Sandbox AG
=Portal vein thrombosis
| Portal vein thrombosis | |
 | |
|---|---|
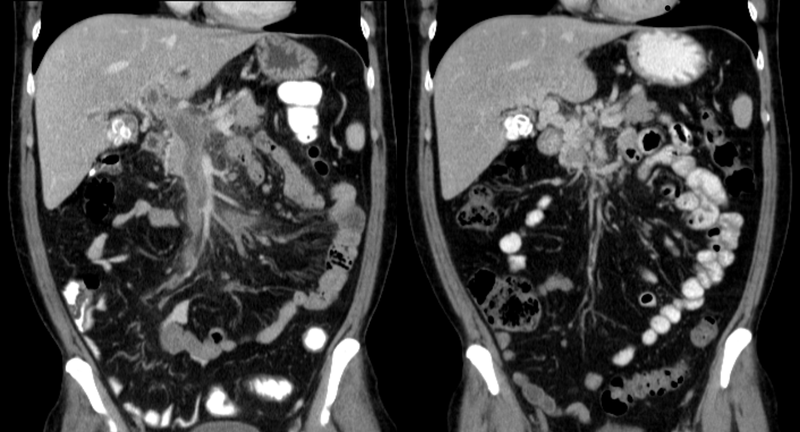
| Portal vein thrombosis in computertomography. | |
| ICD-10 | I81 |
| ICD-9 | 452 |
|
Portal vein thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sandbox AG On the Web |
|
American Roentgen Ray Society Images of Sandbox AG |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Portal vein thrombosis is a form of venous thrombosis affecting the hepatic portal vein, which can lead to portal hypertension and reduction in the blood supply to the liver.
Causes
Causes can include pancreatitis, cirrhosis, diverticulitis, and cholangiocarcinoma. It is also a known complication of splenectomy.[1] Drugs such as Romiplostim.
Diagnosis
The diagnosis of portal vein thrombosis is usually made by ultrasound, computed tomography with contrast or magnetic resonance imaging. D-dimer levels in the blood blood may be elevated as a result of fibrin degradation.
Treatment
-
Portal vein thrombosis on computed tomography (left) and cavernous transformation of the portal vein after 1 year (right)
Treatments include anticoagulants, shunts, bypass surgery, and transplants.
Related Chapters
References
- ↑ Ali Cadili, Chris de Gara, "Complications of Splenectomy", The American Journal of Medicine, 2008, pp 371-375.
External links
| Wikimedia Commons has media related to Portal vein thrombosis. |
Encephalitis Table
Reference list includes:[1][2]
| Disease | Similarities | Differentials |
|---|---|---|
| Meningitis | Classic triad of fever, nuchal rigidity, and altered mental status | Photophobia, phonophobia, rash associated with meningococcemia, concomitant sinusitis or otitis, swelling of the fontanelle in infants (0-6 months) |
| Brain abscess | Fever, headache, hemiparesis | Varies depending on the location of the abscess; clinically, visual disturbance including papilledema, decreased sensation; on imaging, a lesion demonstrates both ring enhancement and central restricted diffusion |
| Demyelinating diseases | Ataxia, lethargy | Multiple sclerosis: clinically, nystagmus, internuclear ophthalmoplegia, Lhermitte's sign; on imaging, well-demarcated ovoid lesions with possible T1 hypointensities (“black holes”)
Acute disseminated encephalomyelitis: ; on imaging, diffuse or multi-lesion enhancement, with indistinct lesion borders |
| Substance abuse | Tremor, headache, altered mental status | Varies depending on type of substance: prior history, drug-seeking behavior, attention-seeking behavior, paranoia, sudden panic, anxiety, hallucinations |
| Electrolyte disturbance | Fatigue, headache, nausea | Varies depending on deficient ions; clinically, edema, constipation, hallucinations; on EKG, abnormalities in T wave, P wave, QRS complex; possible presentations include arrhythmia, dehydration, renal failure |
| Stroke | Ataxia, aphasia, dizziness | Varies depending on classification of stroke; presents with positional vertigo, high blood pressure, extremity weakness |
| Intracranial hemorrhage | Headache, coma, dizziness | Lobar hemorrhage, numbness, tingling, hypertension, hemorrhagic diathesis |
| Trauma | Headache, altered mental status | Amnesia, loss of consciousness, dizziness, concussion, contusion |
References
- ↑ Eckstein C, Saidha S, Levy M (2012). "A differential diagnosis of central nervous system demyelination: beyond multiple sclerosis". J Neurol. 259 (5): 801–16. doi:10.1007/s00415-011-6240-5. PMID 21932127.
- ↑ De Kruijk JR, Twijnstra A, Leffers P (2001). "Diagnostic criteria and differential diagnosis of mild traumatic brain injury". Brain Inj. 15 (2): 99–106. doi:10.1080/026990501458335. PMID 11260760.