Irinotecan hydrochloride (Onivyde)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
SEVERE NEUTROPENIA AND SEVERE DIARRHEA
See full prescribing information for complete Boxed Warning.
Fatal neutropenic sepsis occurred in 0.8% of patients receiving Irinotecan. Severe or life-threatening neutropenic fever or sepsis occurred in 3% and severe or life-threatening neutropenia occurred in 20% of patients receiving Irinotecan in combination with fluorouracil and leucovorin. Withhold Irinotecan for absolute neutrophil count below 1500/mm3 or neutropenic fever. Monitor blood cell counts periodically during treatment.
Severe diarrhea occurred in 13% of patients receiving Irinotecan in combination with fluorouracil and leucovorin. Do not administer Irinotecan to patients with bowel obstruction. Withhold Irinotecan for diarrhea of Grade 2-4 severity. Administer loperamide for late diarrhea of any severity. Administer atropine, if not contraindicated, for early diarrhea of any severity.
|
Overview
Irinotecan hydrochloride (Onivyde) is a topoisomerase inhibitor that is FDA approved for the treatment of patients with metastatic adenocarcinoma of the pancreas (in combination with fluorouracil and leucovorin) after disease progression following gemcitabine-based therapy.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include diarrhea, fatigue/asthenia, vomiting, nausea, decreased appetite, stomatitis, and pyrexia (≥ 20%)..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Irinotecan hydrochloride is indicated, in combination with fluorouracil and leucovorin, for the treatment of patients with metastatic adenocarcinoma of the pancreas after disease progression following gemcitabine-based therapy.
Limitation of Use: Irinotecan hydrochloride is not indicated as a single agent for the treatment of patients with metastatic adenocarcinoma of the pancreas.
Dosage
- Important Use Information
DO NOT SUBSTITUTE this drug for other drugs containing irinotecan HCl.
- Recommended Dose
Administer Irinotecan hydrochloride prior to leucovorin and fluorouracil.
- The recommended dose of Irinotecan is 70 mg/m 2 administered by intravenous infusion over 90 minutes every 2 weeks.
- The recommended starting dose of Irinotecan in patients known to be homozygous for the UGT1A1*28 allele is 50 mg/m2 administered by intravenous infusion over 90 minutes. Increase the dose of Irinotecan to 70 mg/m 2 as tolerated in subsequent cycles.
- There is no recommended dose of Irinotecan for patients with serum bilirubin above the upper limit of normal.
- Premedication: Administer a corticosteroid and an anti-emetic 30 minutes prior to Irinotecan infusion.
- Dose Modifications for Adverse Reactions
- Table 1: Recommended Dose Modifications for Irinotecan hydrochloride

ONIVYDE: Irinotecan hydrochloride's Brand name
For recommended dose modifications of fluorouracil (5-FU) or leucovorin (LV), refer to the Full Prescribing Information; refer to Clinical Studies.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- Carcinoma of cervix[1]
- Carcinoma of esophagus[2]
- Extensive stage small cell lung cancer, First-line treatment, in combination with carboplatin[3][4]
- Extensive stage small cell lung cancer, First-line treatment, in combination with cisplatin[5][6]
- Gastric cancer[7][8][9]
- Liver carcinoma[10]
- Malignant glioma of brain, Recurrent or progressive disease[11][12][13][14][15]
- Metastatic breast cancer, Refractory[16][17]
- Non-Hodgkin's lymphoma[18]
- Non-small cell lung cancer[19][20][21][22]
- Ovarian cancer, Platinum-refractory or platinum-resistant[23][24][25]
- Rhabdomyosarcoma, Single-agent therapy[26][27]
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Irinotecan hydrochloride in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness of Irinotecan hydrochloride have not been established in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Irinotecan hydrochloride in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Irinotecan hydrochloride in pediatric patients.
Contraindications
Irinotecan hydrochloride is contraindicated in patients who have experienced a severe hypersensitivity reaction to this drug or irinotecan HCl.
Warnings
|
SEVERE NEUTROPENIA AND SEVERE DIARRHEA
See full prescribing information for complete Boxed Warning.
Fatal neutropenic sepsis occurred in 0.8% of patients receiving Irinotecan. Severe or life-threatening neutropenic fever or sepsis occurred in 3% and severe or life-threatening neutropenia occurred in 20% of patients receiving Irinotecan in combination with fluorouracil and leucovorin. Withhold Irinotecan for absolute neutrophil count below 1500/mm3 or neutropenic fever. Monitor blood cell counts periodically during treatment.
Severe diarrhea occurred in 13% of patients receiving Irinotecan in combination with fluorouracil and leucovorin. Do not administer Irinotecan to patients with bowel obstruction. Withhold Irinotecan for diarrhea of Grade 2-4 severity. Administer loperamide for late diarrhea of any severity. Administer atropine, if not contraindicated, for early diarrhea of any severity.
|
Severe Neutropenia
Irinotecan can cause severe or life-threatening neutropenia and fatal neutropenic sepsis. In Study 1, the incidence of fatal neutropenic sepsis was 0.8% among patients receiving Irinotecan, occurring in one of 117 patients in the Irinotecan plus fluorouracil/leucovorin (Irinotecan/5-FU/LV) arm and one of 147 patients receiving Irinotecan as a single agent. Severe or life-threatening neutropenia occurred in 20% of patients receiving Irinotecan/5-FU/LV compared to 2% of patients receiving fluorouracil/leucovorin alone (5-FU/LV). Grade 3 or 4 neutropenic fever/neutropenic sepsis occurred in 3% of patients receiving Irinotecan/5-FU/LV, and did not occur in patients receiving 5-FU/LV.
In patients receiving Irinotecan/5-FU/LV, the incidence of Grade 3 or 4 neutropenia was higher among Asian patients [18 of 33 (55%)] compared to White patients [13 of 73 (18%)]. Neutropenic fever/neutropenic sepsis was reported in 6% of Asian patients compared to 1% of White patients.
Monitor complete blood cell counts on Days 1 and 8 of every cycle and more frequently if clinically indicated. Withhold Irinotecan if the absolute neutrophil count (ANC) is below 1500/mm 3 or if neutropenic fever occurs. Resume Irinotecan when the ANC is 1500/mm 3 or above. Reduce Irinotecan dose for Grade 3-4 neutropenia or neutropenic fever following recovery in subsequent cycles.
Severe Diarrhea
Irinotecan can cause severe and life-threatening diarrhea. Do not administer Irinotecan to patients with bowel obstruction.
Severe or life-threatening diarrhea followed one of two patterns: late onset diarrhea (onset more than 24 hours following chemotherapy) and early onset diarrhea (onset within 24 hours of chemotherapy, sometimes occurring with other symptoms of cholinergic reaction). An individual patient may experience both early and late-onset diarrhea.
In Study 1, Grade 3 or 4 diarrhea occurred in 13% receiving Irinotecan/5-FU/LV compared to 4% receiving 5-FU/LV. The incidence of Grade 3 or 4 late onset diarrhea was 9% in patients receiving Irinotecan/5-FU/LV, compared to 4% in patients receiving 5-FU/LV. The incidence of Grade 3 or 4 early onset diarrhea was 3% in patients receiving Irinotecan/5-FU/LV, compared to no Grade 3 or 4 early onset diarrhea in patients receiving 5-FU/LV. Of patients receiving Irinotecan/5-FU/LV in Study 1, 34% received loperamide for late-onset diarrhea and 26% received atropine for early-onset diarrhea. Withhold Irinotecan for Grade 2-4 diarrhea. Initiate loperamide for late onset diarrhea of any severity. Administer intravenous or subcutaneous atropine 0.25 to 1 mg (unless clinically contraindicated) for early onset diarrhea of any severity. Following recovery to Grade 1 diarrhea, resume Irinotecan at a reduced dose.
Interstitial Lung Disease
Irinotecan HCl can cause severe and fatal interstitial lung disease (ILD). Withhold Irinotecan in patients with new or progressive dyspnea, cough, and fever, pending diagnostic evaluation. Discontinue Irinotecan in patients with a confirmed diagnosis of ILD.
Severe Hypersensitivity Reaction
Irinotecan HCl can cause severe hypersensitivity reactions, including anaphylactic reactions. Permanently discontinue Irinotecan in patients who experience a severe hypersensitivity reaction.
Embryo-Fetal Toxicity
Based on animal data with irinotecan HCl and the mechanism of action of Irinotecan, Irinotecan can cause fetal harm when administered to a pregnant woman. Embryotoxicity and teratogenicity were observed following treatment with irinotecan HCl, at doses resulting in irinotecan exposures lower than those achieved with Irinotecan 70 mg/m 2 in humans, administered to pregnant rats and rabbits during organogenesis. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with Irinotecan and for one month following the final dose.
Adverse Reactions
Clinical Trials Experience
The following adverse drug reactions are discussed in greater detail in other sections of the label:
- Severe Neutropenia
- Severe Diarrhea
- Interstitial Lung Disease
- Severe Hypersensitivity Reactions
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of Irinotecan cannot be directly compared to rates in clinical trials of other drugs and may not reflect the rates observed in practice.
The safety data described below are derived from patients with metastatic adenocarcinoma of the pancreas previously treated with gemcitabine-based therapy who received any part of protocol-specified therapy in Study 1, an international, randomized, active-controlled, open-label trial. Protocol-specified therapy consisted of Irinotecan 70 mg/m2 with leucovorin 400 mg/m2 and fluorouracil 2400 mg/m2 over 46 hours every 2 weeks (Irinotecan/5-FU/LV; N=117), Irinotecan 100 mg/m 2 every 3 weeks (N=147), or leucovorin 200 mg/m 2 and fluorouracil 2000 mg/m2 over 24 hours weekly for 4 weeks followed by 2 week rest (5-FU/LV; N=134). Serum bilirubin within the institutional normal range, albumin ≥ 3 g/dL, and Karnofsky Performance Status (KPS) ≥ 70 were required for study entry. The median duration of exposure was 9 weeks in the Irinotecan/5-FU/LV arm, 9 weeks in the Irinotecan monotherapy arm, and 6 weeks in the 5-FU/LV arm.
The most common adverse reactions (≥ 20%) of Irinotecan were diarrhea, fatigue/asthenia, vomiting, nausea, decreased appetite, stomatitis, and pyrexia. The most common, severe laboratory abnormalities (≥ 10% Grade 3 or 4) were lymphopenia and neutropenia. The most common serious adverse reactions (≥ 2%) of Irinotecan were diarrhea, vomiting, neutropenic fever or neutropenic sepsis, nausea, pyrexia, sepsis, dehydration, septic shock, pneumonia, acute renal failure, and thrombocytopenia.
Adverse reactions led to permanent discontinuation of Irinotecan in 11% of patients receiving Irinotecan/5-FU/LV; the most frequent adverse reactions resulting in discontinuation of Irinotecan were diarrhea, vomiting, and sepsis. Dose reductions of Irinotecan for adverse reactions occurred in 33% of patients receiving Irinotecan/5-FU/LV; the most frequent adverse reactions requiring dose reductions were neutropenia, diarrhea, nausea, and anemia. Irinotecan was withheld or delayed for adverse reactions in 62% of patients receiving Irinotecan/5-FU/LV; the most frequent adverse reactions requiring interruption or delays were neutropenia, diarrhea, fatigue, vomiting, and thrombocytopenia.
Table 2 provides the frequency and severity of adverse reactions in Study 1 that occurred with higher incidence (≥5% difference for Grades 1-4 or ≥2% difference for Grades 3-4) in patients who received Irinotecan/5-FU/LV compared to patients who received 5-FU/LV.
- Table 2: Adverse Reactions with Higher Incidence (≥5% Difference for Grades 1-4 * or ≥2% Difference for Grades 3 and 4) in the Irinotecan hydrochloride/5-FU/LV Arm

ONIVYDE: Irinotecan hydrochloride's Brand name
- Cholinergic Reactions: Irinotecan can cause cholinergic reactions manifesting as rhinitis, increased salivation, flushing, bradycardia, miosis, lacrimation, diaphoresis, and intestinal hyperperistalsis with abdominal cramping and early onset diarrhea . In Study 1, Grade 1 or 2 cholinergic symptoms other than early diarrhea occurred in 12 (4.5%) Irinotecan-treated patients. Six of these 12 patients received atropine and in 1 of the 6 patients, atropine was administered for cholinergic symptoms other than diarrhea.
Laboratory abnormalities that occurred with higher incidence in the Irinotecan/5-FU/LV arm compared to the 5-FU/LV arm (≥5% difference) are summarized in the following table.
- Table 3: Laboratory Abnormalities with Higher Incidence (≥5% Difference) in the Irinotecan hydrochloride/5-FU/LV Arm *#

ONIVYDE: Irinotecan hydrochloride's Brand name
Postmarketing Experience
There is limited information regarding Irinotecan hydrochloride (Onivyde) Postmarketing Experience in the drug label.
Drug Interactions
Strong CYP3A4 Inducers
Following administration of non-liposomal irinotecan (i.e., irinotecan HCl), exposure to irinotecan or its active metabolite, SN-38, is substantially reduced in adult and pediatric patients concomitantly receiving the CYP3A4 enzyme-inducing anticonvulsants phenytoin and strong CYP3A4 inducers. Avoid the use of strong CYP3A4 inducers (e.g., rifampin, phenytoin, carbamazepine, rifabutin, rifapentine, phenobarbital, St. John's wort ) if possible. Substitute non-enzyme inducing therapies at least 2 weeks prior to initiation of Irinotecan therapy.
Strong CYP3A4 or UGT1A1 Inhibitors
Following administration of non-liposomal irinotecan (i.e., irinotecan HCl), patients receiving concomitant ketoconazole, a CYP3A4 and UGT1A1 inhibitor, have increased exposure to irinotecan and its active metabolite SN-38. Co-administration of Irinotecan with other inhibitors of CYP3A4 (e.g., clarithromycin, indinavir, itraconazole, lopinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telaprevir, voriconazole) or UGT1A1 (e.g., atazanavir, gemfibrozil, indinavir) may increase systemic exposure to irinotecan or SN-38. Avoid the use of strong CYP3A4 or UGT1A1 inhibitors if possible. Discontinue strong CYP3A4 inhibitors at least 1 week prior to starting Irinotecan therapy.
Use in Specific Populations
Pregnancy
- Risk Summary
Based on animal data with irinotecan HCl and the mechanism of action of Irinotecan, Irinotecan can cause fetal harm when administered to a pregnant woman. There are no available data in pregnant women. Embryotoxicity and teratogenicity were observed following treatment with irinotecan HCl, at doses resulting in irinotecan exposures lower than those achieved with Irinotecan 70 mg/m2 in humans, administered to pregnant rats and rabbits during organogenesis. Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
- Data
- Animal Data
No animal studies have been conducted to evaluate the effect of irinotecan liposome on reproduction and fetal development; however, studies have been conducted with irinotecan HCl. Irinotecan crosses the placenta of rats following intravenous administration. Intravenous administration of irinotecan at a dose of 6 mg/kg/day to rats and rabbits during the period of organogenesis resulted in increased post-implantation loss and decreased numbers of live fetuses. In separate studies in rats, this dose resulted in an irinotecan exposure of approximately 0.002 times the exposure of irinotecan based on area under the curve (AUC) in patients administered Irinotecan at the 70 mg/m2 dose. Administration of irinotecan HCl resulted in structural abnormalities and growth delays in rats at doses greater than 1.2 mg/kg/day (approximately 0.0002 times the clinical exposure to irinotecan in Irinotecan hydrochloride based on AUC). Teratogenic effects included a variety of external, visceral, and skeletal abnormalities. Irinotecan HCl administered to rat dams for the period following organogenesis through weaning at doses of 6 mg/kg/day caused decreased learning ability and decreased female body weights in the offspring.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Irinotecan hydrochloride (Onivyde) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Irinotecan hydrochloride (Onivyde) during labor and delivery.
Nursing Mothers
- Risk Summary
There is no information regarding the presence of irinotecan liposome, irinotecan, or SN-38 (an active metabolite of irinotecan) in human milk, or the effects on the breastfed infant or on milk production. Irinotecan is present in rat milk.
Because of the potential for serious adverse reactions in breastfed infants from Irinotecan hydrochloride, advise a nursing woman not to breastfeed during treatment with Irinotecan hydrochloride and for one month after the final dose.
- Data
Radioactivity appeared in rat milk within 5 minutes of intravenous administration of radiolabeled irinotecan HCl and was concentrated up to 65-fold at 4 hours after administration relative to plasma concentrations.
Pediatric Use
Safety and effectiveness of Irinotecan hydrochloride have not been established in pediatric patients.
Geriatic Use
Of the 264 patients who received Irinotecan hydrochloride as a single agent or in combination with 5-FU and leucovorin in Study 1, 49% were ≥ 65 years old and 13% were ≥ 75 years old. No overall differences in safety and effectiveness were observed between these patients and younger patients.
Gender
There is no FDA guidance on the use of Irinotecan hydrochloride (Onivyde) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Irinotecan hydrochloride (Onivyde) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Irinotecan hydrochloride (Onivyde) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Irinotecan hydrochloride (Onivyde) in patients with hepatic impairment.
Females of Reproductive Potential and Males
- Females
Irinotecan hydrochloride can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with Irinotecan hydrochloride and for one month after the final dose.
- Males
Because of the potential for genotoxicity, advise males with female partners of reproductive potential to use condoms during treatment with Irinotecan hydrochloride and for four months after the final dose.
Immunocompromised Patients
There is no FDA guidance one the use of Irinotecan hydrochloride (Onivyde) in patients who are immunocompromised.
Administration and Monitoring
Administration
Irinotecan hydrochloride is a cytotoxic drug. Follow applicable special handling and disposal procedures.
- Preparation
- Withdraw the calculated volume of Irinotecan hydrochloride from the vial. Dilute Irinotecan hydrochloride in 500 mL 5% Dextrose Injection, USP or 0.9% Sodium Chloride Injection, USP and mix diluted solution by gentle inversion.
- Protect diluted solution from light.
- Administer diluted solution within 4 hours of preparation when stored at room temperature or within 24 hours of preparation when stored under refrigerated conditions [2ºC to 8ºC (36ºF to 46ºF)]. Allow diluted solution to come to room temperature prior to administration.
- Do NOT freeze.
- Administration
Infuse diluted solution intravenously over 90 minutes. Do not use in-line filters. Discard unused portion.
Monitoring
There is limited information regarding Irinotecan hydrochloride (Onivyde) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Irinotecan hydrochloride (Onivyde) and IV administrations.
Overdosage
There are no treatment interventions known to be effective for management of overdosage of Irinotecan hydrochloride.
Pharmacology
Mechanism of Action
Irinotecan liposome injection is a topoisomerase 1 inhibitor encapsulated in a lipid bilayer vesicle or liposome. Topoisomerase 1 relieves torsional strain in DNA by inducing single-strand breaks. Irinotecan and its active metabolite SN-38 bind reversibly to the topoisomerase 1-DNA complex and prevent re-ligation of the single-strand breaks, leading to exposure time-dependent double-strand DNA damage and cell death. In mice bearing human tumor xenografts, irinotecan liposome administered at irinotecan HCl-equivalent doses 5-fold lower than irinotecan HCl achieved similar intratumoral exposure of SN-38.
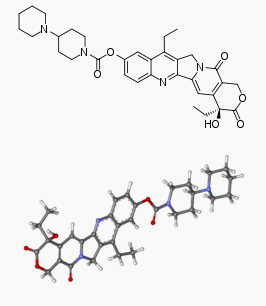
Structure
Irinotecan hydrochloride is formulated with irinotecan hydrochloride trihydrate, a topoisomerase inhibitor, into a liposomal dispersion for intravenous use. The chemical name of irinotecan hydrochloride trihydrate is (S)-4,11-diethyl-3,4,12,14-tetrahydro-4-hydroxy-3,14-dioxo1H-pyrano[3’,4’:6,7]-indolizino[1,2-b]quinolin-9-yl-[1,4’bipiperidine]-1’-carboxylate, monohydrochloride, trihydrate. The empirical formula is C 33H 38N 4O 6∙HCl∙3H 2O and the molecular weight is 677.19 g/mole. The molecular structure is:

Irinotecan hydrochloride is a sterile, white to slightly yellow opaque isotonic liposomal dispersion. Each 10 mL single-dose vial contains 43 mg irinotecan free base at a concentration of 4.3 mg/mL. The liposome is a unilamellar lipid bilayer vesicle, approximately 110 nm in diameter, which encapsulates an aqueous space containing irinotecan in a gelated or precipitated state as the sucrose octasulfate salt. The vesicle is composed of 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC) 6.81 mg/mL, cholesterol 2.22 mg/mL, and methoxy-terminated polyethylene glycol (MW 2000)-distearoylphosphatidyl ethanolamine (MPEG-2000-DSPE) 0.12 mg/mL. Each mL also contains 2-[4-(2-hydroxyethyl) piperazin-1-yl]ethanesulfonic acid (HEPES) as a buffer 4.05 mg/mL and sodium chloride as an isotonicity reagent 8.42 mg/mL.
Pharmacodynamics
There is limited information regarding Irinotecan hydrochloride (Onivyde) Pharmacodynamics in the drug label.
Pharmacokinetics
The plasma pharmacokinetics of total irinotecan and total SN-38 were evaluated in patients with cancer who received Irinotecan hydrochloride, as a single agent or as part of combination chemotherapy, at doses between 50 and 155 mg/m2 and 353 patients with cancer using population pharmacokinetic analysis.
The pharmacokinetic parameters of total irinotecan and total SN-38 following the administration of Irinotecan hydrochloride 70 mg/m2 as a single agent or part of combination chemotherapy are presented in Table 4.
- Table 4: Summary of Mean (±Standard Deviation) Total Irinotecan and Total SN-38

Over the dose range of 50 to 155 mg/m2, the Cmax and AUC of total irinotecan increases with dose. Additionally, the Cmax of total SN-38 increases proportionally with dose; however, the AUC of total SN-38 increases less than proportionally with dose.
Direct measurement of irinotecan liposome showed that 95% of irinotecan remains liposome-encapsulated, and the ratios between total and encapsulated forms did not change with time from 0 to 169.5 hours post-dose. The mean volume of distribution is summarized in Table 4.
Plasma protein binding is <0.44% of the total irinotecan in Irinotecan hydrochloride.
- Elimination
The metabolism of irinotecan liposome has not been evaluated. Irinotecan is subject to extensive metabolic conversion by various enzyme systems, including esterases to form the active metabolite SN-38, and UGT1A1 mediating glucuronidation of SN-38 to form the inactive glucuronide metabolite SN-38G. Irinotecan can also undergo CYP3A4-mediated oxidative metabolism to several inactive oxidation products, one of which can be hydrolyzed by carboxylesterase to release SN-38. In the population pharmacokinetic analysis using the results of a subset with UGT1A1*28 genotypic testing, in which the analysis adjusted for the lower dose administered to patients homozygous for the UGT1A1*28 allele, patients homozygous (N=14) and non-homozygous (N=244) for this allele had total SN-38 average steady-state concentrations of 1.06 and 0.95 ng/mL, respectively.
The disposition of Irinotecan hydrochloride has not been elucidated in humans. Following administration of irinotecan HCl , the urinary excretion of irinotecan is 11 to 20%; SN-38, <1%; and SN-38 glucuronide, 3%. The cumulative biliary and urinary excretion of irinotecan and its metabolites (SN-38 and SN-38 glucuronide), over a period of 48 hours following administration of irinotecan HCl in two patients, ranged from approximately 25% (100 mg/m 2) to 50% (300 mg/m 2).
- Specific Populations
- Age, Gender, and Renal Impairment:
The population pharmacokinetic analysis suggests that age (28 to 87 years) had no clinically meaningful effect on the exposure of irinotecan and SN-38.
The population pharmacokinetic analysis suggests that gender (196 males and 157 females) had no clinically meaningful effect on the exposure of irinotecan and SN-38 after adjusting for body surface area (BSA).
In a population pharmacokinetic analysis, mild-to-moderate renal impairment had no effect on the exposure of total SN-38 after adjusting for BSA. The analysis included 68 patients with moderate (CLcr 30 - 59 mL/min) renal impairment, 147 patients with mild (CLcr 60 - 89 mL/min) renal impairment, and 135 patients with normal renal function (CLcr > 90 mL/min). There was insufficient data in patients with severe renal impairment (CLcr < 30 mL/min) to assess its effect on pharmacokinetics.
- Ethnicity: The population pharmacokinetic analysis suggests that Asians (East Asians, N=150) have 56% lower total irinotecan average steady state concentration and 8% higher total SN-38 average steady state concentration than Whites (N=182).
- Hepatic Impairment: The pharmacokinetics of irinotecan liposome have not been studied in patients with hepatic impairment. In a population pharmacokinetic analysis, patients with baseline bilirubin concentrations of 1-2 mg/dL (N=19) had average steady state concentrations for total SN-38 that were increased by 37% compared to patients with baseline bilirubin concentrations of <1 mg/dL (N=329); however, there was no effect of elevated ALT/AST concentrations on total SN-38 concentrations. No data are available in patients with bilirubin >2 mg/dL.
- Drug Interactions
In a population pharmacokinetic analysis, the pharmacokinetics of total irinotecan and total SN-38 were not altered by the co-administration of fluorouracil/leucovorin.
Following administration of irinotecan HCl, dexamethasone, a moderate CYP3A4 inducer, does not alter the pharmacokinetics of irinotecan.
In vitro studies indicate that irinotecan, SN-38 and another metabolite, aminopentane carboxylic acid (APC), do not inhibit cytochrome P-450 isozymes.
Pharmacogenomics
Individuals who are homozygous for the UGT1A1*28 allele are at increased risk for neutropenia from irinotecan HCl. In Study 1, patients homozygous for the UGT1A1*28 allele (N=7) initiated Irinotecan hydrochloride at a reduced dose of 50 mg/m 2 in combination with 5-FU/LV. The frequency of Grade 3 or 4 neutropenia in these patients [2 of 7 (28.6% )] was similar to the frequency in patients not homozygous for the UGT1A1*28 allele who received a starting dose of Irinotecan hydrochloride of 70 mg/m2 [30 of 110 (27.3%)].
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been performed to assess the potential of irinotecan liposome for carcinogenicity, genotoxicity or impairment of fertility. Intravenous administration of irinotecan hydrochloride to rats once weekly for 13 weeks followed by a 91-week recovery period resulted in a significant linear trend between irinotecan HCl dosage and the incidence of combined uterine horn endometrial stromal polyps and endometrial stromal sarcomas. Irinotecan HCl was clastogenic both in vitro (chromosome aberrations in Chinese hamster ovary cells) and in vivo (micronucleus test in mice). Neither irinotecan nor its active metabolite, SN-38, was mutagenic in the in vitro Ames assay.
Dedicated fertility studies have not been performed with irinotecan liposome injection. Atrophy of male and female reproductive organs was observed in dogs receiving irinotecan liposome injection every 3 weeks at doses equal to or greater than 15 mg/kg, (approximately 3 times the clinical exposure of irinotecan following administration to Irinotecan hydrochloride dosed at 70 mg/m2 ) for a total of 6 doses. No significant adverse effects on fertility and general reproductive performance were observed after intravenous administration of irinotecan HCl in doses of up to 6 mg/kg/day to rats; however, atrophy of male reproductive organs was observed after multiple daily irinotecan HCl doses both in rodents at 20 mg/kg (approximately 0.007 times the clinical irinotecan exposure following Irinotecan hydrochloride administration at 70 mg/m2) and in dogs at 0.4 mg/kg (0.0007 times the clinical exposure to irinotecan following administration of Irinotecan hydrochloride).
Clinical Studies
The efficacy of Irinotecan hydrochloride was evaluated in Study 1, a three-arm, randomized, open-label trial in patients with metastatic pancreatic adenocarcinoma with documented disease progression, after gemcitabine or gemcitabine-based therapy. Key eligibility criteria included Karnofsky Performance Status (KPS) ≥70, serum bilirubin within institution limits of normal, and albumin ≥3.0 g/dL. Patients were randomized to receive Irinotecan hydrochloride plus fluorouracil/leucovorin (Irinotecan hydrochloride/5-FU/LV), Irinotecan hydrochloride, or fluorouracil/leucovorin (5-FU/LV). Randomization was stratified by ethnicity (White vs. East Asian vs. other), KPS (70-80 vs. 90-100), and baseline albumin level (≥ 4 g/dL vs. 3.0-3.9 g/dL). Patients randomized to Irinotecan hydrochloride/5-FU/LV received Irinotecan hydrochloride 70 mg/m2 as an intravenous infusion over 90 minutes, followed by leucovorin 400 mg/m2 intravenously over 30 minutes, followed by fluorouracil 2400 mg/m2 intravenously over 46 hours, every 2 weeks. The Irinotecan hydrochloride dose of 70 mg/m 2 is based on irinotecan free base (equivalent to 80 mg/m 2 of irinotecan as the hydrochloride trihydrate). Patients randomized to Irinotecan hydrochloride as a single agent received Irinotecan hydrochloride 100 mg/m 2 as an intravenous infusion over 90 minutes every 3 weeks. Patients randomized to 5-FU/LV received leucovorin 200 mg/m 2 intravenously over 30 minutes, followed by fluorouracil 2000 mg/m 2 intravenously over 24 hours, administered on Days 1, 8, 15 and 22 of a 6-week cycle. Patients homozygous for the UGT1A1*28 allele initiated Irinotecan hydrochloride at a reduced dose (50 mg/m2 Irinotecan hydrochloride, if given with 5-FU/LV or 70 mg/m 2 Irinotecan hydrochloride as a single agent). When Irinotecan hydrochloride was withheld or discontinued for adverse reactions, 5-FU was also withheld or discontinued. When the dose of Irinotecan hydrochloride was reduced for adverse reactions, the dose of 5-FU was reduced by 25%. Treatment continued until disease progression or unacceptable toxicity.
The major efficacy outcome measure was overall survival (OS) with two pair-wise comparisons: Irinotecan hydrochloride versus 5-FU/LV and Irinotecan hydrochloride/5-FU/LV versus 5-FU/LV. Additional efficacy outcome measures were progression-free survival (PFS) and objective response rate (ORR). Tumor status assessments were conducted at baseline and every 6 weeks thereafter. The trial was initiated as a two-arm study and amended after initiation to include a third arm (Irinotecan hydrochloride/5-FU/LV). The comparisons between the Irinotecan hydrochloride/5-FU/LV and the 5-FU/LV arms are limited to patients enrolled in the 5-FU/LV arm after this protocol amendment.
Four hundred seventeen patients were randomized to: Irinotecan hydrochloride/5-FU/LV (N=117), Irinotecan hydrochloride(N=151), or 5-FU/LV (N=149). Baseline demographics and tumor characteristics for the 236 patients randomized to Irinotecan hydrochloride/5-FU/LV or 5-FU/LV (N=119) after the addition of the third arm to the study were a median age of 63 years (range 34-81 years) and with 41% ≥ 65 years of age; 58% were men; 63% were White, 30% were Asian, 3% were Black or African American, and 5% were other. Mean baseline albumin level was 3.97 g/dL, and baseline KPS was 90-100 in 53% of patients. Disease characteristics included liver metastasis (67%) and lung metastasis (31%). A total of 13% of patients received gemcitabine in the neoadjuvant/adjuvant setting only, 55% of patients had 1 prior line of therapy for metastatic disease, and 33% of patients had 2 or more prior lines of therapy for metastatic disease. All patients received prior gemcitabine (alone or in combination with another agent), 54% received prior gemcitabine in combination with another agent, and 13% received prior gemcitabine in combination with nab-paclitaxel.
Study 1 demonstrated a statistically significant improvement in overall survival for the Irinotecan hydrochloride/5-FU/LV arm over the 5-FU/LV arm as summarized in Table 5 and Figure 1.
There was no improvement in overall survival for the Irinotecan hydrochloride arm over the 5-FU/LV arm (hazard ratio=1.00, p-value=0.97 (two-sided log-rank test)).
- Table 5: Efficacy Results from Study 1 †

ONIVYDE: Irinotecan hydrochloride's Brand name
- Figure 1

ONIVYDE: Irinotecan hydrochloride's Brand name
How Supplied
Irinotecan hydrochloride is available in a single-dose vial containing 43 mg irinotecan free base as a white to slightly yellow, opaque, liposomal dispersion at a concentration of 4.3 mg/mL
NDC: 69171-398-01
Storage
Store Irinotecan hydrochloride at 2ºC to 8ºC (36°F to 46°F). Do NOT freeze. Protect from light.
Irinotecan hydrochloride is a cytotoxic drug. Follow applicable special handling and disposal procedures.
Images
Drug Images
{{#ask: Page Name::Irinotecan hydrochloride (Onivyde) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


{{#ask: Label Page::Irinotecan hydrochloride (Onivyde) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise patients of the following:
- Severe Neutropenia
Advise patients of the risk of neutropenia leading to severe and life-threatening infections and the need for monitoring of blood counts. Instruct patients to contact their healthcare provider immediately if experiencing signs of infection, such as fever, chills, dizziness, or shortness of breath.
- Severe Diarrhea
Inform patients of the risk of severe diarrhea. Advise patients to contact their healthcare provider if they experience persistent vomiting or diarrhea; black or bloody stools; or symptoms of dehydration such as lightheadedness, dizziness, or faintness.
Inform patients of the potential risk of ILD. Advise patients to contact their healthcare provider as soon as possible for new onset cough or dyspnea.
- Hypersensitivity to irinotecan HCl or this drug
Advise patients of the potential risk of severe hypersensitivity and that Irinotecan hydrochloride is contraindicated in patients with a history of severe allergic reactions with irinotecan HCl or this drug. Instruct patients to seek immediate medical attention for signs of severe hypersensitivity reaction such as chest tightness; shortness of breath; wheezing; dizziness or faintness; or swelling of the face, eyelids, or lips.
- Females and males of reproductive potential
- Embryo-fetal toxicity: Inform females of reproductive potential of the potential risk to a fetus, to use effective contraception during treatment and for one month after the final dose, and to inform their healthcare provider of a known or suspected pregnancy.
- Contraception: Advise male patients with female partners of reproductive potential to use condoms during treatment with Irinotecan hydrochloride and for four months after the final dose.
- Lactation
Advise women not to breastfeed during treatment with Irinotecan hydrochloride and for one month after the final dose.
Precautions with Alcohol
Alcohol-Irinotecan hydrochloride (Onivyde) interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
ONIVYDE ™
Look-Alike Drug Names
There is limited information regarding Irinotecan hydrochloride (Onivyde) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Verschraegen CF, Levy T, Kudelka AP, Llerena E, Ende K, Freedman RS; et al. (1997). "Phase II study of irinotecan in prior chemotherapy-treated squamous cell carcinoma of the cervix". J Clin Oncol. 15 (2): 625–31. doi:10.1200/jco.1997.15.2.625. PMID 9053486.
- ↑ Ilson DH, Minsky B, Kelsen D (2002). "Irinotecan, cisplatin, and radiation in esophageal cancer". Oncology (Williston Park). 16 (5 Suppl 5): 11–5. PMID 12109799.
- ↑ Hermes A, Bergman B, Bremnes R, Ek L, Fluge S, Sederholm C; et al. (2008). "Irinotecan plus carboplatin versus oral etoposide plus carboplatin in extensive small-cell lung cancer: a randomized phase III trial". J Clin Oncol. 26 (26): 4261–7. doi:10.1200/JCO.2007.15.7545. PMID 18779613.
- ↑ Schmittel A, Fischer von Weikersthal L, Sebastian M, Martus P, Schulze K, Hortig P; et al. (2006). "A randomized phase II trial of irinotecan plus carboplatin versus etoposide plus carboplatin treatment in patients with extended disease small-cell lung cancer". Ann Oncol. 17 (4): 663–7. doi:10.1093/annonc/mdj137. PMID 16423848.
- ↑ Noda K, Nishiwaki Y, Kawahara M, Negoro S, Sugiura T, Yokoyama A; et al. (2002). "Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small-cell lung cancer". N Engl J Med. 346 (2): 85–91. doi:10.1056/NEJMoa003034. PMID 11784874.
- ↑ Lara PN, Natale R, Crowley J, Lenz HJ, Redman MW, Carleton JE; et al. (2009). "Phase III trial of irinotecan/cisplatin compared with etoposide/cisplatin in extensive-stage small-cell lung cancer: clinical and pharmacogenomic results from SWOG S0124". J Clin Oncol. 27 (15): 2530–5. doi:10.1200/JCO.2008.20.1061. PMC 2684855. PMID 19349543.
- ↑ Higuchi K, Tanabe S, Shimada K, Hosaka H, Sasaki E, Nakayama N; et al. (2014). "Biweekly irinotecan plus cisplatin versus irinotecan alone as second-line treatment for advanced gastric cancer: a randomised phase III trial (TCOG GI-0801/BIRIP trial)". Eur J Cancer. 50 (8): 1437–45. doi:10.1016/j.ejca.2014.01.020. PMID 24560487.
- ↑ Hironaka S, Ueda S, Yasui H, Nishina T, Tsuda M, Tsumura T; et al. (2013). "Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combination chemotherapy using fluoropyrimidine plus platinum: WJOG 4007 trial". J Clin Oncol. 31 (35): 4438–44. doi:10.1200/JCO.2012.48.5805. PMID 24190112.
- ↑ Kang JH, Lee SI, Lim DH, Park KW, Oh SY, Kwon HC; et al. (2012). "Salvage chemotherapy for pretreated gastric cancer: a randomized phase III trial comparing chemotherapy plus best supportive care with best supportive care alone". J Clin Oncol. 30 (13): 1513–8. doi:10.1200/JCO.2011.39.4585. PMID 22412140 DOI: 10.1200/JCO.2011.39.4585 PMID: 22412140 DOI: 10.1200/JCO.2011.39.4585 Check
|pmid=value (help). - ↑ O'Reilly EM, Stuart KE, Sanz-Altamira PM, Schwartz GK, Steger CM, Raeburn L; et al. (2001). "A phase II study of irinotecan in patients with advanced hepatocellular carcinoma". Cancer. 91 (1): 101–5. PMID 11148565.
- ↑ Batchelor TT, Gilbert MR, Supko JG, Carson KA, Nabors LB, Grossman SA; et al. (2004). "Phase 2 study of weekly irinotecan in adults with recurrent malignant glioma: final report of NABTT 97-11". Neuro Oncol. 6 (1): 21–7. doi:10.1215/S1152-8517-03-00021-8. PMC 1871974. PMID 14769136.
- ↑ Cloughesy TF, Filka E, Kuhn J, Nelson G, Kabbinavar F, Friedman H; et al. (2003). "Two studies evaluating irinotecan treatment for recurrent malignant glioma using an every-3-week regimen". Cancer. 97 (9 Suppl): 2381–6. doi:10.1002/cncr.11306. PMID 12712460.
- ↑ Prados MD, Lamborn K, Yung WK, Jaeckle K, Robins HI, Mehta M; et al. (2006). "A phase 2 trial of irinotecan (CPT-11) in patients with recurrent malignant glioma: a North American Brain Tumor Consortium study". Neuro Oncol. 8 (2): 189–93. doi:10.1215/15228517-2005-010. PMC 1871932. PMID 16533878.
- ↑ Vredenburgh JJ, Desjardins A, Herndon JE, Dowell JM, Reardon DA, Quinn JA; et al. (2007). "Phase II trial of bevacizumab and irinotecan in recurrent malignant glioma". Clin Cancer Res. 13 (4): 1253–9. doi:10.1158/1078-0432.CCR-06-2309. PMID 17317837.
- ↑ Brandes AA, Tosoni A, Basso U, Reni M, Valduga F, Monfardini S; et al. (2004). "Second-line chemotherapy with irinotecan plus carmustine in glioblastoma recurrent or progressive after first-line temozolomide chemotherapy: a phase II study of the Gruppo Italiano Cooperativo di Neuro-Oncologia (GICNO)". J Clin Oncol. 22 (23): 4779–86. doi:10.1200/JCO.2004.06.181. PMID 15570079.
- ↑ Perez EA, Hillman DW, Mailliard JA, Ingle JN, Ryan JM, Fitch TR; et al. (2004). "Randomized phase II study of two irinotecan schedules for patients with metastatic breast cancer refractory to an anthracycline, a taxane, or both". J Clin Oncol. 22 (14): 2849–55. doi:10.1200/JCO.2004.10.047. PMID 15254052.
- ↑ Shigeoka Y, Itoh K, Igarashi T, Ishizawa K, Saeki T, Fujii H; et al. (2001). "Clinical effect of irinotecan in advanced and metastatic breast cancer patients previously treated with doxorubicin- and docetaxel-containing regimens". Jpn J Clin Oncol. 31 (8): 370–4. PMID 11574629.
- ↑ Takagi T, Saotome T (2001). "Chemotherapy with irinotecan (CPT-11), a topoisomerase-I inhibitor, for refractory and relapsed non-Hodgkin's lymphoma". Leuk Lymphoma. 42 (4): 577–86. doi:10.3109/10428190109099317. PMID 11697485.
- ↑ Chang MH, Kim KH, Jun HJ, Kim HS, Yi SY, Uhm JE; et al. (2009). "Irinotecan and oxaliplatin combination as the first-line treatment for patients with advanced non-small cell lung cancer". Cancer Chemother Pharmacol. 64 (5): 917–24. doi:10.1007/s00280-009-0943-7. PMID 19221753.
- ↑ Masuda N, Fukuoka M, Fujita A, Kurita Y, Tsuchiya S, Nagao K; et al. (1998). "A phase II trial of combination of CPT-11 and cisplatin for advanced non-small-cell lung cancer. CPT-11 Lung Cancer Study Group". Br J Cancer. 78 (2): 251–6. PMC 2062886. PMID 9683302.
- ↑ Kobayashi K, Shinbara A, Kamimura M, Takeda Y, Kudo K, Kabe J; et al. (1998). "Irinotecan (CPT-11) in combination with weekly administration of cisplatin (CDDP) for non-small-cell lung cancer". Cancer Chemother Pharmacol. 42 (1): 53–8. doi:10.1007/s002800050784. PMID 9619758.
- ↑ Masuda N, Fukuoka M, Takada M, Kusunoki Y, Negoro S, Matsui K; et al. (1992). "CPT-11 in combination with cisplatin for advanced non-small-cell lung cancer". J Clin Oncol. 10 (11): 1775–80. doi:10.1200/jco.1992.10.11.1775. PMID 1328551.
- ↑ Polyzos A, Kosmas C, Toufexi H, Malamos N, Lagadas A, Kosmidis C; et al. (2005). "Docetaxel in combination with irinotecan (CPT-11) in platinum-resistant paclitaxel-pretreated ovarian cancer". Anticancer Res. 25 (5): 3559–64. PMID 16101180.
- ↑ Shimizu Y, Umezawa S, Hasumi K (1998). "A phase II study of combined CPT-11 and mitomycin-C in platinum refractory clear cell and mucinous ovarian carcinoma". Ann Acad Med Singapore. 27 (5): 650–6. PMID 9919334.
- ↑ Bodurka DC, Levenback C, Wolf JK, Gano J, Wharton JT, Kavanagh JJ; et al. (2003). "Phase II trial of irinotecan in patients with metastatic epithelial ovarian cancer or peritoneal cancer". J Clin Oncol. 21 (2): 291–7. doi:10.1200/JCO.2003.02.091. PMID 12525521.
- ↑ Pappo AS, Lyden E, Breitfeld P, Donaldson SS, Wiener E, Parham D; et al. (2007). "Two consecutive phase II window trials of irinotecan alone or in combination with vincristine for the treatment of metastatic rhabdomyosarcoma: the Children's Oncology Group". J Clin Oncol. 25 (4): 362–9. doi:10.1200/JCO.2006.07.1720. PMID 17264331.
- ↑ Bisogno G, Riccardi R, Ruggiero A, Arcamone G, Prete A, Surico G; et al. (2006). "Phase II study of a protracted irinotecan schedule in children with refractory or recurrent soft tissue sarcoma". Cancer. 106 (3): 703–7. doi:10.1002/cncr.21629. PMID 16369989.