COVID-19-associated arrhythmia and conduction system disease
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Tayyaba Ali, M.D.[2]
Synonyms and keywords:COVID-19-associated dysrhythmia
Overview
An arrhythmia is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slowly, or with an irregular rhythm. When a heart beats too fast, the condition is called tachycardia. When a heart beats too slowly, the condition is called bradycardia. Cardiac arrhythmia is increasingly recognized as one of the earliest clinical manifestations of COVID-19. There is also anecdotal evidence of sudden cardiac death among COVID-19 patients. According to a study, 51 of 85 fatal cases of COVID-19 from Wuhan developed an arrhythmia, and 2 patients died of malignant arrhythmia. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) utilizes S-spike to bind to angiotensin-converting enzyme 2 (ACE2) receptors to enter the endothelial cells of the heart. The interaction between SARS-CoV-2 and ACE2 can bring about changes in ACE2 pathways prompting intense injury to the lung, heart, and endothelial cells. Hypoxia and electrolyte abnormalities that are common in the acute phase of severe COVID-19 can potentiate cardiac arrhythmias. COVID-19-associated arrhythmia findings include sinus tachycardia, atrial fibrillation, tachy-brady syndrome, sinus rhythm with a first-degree atrioventricular block (AVB) with SITIIIQIII and Sinus tachycardia with incomplete right bundle branch block. All patients with torsades de pointes (TdP) should be determined if they are hemodynamically stable or unstable through immediate evaluation of the symptoms, vital signs, and level of consciousness. Initial treatment with antiarrhythmic medications is not indicated for hemodynamically unstable or pulseless patients except intravenous (IV) magnesium. The clinical situation of a patient determines the rate of magnesium infusion. Infusion occurs over one to two minutes in patients with pulseless cardiac arrest. The infusion should occur over 15 minutes in patients without cardiac arrest as a rapid IV bolus of magnesium can result in hypotension and asystole. Some patients are given a continuous bolus of IV magnesium at a rate of 3 to 20 mg/min until the QT interval is below 0.50 seconds. The treatment for other arrhythmias in COVID-19 patients is the same as in patients with arrhythmias without COVID-19 infection.
To browse the complete chapter of COVID-19, click here.
Historical Perspective
- Diseases of heart and lung are the most common causes of COVID-19-related death.[1]
- Cardiac rhythm problems are increasingly recognized as a clinical manifestation of COVID-19.[2]
- There is also anecdotal evidence of sudden cardiac death among COVID-19 patients.[3] According to a study, 51 of 85 fatal cases of COVID-19 from Wuhan developed an arrhythmia, and 2 patients died of malignant arrhythmia.[4]
- In 137 subjects from Hubei province, 10 patients (7.3 percent) noted palpitations as one of the initial symptoms.[5]
To browse the historical perspective of COVID-19, click here.
Classification
- COVID-19-associated arrhythmia may be classified into two subtypes/groups based on the clinical presentation:
-
- COVID-19 patients with inherited arrhythmia syndromes are believed to be more liable to pro-arrhythmic consequences of SARS-CoV-2 such as stress, fever, use of antiviral medications and electrolyte disturbance.[6] which includes:
- To browse the classification of COVID-19, click here.
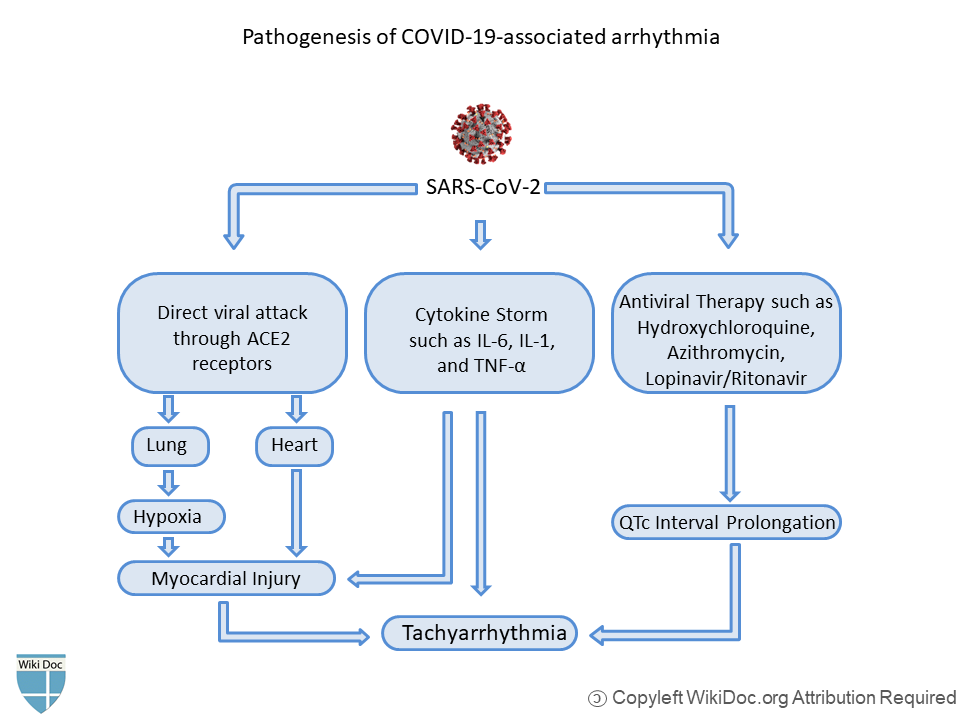
Pathophysiology
- Respiratory disease is the chief target of Coronavirus disease 2019 (COVID-19).
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) utilizes S-spike to bind to angiotensin-converting enzyme 2 (ACE2) receptors to enter the cells.
- Type 1 and type 2 pneumocytes exhibit ACE 2 receptors in the lung. Studies report that coronary endothelial cells in the heart and intrarenal endothelial cells and renal tubular epithelial cells in the kidney exhibit ACE2. ACE2 is an inverse regulator of the renin-angiotensin system.[7]
- The interaction between SARS-CoV-2 and ACE2 can bring about changes in ACE2 pathways prompting intense injury to the lung, heart, and endothelial cells. Hypoxia and electrolyte abnormalities that are common in the acute phase of severe COVID-19 can potentiate cardiac arrhythmias.
- Binding of SARS-CoV-2 to ACE2 receptors can result in hypokalemia which causes various types of arrhythmia.
- Elevated levels of cytokines as a result of the systemic inflammatory response of the severe Coronavirus disease 2019 (COVID-19) can cause injury to multiple organs, including cardiac myocytes.[8]In COVID-19 patients, excessive ranges of circulating cytokines, especially interleukin (IL)-6 is related to in-hospital death.[9]
- As a result of cytokine storm triggered by Sars-CoV-2 that includes IL-6, tumor necrosis factor (TNF) α, and IL-1, duration of ventricular action potential can be prolonged. Studies suggest that cytokine storm can modulate the function of cardiomyocyte ion channels such as Na+, K+ and Ca+ channels (inflammatory cardiac channelopathies).[10]
- According to the data based on studies on previous Severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) epidemic and the ongoing COVID-19 outbreak, multiple mechanisms have been suggested for cardiac damage.[11]
To browse the pathophysiology of COVID-19, click here.
Causes
SARS-CoV-2 causes COVID-19-associated arrhythmia through different mechanisms, including direct viral attack, cytokine storm, etc.
Common causes of arrhythmia include:
- Abnormal levels of potassium or other substances in the body
- Heart attack, or a damaged heart muscle from a past heart attack
- Heart disease that is present at birth (congenital)
- Heart failure or an enlarged heart
- Overactive thyroid gland[12]
To browse the causes of COVID-19, click here.
Differentiating COVID-19-associated arrhythmia from other Diseases
COVID-19-associated arrhythmia and conduction system disease must be differentiated from other diseases that cause arrhythmia, such as:
- Hyperkalemia[12]
- Hypokalemia[12]
- Congenital heart disease[12]
- Heart failure[12]
- Myocardial Infarction[12]
- Hyperthyroidism[12]
- Dehydration[13]
- Hypoglycemia[13]
- Hypocalcemia[13]
- Hypomagnesemia[13]
- Alcohol-induced cardiac arrhythmia[12]
- Caffeine-induced arrhythmia[12]
- Antihyperetnsive therapy-induced arrhythmia[12]
To browse the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- According to the available data on COVID-19-associated arrhythmia, the prevalence of arrhythmias and conduction system disease in patients with COVID-19 varies from population to population. The incidence of COVID-19-associated arrhythmia and conduction system disease in asymptomatic, mildly ill, critically ill, and recovered patients is not known.[3]
- According to a cohort of 137 COVID-19 patients from Hubei province, 10 patients were reported to have palpitations as one of the earliest symptoms.[5]
- In a cohort of 138 COVID-19 patients from Wuhan, arrhythmias were observed in 17 percent of hospitalized patients because of COVID-19-related pneumonia, and in 44 percent of patients admitted to an intensive care unit.[2]
- One-third of patients with the severe disease also reported other symptoms including arrhythmia. According to a study done in Wuhan, China, 16.7% of hospitalized and 44.4% of ICU patients with COVID-19 had arrhythmias.[14]
Age
- The prevalence of arrhythmia and Atrial Fibrillation increases with age.[15]
Gender
- There is not much data available to delineate the gender of COVID-19 patients prone to develop arrhythmia.
Race
- There is not enough data on a racial predilection for COVID-19-associated arrhythmia.
To browse the epidemiology and demographics of COVID-19, click here.
Risk Factors
- Common risk factors in the development of COVID-19-associated arrhythmia are:
- Patients who present with other cardiovascular complications in the setting of COVID-19 infection, such as myocardial injury or myocardial ischemia.[9]
- Patients with hypoxia, shock (septic or cardiogenic), or evidence of widespread systemic inflammation.[16]
- Patients with electrolyte disturbances (eg, hypokalemia).[17]
- Patients who are receiving QT-prolonging therapies and who may develop polymorphic ventricular tachycardia (VT).[16]
- Patients with fever, which can unmask cases of cardiac channelopathies such as Brugada syndrome and long QT syndrome.[18][19]
- To browse the risk factors of COVID-19 click here.
Screening
According to the National Heart, Lung, and Blood Institute, screening for arrhythmia is based on risk factors, such as age or family history.[13]
- An electrocardiogram (EKG or ECG) is the main test for detecting arrhythmia.
- An EKG records the heart’s electrical activity. The doctor may do the test while you are at rest or may do a stress test, which records the heart’s activity when it is working hard.
- The doctor may also give a portable monitor to wear for a day or several days if no arrhythmia was detected during testing in the clinic. If there is a child who is at risk of arrhythmia because of a genetic condition, the doctor may recommend regular testing for the child and his or her siblings.
- Genetic testing can help understand the risk when a family member has been diagnosed with a genetic condition. Testing is especially important if the newborn or another close relative died suddenly and had a genetic risk.
- The doctor may also suggest genetic testing if there is a history of fainting or have survived cardiac arrest or near-drowning.
- Imaging tests, such as cardiac magnetic resonance imaging (MRI), can help detect scarring or other problems that can increase the risk of arrhythmia.[13]
To browse the screening of COVID-19, click here.
Natural History, Complications and Prognosis
Natural History:
- Cardiac arrhythmia is considered as one of the earliest manifestations of COVID-19.[20]
- Arrhythmia presents with the history of:
- Slow or irregular heartbeat or pauses between heartbeats
- Skipping a heartbeat
- Heart pounding or racing
- Anxiety
- Blurred vision
- Chest pain
- Difficulty breathing
- Fainting or nearly fainting
- Foggy thinking
- Fatigue
- Sweating
- Weakness, dizziness, and light-headedness[13]
Complications
Arrhythmias that are unrecognized or left untreated can cause sometimes life-threatening complications affecting the heart and brain.[13]
- Heart failure. To browse COVID-19-associated heart failure, click here.
- Stroke. To browse COVID-19-associated stroke, Click here
- Sudden cardiac arrest. To browse COVID-19-associated cardiac arrest, click here
- Worsening arrhythmia.
Prognosis
- In-hospital death among patients with COVID-19-associated arrhythmia and conduction system disease is 4.3% according to a study by Wang et al[14] and 23% among COVID-19 patients who develop Ventricular fibrillation and Ventricular tachycardia according to a study by Guo et al [21] . According to the data available, the Arrhythmia rate is more frequent in Intensive care unit (ICU) patients.[14]
To browse COVID-19 history, complications, and prognosis, click here.
Diagnosis
Diagnostic Study of Choice
- ECG:
- Most patients with the severe COVID-19, and especially patients who receive QT-prolonging medications, should have a baseline electrocardiogram (ECG) performed at the time of admission to the hospital.The best technique to get the QT interval is with a 12-lead electrocardiogram (ECG). However, to scale back exposure to hospital workers, this could not perpetually be possible. A single-lead ECG might underestimate the QT interval, and there ought to be an effort to use a multiple-lead telemetry system to observe the QT interval.[22][23]
- Transthoracic echocardiography:
- Transthoracic echocardiography is recommended for an inpatient with heart failure, arrhythmia, ECG changes, or newly diagnosed cardiomegaly on chest x-ray or CT-chest.[24]
To browse the diagnostic study of choice of COVID-19, click here.
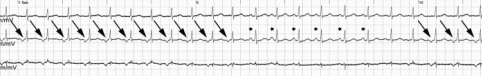
History and Symptoms
Arrhythmia or conduction system disease is the nonspecific clinical presentation of COVID-19. Patients may be tachycardic (with or without palpitations) in the setting of other COVID-19-related symptoms (eg, fever, shortness of breath, pain, etc).
- According to a study done in Hubei province,palpitations were reported as a presenting symptom by 7.3 percent of patients.[5][9]
- Sinus tachycardia
- Atrial fibrillation
- Tachy-brady syndrome.
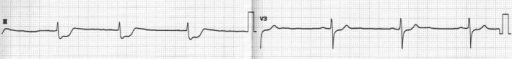
- Sinus rhythm with a first-degree atrioventricular block (AVB) with SITIIIQIII; Sinus tachycardia with incomplete right bundle branch block.[25][26]
To browse the history and symptoms of COVID-19, click here.
Physical Examination
- Patients with COVID-19-associated arrhythmia and conduction system disease on cardiac auscultation reveal tachycardia or arrhythmias (irregular beat).
- Sinus tachycardia, the most common type of arrhythmia in COVID-19 patients can be due to fever, hypoxia, shock due to sepsis, and anxiety. Some pathologic causes of arrhythmias include ventricular tachyarrhythmia, atrial fibrillation (pulse rate 100 to 175 bpm) and atrial flutter (pulse rate 150 bpm).[21]
- To browse the physical examination of COVID-19, click here.
Laboratory Findings
- There are no specific laboratory findings associated with COVID-19-associated arrhythmia.
- COVID-19 patients with elevated troponin T experienced higher risk of ventricular arrhythmias (17.3% in high troponin T group versus 1.5% in normal troponin T group, P < 0.001).[6]
To browse the laboratory findings of COVID-19, click here.
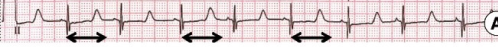
Electrocardiogram
COVID-19-associated arrhythmia findings include:
- Prolong QT Interval:
- According to a multicenter study done in New York that involved 4250 COVID-19 patients, 260 patients (6.1 percent) had corrected QT interval (QTc) >500 milliseconds at the time of admittance. However, in another study that involved 84 patients who got hydroxychloroquine and azithromycin, the baseline QTc interval was 435 milliseconds before receiving these medications.[27][28]
- Atrial Arrhythmia:
- According to a study, among 393 patients with COVID-19, atrial arrhythmias were more common among patients requiring invasive mechanical ventilation than noninvasive mechanical ventilation (17.7 versus 1.9 percent).[29]
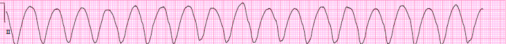
- Ventricular Arrhythmia:
- According to a study done in Wuhan, China. among 187 hospitalized patients with COVID-19, 11 patients (5.9 percent) developed ventricular tachyarrhythmias.[30]
- Cardiac Arrest:
- According to a Lombardia Cardiac Arrest Registry (Lombardia CARe) of the region Lombardia in Italy. Out of 9806 cases of COVID-19, 362 cases of out-of-hospital cardiac arrest were reported during the study time frame in 2020. During a similar period in 2019, 229 cases of out-of-hospital cardiac arrest were reported, which means an increment of 58% was observed in 2020 among COVID-19 patients. According to the records from a tertiary care hospital in Wuhan. Out of 761 patients with severe COVID-19, 151 patients developed in-hospital cardiac arrest. 136 patients received resuscitation. Out of 136 patients, 119 patients had a respiratory cause. 10 patients had a cardiac cause. 7 patients had other causes. Ventricular fibrillation or pulseless ventricular tachycardia was observed in 8 patients (5.9%), Pulseless electrical activity in 6 patients (4.4%), and asystole in 122 COVID-19 patients (89.7%).[31][32]
- To browse the electrocardiogram findings of COVID-19, click here.
X-Ray
- To browse the X-ray finding of COVID-19, click here.
Echocardiography/Ultrasound
- There are no specific echocardiography/ultrasound findings associated with coronavirus infection.
- Non specific echocardiographic findings can include:[33][34]
- Left ventricular systolic dysfunction
- Pericardial effusion
- Myocardial edema
- Increased wall thickness with diffuse biventricular hypokinesis
CT Scan
- To browse the CT-Scan findings of COVID-19, click here.
MRI
- We ought to consider that myocardial injury may bring about atrial or ventricular fibrosis, the substrate for resulting cardiovascular arrhythmias.
- COVID-19 patients with evidence of myocardial injury should undergo cardiac magnetic resonance to assess the extent of myocardial scar.[20]
- To browse the MRI findings of COVID, click here.
Other Imaging Findings
- There are no other imaging findings associated with COVID-19-associated arrhythmia.
Other Diagnostic Studies
- Myocardial biomarkers ought to be assessed in all patients with COVID‐19.[20]
- American Heart Association (AHA) recommends the following tests to diagnose arrhythmia:
Treatment
Medical Therapy
- Polymorphic Ventricular Tachycardia (torsades de pointes):
- All patients with torsades de pointes (TdP) should be determined if they are hemodynamically stable or unstable through immediate evaluation of the symptoms, vital signs, and level of consciousness.[35]
- Unstable patients: Patients with COVID-19 with sustained torsades de pointes (TdP) usually become hemodynamically unstable, severely symptomatic because of perfusion failure, or pulseless and should be treated according to standard resuscitation algorithms, including cardioversion/defibrillation. Initial treatment with antiarrhythmic medications is not indicated for hemodynamically unstable or pulseless patients except intravenous (IV) magnesium.
- Stable patients: In a patient with a single episode of TdP, treatment with IV magnesium along with correction of metabolic/electrolyte disturbances or removal of any inciting medications may be sufficient. The patient should be kept under observation until the electrolytes, and the QT interval nearly normalizes. An IV bolus of 2-gram magnesium sulfate is the standard therapy for an adult. This is equivalent to a dose of 8.12 mmol of magnesium. The clinical situation of a patient determines the rate of magnesium infusion. Infusion occurs over one to two minutes in patients with pulseless cardiac arrest. The infusion should occur over 15 minutes in patients without cardiac arrest as a rapid IV bolus of magnesium can result in hypotension and asystole. Some patients are given a continuous bolus of IV magnesium at a rate of 3 to 20 mg/min until the QT interval is below 0.50 seconds.[36][37]
- Other Cardiac arrhythmia:
- The treatment for other arrhythmias in COVID-19 patients is the same as in patients with arrhythmias without COVID-19 infection. To browse the treatment of other arrhythmias, click here.
Some medicines are used in combination with each other or together with a procedure or a pacemaker. If the dose is too high, medicines to treat arrhythmia can cause an irregular rhythm. This happens more often in women.[13]
- Adenosine to slow a racing heart. Adenosine acts quickly to slow electrical signals. It can cause some chest pain, flushing, and shortness of breath, but any discomfort typically passes soon.
- Atropine to treat a slow heart rate. This medicine may cause difficulty swallowing.
- Beta-blockers to treat high blood pressure or a fast heart rate or to prevent repeat episodes of arrhythmia. Beta blockers can cause digestive trouble, sleep problems, and sexual dysfunction and can make some conduction disorders worse.
- Blood thinners to reduce the risk of blood clots forming. This helps prevent stroke. With blood-thinning medicines, there is a risk of bleeding.
- Calcium channel blockers to slow a rapid heart rate or the speed at which signals travel. Typically, they are used to control arrhythmias of the upper chambers. In some cases, calcium channel blockers can trigger ventricular fibrillation. They can also cause digestive trouble, swollen feet, or low blood pressure.
- Digitalis, or digoxin, to treat a fast heart rate. This medicine can cause nausea and may trigger arrhythmias.
- Potassium channel blockers to slow the heart rate. They work by lengthening the time it takes for heart cells to recover after firing, so that they do not fire and squeeze as often. Potassium channel blockers can cause low blood pressure or other arrhythmias.
- Sodium channel blockers to block transmission of electrical signals, lengthen cell recovery periods, and make cells less excitable. However, these drugs can increase risks of sudden cardiac arrest in people who have heart disease.[13]
- To browse the medical therapy of COVID-19, click here.
Surgery
- Surgery is usually the treatment recommended only if all other options have failed. In this case, a person is put under anesthesia and a surgeon removes the tissue causing the arrhythmia.[38]
- To have a better insight of treatment for different types of arrhythmia, click here.
Primary Prevention
- American Heart Association (AHA) recommends the following change in lifestyle:
- Reduce high blood pressure
- Control cholesterol levels
- Lose excess weight
- Have a heart-healthy diet
- Stop smoking and avoid secondhand smoke.
- Do regular physical activity
- Drink alcohol only in moderation
- To browse the primary prevention of COVID-19, click here.
Secondary Prevention
- Fever can increase the risk of ventricular arrhythmias in patients with Brugada syndrome. Studies have shown significant results with acetaminophen which lowers fever. Patients with prior history of syncope and who develop type 1 ECG finding of Brugada Syndrome should head to the Emergency department if acetaminophen is unable to normalize the fever.[39]
- To browse the secondary prevention of COVID-19, click here.
References
- ↑ Ruan Q, Yang K, Wang W, Jiang L, Song J (2020). "Correction to: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Med. 46 (6): 1294–1297. doi:10.1007/s00134-020-06028-z. PMC 7131986 Check
|pmc=value (help). PMID 32253449 Check|pmid=value (help). - ↑ 2.0 2.1 Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J; et al. (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China". JAMA. doi:10.1001/jama.2020.1585. PMC 7042881 Check
|pmc=value (help). PMID 32031570 Check|pmid=value (help). - ↑ 3.0 3.1 Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M; et al. (2020). "Guidance for Cardiac Electrophysiology During the COVID-19 Pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association". Circulation. 141 (21): e823–e831. doi:10.1161/CIRCULATIONAHA.120.047063. PMC 7243667 Check
|pmc=value (help). PMID 32228309 Check|pmid=value (help). - ↑ Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P; et al. (2020). "Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan. A Retrospective Observational Study". Am J Respir Crit Care Med. 201 (11): 1372–1379. doi:10.1164/rccm.202003-0543OC. PMC 7258652 Check
|pmc=value (help). PMID 32242738 Check|pmid=value (help). - ↑ 5.0 5.1 5.2 Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP; et al. (2020). "Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province". Chin Med J (Engl). 133 (9): 1025–1031. doi:10.1097/CM9.0000000000000744. PMC 7147277 Check
|pmc=value (help). PMID 32044814 Check|pmid=value (help). - ↑ 6.0 6.1 Duan K, Liu B, Li C, Zhang H, Yu T, Qu J; et al. (2020). "Effectiveness of convalescent plasma therapy in severe COVID-19 patients". Proc Natl Acad Sci U S A. 117 (17): 9490–9496. doi:10.1073/pnas.2004168117. PMC 7196837 Check
|pmc=value (help). PMID 32253318 Check|pmid=value (help). - ↑ Xu, Zhe; Shi, Lei; Wang, Yijin; Zhang, Jiyuan; Huang, Lei; Zhang, Chao; Liu, Shuhong; Zhao, Peng; Liu, Hongxia; Zhu, Li; Tai, Yanhong; Bai, Changqing; Gao, Tingting; Song, Jinwen; Xia, Peng; Dong, Jinghui; Zhao, Jingmin; Wang, Fu-Sheng (2020). "Pathological findings of COVID-19 associated with acute respiratory distress syndrome". The Lancet Respiratory Medicine. 8 (4): 420–422. doi:10.1016/S2213-2600(20)30076-X. ISSN 2213-2600.
- ↑ Chen, Mao; Prendergast, Bernard; Redwood, Simon; Xiong, Tian-Yuan (2020). "Coronaviruses and the cardiovascular system: acute and long-term implications". European Heart Journal. 41 (19): 1798–1800. doi:10.1093/eurheartj/ehaa231. ISSN 0195-668X.
- ↑ 9.0 9.1 9.2 Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G; et al. (2020). "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic". J Am Coll Cardiol. 75 (18): 2352–2371. doi:10.1016/j.jacc.2020.03.031. PMC 7198856 Check
|pmc=value (help). PMID 32201335 Check|pmid=value (help). - ↑ Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL (2019). "Cardioimmunology of arrhythmias: the role of autoimmune and inflammatory cardiac channelopathies". Nat Rev Immunol. 19 (1): 63–64. doi:10.1038/s41577-018-0098-z. PMID 30552387.
- ↑ Clerkin, Kevin J.; Fried, Justin A.; Raikhelkar, Jayant; Sayer, Gabriel; Griffin, Jan M.; Masoumi, Amirali; Jain, Sneha S.; Burkhoff, Daniel; Kumaraiah, Deepa; Rabbani, LeRoy; Schwartz, Allan; Uriel, Nir (2020). "COVID-19 and Cardiovascular Disease". Circulation. 141 (20): 1648–1655. doi:10.1161/CIRCULATIONAHA.120.046941. ISSN 0009-7322.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 12.8 12.9 "Arrhythmias: MedlinePlus Medical Encyclopedia".
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 13.8 13.9 "Arrhythmia | NHLBI, NIH".
- ↑ 14.0 14.1 14.2 Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ "Understand Your Risk For Arrhythmia | American Heart Association".
- ↑ 16.0 16.1 Lazzerini PE, Boutjdir M, Capecchi PL (2020). "COVID-19, Arrhythmic Risk, and Inflammation: Mind the Gap!". Circulation. 142 (1): 7–9. doi:10.1161/CIRCULATIONAHA.120.047293. PMID 32286863 Check
|pmid=value (help). - ↑ Skogestad J, Aronsen JM (2018). "Hypokalemia-Induced Arrhythmias and Heart Failure: New Insights and Implications for Therapy". Front Physiol. 9: 1500. doi:10.3389/fphys.2018.01500. PMC 6234658. PMID 30464746.
- ↑ Amin AS, Herfst LJ, Delisle BP, Klemens CA, Rook MB, Bezzina CR; et al. (2008). "Fever-induced QTc prolongation and ventricular arrhythmias in individuals with type 2 congenital long QT syndrome". J Clin Invest. 118 (7): 2552–61. doi:10.1172/JCI35337. PMC 2423868. PMID 18551196.
- ↑ Chang D, Saleh M, Garcia-Bengo Y, Choi E, Epstein L, Willner J (2020). "COVID-19 Infection Unmasking Brugada Syndrome". HeartRhythm Case Rep. doi:10.1016/j.hrcr.2020.03.012. PMC 7138191 Check
|pmc=value (help). PMID 32292696 Check|pmid=value (help). - ↑ 20.0 20.1 20.2 Kochi, Adriano Nunes; Tagliari, Ana Paula; Forleo, Giovanni Battista; Fassini, Gaetano Michele; Tondo, Claudio (2020). "Cardiac and arrhythmic complications in patients with COVID‐19". Journal of Cardiovascular Electrophysiology. 31 (5): 1003–1008. doi:10.1111/jce.14479. ISSN 1045-3873.
- ↑ 21.0 21.1 Guo, Tao; Fan, Yongzhen; Chen, Ming; Wu, Xiaoyan; Zhang, Lin; He, Tao; Wang, Hairong; Wan, Jing; Wang, Xinghuan; Lu, Zhibing (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1017. ISSN 2380-6583.
- ↑ Gandhi, Rajesh T.; Solomon, Caren G.; Lynch, John B.; del Rio, Carlos (2020). "Mild or Moderate Covid-19". New England Journal of Medicine. doi:10.1056/NEJMcp2009249. ISSN 0028-4793.
- ↑ Chang, David; Saleh, Moussa; Gabriels, James; Ismail, Haisam; Goldner, Bruce; Willner, Jonathan; Beldner, Stuart; Mitra, Raman; John, Roy; Epstein, Laurence M. (2020). "Inpatient Use of Ambulatory Telemetry Monitors for COVID-19 Patients Treated With Hydroxychloroquine and/or Azithromycin". Journal of the American College of Cardiology. 75 (23): 2992–2993. doi:10.1016/j.jacc.2020.04.032. ISSN 0735-1097.
- ↑ Inciardi, Riccardo M.; Lupi, Laura; Zaccone, Gregorio; Italia, Leonardo; Raffo, Michela; Tomasoni, Daniela; Cani, Dario S.; Cerini, Manuel; Farina, Davide; Gavazzi, Emanuele; Maroldi, Roberto; Adamo, Marianna; Ammirati, Enrico; Sinagra, Gianfranco; Lombardi, Carlo M.; Metra, Marco (2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1096. ISSN 2380-6583.
- ↑
- ↑
- ↑ Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW; et al. (2020). "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area". JAMA. doi:10.1001/jama.2020.6775. PMC 7177629 Check
|pmc=value (help). PMID 32320003 Check|pmid=value (help). - ↑ Giudicessi, John R.; Noseworthy, Peter A.; Friedman, Paul A.; Ackerman, Michael J. (2020). "Urgent Guidance for Navigating and Circumventing the QTc-Prolonging and Torsadogenic Potential of Possible Pharmacotherapies for Coronavirus Disease 19 (COVID-19)". Mayo Clinic Proceedings. 95 (6): 1213–1221. doi:10.1016/j.mayocp.2020.03.024. ISSN 0025-6196.
- ↑ Goyal, Parag; Choi, Justin J.; Pinheiro, Laura C.; Schenck, Edward J.; Chen, Ruijun; Jabri, Assem; Satlin, Michael J.; Campion, Thomas R.; Nahid, Musarrat; Ringel, Joanna B.; Hoffman, Katherine L.; Alshak, Mark N.; Li, Han A.; Wehmeyer, Graham T.; Rajan, Mangala; Reshetnyak, Evgeniya; Hupert, Nathaniel; Horn, Evelyn M.; Martinez, Fernando J.; Gulick, Roy M.; Safford, Monika M. (2020). "Clinical Characteristics of Covid-19 in New York City". New England Journal of Medicine. 382 (24): 2372–2374. doi:10.1056/NEJMc2010419. ISSN 0028-4793.
- ↑ Guo T, Fan Y, Chen M, Wu X, Zhang L, He T; et al. (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. doi:10.1001/jamacardio.2020.1017. PMC 7101506 Check
|pmc=value (help). PMID 32219356 Check|pmid=value (help). - ↑ Baldi, Enrico; Sechi, Giuseppe M.; Mare, Claudio; Canevari, Fabrizio; Brancaglione, Antonella; Primi, Roberto; Klersy, Catherine; Palo, Alessandra; Contri, Enrico; Ronchi, Vincenza; Beretta, Giorgio; Reali, Francesca; Parogni, Pierpaolo; Facchin, Fabio; Bua, Davide; Rizzi, Ugo; Bussi, Daniele; Ruggeri, Simone; Oltrona Visconti, Luigi; Savastano, Simone (2020). "Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy". New England Journal of Medicine. doi:10.1056/NEJMc2010418. ISSN 0028-4793.
- ↑ Shao, Fei; Xu, Shuang; Ma, Xuedi; Xu, Zhouming; Lyu, Jiayou; Ng, Michael; Cui, Hao; Yu, Changxiao; Zhang, Qing; Sun, Peng; Tang, Ziren (2020). "In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China". Resuscitation. 151: 18–23. doi:10.1016/j.resuscitation.2020.04.005. ISSN 0300-9572.
- ↑ Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M (March 2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. doi:10.1001/jamacardio.2020.1096. PMID 32219357 Check
|pmid=value (help). - ↑ Alhogbani T (2016). "Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus". Ann Saudi Med. 36 (1): 78–80. doi:10.5144/0256-4947.2016.78. PMC 6074274. PMID 26922692.
- ↑ Panchal, Ashish R.; Berg, Katherine M.; Kudenchuk, Peter J.; Del Rios, Marina; Hirsch, Karen G.; Link, Mark S.; Kurz, Michael C.; Chan, Paul S.; Cabañas, José G.; Morley, Peter T.; Hazinski, Mary Fran; Donnino, Michael W. (2018). "2018 American Heart Association Focused Update on Advanced Cardiovascular Life Support Use of Antiarrhythmic Drugs During and Immediately After Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 138 (23). doi:10.1161/CIR.0000000000000613. ISSN 0009-7322.
- ↑ Tzivoni, D; Banai, S; Schuger, C; Benhorin, J; Keren, A; Gottlieb, S; Stern, S (1988). "Treatment of torsade de pointes with magnesium sulfate". Circulation. 77 (2): 392–397. doi:10.1161/01.CIR.77.2.392. ISSN 0009-7322.
- ↑ Neumar, R. W.; Otto, C. W.; Link, M. S.; Kronick, S. L.; Shuster, M.; Callaway, C. W.; Kudenchuk, P. J.; Ornato, J. P.; McNally, B.; Silvers, S. M.; Passman, R. S.; White, R. D.; Hess, E. P.; Tang, W.; Davis, D.; Sinz, E.; Morrison, L. J. (2010). "Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18_suppl_3): S729–S767. doi:10.1161/CIRCULATIONAHA.110.970988. ISSN 0009-7322.
- ↑ "Arrhythmias (for Teens) - Nemours KidsHealth".
- ↑ Wu CI, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C; et al. (2020). "SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes". Heart Rhythm. doi:10.1016/j.hrthm.2020.03.024. PMC 7156157 Check
|pmc=value (help). PMID 32244059 Check|pmid=value (help).