Leopard syndrome history and symptoms
|
Leopard syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Leopard syndrome history and symptoms On the Web |
|
American Roentgen Ray Society Images of Leopard syndrome history and symptoms |
|
Risk calculators and risk factors for Leopard syndrome history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]
Overview
LEOPARD syndrome affects many areas in the body. The characteristic feature associated with the condition is brown skin spots called lentigines. Patients are showing a wide spectrum of features include multiple lentigines, facial dysmorphisms, cardiac anomalies, electrocardiographic (ECG) conduction abnormalities, retardation of growth, abnormal genitalia and sensorineural deafness.[1]
History and Symptoms
The condition is characterized by some of the following conditions.
- Reddish-brown to dark brown macules (surface skin lesion) generally occurring in a high number over a large portion of the skin, have irregular borders and range in size from 1 mm in diameter to café-au-lait spot's, several centimetres in diameter, at times higher than 80% coverage, dispersed mostly on the face, neck, and upper part of the trunk, but sparing the mucosae. In general, lentigines appear at 4–5 years and increase into the thousands until puberty, independently from sun exposure. Also, some areas of vitiligo-like hypopigmentation may be observed.[2]
- Birth weight and length
- Weight is normal or above the average in one third of the newborns.[2] Patients show retardation of growth, with 25% of cases below the 3rd percentile in height and 85% of adults below the 25th percentile.[3]
- Electrocardiographic conduction abnormalities
- Observed conduction abnormalities like axis deviation, prolonged PR intervals, and right bundle branch block, ST-segment abnormalities, and T-wave inversion.[4]
- Wideset eyes, which lead to a similar facial resemblance between patients. Facial abnormalities are the second highest occurring symptom after the lentigines. Abnormalities also include: broad nasal root, prognathism (protruding lower jaw), or low-set, possibly rotated ears.
- Skeletal anomalies
- Including broad chest, pectus carinatum or excavatum are found in up to 75% of the newborns.[2]
- Narrowing of the pulmonary artery as it exits the heart. Other cardiac abnormalities may be present, including aortic stenosis, or mitral valve prolapse.
- Abnormal genitalia
- Usually cryptorchidism (retention of testicles in body) or monorchism (single testicle). In female patients, this presents as missing or single ovaries, much harder by nature to detect. Ultrasound imaging is performed at regular intervals, from the age of 1 year, to determine if ovaries are present.[2] [3]
- Slow, or stunted growth. Most newborns with this syndrome are of normal birth weight and length, but will often slow within the first year.
- Occurs in about 15–25% of patients, most cases are diagnosed at birth or during childhood, but deafness may develop also later in life.[5] [6]
- Additional dermatologic abnormalities (axillary freckling, café-au-lait spot's, localized hypopigmentation, dermatoglyphic abnormalities, interdigital webs, onychodystrophy, multiple granular cell myoblastomas, hyperelasticity)
- Mild mental retardation
- Observed in about 30% of those affected with the syndrome, Hypotonia is common in the newborn and can result in delayed psychomotor development.[2]
- Nystagmus (involuntary eye movements), seizures, or hyposmia (reduced ability to smell) has been documented in a few patients
- In 2004, a patient was reported with recurrent upper extremity aneurysms that required surgical repairs.[7]
- In 2006, a LEOPARD syndrome patient was reported with acute myelogenous leukemia.[8]
Unfortunately, due to the rarity of the syndrome itself, it is hard to determine whether certain additional diseases are actually a threat of the syndrome. With a base population of possibly less than one thousand individuals, one or two outlying cases can skew the statistical population very quickly.
Diagnostic Criteria
A clinical diagnosis is considered made when, with lentigines present there are 2 other symptoms observed, such as EKG abnormalities and ocular hypertelorism, or without lentigines, 3 of the above conditions are present, with a first-degree relative (i.e. parent, child, sibling) with a clinical diagnosis.[9]
Review of the clinical characteristics of patients with LEOPARD syndrome confirmed by molecular study during the first year of life demonstrates that the diagnosis in the first months of age can be clinically suspected in patients presenting with three main features, that is, characteristic facial features (100%), hypertrophic cardiomyopathy (HCM) (87%), and cafe-au-lait spots (75%).[2]
-
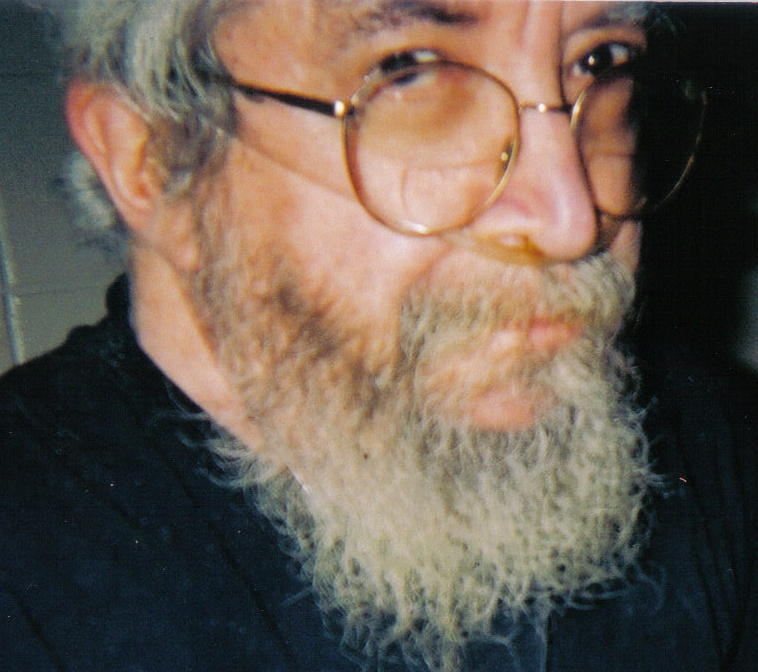
Three-quarter facial view, first generation patient showing slight prognathism and low set ears.
-
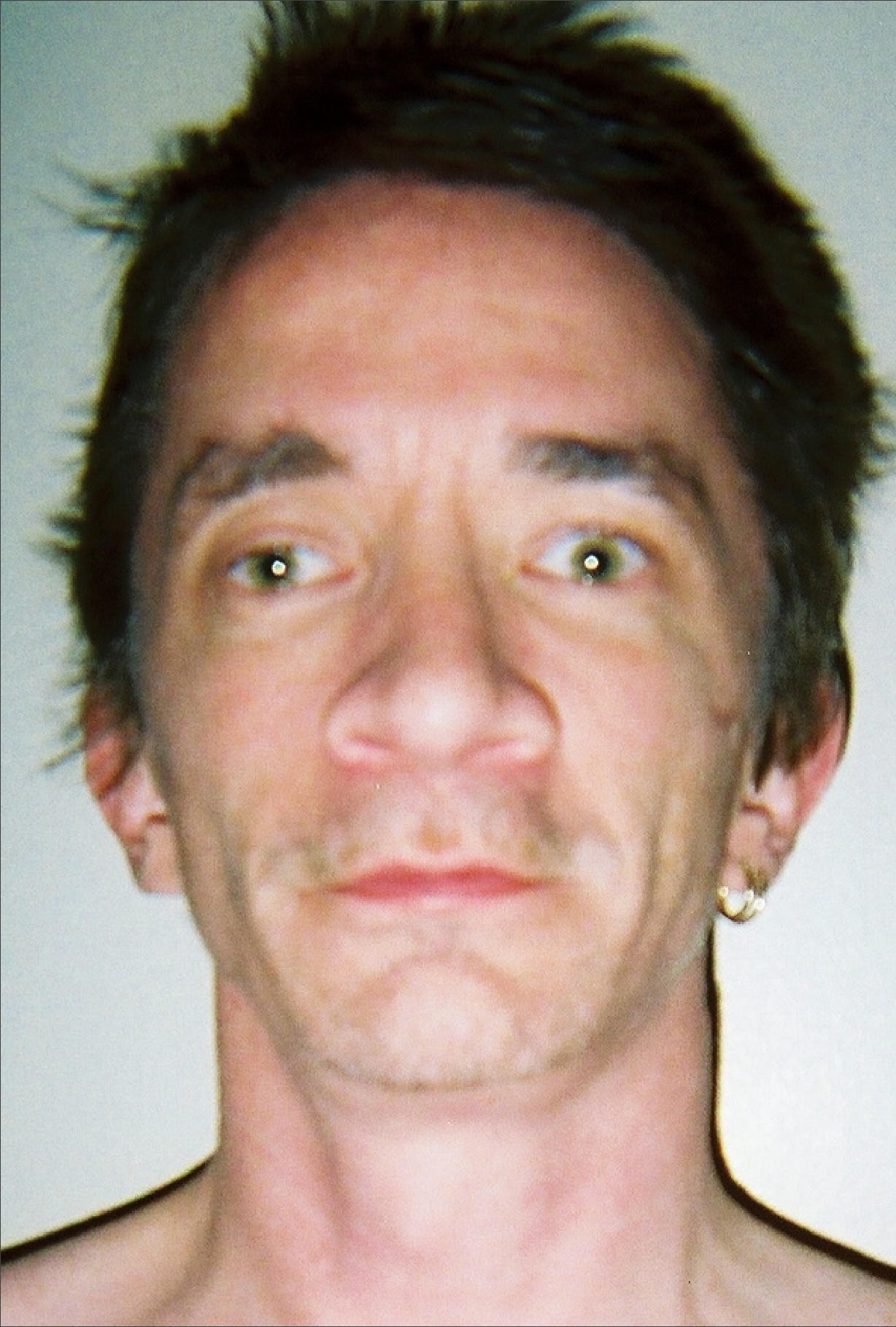
Thirty seven year old, second generation patient, exhibiting hypertelorism, broad nasal root, slight ptosis
-
Hand of thirty seven year old patient showing interdigital webbing
-
Thirty seven year old patient demonstrating hyperelasticity
-
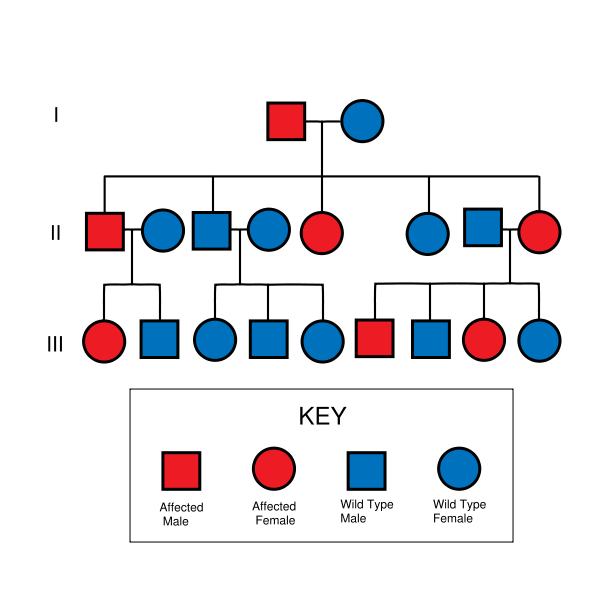
LEOPARD syndrome is inherited in an autosomal dominant fashion, although it can also arise due to spontaneous mutation.
-
21 month old, third generation patient, confirmed by genetic tests as Y279C, exhibiting ocular hyperteliorism, cephalofacial similarity.
-
Torso of thirty seven year old, second generation patient, exhibiting lentiginosis.
Referene
- ↑ Gorlin RJ, Anderson RC, Blaw M (1969). "Multiple lentigenes syndrome". Am J Dis Child. 117 (6): 652–62. PMID 5771505.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Digilio MC, Sarkozy A, de Zorzi A, Pacileo G, Limongelli G, Mingarelli R; et al. (2006). "LEOPARD syndrome: clinical diagnosis in the first year of life". Am J Med Genet A. 140 (7): 740–6. doi:10.1002/ajmg.a.31156. PMID 16523510.
- ↑ 3.0 3.1 Voron DA, Hatfield HH, Kalkhoff RK (1976). "Multiple lentigines syndrome. Case report and review of the literature". Am J Med. 60 (3): 447–56. PMID 1258892.
- ↑ Kim J, Kim MR, Kim HJ, Lee KA, Lee MG (2011). "LEOPARD Syndrome with PTPN11 Gene Mutation Showing Six Cardinal Symptoms of LEOPARD". Ann Dermatol. 23 (2): 232–5. doi:10.5021/ad.2011.23.2.232. PMC 3130872. PMID 21747628.
- ↑ Sarkozy A, Conti E, Digilio MC, Marino B, Morini E, Pacileo G; et al. (2004). "Clinical and molecular analysis of 30 patients with multiple lentigines LEOPARD syndrome". J Med Genet. 41 (5): e68. PMC 1735759. PMID 15121796.
- ↑ Coppin BD, Temple IK (1997). "Multiple lentigines syndrome (LEOPARD syndrome or progressive cardiomyopathic lentiginosis)". J Med Genet. 34 (7): 582–6. PMC 1051000. PMID 9222968.
- ↑ Yagubyan M, Panneton JM, Lindor NM, Conti E, Sarkozy A, Pizzuti A (2004). "LEOPARD syndrome: a new polyaneurysm association and an update on the molecular genetics of the disease". J. Vasc. Surg. 39 (4): 897–900. doi:10.1016/j.jvs.2003.11.030. PMID 15071461. Unknown parameter
|month=ignored (help) - ↑ Uçar C, Calýskan U, Martini S, Heinritz W (2006). "Acute myelomonocytic leukemia in a boy with LEOPARD syndrome (PTPN11 gene mutation positive)". J. Pediatr. Hematol. Oncol. 28 (3): 123–5. doi:10.1097/01.mph.0000199590.21797.0b. PMID 16679933. Unknown parameter
|month=ignored (help) - ↑ Voron DA, Hatfield HH, Kalkhoff RK (1976). "Multiple lentigines syndrome. Case report and review of the literature". Am. J. Med. 60 (3): 447–56. PMID 1258892.