Lyme disease primary prevention: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
*Single spray during spring has shown to nymphal stage of ''I. scapularis'' significantly ranging from 67.9% for carbaryl to 97.4% for chlorpyrifos.<ref name="pmid8433317"/> | *Single spray during spring has shown to nymphal stage of ''I. scapularis'' significantly ranging from 67.9% for carbaryl to 97.4% for chlorpyrifos.<ref name="pmid8433317"/> | ||
*Evidence suggests that removal and controlled burning of vegetation (foilage and leaf litter) results is reduction in density of nymph stage of ''I. scapularis'' ranging from 72.7 to 100%.<ref name="pmid9701937">{{cite journal| author=Stafford KC, Ward JS, Magnarelli LA| title=Impact of controlled burns on the abundance of Ixodes scapularis (Acari: Ixodidae). | journal=J Med Entomol | year= 1998 | volume= 35 | issue= 4 | pages= 510-3 | pmid=9701937 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9701937 }} </ref><ref name="pmid7473629">{{cite journal| author=Schulze TL, Jordan RA, Hung RW| title=Suppression of subadult Ixodes scapularis (Acari: Ixodidae) following removal of leaf litter. | journal=J Med Entomol | year= 1995 | volume= 32 | issue= 5 | pages= 730-3 | pmid=7473629 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7473629 }} </ref> | *Evidence suggests that removal and controlled burning of vegetation (foilage and leaf litter) results is reduction in density of nymph stage of ''I. scapularis'' ranging from 72.7 to 100%.<ref name="pmid9701937">{{cite journal| author=Stafford KC, Ward JS, Magnarelli LA| title=Impact of controlled burns on the abundance of Ixodes scapularis (Acari: Ixodidae). | journal=J Med Entomol | year= 1998 | volume= 35 | issue= 4 | pages= 510-3 | pmid=9701937 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9701937 }} </ref><ref name="pmid7473629">{{cite journal| author=Schulze TL, Jordan RA, Hung RW| title=Suppression of subadult Ixodes scapularis (Acari: Ixodidae) following removal of leaf litter. | journal=J Med Entomol | year= 1995 | volume= 32 | issue= 5 | pages= 730-3 | pmid=7473629 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7473629 }} </ref> | ||
*Permethrin-impregnated cotton balls:<ref name="pmid1941940">{{cite journal| author=Deblinger RD, Rimmer DW| title=Efficacy of a permethrin-based acaricide to reduce the abundance of Ixodes dammini (Acari: Ixodidae). | journal=J Med Entomol | year= 1991 | volume= 28 | issue= 5 | pages= 708-11 | pmid=1941940 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1941940 }} </ref> | |||
**Permethrin-impregnated cotton balls in applicator tube are placed outdoors. | |||
**Fibres from the tube are carried to nests by white-footed mice which is the principle reservoir host of ''B. burgdorferi''. | |||
**Exposure to permethrin killed all ticks infesting these mice. | |||
**This method was a success in coastal New England area. | |||
**These permethrin-impregnated cotton balls are available commercially as 'Damminix tick tubes'. | |||
**However, this method was found uneffective in New York and Connecticut.<ref name="pmid1941916">{{cite journal| author=Daniels TJ, Fish D, Falco RC| title=Evaluation of host-targeted acaricide for reducing risk of Lyme disease in southern New York state. | journal=J Med Entomol | year= 1991 | volume= 28 | issue= 4 | pages= 537-43 | pmid=1941916 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1941916 }} </ref><ref name="pmid1495085">{{cite journal| author=Stafford KC| title=Third-year evaluation of host-targeted permethrin for the control of Ixodes dammini (Acari: Ixodidae) in southeastern Connecticut. | journal=J Med Entomol | year= 1992 | volume= 29 | issue= 4 | pages= 717-20 | pmid=1495085 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1495085 }} </ref> | |||
===Minimizing tick exposure=== | ===Minimizing tick exposure=== | ||
{| | {| | ||
| Line 49: | Line 56: | ||
#After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water. | #After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water. | ||
| | | | ||
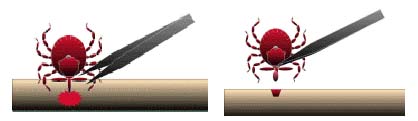
[[Image:Tick removal process.jpg| | [[Image:Tick removal process.jpg|500px|center|thumb|Tick removal process]] | ||
| | |} | ||
{| | |||
| | | | ||
'''Note:''' | '''Note:''' | ||
| Line 56: | Line 64: | ||
*Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. <ref name="Tick Removal CDC”">Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015</ref> | *Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. <ref name="Tick Removal CDC”">Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015</ref> | ||
| | | | ||
[[Image:Removal.jpg| | [[Image:Removal.jpg|300px|center|thumb|Removal of an embedded tick using fine-tipped tweezers]] | ||
|} | |} | ||
Revision as of 20:46, 3 August 2017
|
Lyme disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lyme disease primary prevention On the Web |
|
American Roentgen Ray Society Images of Lyme disease primary prevention |
|
Risk calculators and risk factors for Lyme disease primary prevention |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2]Ilan Dock, B.S.
Overview
Primary prevention of Lyme disease involves reducing exposure to ticks. Scientists have been developing all-natural chemical compounds made from plants that can repel or kill ticks. A Lyme disease vaccine is no longer available.
Primary Prevention
Tick control
- Tick control can help prevent many tick-borne diseases including Lyme disease, human granulomatous anaplasmosis(HGA), babesiosis and many others.
- Use of acaricidal sprays on vegetation where tick lives is consistently most effective method.
- Acaricides are pesticides that kill members of the arachnid subclass Acari, which includes ticks and mites.
- Examples of acaricide includes:[1][2][3]
- Carbaryl
- Chlorpyrifos
- Cyfluthrin
- Deltamethrin
- Single spray during spring has shown to nymphal stage of I. scapularis significantly ranging from 67.9% for carbaryl to 97.4% for chlorpyrifos.[1]
- Evidence suggests that removal and controlled burning of vegetation (foilage and leaf litter) results is reduction in density of nymph stage of I. scapularis ranging from 72.7 to 100%.[4][5]
- Permethrin-impregnated cotton balls:[6]
- Permethrin-impregnated cotton balls in applicator tube are placed outdoors.
- Fibres from the tube are carried to nests by white-footed mice which is the principle reservoir host of B. burgdorferi.
- Exposure to permethrin killed all ticks infesting these mice.
- This method was a success in coastal New England area.
- These permethrin-impregnated cotton balls are available commercially as 'Damminix tick tubes'.
- However, this method was found uneffective in New York and Connecticut.[7][8]
Minimizing tick exposure
 |
Best way to prevent Lyme disease is to avoid tick infested areas. But it is unreasonable to assume that a person can completely eliminate activities that may result in tick exposure. Therefore, preventive measures should emphasize personal protection when exposed to natural areas where ticks are present:[9]
|
The best way to remove a tick
|
Note:
|
 |
Prophylaxis
- After a tick bite, routine use of antibiotic prophylaxis is not recommended.[9]
- A single dose of doxycycline(avoid in pregnancy and children <8 years) may be offered to adults (200mg) and children (4mg/kg, maximum 200mg) if all of the criteria are fulfilled:
- The tick is identified as I. scapularis (adult or nymph)
- The tick is attached for ⩾36 hours. It is estimated by the degree of engorgement of the tick with blood or approximating the time of exposure to the tick.
- Within 72 hours of tick removal
- Local infection rate of tick with B. burgdorferi is ⩾20%
- There is no contraindication to use of doxycycline.
Vaccination
- A vaccine, called Lymerix, against a North American strain of the spirochetal bacteria was available from 1998 to 2002.
- It was produced by GlaxoSmithKline (GSK) and was based on the outer surface protein A (Osp-A) of Borrelia. Osp-A causes the human immune system to create antibodies that attack that protein.
- A group of patients who have been administered Lymerix developed arthritis, muscle pain and other troubling symptoms post-vaccination. Class-action litigation against GSK followed. Cassidy v. SmithKline Beecham, No. 99-10423 (Ct. Common Pleas, PA state court) (common settlement case).[15]
- It was later learned that patients with the genetic allele HLA-DR4 were susceptible to T-cell cross-reactivity between epitopes of OspA and lymphocyte function-associated antigen in these patients causing an autoimmune reaction.[16]
- New vaccines are being researched using outer surface protein C (Osp-C) and glycolipoprotein as methods of immunization.[17][18]
References
- ↑ 1.0 1.1 Curran KL, Fish D, Piesman J (1993). "Reduction of nymphal Ixodes dammini (Acari: Ixodidae) in a residential suburban landscape by area application of insecticides". J Med Entomol. 30 (1): 107–13. PMID 8433317.
- ↑ Stafford KC (1991). "Effectiveness of carbaryl applications for the control of Ixodes dammini (Acari: Ixodidae) nymphs in an endemic residential area". J Med Entomol. 28 (1): 32–6. PMID 1903451.
- ↑ Schulze TL, Jordan RA, Hung RW, Taylor RC, Markowski D, Chomsky MS (2001). "Efficacy of granular deltamethrin against Ixodes scapularis and Amblyomma americanum (Acari: Ixodidade) nymphs". J Med Entomol. 38 (2): 344–6. PMID 11296847.
- ↑ Stafford KC, Ward JS, Magnarelli LA (1998). "Impact of controlled burns on the abundance of Ixodes scapularis (Acari: Ixodidae)". J Med Entomol. 35 (4): 510–3. PMID 9701937.
- ↑ Schulze TL, Jordan RA, Hung RW (1995). "Suppression of subadult Ixodes scapularis (Acari: Ixodidae) following removal of leaf litter". J Med Entomol. 32 (5): 730–3. PMID 7473629.
- ↑ Deblinger RD, Rimmer DW (1991). "Efficacy of a permethrin-based acaricide to reduce the abundance of Ixodes dammini (Acari: Ixodidae)". J Med Entomol. 28 (5): 708–11. PMID 1941940.
- ↑ Daniels TJ, Fish D, Falco RC (1991). "Evaluation of host-targeted acaricide for reducing risk of Lyme disease in southern New York state". J Med Entomol. 28 (4): 537–43. PMID 1941916.
- ↑ Stafford KC (1992). "Third-year evaluation of host-targeted permethrin for the control of Ixodes dammini (Acari: Ixodidae) in southeastern Connecticut". J Med Entomol. 29 (4): 717–20. PMID 1495085.
- ↑ 9.0 9.1 Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS; et al. (2006). "The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America". Clin Infect Dis. 43 (9): 1089–134. doi:10.1086/508667. PMID 17029130.
- ↑ Fradin MS (1998). "Mosquitoes and mosquito repellents: a clinician's guide". Ann Intern Med. 128 (11): 931–40. PMID 9634433.
- ↑ Carroll JF, Klun JA, Debboun M (2005). "Repellency of deet and SS220 applied to skin involves olfactory sensing by two species of ticks". Med Vet Entomol. 19 (1): 101–6. doi:10.1111/j.0269-283X.2005.00559.x. PMID 15752184.
- ↑ Centers for Disease Control (CDC) (1989). "Seizures temporally associated with use of DEET insect repellent--New York and Connecticut". MMWR Morb Mortal Wkly Rep. 38 (39): 678–80. PMID 2506420.
- ↑ General Tick Disease Information. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/symptoms.html Accessed on December 30, 2015
- ↑ Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015
- ↑ Safety/Efficacy concerns re: Lyme vaccine: LYMErix Controversy LymeInfo.net
- ↑ Willett TA, Meyer AL, Brown EL, Huber BT (2004). "An effective second-generation outer surface protein A-derived Lyme vaccine that eliminates a potentially autoreactive T cell epitope". Proc. Natl. Acad. Sci. U.S.A. 101 (5): 1303–8. doi:10.1073/pnas.0305680101. PMID 14742868.
- ↑ Earnhart CG, Marconi RT (2007). "OspC phylogenetic analyses support the feasibility of a broadly protective polyvalent chimeric Lyme disease vaccine". Clin. Vaccine Immunol. 14 (5): 628–34. doi:10.1128/CVI.00409-06. PMID 17360854.
- ↑ Pozsgay V, Kubler-Kielb J (2007). "Synthesis of an experimental glycolipoprotein vaccine against Lyme disease". Carbohydr. Res. 342 (3–4): 621–6. doi:10.1016/j.carres.2006.11.014. PMID 17182019.