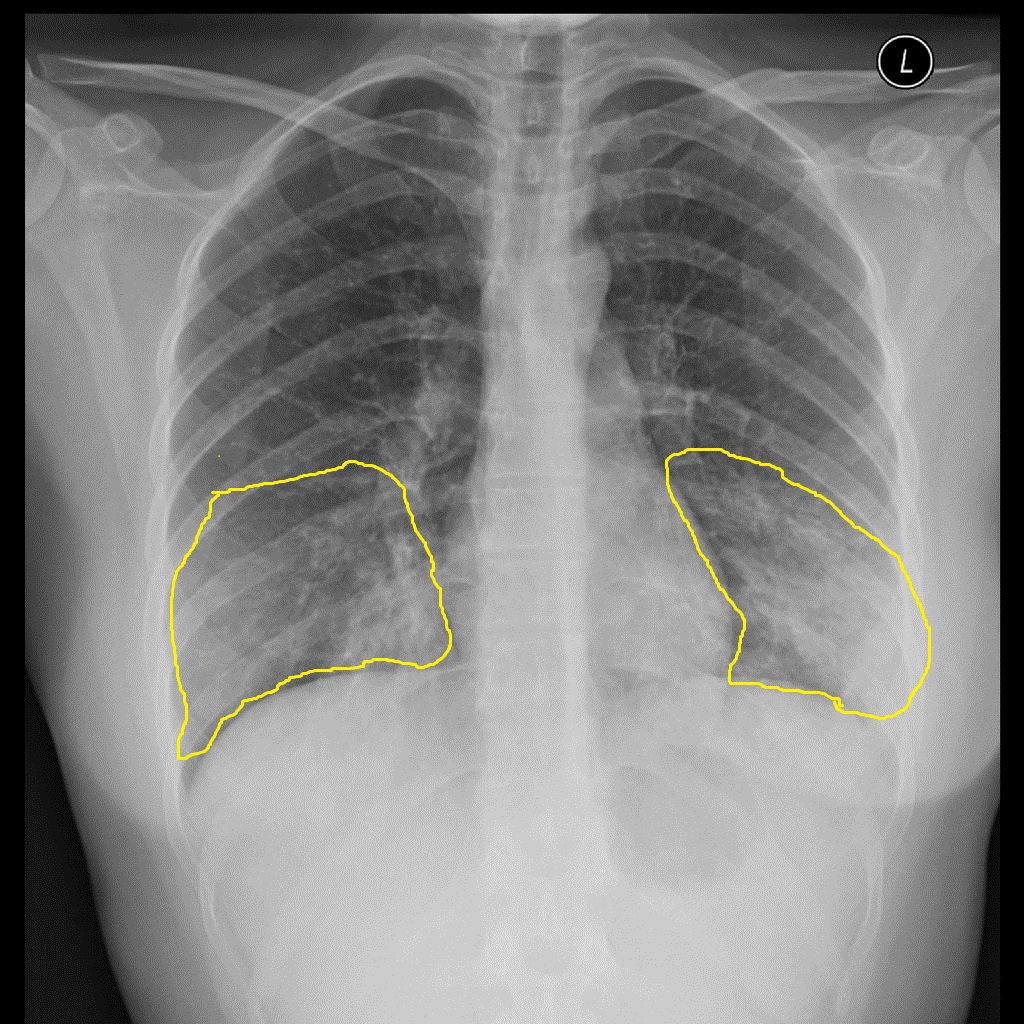 |
| Legionellosis |
|
|
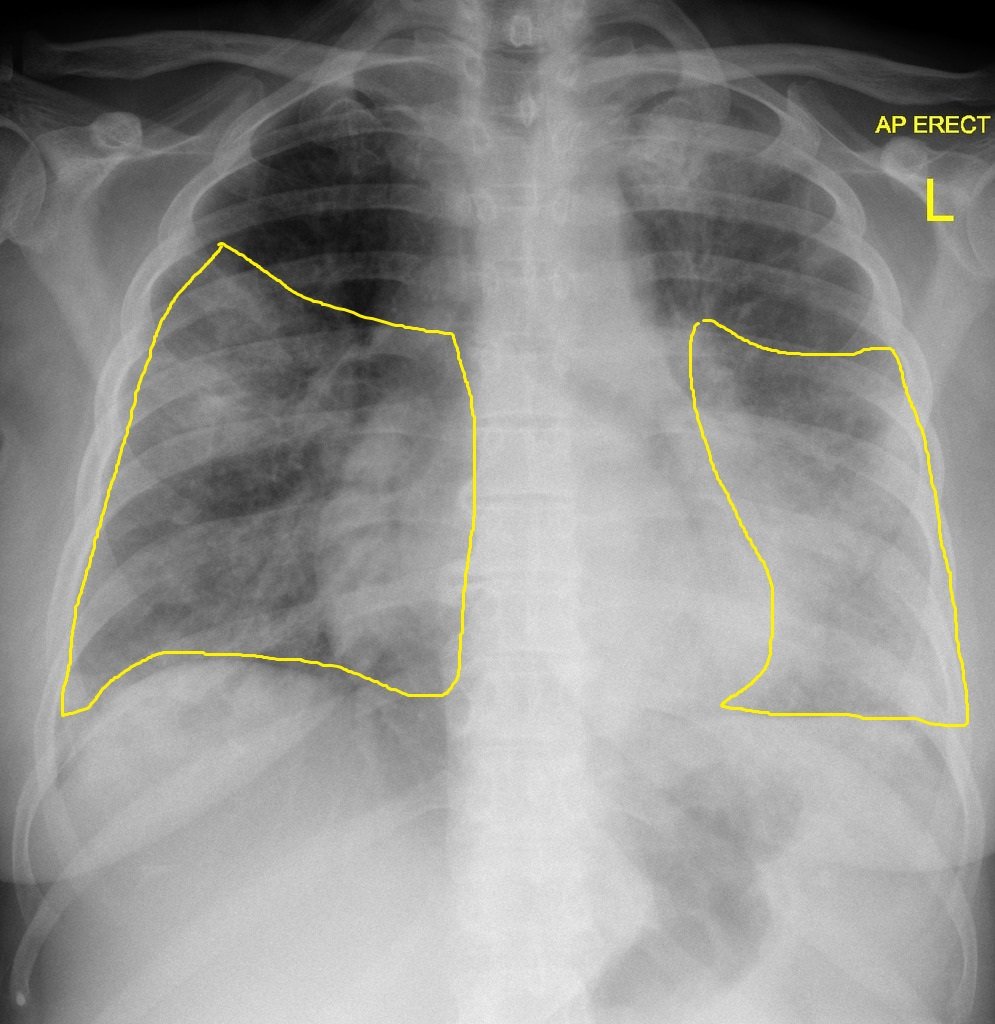 |
| Chlamydia pneumonia |
|
|
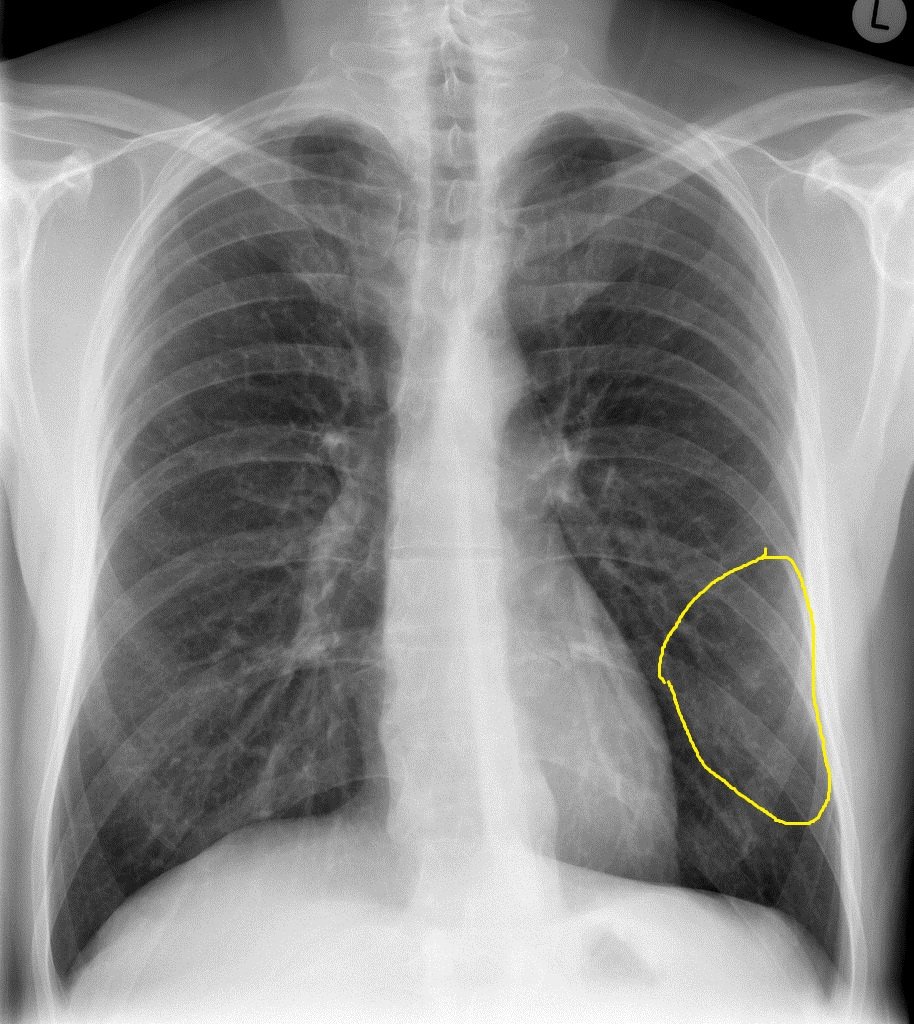 |