Prognathism
| Prognathism | |
 | |
|---|---|
| ICD-10 | K07.1 |
| ICD-9 | 524.10 |
| DiseasesDB | 29354 |
| MeSH | D011378 |
|
WikiDoc Resources for Prognathism |
|
Articles |
|---|
|
Most recent articles on Prognathism Most cited articles on Prognathism |
|
Media |
|
Powerpoint slides on Prognathism |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Prognathism at Clinical Trials.gov Clinical Trials on Prognathism at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Prognathism
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Prognathism Discussion groups on Prognathism Patient Handouts on Prognathism Directions to Hospitals Treating Prognathism Risk calculators and risk factors for Prognathism
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Prognathism |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor in Chief: Berna Zorkun DMD [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
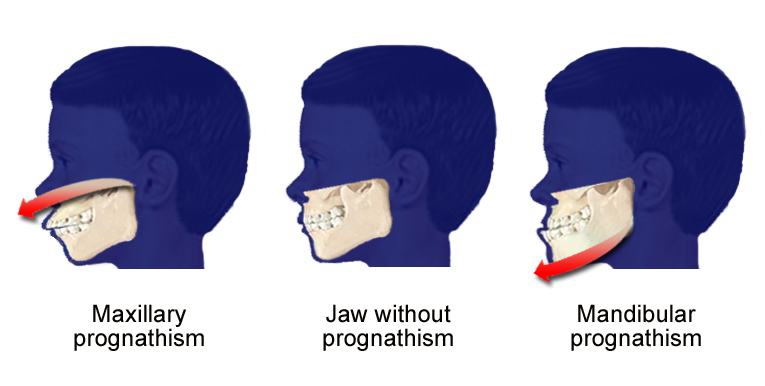
Prognathism is a term used to describe the positional relationship of the mandible and/or maxilla to the skeletal base where either of the jaws protrudes beyond a predetermined imaginary line in the sagittal plane of the skull. In dentistry, oral and maxillofacial surgery and orthodontics this is assessed clinically or radiographically (cephalometrics).
Etymology
The word prognathism derives from Greek pro (forward) and gnathos (jaw).
Presentation
Clinical determinants include soft tissue analysis where the clinician assesses nasolabial angle the relationship of the soft tissue portion of the chin to the nose and the relationship between the upper and lower lips; also used is dental arch relationship assessment such as Angle's classification.
Cephalometric analysis is the most accurate way of determining all types of prognathism as it includes assessments of skeletal base, occlusal plane angulation, facial height, soft tissue assessment and anterior dental angulation. Various calculations and assessments of the information in a cephalometric radiograph allow the clinician to objectively determine dental and skeletal relationships and determine a treatment plan.
Maxillary prognathism is a protrusion of the maxilla, and is also a common feature of many populations. It is not to be confused with micrognathism, although combinations of both may be found. It affects the middle third of the face, causing it to jut out, thereby increasing the facial area. Mandibular prognathism is a protrusion of the mandible, affecting the lower third of the face. Alveolar prognathism is a protrusion of that portion of the maxilla where the teeth are located, in the dental lining of the upper jaw. Prognathism can also be used to describe ways that the maxillary and mandibular dental arches can relate to one another. When there is maxillary and/or alveolar prognathism which causes an alignment of the maxillary incisors significantly anterior to the lower teeth, the condition is called an overbite. When the reverse is the case, and the lower jaw extends forward beyond the upper, the condition is referred to as an underbite.
The vast majority of prognathism in humans is due to normal variation among phenotypes. In human populations where prognathism is not the norm, it may be a malformation, the result of injury, a disease state or a hereditary condition.[1] Prognathism is only a disease if it affects mastication, speech or social function as a byproduct of severely affected aesthetics of the face.
Classification
Alveolar prognathism
Harmful habits, such as thumb sucking or tongue thrusting can result in or exaggerate an alveolar prognathism, causing teeth to misalign. Functional appliances can be used in growing children to help modify bad habits and neuro-muscular function, with the aim of correcting this condition.
Alveolar prognathism can be easily corrected also with fixed orthodontic therapy. However, relapse is quite common, unless the cause is removed or a long term retention is used.
Not all alveolar prognathism is anomalous, and significant differences can be observed among different ethnic groups.[2]
Maxillary Prognathism
In disease states, maxillary prognathism is associated with de Lange Syndrome[3]; however so-called false maxillary prognathism, where there is a lack of growth of the mandible, is by far a more common condition.
Prognathism, if not extremely severe, can be treated in growing patients with orthodontic functional or orthopaedic appliances. In adult patients this condition can be corrected by means of a combined surgical/orthodontic treatment, where most of the time a mandibular advancement is performed. The same can be said for mandibular prognathism.
Mandibular prognathism (progenism)
Pathologic mandibular prognathism is a potentially disfiguring, genetic disorder where the lower jaw outgrows the upper, resulting in an extended chin.
The condition colloquially is known as Habsburg jaw, Habsburg lip or Austrian Lip (see Habsburg) due to its prevalence in that bloodline.[4] The trait is easily traceable in portraits of Habsburg family members.[5] This has provided tools for people interested in studying genetics and pedigree analysis. Most instances are considered polygenetic.[6]
It is alleged to have been derived through a female from the princely Polish family of Piasts, its Masovian branch. The deformation of lips is clearly visible on tomb sculptures of Mazovian Piasts in Warsaw. However this may be, there exists evidence that the trait is longstanding. It is perhaps first observed in Maximilian I (1459-1519).
Traits such as these that were common to royal families are believed to have been passed on and exaggerated over time through royal intermarriage which caused acute inbreeding. Due to the large amount of politically motivated intermarriage among Habsburgs, the dynasty was virtually unparalleled in the degree of its inbreeding. Charles II of Spain is said to have had the most pronounced case of the Habsburg jaw on record. His jaw was so deformed that he was unable to chew.
Many dog breeds have underbite, particularly those with short faces. This may be, as in the case of bulldogs, to a slower growing maxilla in relation to the mandible.
Treatment
The most common treatment for mandibular prognathism is a combination of orthodontics and surgery. The orthodontics can involve braces, removal of teeth, or a bite splint.
Image Gallery
-
10-year-old boy with false maxillary prognathism
-
Alveolar prognathism, caused by thumb sucking and tongue thrusting in a 7 yr old girl.
-
Example of prognathism, where teeth have almost reached their final, straight position by braces. This makes the prognatism more obvious, and it will take a surgery, moving the jaw backwards, to give the ultimate result.
See also
For prognathism as a metric in forensics and ethnic anthropology see
- Craniofacial anthropometry
- Forensics
References
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/003026.htm
- ↑ Vioarsdóttir US, O'Higgins P, Stringer C (2002). "A geometric morphometric study of regional differences in the ontogeny of the modern human facial skeleton". J. Anat. 201 (3): 211–29. PMID 12363273.
- ↑ http://www.medterms.com/script/main/art.asp?articlekey=13301
- ↑ "OMIM - PROGNATHISM, MANDIBULAR". Retrieved 2007-10-31.
- ↑ Chudley AE (1998). "Genetic landmarks through philately--the Habsburg jaw". Clin. Genet. 54 (4): 283–4. PMID 9831338.
- ↑ Wolff G, Wienker TF, Sander H (1993). "On the genetics of mandibular prognathism: analysis of large European noble families". J. Med. Genet. 30 (2): 112–6. PMID 8445614.


