Glioma pathophysiology
|
Glioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glioma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Glioma pathophysiology |
|
Risk calculators and risk factors for Glioma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2], Sujit Routray, M.D. [3]
Overview
High-grade gliomas are highly-vascular tumors and have a tendency to infiltrate. Low-grade gliomas grow slowly, and treatment is not necessarily needed until it become symptomatic.
Pathophysiology
Pathogenesis
- High-grade gliomas are highly-vascular tumors and have a tendency to infiltrate. They have extensive areas of necrosis and hypoxia. Often tumor growth causes a breakdown of the blood-brain barrier in the vicinity of the tumor.
- Low-grade gliomas grow slowly, often over many years, and can be followed without treatment unless they grow and cause symptoms.
Genetics
Genes involved in the pathogenesis of glioma include:[1][2]
Associated Conditions
Gliomas may be associated with:[3][2]
- Neurofibromatosis type 1
- Neurofibromatosis type 2
- Tuberous sclerosis
- Li-Fraumeni syndrome
- Turcot syndrome
- Maffucci syndrome
- Von Hippel-Lindau disease
- Retinoblastoma
Gross Pathology
Gross pathology of glioma differ with the type. The various types of glioma with the distinct gross pathological features include:[4]
Pilocytic astrocytoma
- On gross pathology, pilocytic astrocytoma is characterized by well-circumscribed cystic tumor with a solid mural nodule.
- They are commonly located in the cerebellum.
Low-grade astrocytoma
- On gross pathology, low-grade astrocytoma is characterized by poorly demarcated tumor resulting in enlargement of the involved portion of the brain and blurring of anatomical landmarks.
- They can arise anywhere in the CNS, but are commonly located in the cerebral hemisphere.
Anaplastic astrocytoma
- On gross pathology, the characteristic findings of anaplastic astrocytoma include a spongy or gelationous mass with ill defined borders, microcysts, and calcification.
- They are better demarcated from surrounding brain structures than low-grade astrocytomas.
- They are commonly located in frontal lobe, temporal lobe, brain stem, or spinal cord.
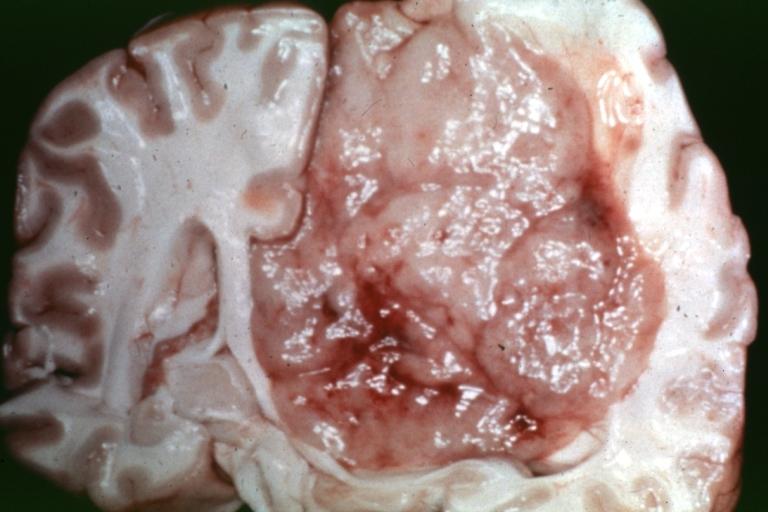
Glioblastoma multiforme
- On gross pathology, the characteristic findings of glioblastoma multiforme include a poorly-marginated, diffusely infiltrating, firm or gelatinous mass with a central necrotic core.
- They are commonly located in the frontal and temporal lobe.
Oligodendroglioma
- On gross pathology, the characteristic findings of oligodendroglioma include a pinkish-white, well circumscribed mass with or without mucinous changes.
- They are commonly located in the frontal lobe, followed by parietal and temporal lobes.
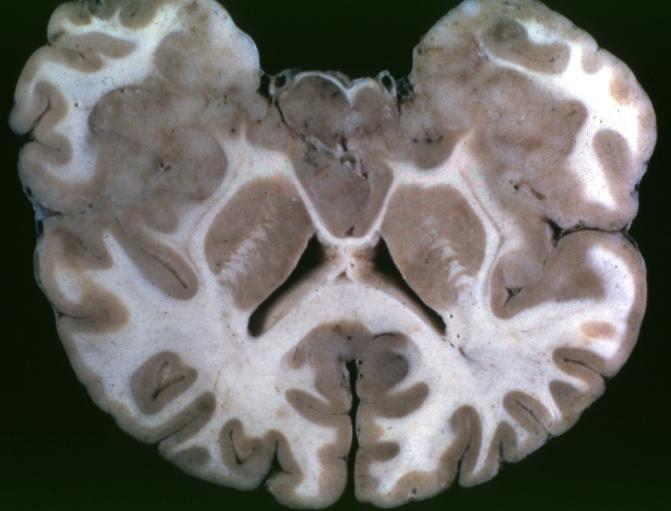
Ependymoma
- On gross pathology, the characteristic findings of ependymoma include a well-differentiated mass growing in an exophytic fashion protruding into the fourth ventricle.
- Myxopapillary ependymoma is commonly located at the filum terminale.
-
Brain: Pontine Glioma: Gross; fixed tissue, anterior view of brain stem and cerebellum with bosselated tumor adjacent to basilar artery
-
Brain: Pontine Glioma: Gross; fixed tissue, sagittal section brain stem and cerebellum
-
Brain: Glioma: Gross; fixed tissue, horizontal section brain stem and cerebellum with obvious gelatinous appearing neoplasm a pontine glioma
-
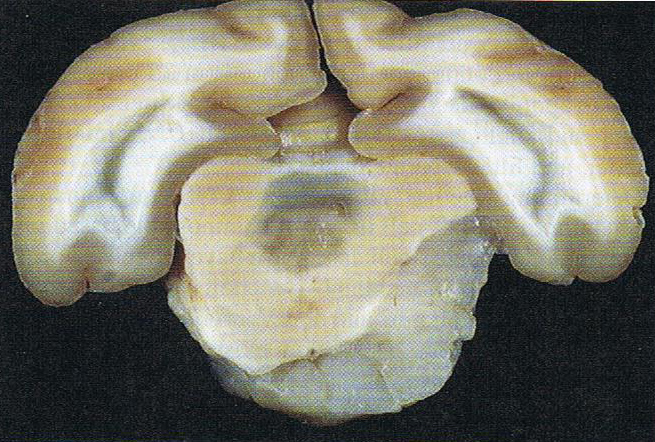
Brain: Oligodendroglioma: Gross; natural color, large, well circumscribed lesion in left frontal lobe
-
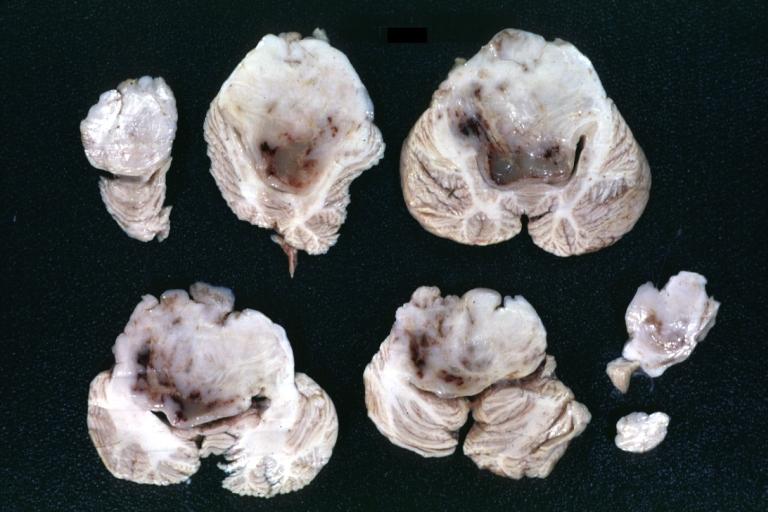
Brain: Glioma: Gross; fixed tissue, horizontal sections brain stem and cerebellum showing large pontine glioma
-
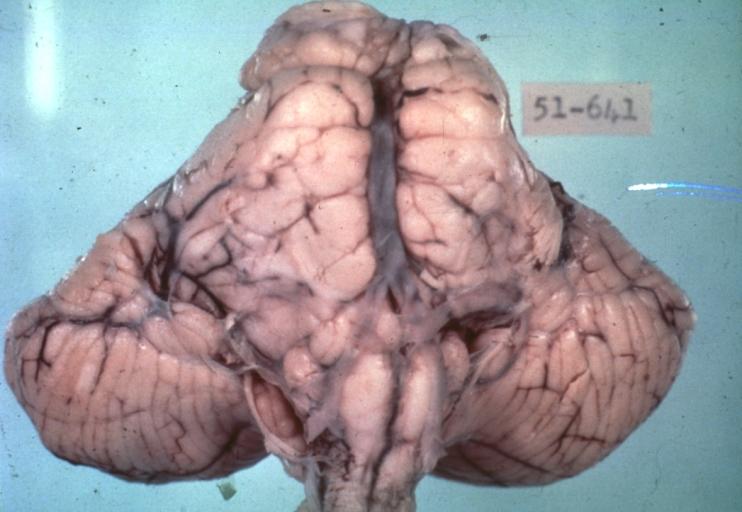
Brain: Pontine Glioma and Diffuse Meningeal Gliomatosis: Gross; fixed tissue, view of cerebral hemispheres from inferior with brain stem and cerebellum removed. Pontine asymmetry is easily seen due to low grade astrocytoma and meningeal gliomatosis is easily seen over frontal lobes
-
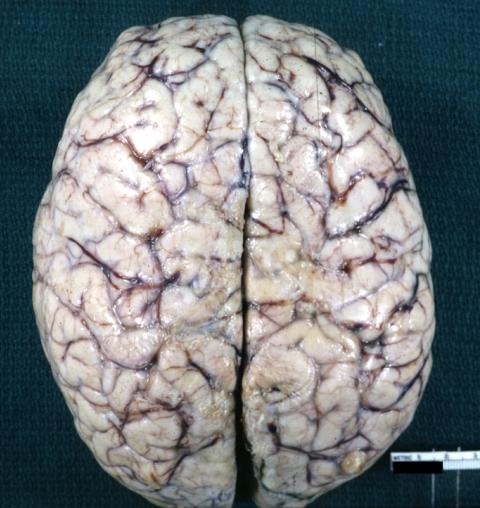
Brain: Pontine Glioma and Diffuse Meningeal Gliomatosis in 7 yo boy: Gross; fixed tissue, view of cerebral hemispheres from vertex meningeal gliomatosis.
-
Brain: Pontine Glioma and Diffuse Meningeal Gliomatosis: Gross; in situ dural nodule
-
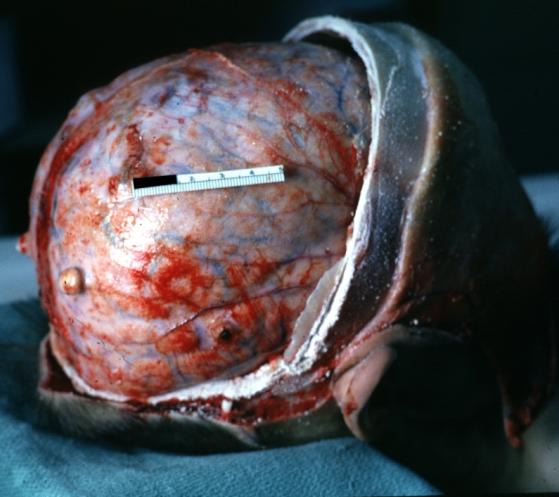
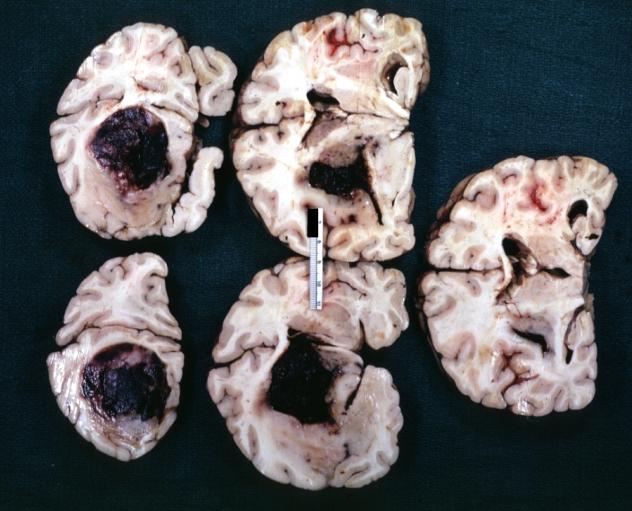
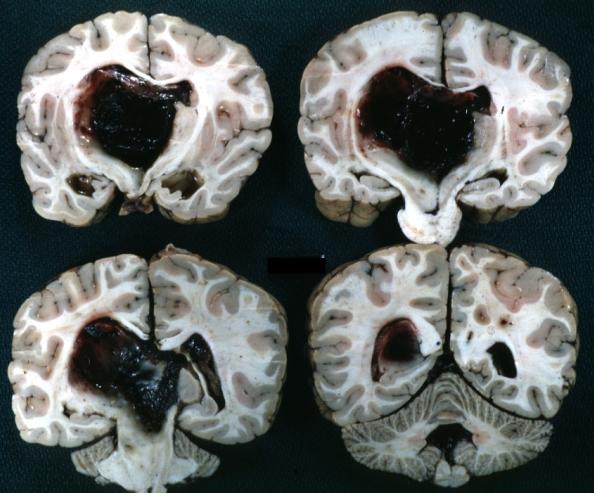
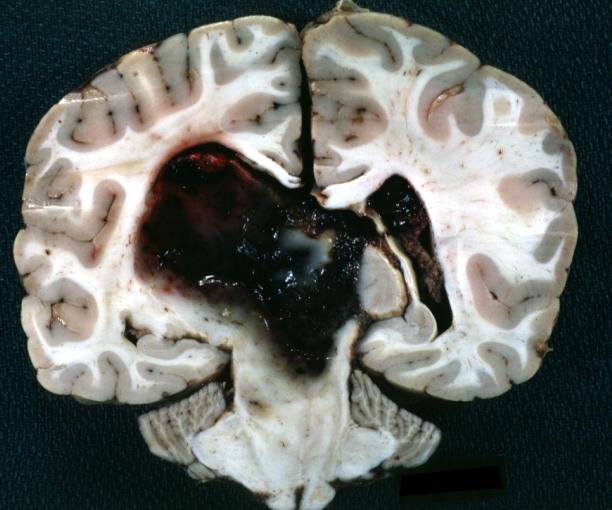
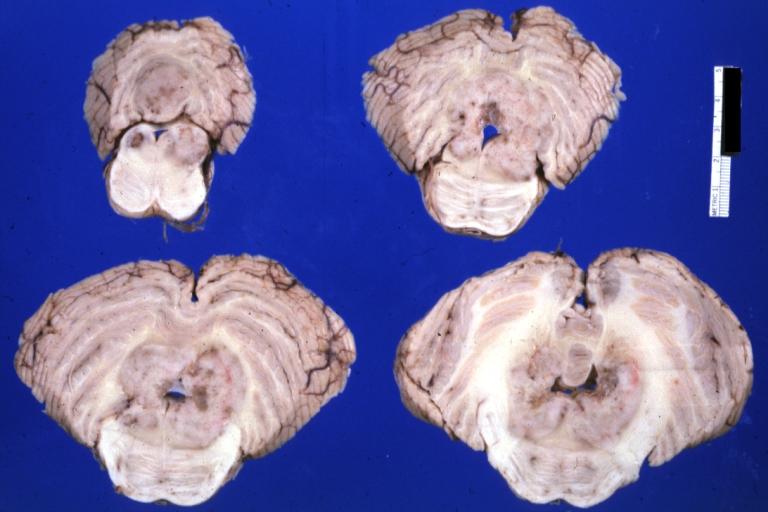
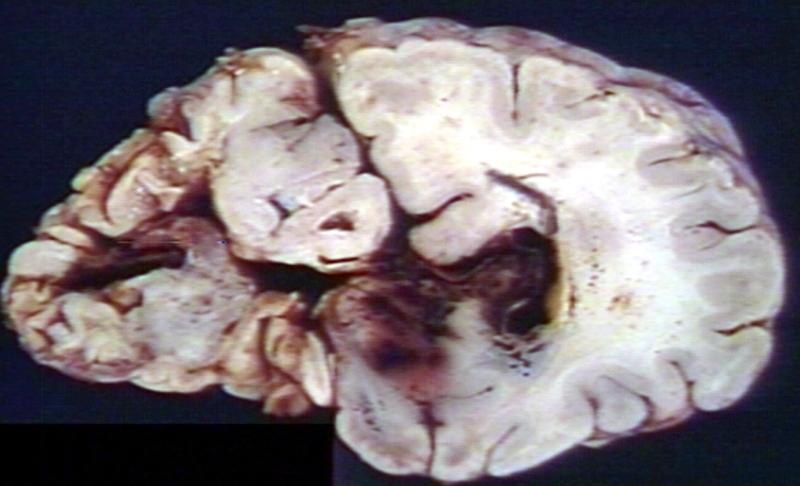
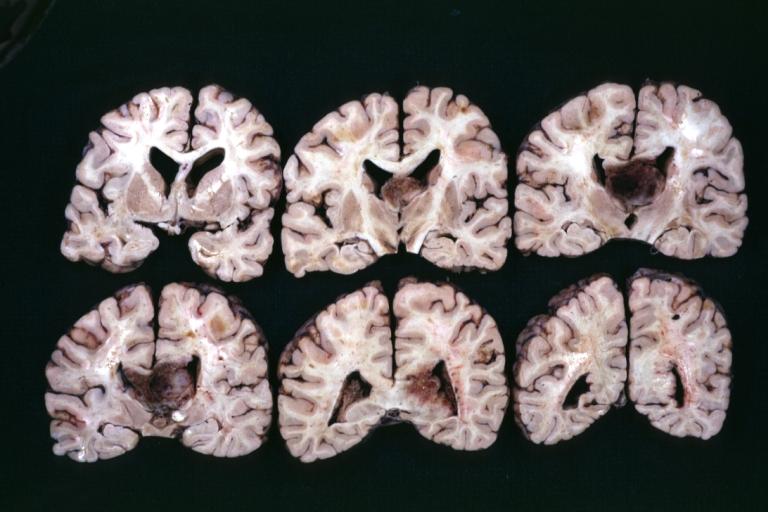
Brain: Oligodendroglioma: Gross; fixed tissue, multiple coronal sections, cerebral hemispheres with large tumor and hemorrhage into tumor
-
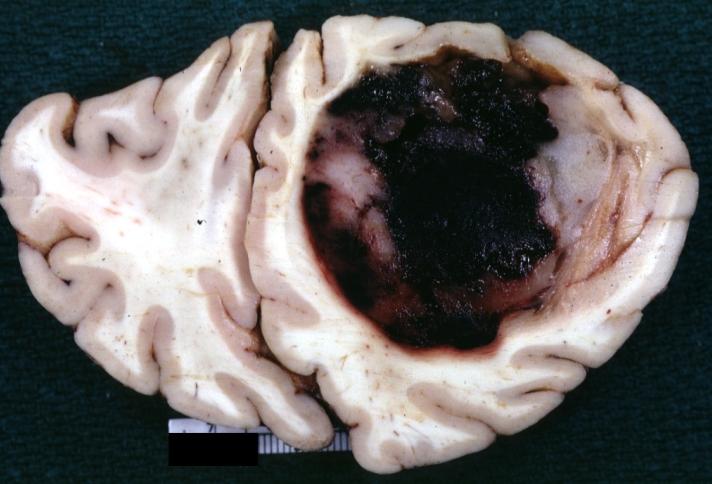
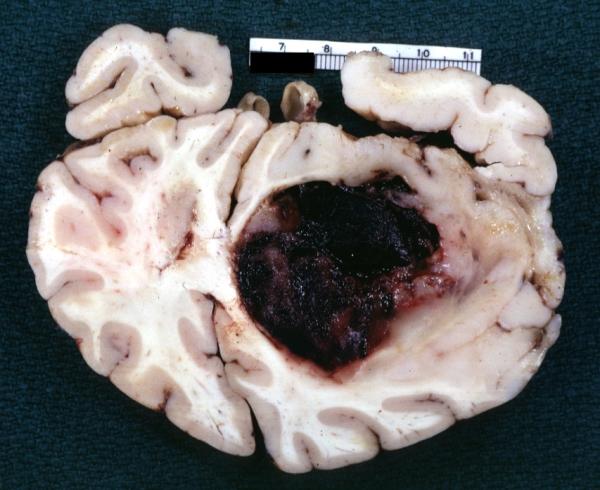
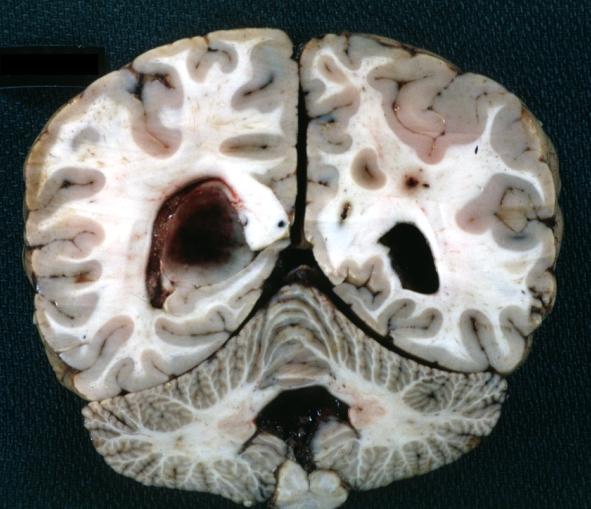
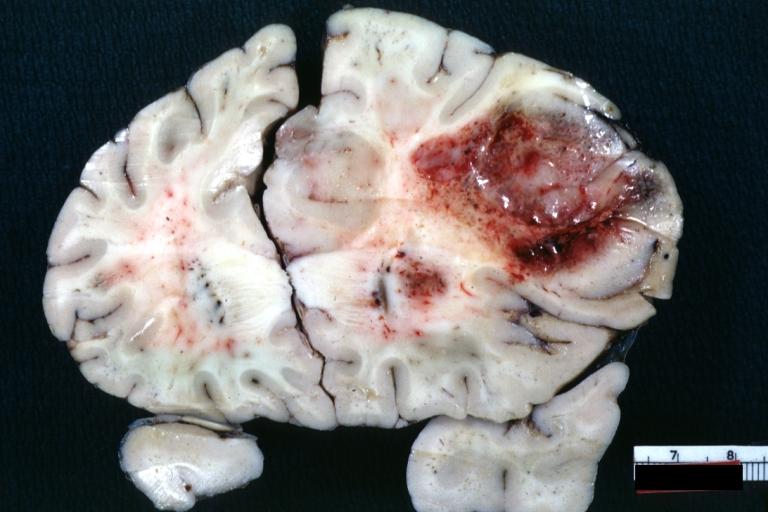
Brain: Oligodendroglioma: Gross; fixed tissue, coronal section, cerebral hemispheres, large hemorrhagic lesion in one hemisphere
-
Brain: Oligodendroglioma: Gross; fixed tissue, ischemic tissue, anterior to tumor mass
-
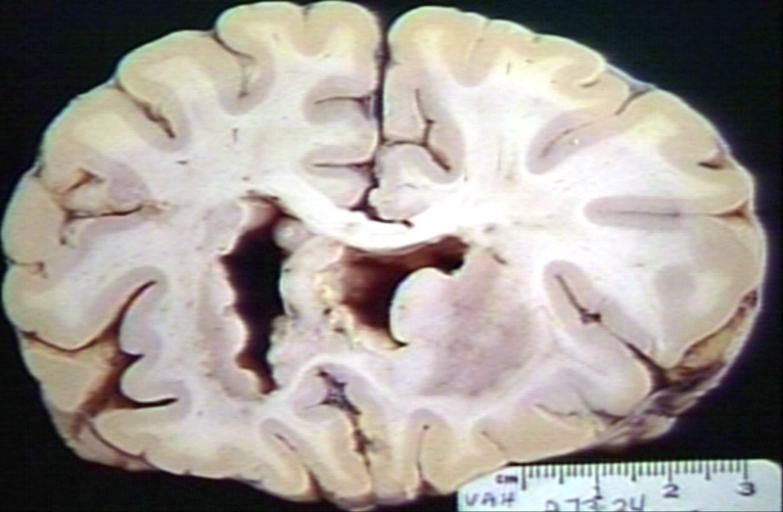
Brain: Oligodendroglioma: Gross; natural color, coronal section, cerebral hemispheres, large lesion, left parieto occipital white matter
-
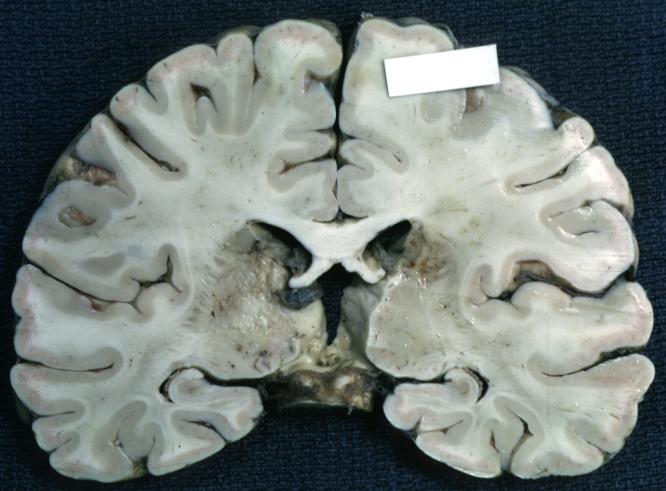
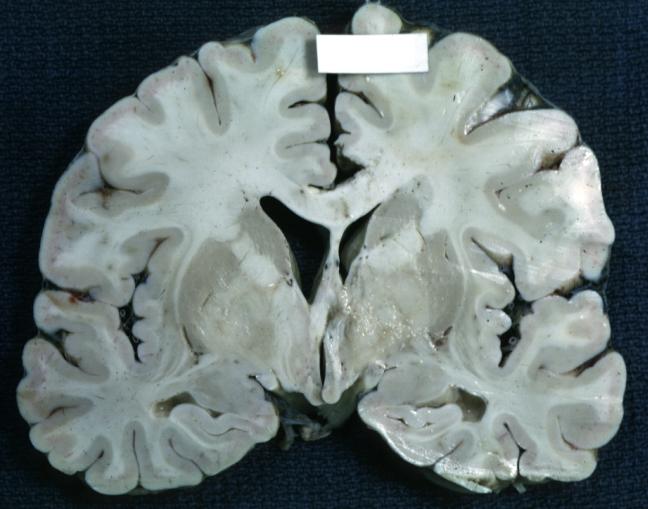
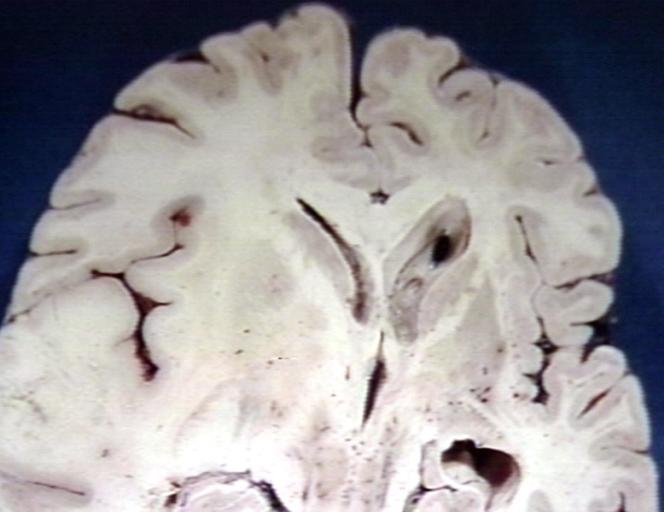
Brain: Gliomatosis Cerebri: Gross; fixed tissue, coronal sections, cerebral hemispheres, lesion is in temporal lobes and hypothalamus
-
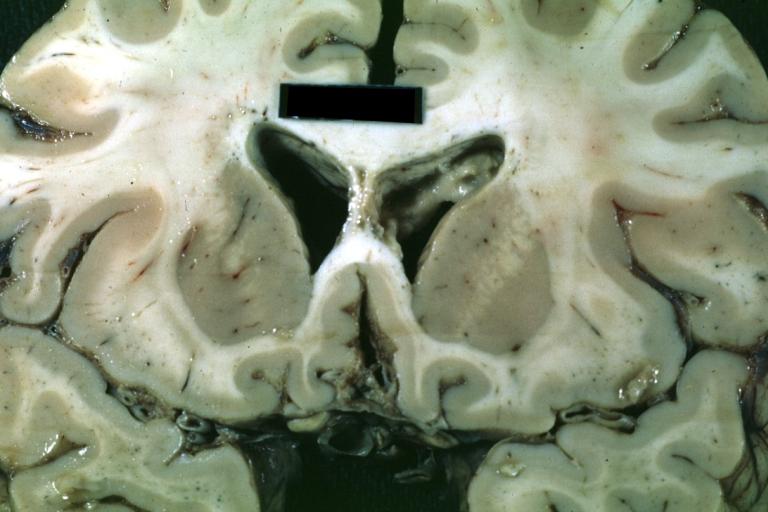
Brain: Ventriculitis: Gross; fixed tissue, case of glioma with meningitis, a nice view of ventriculitis in one lateral ventricle
-
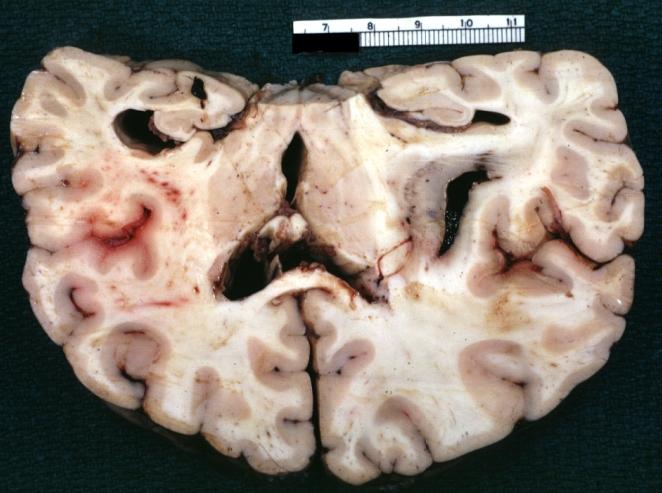
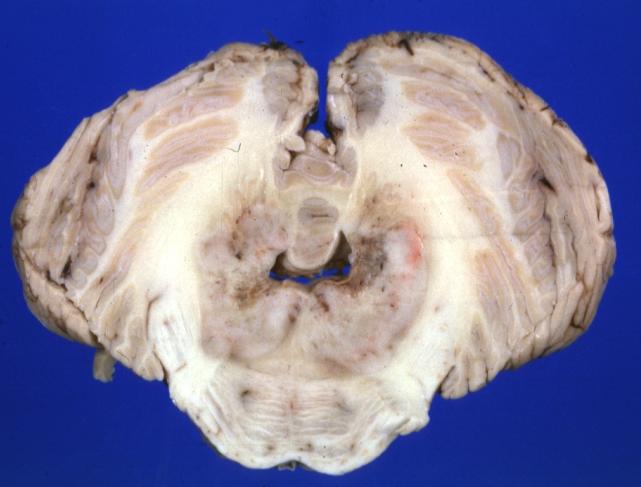
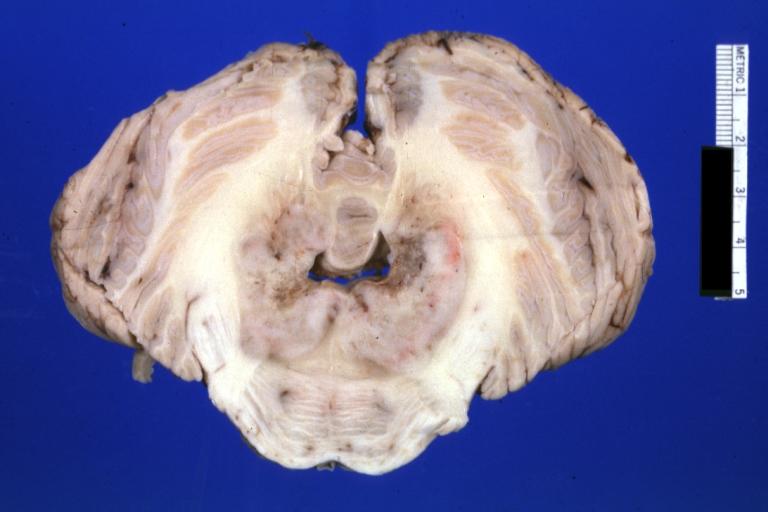
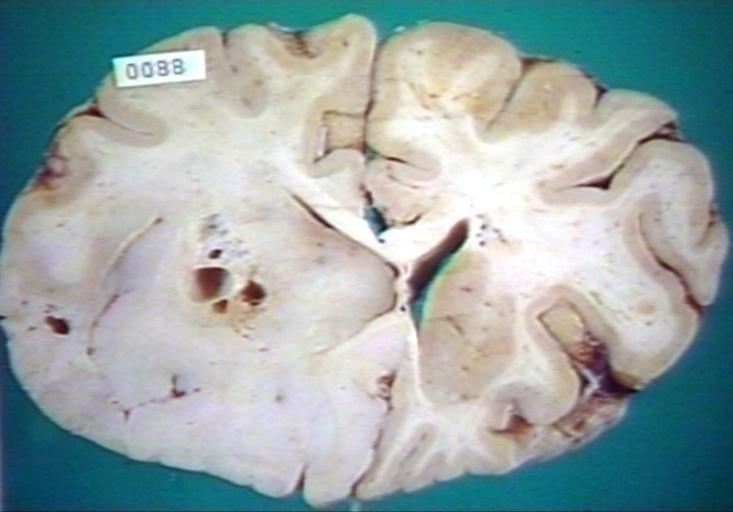
Brain: Glioma Thalamic Grade Ii-Iii: Gross; fixed tissue, four coronal sections, cerebral hemispheres, very large hemorrhagic lesion
-
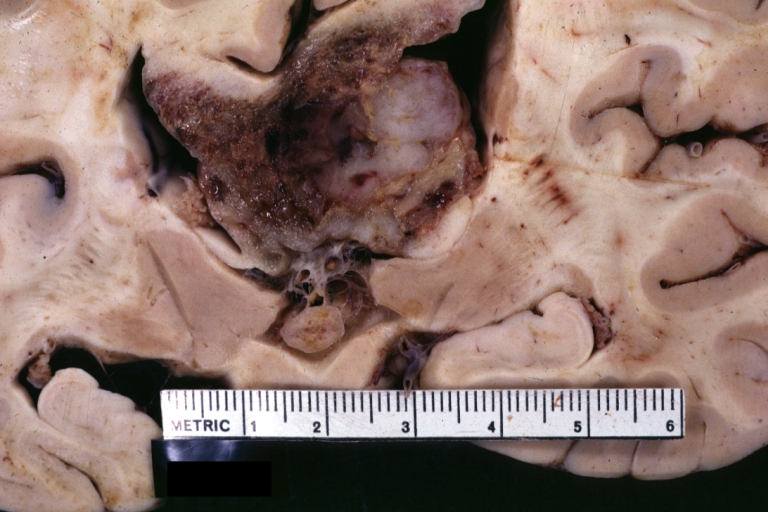
Brain: Glioma Thalamic Grade Ii-Iii: Gross; fixed tissue, coronal section, cerebral hemispheres with large hemorrhagic lesion
-
Brain: Glioma Thalamic Grade Ii-Iii: Gross fixed tissue coronal section cerebral hemispheres lesions appears to be in choroid plexus of lateral ventricle in this picture. There is blood in fourth ventricle
-
Brain: Cerebral Sarcoma or Microglioma: Gross; fixed tissue, coronal section, cerebral hemispheres (58 yo man)
-
Brain: Cerebral Sarcoma or Microglioma: Gross; fixed tissue, coronal section, cerebral hemispheres
-
Brain: Cerebral Sarcoma or Microglioma: Gross; fixed tissue, coronal section, cerebral hemispheres
-
Brain: Infarct Subcortical: Gross; fixed tissue, close-up view of old small subcortical infarct, a case of microglioma
-
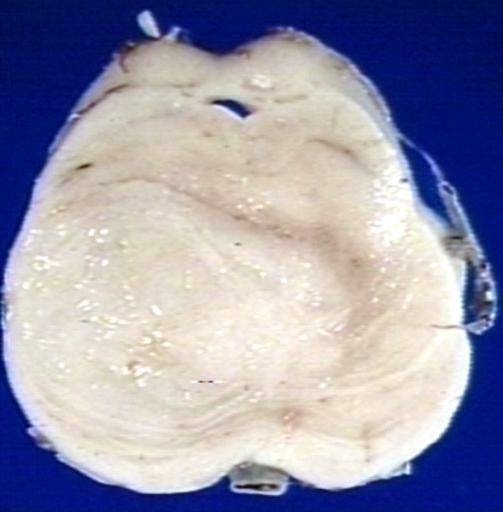
Brain: Microglioma: Gross; fixed tissue; cerebellum and fourth ventricle with periventricular tumor invasion
-
Brain: Microglioma: Gross fixed tissue horizontal sections cerebellum and brain stem with periventricular neoplastic infiltrate
-
Brain: Microglioma: Gross fixed tissue horizontal section midbrain and cerebellum at mid pons level periventricular tumor infiltration
-
Brain: Microglioma: Gross fixed tissue horizontal section rostral pons and cerebellum
-
Brain: Microglioma: Gross fixed tissue horizontal section rostral pons and cerebellum periventricular tumor invasion
-
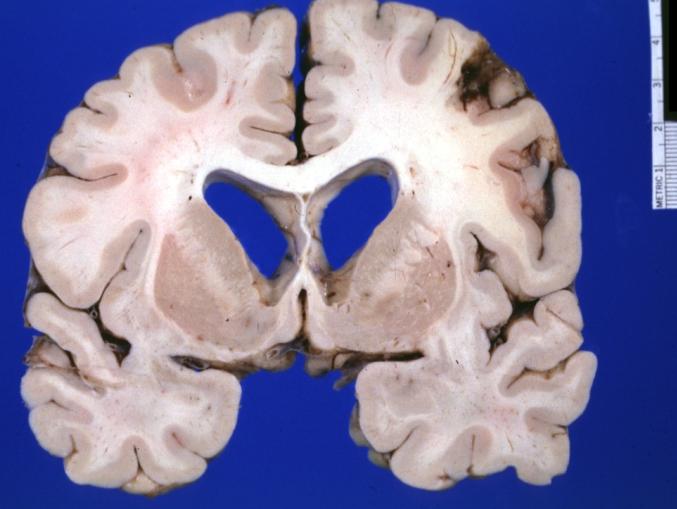
Brain: Microglioma: Gross fixed tissue coronal section cerebral hemispheres with mild ventricular dilation
-
Glioma: Optic Nerve
-
Brain: Oligodendroglioma, Frontal Lobe
-
Brain: Oligodendroglioma, Mixed Astrocytoma & Oligodendroglioma
-
Brain: Glioma, Grade II Anaplastic
-
Brain: Glioma, Brain stem, Low Grade
-
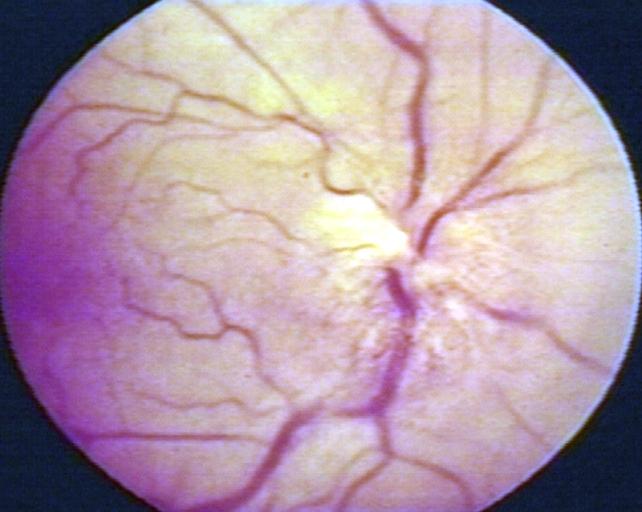
Fundoscopy: Eye; Optic Nerve Glioma, Optic Nerve
-
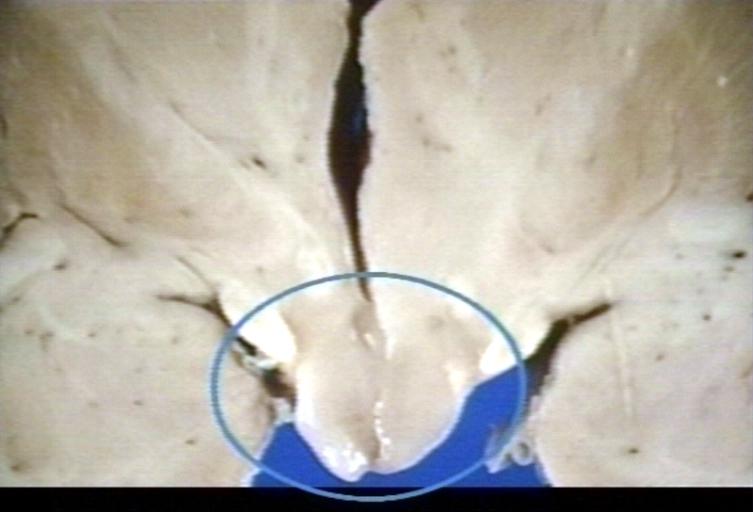
Brain: Glioma, Hypothalamic, Circle Around Region of Tumor
-
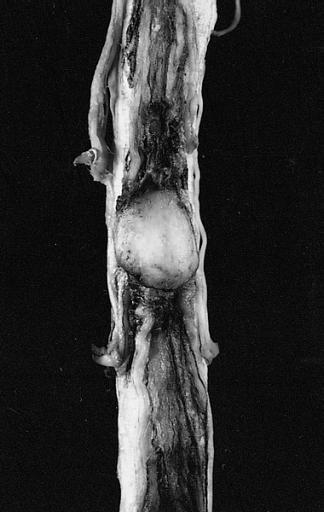
CNS: Pilocytic Astrocytoma of the Spinal Cord. The fusiform expansion of the spinal cord produced by this pilocytic astrocytoma is not, on external examination alone, distinguishable from that produced by a nonresectable diffuse glioma.
-
Brain: Glioma, Pontine
-
Brain: Glioblastoma Multiforme: Gross fixed tissue close-up large necrotic tumor mass in septum pellucidum
-
Brain: Glioblastoma Multiforme: Gross fixed tissue coronal section of the brain with a large necrotic tumor mass in septum pellucidum diagnosed as astrocytoma grade III
-
Brain: Glioblastoma Multiforme: Gross natural color large hemorrhagic lesion in right centrum semiovale
-
CNS: Malignant pilocytic astrocytoma: A 29-year-old woman died 2 years after a diagnosis of "atypical pilocytic astrocytoma" of the pineal region. At autopsy, multiple tumor implants were present in the craniospinal subarachnoid spaces.
Microscopic Pathology
Microscopic pathology of glioma differ with the type. The various types of glioma with the distinct microscopic histopathological features include:[5]
| Type of glioma | Histopathological features |
|---|---|
| |
| |
| |
| |
|
-
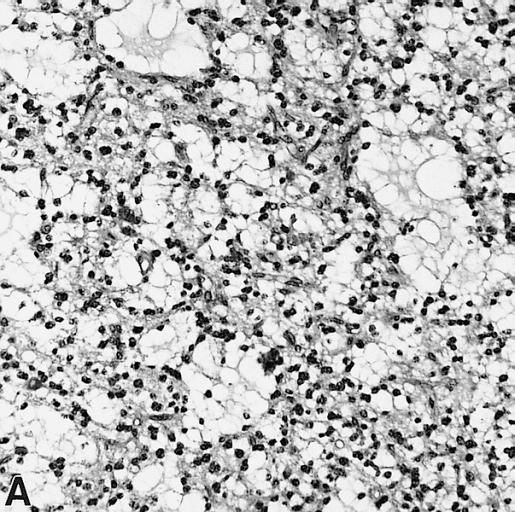
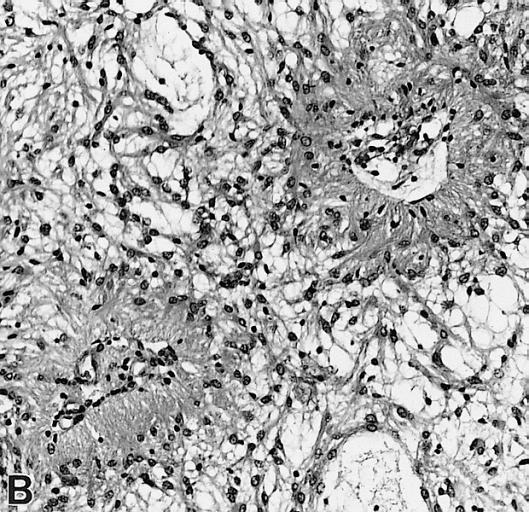
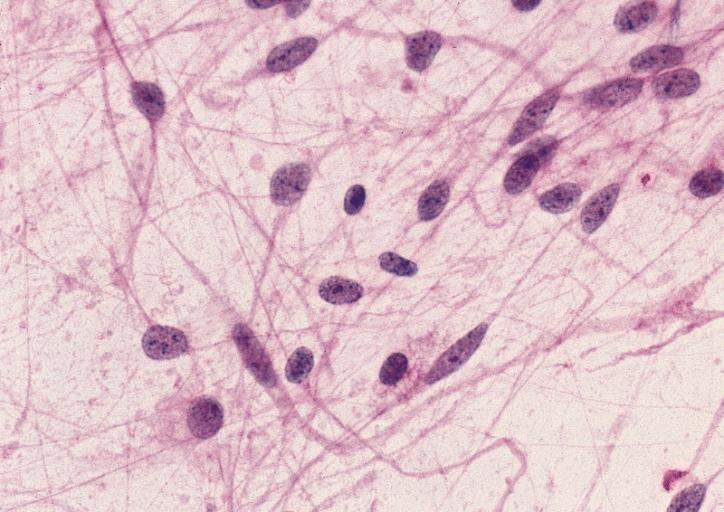
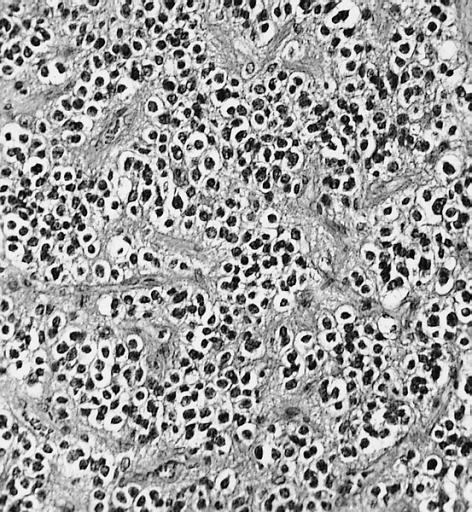
CNS: Pilocytic astrocytoma: variations in histologic appearance. As illustrated, many lesions are composed largely of spongy tissue rich in microcysts. Characteristic of pilocytic astrocytomas in general, the lesion is largely a solid mass of neoplastic cells without an obvious background of infiltrated brain.
-
CNS: Pilocytic astrocytoma: variations in histologic appearance. The perivascular radiating processes in some lesions can create a likeness to an ependymoma. Note the spongy background unusual for ependymomas.
-
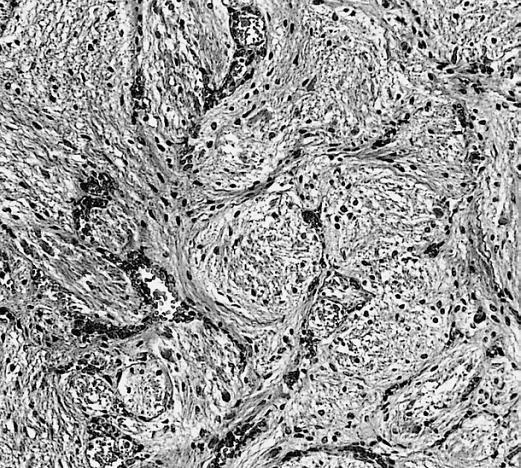
CNS: Pilocytic astrocytoma: variations in histologic appearance. Other pilocytic astrocytomas are solid, rather than microcystic, and may be lobular.
-
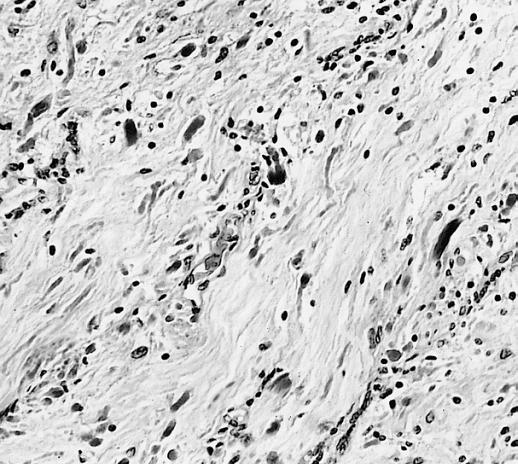
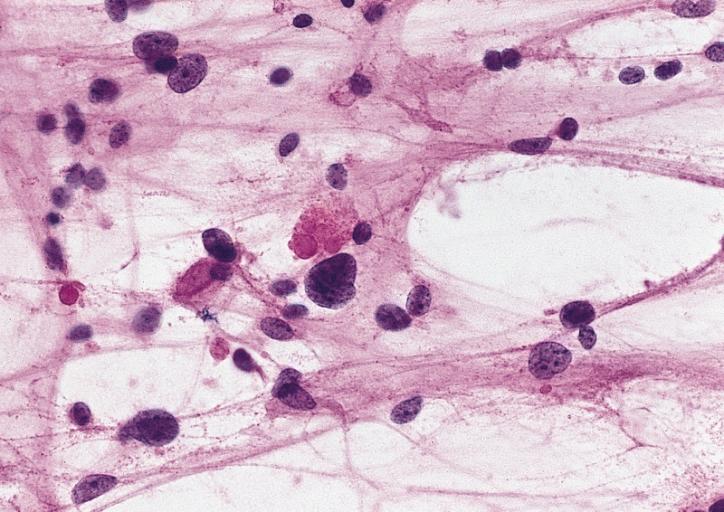
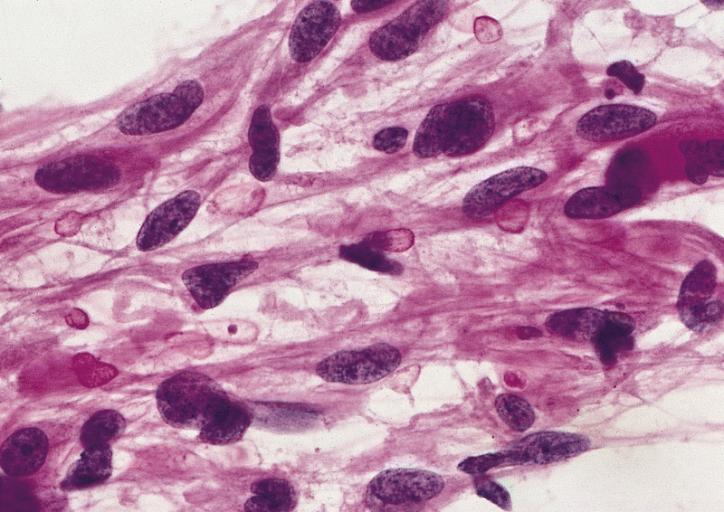
CNS: Pilocytic astrocytoma: variations in histologic appearance. Rosenthal fibers, usually confined to the solid rather than spongy regions are found in many pilocytic astrocytomas, but are not requisite for the diagnosis.
-
CNS: Pilocytic astrocytoma: variations in histologic appearance. Rosenthal fibers are extremely abundant in some lesions. Particularly in the cerebellum, it can be difficult to distinguish such solid, paucicellular, highly fibrillar pilocytic astrocytomas from reactive gliosis with abundant Rosenthal fiber formation.
-
CNS: Pilocytic astrocytoma: variations in histologic appearance. A loose array of polar cells creates an additional variant of pilocytic astrocytoma.
-
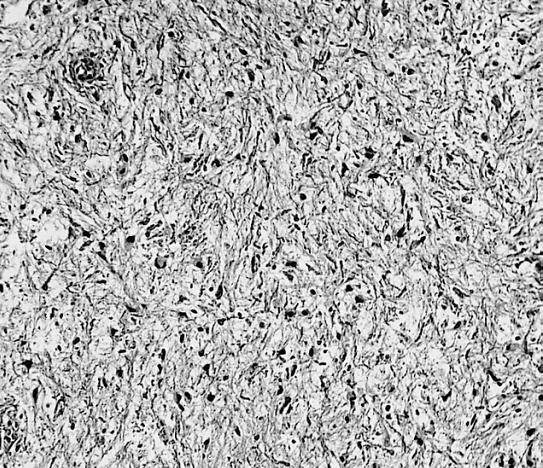
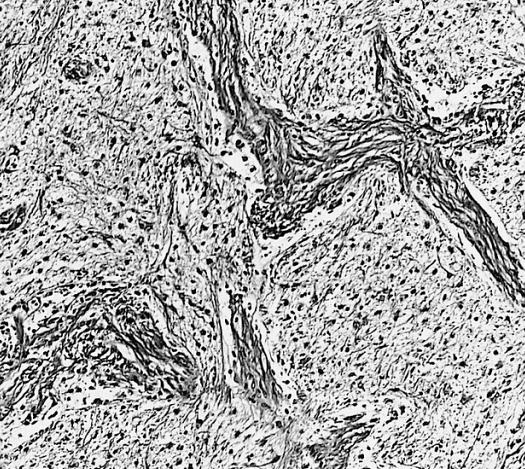
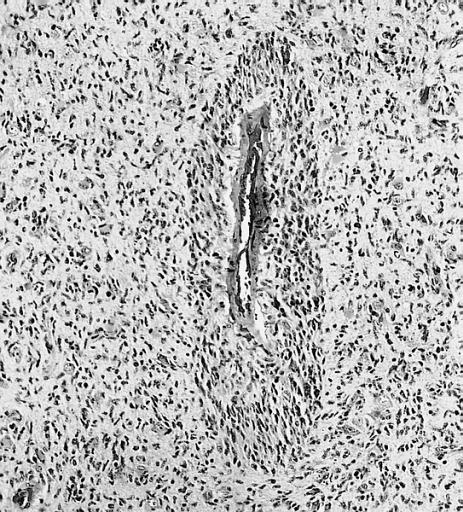
CNS: Pilocytic astrocytoma: variations in histologic appearance. Some pilocytic astrocytomas are traversed by prominent collagenous septa.
-
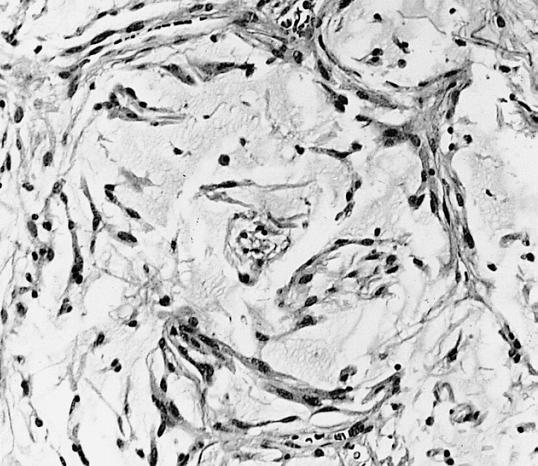
CNS: Pilocytic astrocytoma: variations in histologic appearance. Unusual pilocytic astrocytomas have an extensive mucinous background without microcysts.
-
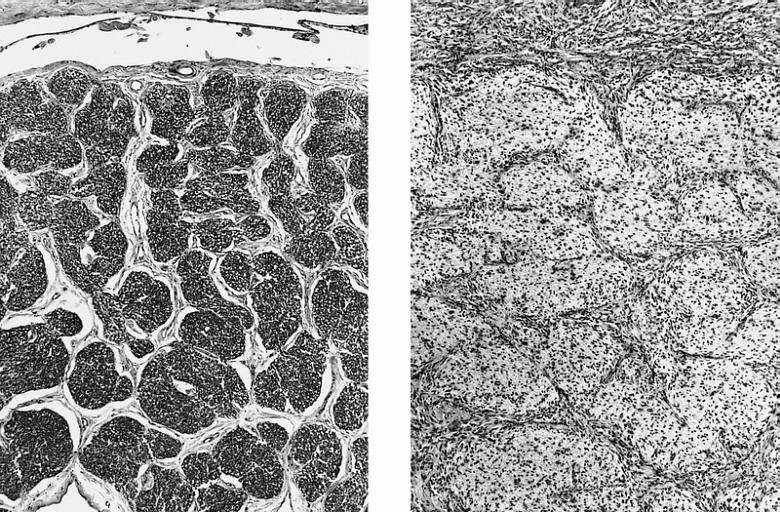
CNS: Comparison of normal optic nerve and pilocytic astrocytoma of the optic nerve. These two figures compare, at the same magnification, the normal optic nerve (left) with one containing a pilocytic astrocytoma (right). The neoplasm enlarges the compartments of the nerve and extends in collar-like fashion into the subarachnoid space.
-
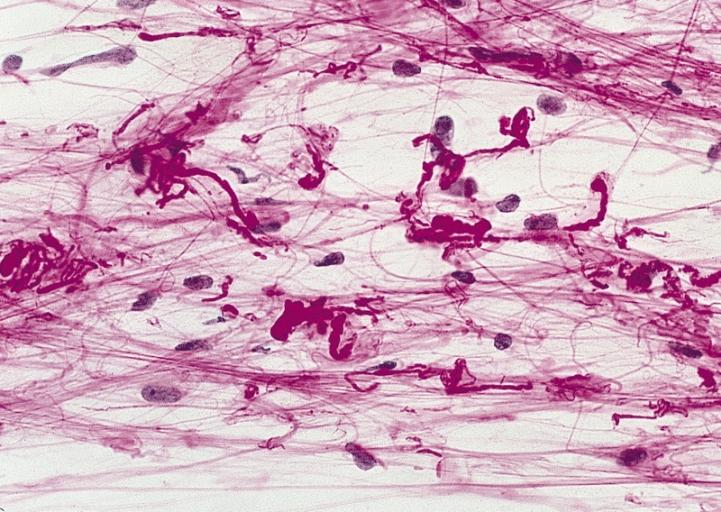
CNS: Pilocytic astrocytoma; The "hair cells" for which this lesion is named are readily seen.
-
CNS: Pilocytic astrocytoma; Nuclear hyperchromasia and pleomorphism are common. Note the typical cellular elongation, and, at the center of the illustration, the eosinophilic granular body that populates pilocytic astrocytomas and certain other slowly growing gliomas.
-
CNS: Pilocytic astrocytoma; Intracytoplasmic Rosenthal fibers are prominent in some pilocytic neoplasms.
-
Brain: Malignant ependymoma: Micro med mag H&E tumor cells.
-
CNS: Oligodendroglioma; Occasional oligodendrogliomas contain cells with minute, refractile eosinophilic bodies representing miniature Rosenthal fibers.
-
CNS: Oligodendroglioma; The cells of some oligodendrogliomas acquire sufficient cytoplasm and process formation to become decidedly astrocytic, but their nuclei retain the roundness, uniformity, and chromatin distribution typical of oligodendroglioma.
-
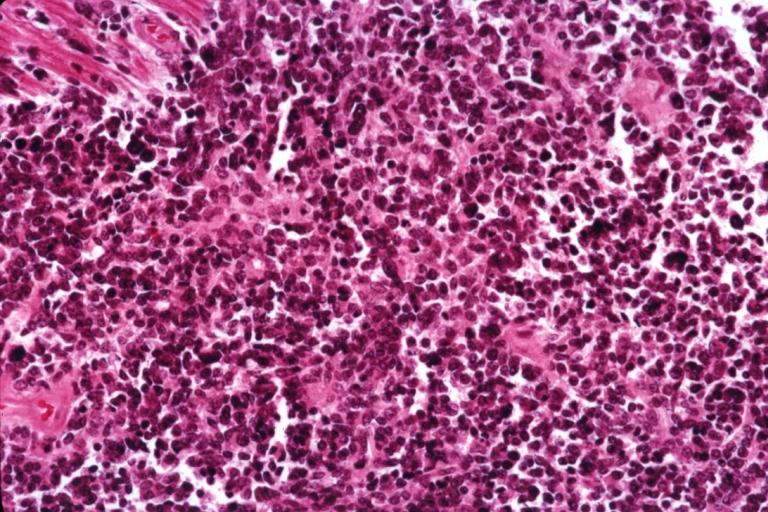
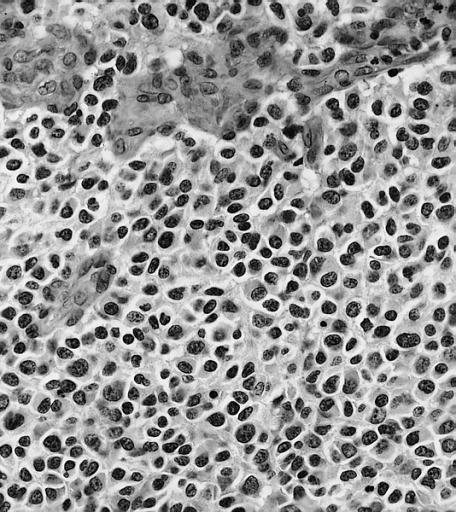
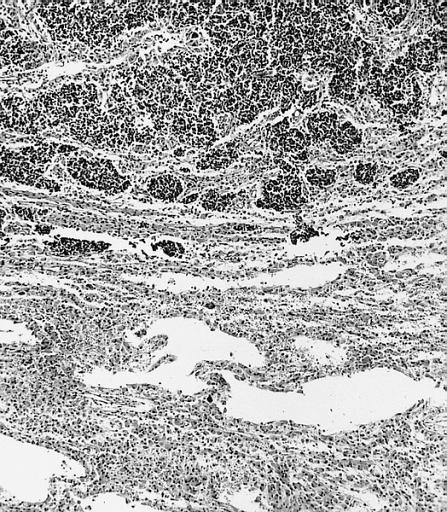
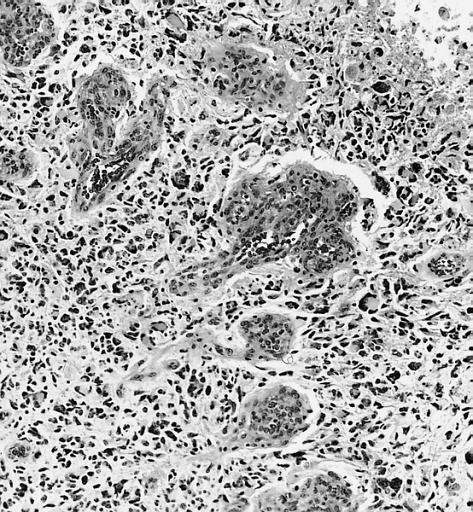
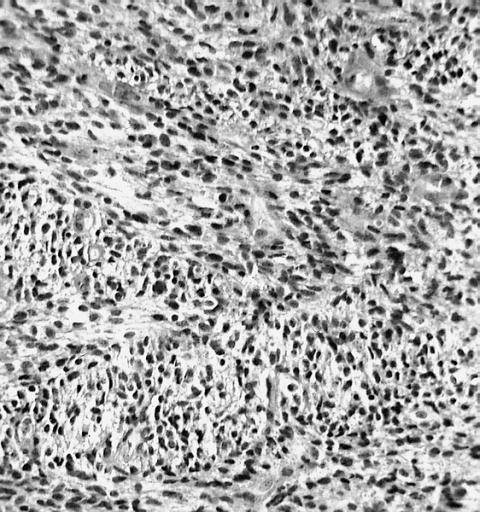
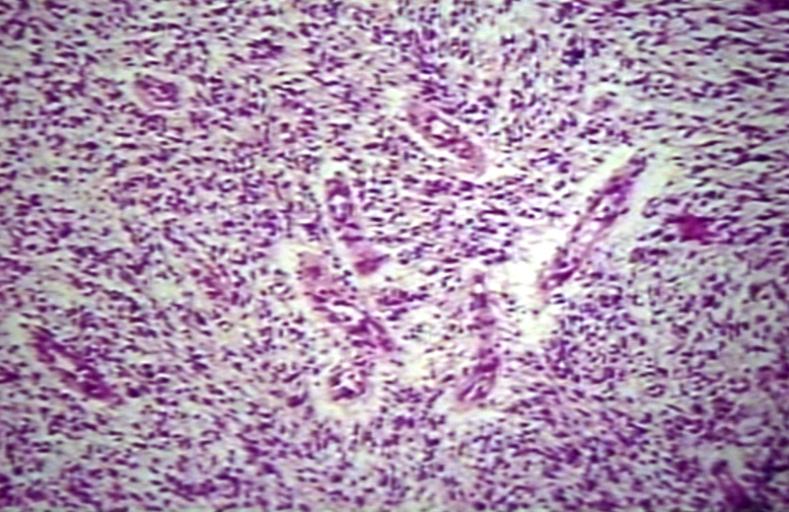
Anaplastic oligodendroglioma: Anaplastic oligodendrogliomas are highly cellular and associated with vascular proliferation.
-
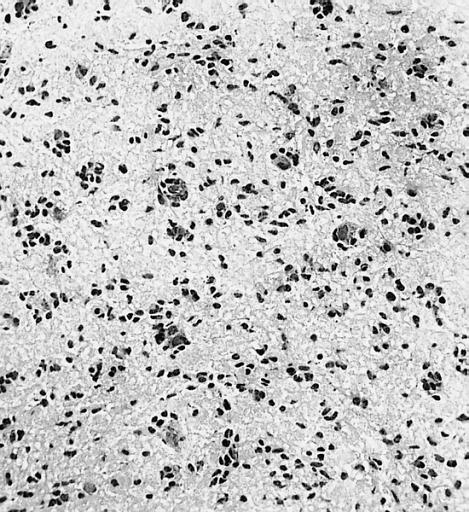
CNS: Oligodendroglioma (frozen section); Oligodendrogliomas in frozen sections lack the distinctive halos so often seen in permanent sections. Cellular monomorphism and infiltration of cerebral cortex with perineuronal satellitosis suggest the correct diagnosis.
-
CNS: Clear cell ependymoma; Perinuclear clearing similar to that seen in oligodendrogliomas is a prominent feature of the clear cell variant. Note the vague perivascular pseudorosettes. The lesion was a discrete occipital intraventricular mass.
-
CNS: Glioblastoma multiforme; Brain: Glioblastoma multiforme. Grade I-Ii: Micro med mag with H&E, tumor well shown
-
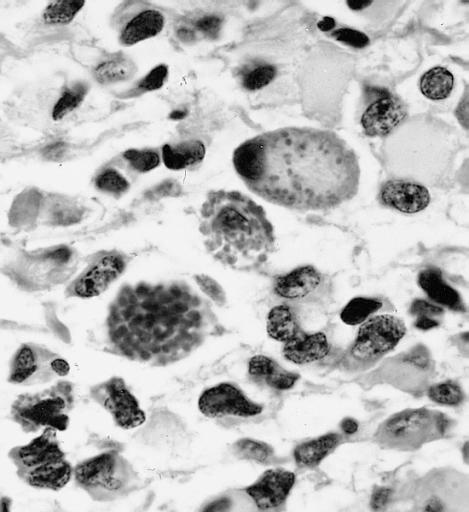
CNS: Glioblastoma multiforme arising in an astrocytoma. At higher magnification, gemistocytic astrocytoma with microcystic change is apparent at the bottom of the illustration and cellular nodules of glioblastoma multiforme are seen at the top. The 6-year history of symptoms attested to the initially low-grade nature of this astrocytic tumor.
-
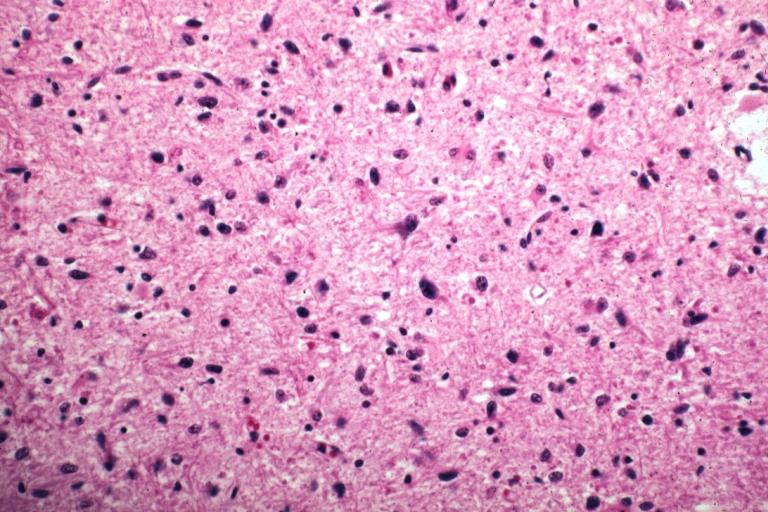
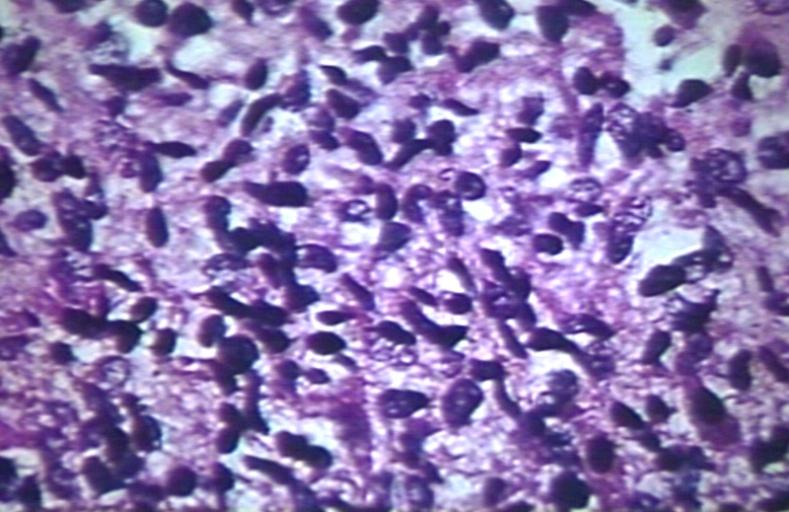
CNS: Glioblastoma multiforme; Characteristic of most glioblastomas are small cells with elongated nuclei and bipolar processes. As here, the chromatin is generally not markedly dense nor are nucleoli usually prominent.
-
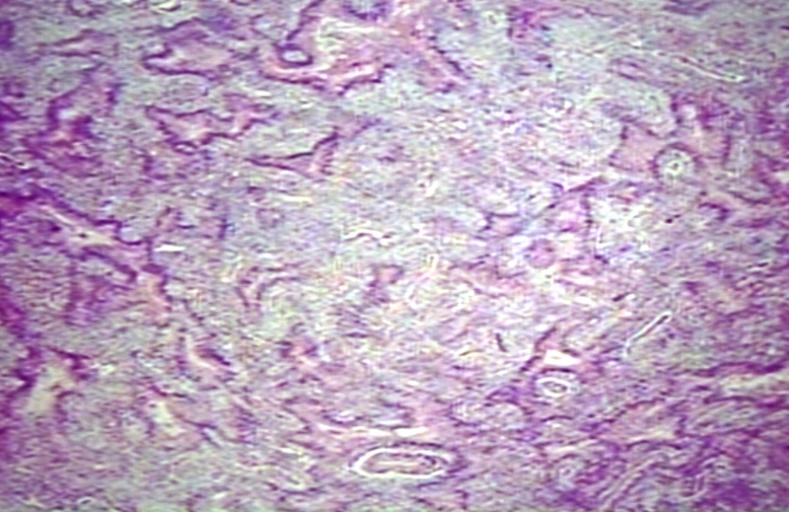
CNS: Glioblastoma multiforme; Vascular proliferation, a common feature of glioblastoma, produces tufts which often grow directionally. Here, as is often the case, they are oriented toward a focus of necrosis (top right).
-
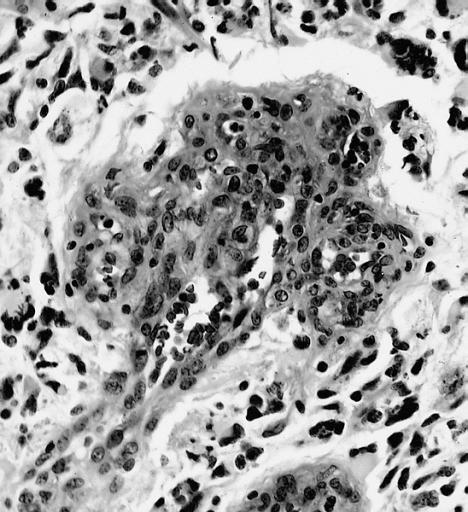
CNS: Glioblastoma multiforme; At high magnification, the neovascular tuft is a mass which, as can be confirmed by immunohistochemistry, is formed of both endothelial cells and smooth muscle cells (pericytes).
-
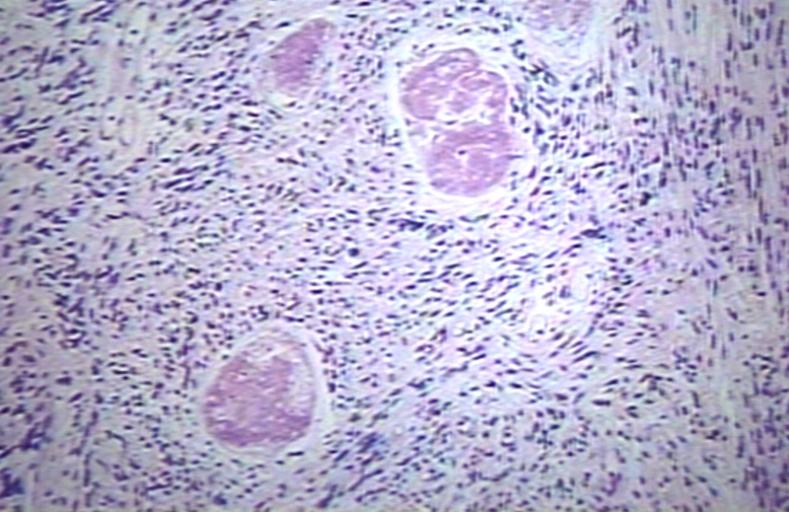
CNS: Glioblastoma multiforme; In many instances, necrosis is surrounded by a distinctive collar of cells, which are often smaller than those in surrounding neoplastic tissue. The phenomenon is referred to as pseudopalisading.
-
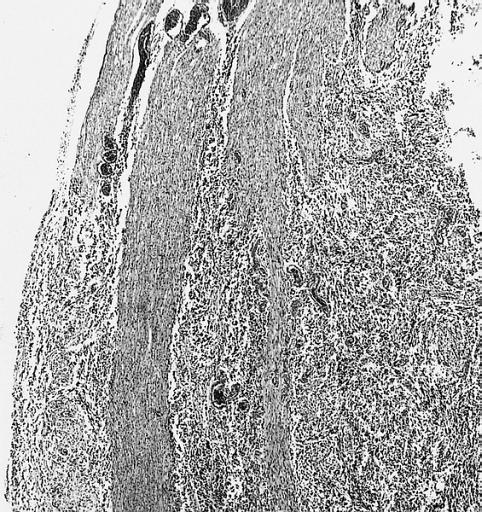
CNS: Cerebrospinal dissemination of glioblastoma multiforme; As seen at low (left) and high (right) magnification, the small undifferentiated-appearing cells of this glioblastoma are drop metastases colonizing the nerve roots of the cauda equina.
-
CNS: Cerebrospinal dissemination of glioblastoma multiforme; As seen at low (left) and high (right) magnification, the small undifferentiated-appearing cells of this glioblastoma are drop metastases colonizing the nerve roots of the cauda equina.
-
CNS: Glioblastoma multiforme; Higher magnification reveals the small cell nature of such tumors.
-
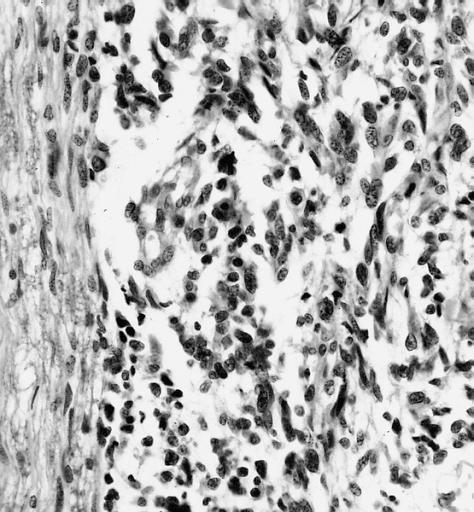
CNS: Glioblastoma multiforme; Some glioblastomas are especially infiltrative of the cerebral cortex where subpial, perivascular, and perineuronal accumulations are prominent.
-
CNS: Glioblastoma multiforme; Although this densely cellular and largely undifferentiated lesion technically merits a diagnosis of anaplastic astrocytoma, it is, for practical purposes, a glioblastoma.
-
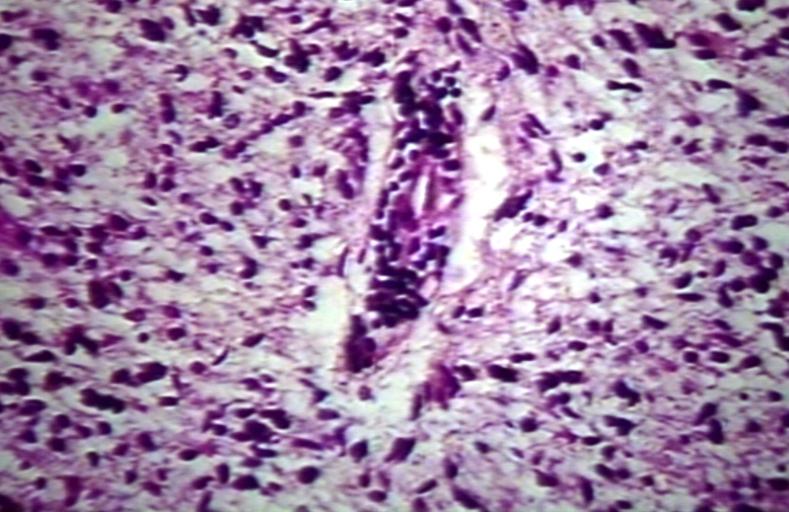
Brain: Glioblastoma multiforme; pallisading
-
Brain: Glioblastoma multiforme; vascular proliferation
-
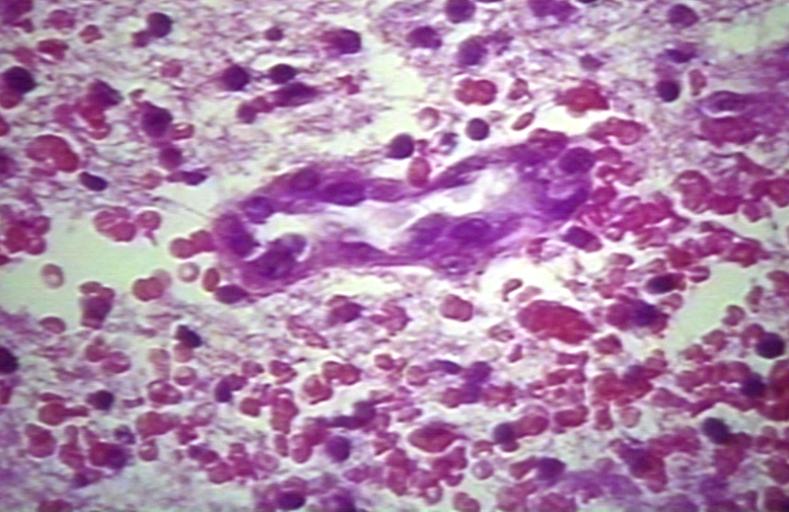
Brain: Glioblastoma multiforme; Plump and juicy endothelial cells, extravasated blood
-
Brain: Glioblastoma multiforme; perivascular lymphocytes
-
Brain: Glioblastoma multiforme; thrombosed vessel
-
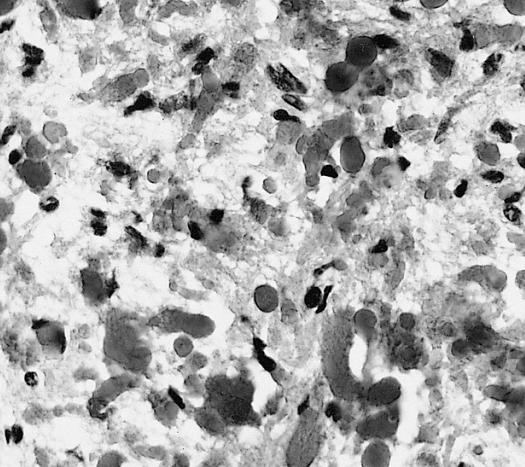
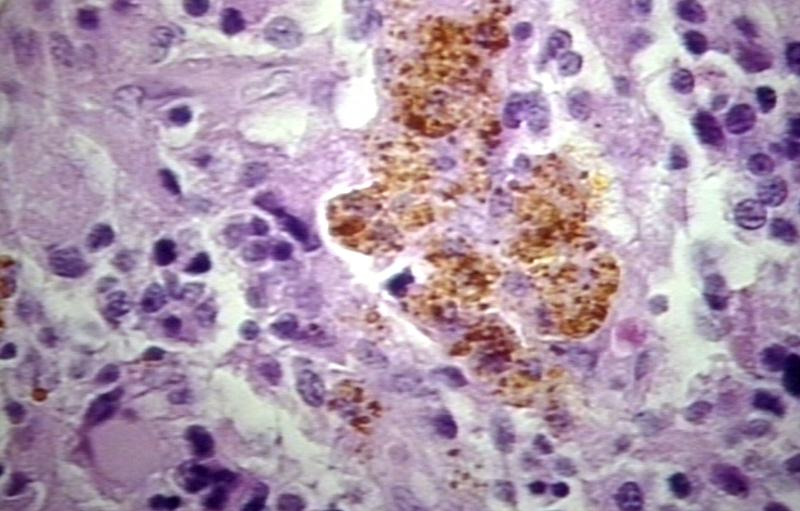
Brain: Glioblastoma multiforme; Hemosiderin in glioblastoma
References
- ↑ Pathology of glioma. Wikipedia. https://en.wikipedia.org/wiki/Glioma
- ↑ 2.0 2.1 Schwartzbaum JA, Fisher JL, Aldape KD, Wrensch M (2006). "Epidemiology and molecular pathology of glioma". Nat Clin Pract Neurol. 2 (9): 494–503, quiz 1 p following 516. doi:10.1038/ncpneuro0289. PMID 16932614.
- ↑ Reuss, D; von Deimling, A (2009). "Hereditary tumor syndromes and gliomas". Recent results in cancer research. Fortschritte der Krebsforschung. Progres dans les recherches sur le cancer. 171: 83–102. doi:10.1007/978-3-540-31206-2_5. PMID 19322539.
- ↑ Pathology of gliomas. Libre Pathology. http://librepathology.org/wiki/index.php/Oligodendroglioma
- ↑ Pathology of gliomas. Libre Pathology. http://librepathology.org/wiki/index.php/Oligodendroglioma