Loeffler endocarditis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 24: | Line 24: | ||
It is named for Wilhelm Löffler.<ref>{{WhoNamedIt|synd|582}}</ref><ref>W. Löffler. Endocarditis parietalis fibroplastica mit Bluteosinophilie. Ein eigenartiges Krankheitsbild. Schweizerische medizinische Wochenschrift, Basel, 1936, 66: 817-820.</ref> | It is named for Wilhelm Löffler.<ref>{{WhoNamedIt|synd|582}}</ref><ref>W. Löffler. Endocarditis parietalis fibroplastica mit Bluteosinophilie. Ein eigenartiges Krankheitsbild. Schweizerische medizinische Wochenschrift, Basel, 1936, 66: 817-820.</ref> | ||
++++++ | |||
My references: | |||
general | |||
<ref name="pmid28890659">Alam A, Thampi S, Saba SG, Jermyn R (2017) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=28890659 Loeffler Endocarditis: A Unique Presentation of Right-Sided Heart Failure Due to Eosinophil-Induced Endomyocardial Fibrosis.] ''Clin Med Insights Case Rep'' 10 ():1179547617723643. [http://dx.doi.org/10.1177/1179547617723643 DOI:10.1177/1179547617723643] PMID: [https://pubmed.gov/28890659 28890659]</ref> | |||
<ref name="pmid28890659">Alam A, Thampi S, Saba SG, Jermyn R (2017) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=28890659 Loeffler Endocarditis: A Unique Presentation of Right-Sided Heart Failure Due to Eosinophil-Induced Endomyocardial Fibrosis.] ''Clin Med Insights Case Rep'' 10 ():1179547617723643. [http://dx.doi.org/10.1177/1179547617723643 DOI:10.1177/1179547617723643] PMID: [https://pubmed.gov/28890659 28890659]</ref> | |||
<ref name="pmid17573694">Benezet-Mazuecos J, de la Fuente A, Marcos-Alberca P, Farre J (2007) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=17573694 Loeffler endocarditis: what have we learned?] ''Am J Hematol'' 82 (10):861-2. [http://dx.doi.org/10.1002/ajh.20957 DOI:10.1002/ajh.20957] PMID: [https://pubmed.gov/17573694 17573694]</ref> | |||
<ref name="pmid29538200">Gao M, Zhang W, Zhao W, Qin L, Pei F, Zheng Y (2018) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=29538200 Loeffler endocarditis as a rare cause of heart failure with preserved ejection fraction: A case report and review of literature.] ''Medicine (Baltimore)'' 97 (11):e0079. [http://dx.doi.org/10.1097/MD.0000000000010079 DOI:10.1097/MD.0000000000010079] PMID: [https://pubmed.gov/29538200 29538200]</ref> | |||
<ref name="pmid30701721">Kalra DK, Park J, Hemu M, Goldberg A (2019) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=30701721 Loeffler Endocarditis: A Diagnosis Made with Cardiovascular Magnetic Resonance.] ''J Cardiovasc Imaging'' 27 (1):70-72. [http://dx.doi.org/10.4250/jcvi.2019.27.e5 DOI:10.4250/jcvi.2019.27.e5] PMID: [https://pubmed.gov/30701721 30701721]</ref> | |||
<ref name="pmid17534930">Chao BH, Cline-Parhamovich K, Grizzard JD, Smith TJ (2007) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=17534930 Fatal Loeffler's endocarditis due to hypereosinophilic syndrome.] ''Am J Hematol'' 82 (10):920-3. [http://dx.doi.org/10.1002/ajh.20933 DOI:10.1002/ajh.20933] PMID: [https://pubmed.gov/17534930 17534930]</ref> | |||
<ref name="pmid18480530">Sen T, Ponde CK, Udwadia ZF (2008) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18480530 Hypereosinophilic syndrome with isolated Loeffler's endocarditis: complete resolution with corticosteroids.] ''J Postgrad Med'' 54 (2):135-7. PMID: [https://pubmed.gov/18480530 18480530]</ref> | |||
<ref name="pmid27883350">Osovska NY, Kuzminova NV, Knyazkova II (2016) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=27883350 Loeffler endocarditis in young woman - a case report.] ''Pol Merkur Lekarski'' 41 (245):231-237. PMID: [https://pubmed.gov/27883350 27883350]</ref> | |||
<ref name="pmid23046536">Niemeijer ND, van Daele PL, Caliskan K, Oei FB, Loosveld OJ, van der Meer NJ (2012) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=23046536 Löffler endocarditis: a rare cause of acute cardiac failure.] ''J Cardiothorac Surg'' 7 ():109. [http://dx.doi.org/10.1186/1749-8090-7-109 DOI:10.1186/1749-8090-7-109] PMID: [https://pubmed.gov/23046536 23046536]</ref> | |||
adalimumab <ref name="pmid30788072">Hussain N, Patel P, Yin J, Davis R, Ikladios O (2019) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=30788072 A case of Loeffler's endocarditis after initiation of adalimumab.] ''J Community Hosp Intern Med Perspect'' 9 (1):29-32. [http://dx.doi.org/10.1080/20009666.2018.1562852 DOI:10.1080/20009666.2018.1562852] PMID: [https://pubmed.gov/30788072 30788072]</ref> | |||
3d echo: | |||
<ref name="pmid28600838">Hernandez CM, Arisha MJ, Ahmad A, Oates E, Nanda NC, Nanda A et al. (2017) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=28600838 Usefulness of three-dimensional echocardiography in the assessment of valvular involvement in Loeffler endocarditis.] ''Echocardiography'' 34 (7):1050-1056. [http://dx.doi.org/10.1111/echo.13575 DOI:10.1111/echo.13575] PMID: [https://pubmed.gov/28600838 28600838]</ref> | |||
Churg-Strauss | |||
<ref name="pmid20661332">Seo JS, Song JM, Kim DH, Kang DH, Song JK (2010) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=20661332 A Case of Loeffler's Endocarditis Associated with Churg-Strauss Syndrome.] ''J Cardiovasc Ultrasound'' 18 (1):21-4. [http://dx.doi.org/10.4250/jcu.2010.18.1.21 DOI:10.4250/jcu.2010.18.1.21] PMID: [https://pubmed.gov/20661332 20661332]</ref> | |||
Multiparametric cardiac magnetic resonance imaging (CMR) | |||
<ref name="pmid28284183">Gastl M, Behm P, Jacoby C, Kelm M, Bönner F (2017) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=28284183 Multiparametric cardiac magnetic resonance imaging (CMR) for the diagnosis of Loeffler's endocarditis: a case report.] ''BMC Cardiovasc Disord'' 17 (1):74. [http://dx.doi.org/10.1186/s12872-017-0492-7 DOI:10.1186/s12872-017-0492-7] PMID: [https://pubmed.gov/28284183 28284183]</ref> | |||
==Overview== | ==Overview== | ||
Revision as of 16:05, 14 June 2019
| Loeffler endocarditis | |
 | |
|---|---|
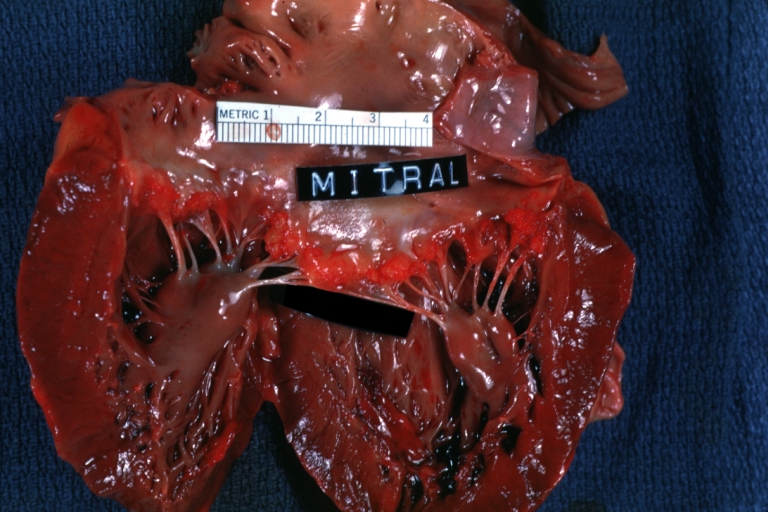
| HEART: An excellent example of Thrombotic Nonbacterial Endocarditis. Gross: Mitral valve Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | I42.3 |
| ICD-9 | 421.0 |
| DiseasesDB | 4291 |
| eMedicine | med/1318 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Soroush Seifirad, M.D.[2]
Loeffler endocarditis, a form of endocarditis, is one of the two forms of hypereosinophilic syndrome. It is a restricive cardiomyopathy characterized eosinophilia and eosinophilic penetration leading to the fibrotic thickening of portions of the heart (similar to that of endomyocardial fibrosis) and commonly has large mural thrombi. Commonly found in temperate climates.
Common symptoms include edema and breathlessness.
It is named for Wilhelm Löffler.[1][2]
++++++
My references:
general [3]
adalimumab [11]
3d echo: [12]
Churg-Strauss [13]
Multiparametric cardiac magnetic resonance imaging (CMR) [14]
Overview
Historical Perspective
[Disease name] was first discovered by [name of scientist], a [nationality + occupation], in [year]/during/following [event].
The association between [important risk factor/cause] and [disease name] was made in/during [year/event].
In [year], [scientist] was the first to discover the association between [risk factor] and the development of [disease name].
In [year], [gene] mutations were first implicated in the pathogenesis of [disease name].
There have been several outbreaks of [disease name], including -----.
In [year], [diagnostic test/therapy] was developed by [scientist] to treat/diagnose [disease name].
Classification
There is no established system for the classification of [disease name].
OR
[Disease name] may be classified according to [classification method] into [number] subtypes/groups: [group1], [group2], [group3], and [group4].
OR
[Disease name] may be classified into [large number > 6] subtypes based on [classification method 1], [classification method 2], and [classification method 3]. [Disease name] may be classified into several subtypes based on [classification method 1], [classification method 2], and [classification method 3].
OR
Based on the duration of symptoms, [disease name] may be classified as either acute or chronic.
OR
If the staging system involves specific and characteristic findings and features: According to the [staging system + reference], there are [number] stages of [malignancy name] based on the [finding1], [finding2], and [finding3]. Each stage is assigned a [letter/number1] and a [letter/number2] that designate the [feature1] and [feature2].
OR
The staging of [malignancy name] is based on the [staging system].
OR
There is no established system for the staging of [malignancy name].
Pathophysiology
The exact pathogenesis of [disease name] is not fully understood.
OR
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
OR
[Pathogen name] is usually transmitted via the [transmission route] route to the human host.
OR
Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
OR
[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
OR
The progression to [disease name] usually involves the [molecular pathway].
OR
The pathophysiology of [disease/malignancy] depends on the histological subtype.
Causes
Disease name] may be caused by [cause1], [cause2], or [cause3].
OR
Common causes of [disease] include [cause1], [cause2], and [cause3].
OR
The most common cause of [disease name] is [cause 1]. Less common causes of [disease name] include [cause 2], [cause 3], and [cause 4].
OR
The cause of [disease name] has not been identified. To review risk factors for the development of [disease name], click here.
Differentiating ((Page name)) from Other Diseases
[Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as [differential dx1], [differential dx2], and [differential dx3].
OR
[Disease name] must be differentiated from [[differential dx1], [differential dx2], and [differential dx3].
Epidemiology and Demographics
The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide.
OR
In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide.
OR
In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%.
Patients of all age groups may develop [disease name].
OR
The incidence of [disease name] increases with age; the median age at diagnosis is [#] years.
OR
[Disease name] commonly affects individuals younger than/older than [number of years] years of age.
OR
[Chronic disease name] is usually first diagnosed among [age group].
OR
[Acute disease name] commonly affects [age group].
There is no racial predilection to [disease name].
OR
[Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name].
[Disease name] affects men and women equally.
OR
[Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1.
The majority of [disease name] cases are reported in [geographical region].
OR
[Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2].
Risk Factors
There are no established risk factors for [disease name].
OR
The most potent risk factor in the development of [disease name] is [risk factor 1]. Other risk factors include [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] include [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] may be occupational, environmental, genetic, and viral.
Screening
There is insufficient evidence to recommend routine screening for [disease/malignancy].
OR
According to the [guideline name], screening for [disease name] is not recommended.
OR
According to the [guideline name], screening for [disease name] by [test 1] is recommended every [duration] among patients with [condition 1], [condition 2], and [condition 3].
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4].
OR
The diagnosis of [disease name] is based on the [criteria name] criteria, which include [criterion 1], [criterion 2], and [criterion 3].
OR
The diagnosis of [disease name] is based on the [definition name] definition, which includes [criterion 1], [criterion 2], and [criterion 3].
OR
There are no established criteria for the diagnosis of [disease name].
History and Symptoms
The majority of patients with [disease name] are asymptomatic.
OR
The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Template:WhoNamedIt
- ↑ W. Löffler. Endocarditis parietalis fibroplastica mit Bluteosinophilie. Ein eigenartiges Krankheitsbild. Schweizerische medizinische Wochenschrift, Basel, 1936, 66: 817-820.
- ↑ 3.0 3.1 Alam A, Thampi S, Saba SG, Jermyn R (2017) Loeffler Endocarditis: A Unique Presentation of Right-Sided Heart Failure Due to Eosinophil-Induced Endomyocardial Fibrosis. Clin Med Insights Case Rep 10 ():1179547617723643. DOI:10.1177/1179547617723643 PMID: 28890659
- ↑ Benezet-Mazuecos J, de la Fuente A, Marcos-Alberca P, Farre J (2007) Loeffler endocarditis: what have we learned? Am J Hematol 82 (10):861-2. DOI:10.1002/ajh.20957 PMID: 17573694
- ↑ Gao M, Zhang W, Zhao W, Qin L, Pei F, Zheng Y (2018) Loeffler endocarditis as a rare cause of heart failure with preserved ejection fraction: A case report and review of literature. Medicine (Baltimore) 97 (11):e0079. DOI:10.1097/MD.0000000000010079 PMID: 29538200
- ↑ Kalra DK, Park J, Hemu M, Goldberg A (2019) Loeffler Endocarditis: A Diagnosis Made with Cardiovascular Magnetic Resonance. J Cardiovasc Imaging 27 (1):70-72. DOI:10.4250/jcvi.2019.27.e5 PMID: 30701721
- ↑ Chao BH, Cline-Parhamovich K, Grizzard JD, Smith TJ (2007) Fatal Loeffler's endocarditis due to hypereosinophilic syndrome. Am J Hematol 82 (10):920-3. DOI:10.1002/ajh.20933 PMID: 17534930
- ↑ Sen T, Ponde CK, Udwadia ZF (2008) Hypereosinophilic syndrome with isolated Loeffler's endocarditis: complete resolution with corticosteroids. J Postgrad Med 54 (2):135-7. PMID: 18480530
- ↑ Osovska NY, Kuzminova NV, Knyazkova II (2016) Loeffler endocarditis in young woman - a case report. Pol Merkur Lekarski 41 (245):231-237. PMID: 27883350
- ↑ Niemeijer ND, van Daele PL, Caliskan K, Oei FB, Loosveld OJ, van der Meer NJ (2012) Löffler endocarditis: a rare cause of acute cardiac failure. J Cardiothorac Surg 7 ():109. DOI:10.1186/1749-8090-7-109 PMID: 23046536
- ↑ Hussain N, Patel P, Yin J, Davis R, Ikladios O (2019) A case of Loeffler's endocarditis after initiation of adalimumab. J Community Hosp Intern Med Perspect 9 (1):29-32. DOI:10.1080/20009666.2018.1562852 PMID: 30788072
- ↑ Hernandez CM, Arisha MJ, Ahmad A, Oates E, Nanda NC, Nanda A et al. (2017) Usefulness of three-dimensional echocardiography in the assessment of valvular involvement in Loeffler endocarditis. Echocardiography 34 (7):1050-1056. DOI:10.1111/echo.13575 PMID: 28600838
- ↑ Seo JS, Song JM, Kim DH, Kang DH, Song JK (2010) A Case of Loeffler's Endocarditis Associated with Churg-Strauss Syndrome. J Cardiovasc Ultrasound 18 (1):21-4. DOI:10.4250/jcu.2010.18.1.21 PMID: 20661332
- ↑ Gastl M, Behm P, Jacoby C, Kelm M, Bönner F (2017) Multiparametric cardiac magnetic resonance imaging (CMR) for the diagnosis of Loeffler's endocarditis: a case report. BMC Cardiovasc Disord 17 (1):74. DOI:10.1186/s12872-017-0492-7 PMID: 28284183