Minoxidil (oral)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gerald Chi
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNINGS
See full prescribing information for complete Boxed Warning.
* Minoxidil tablets contain the powerful antihypertensive agent, minoxidil, which may produce serious adverse effects. It can cause pericardial effusion, occasionally progressing to tamponade, and angina pectoris may be exacerbated. Minoxidil should be reserved for hypertensive patients who do not respond adequately to maximum therapeutic doses of a diuretic and two other antihypertensive agents.
|
Overview
Minoxidil (oral) is a vasodilator that is FDA approved for the treatment of hypertension that is symptomatic or associated with target organ damage and is not manageable with maximum therapeutic doses of diuretic plus two other antihypertensive drugs. There is a Black Box Warning for this drug as shown here. Common adverse reactions include hypotension, hirsutism, hypertrichosis, fluid retention, and hypernatremia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Refractory Hypertension Associated with End Organ Damage
- Dosing Information
- Initial Dosage
- 5 mg/day PO as single dose or 2 divided doses; adjust in 100% increments as required
- Maintenance Dosage
- 10-40 mg/day ORALLY daily in 1-2 divided doses; maximum 100 mg/day
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Minoxidil (oral) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Minoxidil (oral) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Refractory Hypertension Associated with End Organ Damage
- Dosing Information
- Dosage
- Initial Dosage
- 0.2 mg/kg/day PO in a single dose or as 2 divided doses; adjust as required up to 50 mg/day
- Maintenance Dosage
- 0.25-1 mg/kg/day PO in a single dose or as 2 divided daily doses; maximum 50 mg/day
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Minoxidil (oral) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Minoxidil (oral) in pediatric patients.
Contraindications
- Minoxidil tablets are contraindicated in pheochromocytoma, because it may stimulate secretion of catecholamines from the tumor through its antihypertensive action.
- Minoxidil tablets are contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation.
Warnings
|
WARNINGS
See full prescribing information for complete Boxed Warning.
* Minoxidil tablets contain the powerful antihypertensive agent, minoxidil, which may produce serious adverse effects. It can cause pericardial effusion, occasionally progressing to tamponade, and angina pectoris may be exacerbated. Minoxidil should be reserved for hypertensive patients who do not respond adequately to maximum therapeutic doses of a diuretic and two other antihypertensive agents.
|
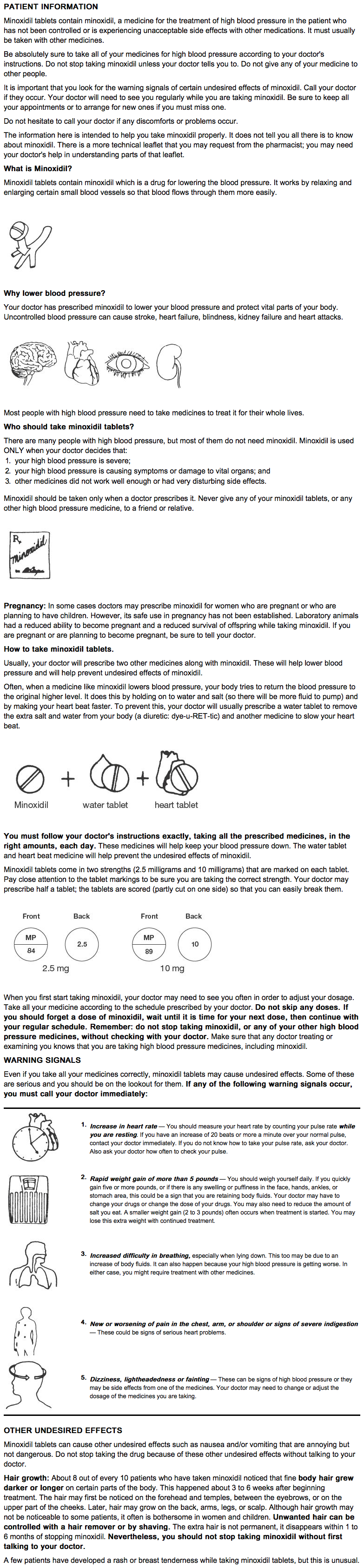
Salt and Water Retention
- Congestive Heart Failure — concomitant use of an adequate diuretic is required — Minoxidil tablets must usually be administered concomitantly with a diuretic adequate to prevent fluid retention and possible congestive heart failure; a high ceiling (loop) diuretic is almost always required. Body weight should be monitored closely. If minoxidil is used without a diuretic, retention of several hundred milliequivalents of salt and corresponding volumes of water can occur within a few days, leading to increased plasma and interstitial fluid volume and local or generalized edema. diuretic treatment alone, or in combination with restricted salt intake, will usually minimize fluid retention, although reversible edema did develop in approximately 10% of nondialysis patients so treated. Ascites has also been reported. diuretic effectiveness was limited mostly by disease-related impaired renal function. The condition of patients with pre-existing congestive heart failure occasionally deteriorated in association with fluid retention although because of the fall in blood pressure (reduction of afterload), more than twice as many improved than worsened. Rarely, refractory fluid retention may require discontinuation of minoxidil. Provided that the patient is under close medical supervision, it may be possible to resolve refractory salt retention by discontinuing minoxidil for 1 or 2 days and then resuming treatment in conjunction with vigorous diuretic therapy.
Concomitant Treatment to Prevent Tachycardia is Usually Required
- Minoxidil increases the heart rate. Angina may worsen or appear for the first time during minoxidil treatment, probably because of the increased oxygen demands associated with increased heart rate and cardiac output. The increase in rate and the occurrence of angina generally can be prevented by the concomitant administration of a beta-adrenergic blocking drug or other sympathetic nervous system suppressant. The ability of beta-adrenergic blocking agents to minimize papillary muscle lesions in animals is further reason to utilize such an agent concomitantly. Round-the-clock effectiveness of the sympathetic suppressant should be ensured.
Pericarditis, Pericardial Effusion and Tamponade
- There have been reports of pericarditis occurring in association with the use of minoxidil. The relationship of this association to renal status is uncertain. Pericardial effusion, occasionally with tamponade, has been observed in about 3% of treated patients not on dialysis, especially those with inadequate or compromised renal function. Although in many cases, the pericardial effusion was associated with a connective tissue disease, the uremic syndrome, congestive heart failure, or marked fluid retention, there have been instances in which these potential causes of effusion were not present. Patients should be observed closely for any suggestion of a pericardial disorder, and echocardiographic studies should be carried out if suspicion arises. More vigorous diuretic therapy, dialysis, pericardiocentesis, or surgery may be required. If the effusion persists, withdrawal of minoxidil should be considered in light of other means of controlling the hypertension and the patient's clinical status.
Interaction with Guanethidine
- Although minoxidil does not itself cause orthostatic hypotension, its administration to patients already receiving guanethidine can result in profound orthostatic effects. If at all possible, guanethidine should be discontinued well before minoxidil is begun. Where this is not possible, minoxidil therapy should be started in the hospital and the patient should remain institutionalized until severe orthostatic effects are no longer present or the patient has learned to avoid activities that provoke them.
Hazard of Rapid Control of Blood Pressure
- In patients with very severe blood pressure elevation, too rapid control of blood pressure, especially with intravenous agents, can precipitate syncope, cerebrovascular accidents, myocardial infarction and ischemia of special sense organs with resulting decrease or loss of vision or hearing. Patients with compromised circulation or cryoglobulinemia may also suffer ischemic episodes of the affected organs. Although such events have not been unequivocally associated with minoxidil use, total experience is limited at present.
- Any patient with malignant hypertension should have initial treatment with minoxidil carried out in a hospital setting, both to assure that blood pressure is falling and to assure that it is not falling more rapidly than intended.
Precautions
General Precautions
- Monitor fluid and electrolyte balance and body weight.
- Observe patients for signs and symptoms of pericardial effusion.
- Use after myocardial infarction
- Minoxidil tablets have not been used in patients who have had a myocardial infarction within the preceding month.
- It is possible that a reduction of arterial pressure with minoxidil might further limit blood flow to the myocardium, although this might be compensated by decreased oxygen demand because of lower blood pressure.
- Possible hypersensitivity to minoxidil, manifested as a skin rash, has been seen in less than 1% of patients; whether the drug should be discontinued when this occurs depends on treatment alternatives.
- Renal failure or dialysis patients may require smaller doses of minoxidil and should have close medical supervision to prevent exacerbation of renal failure or precipitation of cardiac failure.
Laboratory Tests
- Those laboratory tests which are abnormal at the time of initiation of minoxidil therapy, such as urinalysis, renal function tests, EKG, chest x-ray, echocardiogram, etc., should be repeated at intervals to ascertain whether improvement or deterioration is occurring under minoxidil therapy. Initially, such tests should be performed frequently, e.g., 1 to 3 month intervals; later as stabilization occurs, at intervals of 6 to 12 months.
Unapproved Use
- Use of minoxidil tablets, in any formulation, to promote hair growth is not an approved indication.
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Clinical Trial Experience of Minoxidil (oral) in the drug label.
Postmarketing Experience
- Salt and Water Retention
- Temporary edema developed in 7% of patients who were not edematous at the start of therapy.
- Dermatologic
- Hypertrichosis (elongation, thickening, and enhanced pigmentation of fine body hair)) is seen in about 80% of patients taking minoxidil tablets. This develops within 3 to 6 weeks after starting therapy. It is usually first noticed on the temples, between the eyebrows, between the hairline and the eyebrows, or in the side-burn area of the upper lateral cheek, later extending to the back, arms, legs, and scalp. Upon discontinuation of minoxidil, new hair growth stops, but 1 to 6 months may be required for restoration to pretreatment appearance. No endocrine abnormalities have been found to explain the abnormal hair growth; thus, it is hypertrichosis without virilism. Hair growth is especially disturbing to children and women and such patients should be thoroughly informed about this effect before therapy with minoxidil is begun.
- Allergic
- Rashes have been reported, including rare reports of bullous eruptions, and Stevens-Johnson syndrome.
- Hematologic
- Thrombocytopenia and leukopenia (WBC <3000/mm3) have rarely been reported.
- Gastrointestinal
- Miscellaneous
- Breast tenderness developed in less than 1% of patients.
- Altered Laboratory Findings
- ECG changes:
- Changes in direction and magnitude of the ECG T waves occur in approximately 60% of patients treated with minoxidil. In rare instances a large negative amplitude of the T wave may encroach upon the S-T segment, but the S-T segment is not independently altered. These changes usually disappear with continuance of treatment and revert to the pretreatment state if minoxidil is discontinued. No symptoms have been associated with these changes, nor have there been alterations in blood cell counts or in plasma enzyme concentrations that would suggest myocardial damage. Long-term treatment of patients manifesting such changes has provided no evidence of deteriorating cardiac function. At present the changes appear to be nonspecific and without identifiable clinical significance.
- Effects of hemodilution
- Hematocrit, hemoglobin, and erythrocyte count usually fall about 7% initially and then recover to pretreatment levels.
- Other
- Alkaline phosphatase increased varyingly without other evidence of liver or bone abnormality.
- Serum creatinine increased an average of 6% and BUN slightly more, but later declined to pretreatment levels.
Drug Interactions
- Although minoxidil does not itself cause orthostatic hypotension, its administration to patients already receiving guanethidine can result in profound orthostatic effects. If at all possible, guanethidine should be discontinued well before minoxidil is begun. Where this is not possible, minoxidil therapy should be started in the hospital and the patient should remain institutionalized until severe orthostatic effects are no longer present or the patient has learned to avoid activities that provoke them.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- Oral administration of minoxidil has been associated with evidence of increased fetal resorption in rabbits but not rats, when administered at five times the maximum recommended oral antihypertensive human dose. There was no evidence of teratogenic effects in rats and rabbits. Subcutaneous administration of minoxidil to pregnant rats at 80 mg/kg/day was maternally toxic but not teratogenic. Higher subcutaneous doses produced evidence of developmental toxicity. There are no adequate and well controlled studies in pregnant women. Minoxidil should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Minoxidil (oral) in women who are pregnant.
Labor and Delivery
- The effects on labor and delivery are unknown.
Nursing Mothers
- There has been one report of minoxidil excretion in the breast milk of a woman treated with 5 mg oral minoxidil twice daily for hypertension. Because of the potential for adverse effects in nursing infants from minoxidil absorption, minoxidil should not be administered to a nursing woman.
Pediatric Use
- Use in pediatric patients has been limited to date, particularly in infants. The recommendations can be considered only a rough guide at present and careful titration is essential.
Geriatic Use
- Clinical studies of minoxidil tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they responded differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Minoxidil (oral) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Minoxidil (oral) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Minoxidil (oral) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Minoxidil (oral) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Minoxidil (oral) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Minoxidil (oral) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Minoxidil (oral) in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Minoxidil (oral) in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- There have been only a few instances of deliberate or accidental overdosage with minoxidil tablets. One patient recovered after taking 50 mg of minoxidil together with 500 mg of a barbiturate. When exaggerated hypotension is encountered, it is most likely to occur in association with residual sympathetic nervous system blockade from previous therapy (guanethidine-like effects or alpha-adrenergic blockage), which prevents the usual compensatory maintenance of blood pressure. Intravenous administration of normal saline will help to maintain blood pressure and facilitate urine formation in these patients. Sympathomimetic drugs such as norepinephrine or epinephrine should be avoided because of their excessive cardiac stimulating action. Phenylephrine, angiotensin II, vasopressin, and dopamine all reverse hypotension due to minoxidil, but should only be used if underperfusion of a vital organ is evident.
- Radioimmunoassay can be performed to determine the concentration of minoxidil in the blood. At the maximum adult dose of 100 mg/day, peak blood levels of 1641 ng/mL and 2441 ng/mL were observed in two patients, respectively. Due to patient-to-patient variation in blood levels, it is difficult to establish an overdosage warning level. In general, a substantial increase above 2000 ng/mL should be regarded as overdosage, unless the physician is aware that the patient has taken no more than the maximum dose.
- Oral LD50 in rats has ranged from 1321 to 3492 mg/kg; in mice, 2456 to 2648 mg/kg.
Chronic Overdose
There is limited information regarding Chronic Overdose of Minoxidil (oral) in the drug label.
Pharmacology
| |

| |
Minoxidil (oral)
| |
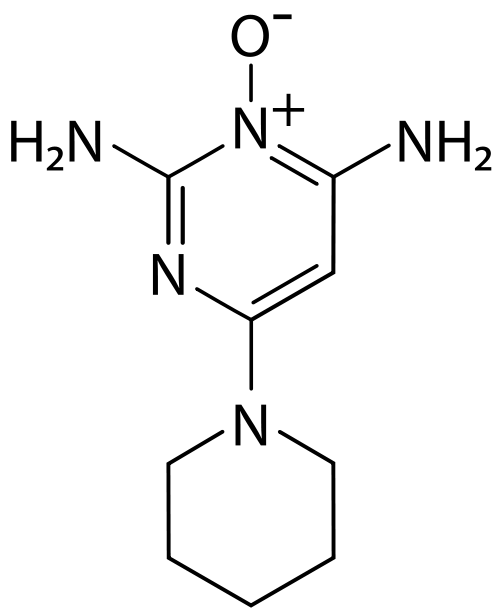
| Systematic (IUPAC) name | |
| 6-Piperidin-1-ylpyrimidine-2,4-diamine 3-oxide | |
| Identifiers | |
| CAS number | |
| ATC code | C02 D11AX01 (WHO) |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 209.251 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | Primarily hepatic |
| Half life | 4.2 hours |
| Excretion | renal |
| Therapeutic considerations | |
| Pregnancy cat. |
C |
| Legal status |
P(UK) for topical use, otherwise POM. Cannot be prescribed on the NHS. |
| Routes | Oral / topical |
Mechanism of Action
General Pharmacologic Properties
- Minoxidil is an orally effective direct acting peripheral vasodilator that reduces elevated systolic and diastolic blood pressure by decreasing peripheral vascular resistance. Microcirculatory blood flow in animals is enhanced or maintained in all systemic vascular beds. In man, forearm and renal vascular resistance decline; forearm blood flow increases while renal blood flow and glomerular filtration rate are preserved.
- Because it causes peripheral vasodilation, minoxidil elicits a number of predictable reactions. Reduction of peripheral arteriolar resistance and the associated fall in blood pressure trigger sympathetic, vagal inhibitory, and renal homeostatic mechanisms, including an increase in renin secretion, that lead to increased cardiac rate and output and salt and water retention. These adverse effects can usually be minimized by concomitant administration of a diuretic and a beta-adrenergic blocking agent or other sympathetic nervous system suppressant.
- Minoxidil does not interfere with vasomotor reflexes and therefore does not produce orthostatic hypotension. The drug does not enter the central nervous system in experimental animals in significant amounts, and it does not affect CNS function in man.
Effects on Blood Pressure and Target Organs
- The extent and time-course of blood pressure reduction by minoxidil do not correspond closely to its concentration in plasma. After an effective single oral dose, blood pressure usually starts to decline within one-half hour, reaches a minimum between 2 and 3 hours and recovers at an arithmetically linear rate of about 30%/day. The total duration of effect is approximately 75 hours. When minoxidil is administered chronically, once or twice a day, the time required to achieve maximum effect on blood pressure with a given daily dose is inversely related to the size of the dose. Thus, maximum effect is achieved on 10 mg/day within 7 days, on 20 mg/day within 5 days, and on 40 mg/day within 3 days.
- The blood pressure response to minoxidil is linearly related to the logarithm of the dose administered. The slope of this log-linear dose-response relationship is proportional to the extent of hypertension and approaches zero at a supine diastolic blood pressure of approximately 85 mmHg.
- When used in severely hypertensive patients resistant to other therapy, frequently with an accompanying diuretic and beta-blocker, minoxidil tablets usually decreased the blood pressure and reversed encephalopathy and retinopathy.
Structure
- Minoxidil tablets contain minoxidil, an antihypertensive peripheral vasodilator. Minoxidil occurs as a white to off-white, odorless, crystalline solid that is soluble in water to the extent of approximately 2 mg/mL, is readily soluble in propylene glycol or ethanol, and is almost insoluble in acetone, chloroform or ethyl acetate. The chemical name for minoxidil is 2,4-pyrimidinediamine, 6-(1-piperidinyl)-, 3-oxide.
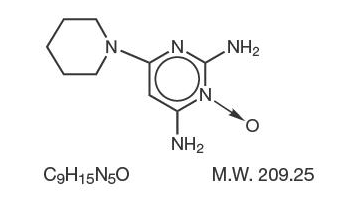
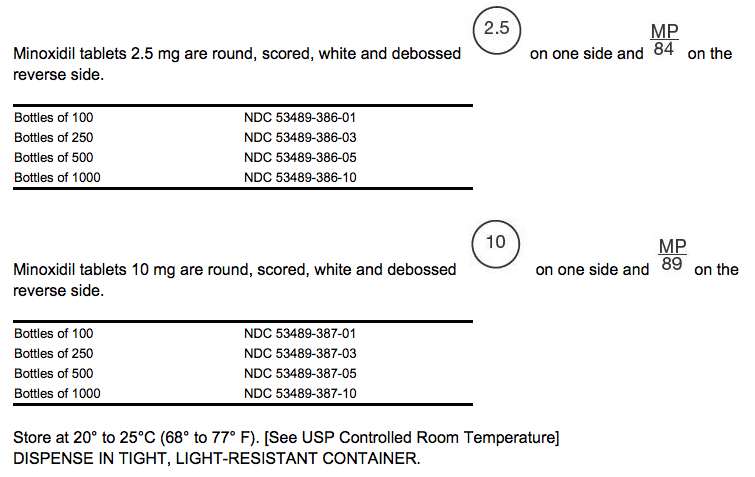
- Minoxidil tablets for oral administration contain either 2.5 mg or 10 mg of minoxidil. Inactive ingredients include colloidal silicon dioxide, corn starch, lactose anhydrous, magnesium stearate and microcrystalline cellulose.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Minoxidil (oral) in the drug label.
Pharmacokinetics
- Minoxidil is at least 90% absorbed from the GI tract in experimental animals and man. Plasma levels of the parent drug reach maximum within the first hour and decline rapidly thereafter. The average plasma half-life in man is 4.2 hours. Approximately 90% of the administered drug is metabolized, predominantly by conjugation with glucuronic acid at the N-oxide position in the pyrimidine ring, but also by conversion to more polar products. Known metabolites exert much less pharmacologic effect than minoxidil itself; all are excreted principally in the urine. Minoxidil does not bind to plasma proteins, and its renal clearance corresponds to the glomerular filtration rate. In the absence of functional renal tissue, minoxidil and its metabolites can be removed by hemodialysis.
Nonclinical Toxicology
Cardiac Lesions in Animals
- Minoxidil produces several cardiac lesions in animals. Some are characteristic of agents that cause tachycardia and diastolic hypotension (beta-agonists like isoproterenol, arterial dilators like hydralazine) while others are produced by a narrower range of agents with arterial dilating properties. The significance of these lesions for humans is not clear, as they have not been recognized in patients treated with oral minoxidil at systemically active doses, despite formal review of over 150 autopsies of treated patients.
- Papillary muscle/subendocardial necrosis
- The most characteristic lesion of minoxidil, seen in rat, dog, and minipig (but not monkeys) is focal necrosis of the papillary muscle and subendocardial areas of the left ventricle. These lesions appear rapidly, within a few days of treatment with doses of 0.5 mg to 10 mg/kg/day in the dog and minipig, and are not progressive, although they leave residual scars. They are similar to lesions produced by other peripheral arterial dilators, by theobromine, and by beta-adrenergic receptor agonists such as isoproterenol, epinephrine, and albuterol. The lesions are thought to reflect ischemia provoked by increased oxygen demand (tachycardia, increased cardiac output) and relative decrease in coronary flow (decreased diastolic pressure and decreased time in diastole) caused by the vasodilatory effects of these agents coupled with reflex or directly induced tachycardia.
- Hemorrhagic lesions
- After acute oral minoxidil treatment (0.5 mg to 10 mg/kg/day) in dogs and mini-pigs, hemorrhagic lesions are seen in many parts of the heart, mainly in the epicardium, endocardium, and walls of small coronary arteries and arterioles. In minipigs the lesions occur primarily in the left atrium while in dogs they are most prominent in the right atrium, frequently appearing as grossly visible hemorrhagic lesions. With exposure of 1 to 20 mg/kg/day in the dog for 30 days or longer, there is replacement of myocardial cells by proliferating fibroblasts and angioblasts, hemorrhage and hemosiderin accumulation. These lesions can be produced by topical minoxidil administration that gives systemic absorption of 0.5 to 1 mg/kg/day. Other peripheral dilators, including an experimental agent, nicorandil and theobromine have produced similar lesions.
- Epicarditis
- A less fully studied lesion is local epicarditis, seen in dogs after 2 days of oral minoxidil. More recently, chronic proliferative epicarditis was observed in dogs treated topically twice a day for 90 days. In a one year oral dog study, serosanguineous pericardial fluid was seen.
- Hypertrophy and Dilation
- Oral and topical studies in rats, dogs, monkeys (oral only), and rabbits (dermal only) show cardiac hypertrophy and dilation. This is presumed to represent the consequences of prolonged fluid overload; there is preliminary evidence in monkeys that diuretics partly reverse these effects.
- Autopsies of over 150 patients who died of various causes after receiving minoxidil for hypertension have not revealed the characteristic hemorrhagic (especially atrial) lesions seen in dogs and minipigs. While areas of papillary muscle and subendocardial necrosis were occasionally seen, they occurred in the presence of known pre-existing coronary artery disease and were also seen in patients never exposed to minoxidil in another series using similar, but not identical autopsy methods.
Carcinogenesis and Mutagenesis and Impairment of Fertility
- Two-year carcinogenicity studies of minoxidil have been conducted by the dermal and oral (dietary) routes of administration in mice and rats. There were no positive findings with the oral (dietary) route of administration in rats.
- In the two-year dermal study in mice, an increased incidence of mammary adenomas and adenocarcinomas in the females at all dose levels (8, 25 and 80 mg/kg/day) was attributed to increased prolactin activity. Hyperprolactinemia is a well-known mechanism in the enhancement of mouse mammary tumors, but has not been associated with mammary tumorigenesis in women. Additionally, topical minoxidil has not been shown to cause hyperprolactinemia in women on clinical trials. Absorption of minoxidil through rodent skin is greater than would be experienced by patients treated topically with minoxidil for hair loss. Dietary administration of minoxidil to mice for up to 2 years was associated with an increased incidence of malignant lymphomas in females at all dose levels (10, 25 and 63 mg/kg/day) and an increased incidence of hepatic nodules in males (63 mg/kg/day). There was no effect of dietary minoxidil on the incidence of malignant liver tumors.
- In the two-year dermal study in rats there were significant increases in incidence of pheochromocytomas in males and females and preputial gland adenomas in males. Changes in incidence of neoplasms found to be increased in the dermal or oral carcinogenicity studies were typical of those expected in rodents treated with other hypotensive agents (adrenal pheochromocytomas in rats), treatment-related hormonal alterations (mammary carcinomas in female mice; preputial gland adenomas in male rats) or representative of normal variations within the range of historical incidence for rodent neoplasms (malignant lymphomas, liver nodules/adenomas in mice). Based on differences in absorption of minoxidil and mechanisms of tumorigenesis in these rodent species, none of these changes were considered to be relevant to the safety of patients treated topically with minoxidil for hair loss.
- There was no evidence of epithelial hyperplasia or tumorigenesis at the sites of topical application of minoxidil in either species in the 2-year dermal carcinogenesis studies. No evidence of carcinogenicity was detected in rats or rabbits treated topically with minoxidil for one year. Topical minoxidil (2% and 5%) did not significantly (p<0.05) reduce the latency period of UV light-initiated skin tumors in hairless mice, as compared to controls, in a 12-month photocarcinogenicity study.
- Minoxidil was not mutagenic in the Salmonella (Ames) test, the DNA damage alkaline elution assay, the in vitro rat hepatocyte unscheduled DNA synthesis (UDS) assay, the rat bone marrow micronucleus assay, or the mouse bone marrow micronucleus assay. An equivocal result was recorded in an in vitro cytogenetic assay using Chinese hamster cells at long exposure times, but a similar assay using human lymphocytes was negative.
- In a study in which male and female rats received one to five times the maximum recommended human oral antihypertensive dose of minoxidil (multiples based on a 50 kg patient) there was a dose-dependent reduction in conception rate.
Clinical Studies
There is limited information regarding Clinical Studies of Minoxidil (oral) in the drug label.
How Supplied
Storage
There is limited information regarding Minoxidil (oral) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Minoxidil (oral) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Minoxidil (oral) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- The patient should be fully aware of the importance of continuing all of his antihypertensive medications and of the nature of symptoms that would suggest fluid overload. The patient brochure below has been prepared and is included with each minoxidil package.
Precautions with Alcohol
- Alcohol-Minoxidil (oral) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.[1]
Brand Names
- Loniten®
Look-Alike Drug Names
- Loniten® — Lipitor®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "MINOXIDIL tablet [American Health Packaging]". line feed character in
|title=at position 18 (help) - ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Minoxidil (oral)
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Minoxidil (oral) |Label Name=Minoxidil04.png
}}
{{#subobject:
|Label Page=Minoxidil (oral) |Label Name=Minoxidil05.png
}}
{{#subobject:
|Label Page=Minoxidil (oral) |Label Name=Minoxidil06.png
}}