Gonorrhea overview: Difference between revisions
No edit summary |
(→Images) |
||
| Line 65: | Line 65: | ||
The following are images associated with gonorrhea physical examination.<ref>STD Gonorrhea Infection Gallery http://www.std-gov.org/std_picture/gonorrhea_w.htm Accessed on September 22, 2016</ref><ref name=CDCGonorrheapic>Centers for Disease Control and Prevention. Public Health Image Library (PHIL) http://phil.cdc.gov/phil/home.asp Accessed on September 22, 2016</ref> | The following are images associated with gonorrhea physical examination.<ref>STD Gonorrhea Infection Gallery http://www.std-gov.org/std_picture/gonorrhea_w.htm Accessed on September 22, 2016</ref><ref name=CDCGonorrheapic>Centers for Disease Control and Prevention. Public Health Image Library (PHIL) http://phil.cdc.gov/phil/home.asp Accessed on September 22, 2016</ref> | ||
<div align="center"> | <div align="center"> | ||
<gallery heights=" | <gallery heights="150" widths="150"> | ||
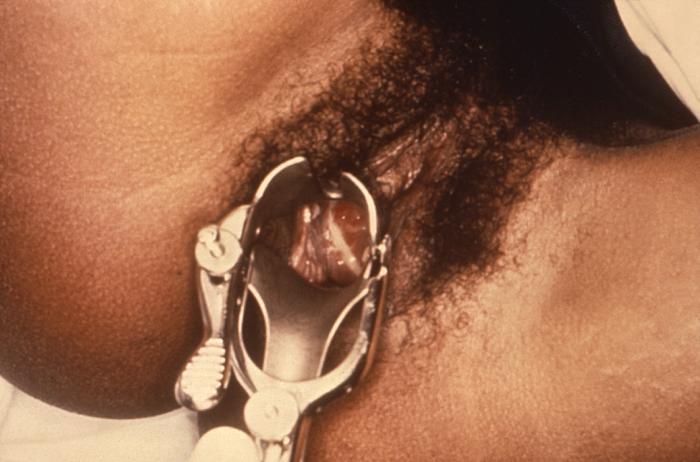
Image: Gonorrhea07.jpeg|Purulent discharge emanating from the cervical os, and pooling in the vagina | Image: Gonorrhea07.jpeg|Purulent discharge emanating from the cervical os, and pooling in the vagina | ||
Image:Gonorrhea penile discharge.jpg|Penile discharge in a patient with gonorrhea | Image:Gonorrhea penile discharge.jpg|Penile discharge in a patient with gonorrhea | ||
| Line 71: | Line 71: | ||
Image:220px-Gonococcal_ophthalmia_neonatorum.jpg|[[Ophthalmia neonatorum]] | Image:220px-Gonococcal_ophthalmia_neonatorum.jpg|[[Ophthalmia neonatorum]] | ||
Image:Ophthalmia neonatorum (gonococcal conjunctivitis).jpg|Gonococcal infection of the conjunctiva in a neonate | Image:Ophthalmia neonatorum (gonococcal conjunctivitis).jpg|Gonococcal infection of the conjunctiva in a neonate | ||
Image:Gonorrhea28.jpg[[Colposcopic]] view of this patient’s [[cervix]] reveled an eroded ostium due to Neisseria gonorrhea infection | Image:Gonorrhea28.jpg[[Colposcopic]] view of this patient’s [[cervix]] reveled an eroded ostium due to Neisseria gonorrhea infection | ||
Image:Gonorrhea29.jpg|The lesion on the left hand due to the systemic dissemination of the Neisseria gonorrhea. | Image:Gonorrhea29.jpg|The lesion on the left hand due to the systemic dissemination of the Neisseria gonorrhea. | ||
Revision as of 04:14, 3 October 2016
|
Gonorrhea Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gonorrhea overview On the Web |
|
American Roentgen Ray Society Images of Gonorrhea overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2]
Overview
Gonorrhea (gonorrhoea in British English) is amongst the most common sexually transmitted diseases in the world and is caused by Gram-negative bacterium Neisseria gonorrheae. The term comes from Ancient Greek γονόρροια (gonórrhoia), literally "flow of seed"; in ancient times it was incorrectly believed that the pus discharge associated with the disease contained semen.[1]
The first place this bacterium infects is usually the columnar epithelium of the urethra and endocervix. Non-genital sites in which it thrives are in the rectum, the oropharynx and the conjunctivae of the eyes. The vulva and vagina in women are usually spared because they are lined by stratified epithelial cells—in women the cervix is the usual first site of infection.
Gonorrhea spreads during sexual intercourse. Infected women also can pass gonorrhea to their newborn infants during delivery, causing eye infections (conjunctivitis) in their babies (which if left untreated, can cause blindness). Doctors have often attempted to treat this immediately by applying small amounts of silver nitrate to the eyes of all newborn babies. Gonorrhea among females can also be transmitted from one individual to another via contact to surfaces that may still be damp from prior contact.
Historical Perspective
Gonorrhea is an ancient disease with Biblical Testament references. However, the exact time of onset of gonorrhea cannot be accurately determined from the historical record.[2] The term comes from Ancient Greek γονόρροια (gonórrhoia), literally "flow of seed"; in ancient times it was incorrectly believed that the pus discharge associated with the disease contained semen.[3] In 1879, gonorrhea was referred to as “the clap” by German bacteriologist Albert Neisser.[4]
Classification
Based on anatomic location gonorrhea may be classified into three subtypes: urogenital, extragenital, and disseminated gonococcal infection. Additionally, gonococcal infections may be classified according to the affected organ system into many subtypes.[5][6][7]
Pathophysiology
Gonorrhea is a sexually transmitted disease (STD) that is caused by Neisseria gonorrhea. It can infect mucus-secreting epithelial cells both in men and women. The recognized routes of transmission of the Neisseria gonorrhoeae include vaginal intercourse, rectal intercourse, fellatio, cunnilingus, and perinatal. The main pathogenicity of the Neisseria gonorrhea obtains from the attachment ability of the surface pili to the surface of the urethra, fallopian tubes and endocervix.[8][9][10] Anotehr virulence factors of gonorrhea is porin. two main porin serotypes include PorB.1A strains (resulting in a disseminated gonococcal infection) and PorB.1B strains (resulting in local genital infections).[11][12][13]
In pregnancy, gonococcus can be transmitted to the fetus at the time of delivery. This results in infection of the conjuctiva. This appears 1 to 4 days after birth as severe discharge with marked swelling and redness of the eyelids and conjunctiva. Additionally, development of disseminated gonococcal infection is the result of Neisserial organisms dissemination to the blood due to a variety of predisposing factors, such as change in PH, pregnancy, menstruation, PorB.1A strains, and complement deficiencies.[14][15][16][17]
Causes
Neisseria gonorrhoeae, also known as gonococci (plural), gonococcus (singular), or gonorrhoea (in British English), is a species of Gram-negative coffee bean-shaped diplococci bacteria responsible for the sexually transmitted infection gonorrhea.[18] Gonorrhea (gonorrhoea in British English) is amongst the most common sexually transmitted diseases in the world and is caused by Gram-negative bacterium Neisseria gonorrheae. The term comes from Ancient Greek γονόρροια (gonórrhoia), literally "flow of seed"; in ancient times it was incorrectly believed that the pus discharge associated with the disease contained semen.[19]
Differential diagnosis
Gonorrhea must be differentiated from other sexually transmitted pathogens, nongonococcal urethritis, vaginitis, cervicitis, urinary tract infections, prostatitis, and orchitis. Additionally, disseminated gonococcal infection must be differentiated from herpes simplex virus (HSV), nongonococcal septic arthritis, syphilis, HIV infection, rheumatic fever, reactive arthritis , and Lyme disease.[5][6][7]
Epidemiology
Gonorrhea is a very common infectious disease. In the United State, gonorrhea is the second most common STD after chlamydia.[20] In 2012, the incidence of gonorrhea was reported 106 million cases worldwide.[21] In 2014, a total 350,062 cases gonorrhea were reported in United States.[22]
Risk factors
Common risk factors in the development of gonorrhea include sexual activity, multiple sex partners, previous history of sexually transmitted diseases, partner with a past history of any sexually transmitted disease, and failure to use a condom during sex.[23][24][25]
Screening
The U.S. Preventive Services and Task Force (USSTF) recommends screening for gonorrhea in sexually active women age 24 years and younger and in older women who are at increased risk for infection. The current evidence is insufficient to assess the balance of benefits and harms of screening for gonorrhea in heterosexual men. However, USSTF recommends at least annual screening for gonorrhea among men who have sex with men (MSM).[26][27][28]
Natural history, complications, and prognosis
In 50 to 70% of women, the Initial infection with Neisseria gonorrhea may be asymptomatic. Initial infection is usually seen in the cervical region, but due to the presence of the surface pili, the infection may ascend through the uterus into the fallopian tubes and finally out into the peritoneal cavity. The exact incubation period of gonorrhea is unknown. It may result in cervicitis and urethritis which may present with dysuria, vaginal pruritus and vaginal mucopurulent discharge. If gonococcal infection left untreated, it can progress to fibrosis. The fibrosis can result in fallopian tube stricture, tubo-ovarian cyst or abscess, pelvic inflammatory disease (PID), Perihepatitis (Fitz-Hugh-Curtis syndrome),and bartholinitis.The most common complication of untreated gonorrhea is pelvic inflammatory disease (PID) which may lead to increased risks of ectopic pregnancy. If left untreated, Ectopic pregnancies can be life-threatening to the mother.[29][30] In men, untreated gonorrhea may result in inflammation of the epididymis (epididymitis), prostate gland (prostatitis) and urethral structure (urethritis). disseminated gonococcal infection (DGI) occurs in about 0.5 to 3% of patients, commonly following asymptomatic mucosal infection in both sexes. However, women are more likely to developed disseminated gonococcal infection than men. Disseminated gonococcal infection can lead to multiple distant sites of infection such as brain, heart and joints. Most common sign and symptoms include arthritis or arthralgias, tenosynovitis, and multiple skin lesions.
Common complications of gonococcal infection in women may include salpingitis, pelvic inflammatory disease, Infertility, dyspareunia, and ectopic pregnancy Common complications of gonococcal infection in men may include post-inflammatory urethral strictures, urethral abscess, Penile lymphangitis, *penile edema, urinary tract infection, and kidney failure. The prognosis of urogenital and disseminated gonococcal infection are generally good with adequate treatment.
Diagnosis
History and Symptoms
It is critical to obtain a detailed and thorough sexual history from the patient. Specific areas of focus when obtaining a history from the patient include number and type of sexual partners, contraception use, and previous history of sexually transmitted diseases.The majority of women with gonorrhea are asymptomatic while others have vaginal discharge, lower abdominal pain, or pain with intercourse. Common symptom of gonococcal infection among men includes urethritis, which associated with burning with urination and discharge from the penis. Either sex may also acquire gonorrhea of the throat from performing oral sex on an infected partner, usually a male partner. Such infection is asymptomatic in 90% of cases, and produces a sore throat in the remaining 10%. The incubation period is 2 to 14 days with most of these symptoms occurring between 4–6 days after being infected.[5][31][32][33] Rarely, gonorrhea may cause skin legions and joint infection (pain and swelling in the joints) after traveling through the blood stream. Very rarely it may settle in the heart causing endocarditis or in the spinal column causing meningitis.[7]
Physical examination
Women with gonococcal infection usually appear to be well until complications such as PID develop. Physical examination of women with gonococcal infection is usually remarkable for mucopurulent urethral, cervical or vaginal discharge, friable appearance of the cervix, and cervical motion tenderness. Common physical examination finding of gonococcal infection among men includes mucopurulent urethral discharge. Less commonly penile edema, and epididymal tenderness and edema (epididymitis) may also be seen as a part of complicated gonococcal infection.[5][31][32]
Physical examination of patients with pharyngeal gonococcal infection is usually remarkable for mild pharyngeal exudates and rectal gonococcal infection is usually remarkable for mucopurulent anal discharge. Physical examination of patients with disseminated gonococcal infection (DGI) is usually remarkable for fever, pustular or vesicular rash, and musculoskeletal findings.[5][7]
Images
The following are images associated with gonorrhea physical examination.[34][35]
-
Purulent discharge emanating from the cervical os, and pooling in the vagina
-
Penile discharge in a patient with gonorrhea
-
Gonococcal pharyngitis
-
Gonococcal infection of the conjunctiva in a neonate
-
The lesion on the left hand due to the systemic dissemination of the Neisseria gonorrhea.
-
Lesions of skin and arthritic knee joints due to Neisseria gonorrhea
References
- ↑ Definition of the term gonorrhea
- ↑ Genco, Caroline Attardo. Neisseria: molecular mechanisms of pathogenesis. Horizon Scientific Press, 2010.
- ↑ Definition of the term gonorrhea
- ↑ Unemo M, Shafer WM. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin Microbiol Rev 2014;27:587–613.
- ↑ 5.0 5.1 5.2 5.3 5.4 Workowski KA, Bolan GA, Centers for Disease Control and Prevention (2015). "Sexually transmitted diseases treatment guidelines, 2015". MMWR Recomm Rep. 64 (RR-03): 1–137. PMID 26042815.
- ↑ 6.0 6.1 Rompalo AM, Hook EW, Roberts PL, Ramsey PG, Handsfield HH, Holmes KK (1987). "The acute arthritis-dermatitis syndrome. The changing importance of Neisseria gonorrhoeae and Neisseria meningitidis". Arch Intern Med. 147 (2): 281–3. PMID 3101626.
- ↑ 7.0 7.1 7.2 7.3 Rice PA (2005). "Gonococcal arthritis (disseminated gonococcal infection)". Infect Dis Clin North Am. 19 (4): 853–61. doi:10.1016/j.idc.2005.07.003. PMID 16297736.
- ↑ Sparling PF (1966). "Genetic transformation of Neisseria gonorrhoeae to streptomycin resistance". J Bacteriol. 92 (5): 1364–71. PMC 276432. PMID 4958881.
- ↑ Swanson J (1973). "Studies on gonococcus infection. IV. Pili: their role in attachment of gonococci to tissue culture cells". J Exp Med. 137 (3): 571–89. PMC 2139381. PMID 4631989.
- ↑ Wolfgang M, Lauer P, Park HS, Brossay L, Hébert J, Koomey M (1998). "PilT mutations lead to simultaneous defects in competence for natural transformation and twitching motility in piliated Neisseria gonorrhoeae". Mol Microbiol. 29 (1): 321–30. PMID 9701824.
- ↑ Young JD, Blake M, Mauro A, Cohn ZA (1983). "Properties of the major outer membrane protein from Neisseria gonorrhoeae incorporated into model lipid membranes". Proc Natl Acad Sci U S A. 80 (12): 3831–5. PMC 394146. PMID 6407021.
- ↑ Ram S, Cullinane M, Blom AM, Gulati S, McQuillen DP, Monks BG; et al. (2001). "Binding of C4b-binding protein to porin: a molecular mechanism of serum resistance of Neisseria gonorrhoeae". J Exp Med. 193 (3): 281–95. PMC 2195916. PMID 11157049.
- ↑ Ram S, McQuillen DP, Gulati S, Elkins C, Pangburn MK, Rice PA (1998). "Binding of complement factor H to loop 5 of porin protein 1A: a molecular mechanism of serum resistance of nonsialylated Neisseria gonorrhoeae". J Exp Med. 188 (4): 671–80. PMC 2213355. PMID 9705949.
- ↑ WATRING, WATSON G., and DANIEL L. VAUGHN. "Gonococcemia in pregnancy." Obstetrics & Gynecology 48.4 (1976): 428-430.
- ↑ Angulo, Juan M., and Luis R. Espinoza. "Gonococcal arthritis." Comprehensive therapy 25.3 (1999): 155-162.
- ↑ Bohnhoff M, Morello JA, Lerner SA (1986). "Auxotypes, penicillin susceptibility, and serogroups of Neisseria gonorrhoeae from disseminated and uncomplicated infections". J Infect Dis. 154 (2): 225–30. PMID 3088132.
- ↑ O'Brien JP, Goldenberg DL, Rice PA (1983). "Disseminated gonococcal infection: a prospective analysis of 49 patients and a review of pathophysiology and immune mechanisms". Medicine (Baltimore). 62 (6): 395–406. PMID 6415361.
- ↑ Ryan, KJ; Ray, CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Definition of the term gonorrhea
- ↑ CDC. Sexually transmitted disease surveillance 2013. Atlanta: US Department of Health and Human Services; 2014.
- ↑ World Health Organization. Emergence of multi-drug resistant Neisseria gonorrhoeae http://apps.who.int/iris/bitstream/10665/70603/1/WHO_RHR_11.14_eng.pdf Accessed on September 8, 2016
- ↑ Centers for Disease Control and Prevention. Reported STDs in the United States 2014 National Data for Chlamydia, Gonorrhea, and Syphilis http://www.cdc.gov/std/stats14/std-trends-508.pdf
- ↑ Klausner JD, Barrett DC, Dithmer D, Boyer CB, Brooks GF, Bolan G (1998). "Risk factors for repeated gonococcal infections: San Francisco, 1990-1992". J Infect Dis. 177 (6): 1766–9. PMID 9607868.
- ↑ Centers for Disease Control and Prevention http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm Accessed September 20, 2016
- ↑ Mertz KJ, Levine WC, Mosure DJ, Berman SM, Dorian KJ, Hadgu A (1997). "Screening women for gonorrhea: demographic screening criteria for general clinical use". Am J Public Health. 87 (9): 1535–8. PMC 1380985. PMID 9314811.
- ↑ "2015 Sexually Transmitted Diseases Treatment Guidelines (CDC)".
- ↑ Workowski KA, Bolan GA. Sexually transmitted diseases treat- ment guidelines, 2015. MMWR Recomm Rep 2015;64:60–68.
- ↑ US preventive services task forces. Gonorrhea and chlamydia screening (2014) https://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/chlamydia-and-gonorrhea-screening Accessed on September 28, 2016
- ↑ McNeeley SG (1989). "Gonococcal infections in women". Obstet Gynecol Clin North Am. 16 (3): 467–78. PMID 2512520.
- ↑ Stansfield VA (1980). "Diagnosis and management of anorectal gonorrhoea in women". Br J Vener Dis. 56 (5): 319–21. PMC 1045815. PMID 7427703.
- ↑ 31.0 31.1 Sherrard J, Barlow D (1996). "Gonorrhoea in men: clinical and diagnostic aspects". Genitourin Med. 72 (6): 422–6. PMC 1195730. PMID 9038638.
- ↑ 32.0 32.1 Barlow D, Phillips I (1978). "Gonorrhoea in women. Diagnostic, clinical, and laboratory aspects". Lancet. 1 (8067): 761–4. PMID 76760.
- ↑ Osborne NG, Grubin L (1979). "Colonization of the pharynx with Neisseria gonorrhoeae: experience in a clinic for sexually transmitted diseases". Sex Transm Dis. 6 (4): 253–6. PMID 119330.
- ↑ STD Gonorrhea Infection Gallery http://www.std-gov.org/std_picture/gonorrhea_w.htm Accessed on September 22, 2016
- ↑ Centers for Disease Control and Prevention. Public Health Image Library (PHIL) http://phil.cdc.gov/phil/home.asp Accessed on September 22, 2016