Influenza pandemic
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4]
Overview
An influenza pandemic is an epidemic of the influenza virus that spreads on a worldwide scale and infects a large proportion of the human population. In contrast to the regular seasonal epidemics of influenza, these pandemics occur irregularly, with the 1918 Spanish flu the most serious pandemic in recent history. Pandemics can cause high levels of mortality, with the Spanish influenza being responsible for the deaths of over 50 million people. There have been about 3 influenza pandemics in each century for the last 300 years. The most recent ones were the Asian Flu in 1957 and the Hong Kong Flu in 1968.
Influenza pandemics occur when a new strain of the influenza virus is transmitted to humans from another animal species. Species that are thought to be important in the emergence of new human strains are pigs, chickens and ducks. These novel strains are unaffected by any immunity people may have to older strains of human influenza and can therefore spread extremely rapidly and infect very large numbers of people. Influenza A viruses can occasionally be transmitted from wild birds to other species causing outbreaks in domestic poultry and may give rise to human influenza pandemics.[1] [2]
The World Health Organization (WHO) warns that there is a substantial risk of an influenza pandemic within the next few years. One of the strongest candidates is a highly pathogenic variation of the H5N1 subtype of Influenza A virus. As of 2006, prepandemic influenza vaccines are being developed against the most likely suspects which include H5N1, H7N1, and H9N2.[3]
Influenza
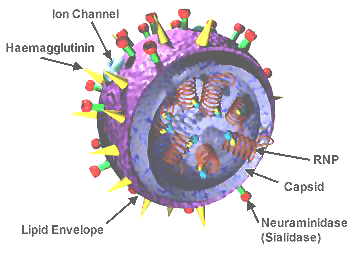
Influenza, commonly known as flu, is an infectious disease of birds and mammals caused by an RNA virus of the family Orthomyxoviridae (the influenza viruses). In humans, common symptoms of influenza infection are fever, sore throat, muscle pains, severe headache, coughing, and weakness and fatigue.[4] In more serious cases, influenza causes pneumonia, which can be fatal, particularly in young children and the elderly. Sometimes confused with the common cold, influenza is a much more severe disease and is caused by a different type of virus.[5] Although nausea and vomiting can be produced, especially in children,[4] these symptoms are more characteristic of the unrelated gastroenteritis, which is sometimes called "stomach flu" or "24-hour flu."[6]
Typically, influenza is transmitted from infected mammals through the air by coughs or sneezes, creating aerosols containing the virus, and from infected birds through their droppings. Influenza can also be transmitted by saliva, nasal secretions, feces and blood. Infections occur through contact with these bodily fluids or with contaminated surfaces. Flu viruses can remain infectious for about one week at human body temperature, over 30 days at 0 °C (32 °F), and indefinitely at very low temperatures (such as lakes in northeast Siberia). Most influenza strains can be inactivated easily by disinfectants and detergents.[7][8][9]
Flu spreads around the world in seasonal epidemics, killing millions of people in pandemic years and hundreds of thousands in non-pandemic years. Three influenza pandemics occurred in the 20th century and killed tens of millions of people, with each of these pandemics being caused by the appearance of a new strain of the virus in humans. Often, these new strains result from the spread of an existing flu virus to humans from other animal species. Since it first killed humans in Asia in the 1990s, a deadly avian strain of H5N1 has posed the greatest risk for a new influenza pandemic; however, this virus has not mutated to spread easily between people.[10]
Vaccinations against influenza are most commonly given to high-risk humans in industrialized countries[11] and to farmed poultry.[12] The most common human vaccine is the trivalent influenza vaccine that contains purified and inactivated material from three viral strains. Typically this vaccine includes material from two influenza A virus subtypes and one influenza B virus strain.[13] A vaccine formulated for one year may be ineffective in the following year, since the influenza virus changes rapidly over time and different strains become dominant. Antiviral drugs can be used to treat influenza, with neuraminidase inhibitors being particularly effective.
Variants and subtypes of Influenzavirus A
Variants of Influenzavirus A are identified and named according to the isolate that they are like and thus are presumed to share lineage (example Fujian flu virus like); according to their typical host (example Human flu virus); according to their subtype (example H3N2); and according to their deadliness (example LP). So a flu from a virus similar to the isolate A/Fujian/411/2002(H3N2) is called Fujian flu, human flu, and H3N2 flu.[14]
Variants are sometimes named according to the species (host) the strain is endemic in or adapted to. Some variants named using this convention are:[15]
Avian variants have also sometimes been named according to their deadliness in poultry, especially chickens:
- Low Pathogenic Avian Influenza (LPAI)
- Highly Pathogenic Avian Influenza (HPAI), also called: deadly flu or death flu
The Influenza A virus subtypes are labeled according to an H number (for hemagglutinin) and an N number (for neuraminidase). Each subtype virus has mutated into a variety of strains with differing pathogenic profiles; some pathogenic to one species but not others, some pathogenic to multiple species. Most known strains are extinct strains. For example, the annual flu subtype H3N2 no longer contains the strain that caused the Hong Kong Flu.[14]
Influenza A viruses are negative sense, single-stranded, segmented RNA viruses. "There are 16 different HA antigens (H1 to H16) and nine different NA antigens (N1 to N9) for influenza A. Until recently, 15 HA types had been recognized, but a new type (H16) was isolated from black-headed gulls caught in Sweden and the Netherlands in 1999 and reported in the literature in 2005." [16]
Nature of a flu pandemic
Some pandemics are relatively minor such as the one in 1957 called "Asian flu". Others have a higher Pandemic Severity Index whose severity warrants more comprehensive social isolation measures.[17]
In a bad pandemic, some communities attempt to cut themselves off totally while others have half (or more) of their population die, and others may not feel many of the effects but may still be affected due to the high degree of illness and the bereavement felt by the members of the community. Desperate people try anything to cure or prevent the illness.[18] The 1918 pandemic killed around 150,000 people in the UK, but even the loss of this relatively small number of people in the population caused upheaval and psychological damage to many people.[19] There are not enough doctors, hospital rooms, or medical supplies for the living due to their contracting the disease and dead bodies often lie unburied as few people are available to deal with them. There is great social disruption and a sense of fear and efforts to deal with the pandemic always leave a great deal to be desired due to selfishness, lack of trust, illegal behavior, and ignorance. For example in the 1918 pandemic "This horrific disconnect between reassurances and reality destroyed the credibility of those in authority. People felt they had no one to turn to, no one to rely on, no one to trust." [20]
A letter from a physician at one U.S. Army camp in the 1918 pandemic said:
- It is only a matter of a few hours then until death comes [...]. It is horrible. One can stand it to see one, two or twenty men die, but to see these poor devils dropping like flies [...]. We have been averaging about 100 deaths per day [...]. Pneumonia means in about all cases death [...]. We have lost an outrageous number of Nurses and Drs. It takes special trains to carry away the dead. For several days there were no coffins and the bodies piled up something fierce [...]. [21]
Wave nature
Flu pandemics typically come in waves. The 1889–1890 and 1918-1919 flu pandemics each came in three or four waves of increasing lethality. [22] But within a wave, mortality was greater at the beginning of the wave. [23]
Variable mortality
Mortality varies widely in a pandemic. In the 1918 pandemic:
- In U.S. Army camps where reasonably reliable statistics were kept, case mortality often exceeded 5 percent, and in some circumstances exceeded 10 percent. In the British Army in India, case mortality for white troops was 9.6 percent, for Indian troops 21.9 percent. In isolated human populations, the virus killed at even higher rates. In the Fiji islands, it killed 14 percent of the entire population in 16 days. In Labrador and Alaska, it killed at least one-third of the entire native population. [24]
Notable influenza pandemics
| Name of pandemic | Date | Deaths | Subtype involved |
|---|---|---|---|
| Asiatic (Russian) Flu | 1889-90 | 1 million | possibly H2N2 |
| Spanish Flu | 1918-20 | 40 million | H1N1 |
| Asian Flu | 1957-58 | 1 to 1.5 million | H2N2 |
| Hong Kong Flu | 1968-69 | 0.75 to 1 million | H3N2 |
Spanish Flu (1918–1920)
The 1918 flu pandemic, commonly referred to as the Spanish flu, was a category 5 influenza pandemic caused by an unusually severe and deadly Influenza A virus strain of subtype H1N1. Many of its victims were healthy young adults, in contrast to most influenza outbreaks which predominantly affect juvenile, elderly, or otherwise weakened patients.

The Spanish flu pandemic lasted from 1918 to 1919. Older estimates say it killed 40–50 million people[27] while current estimates say 50 million to 100 million people worldwide were killed.[28] This pandemic has been described as "the greatest medical holocaust in history" and may have killed as many people as the Black Death.[29] This huge death toll was caused by an extremely high infection rate of up to 50% and the extreme severity of the symptoms, suspected to be caused by cytokine storms.[27] Indeed, symptoms in 1918 were so unusual that initially influenza was misdiagnosed as dengue, cholera, or typhoid. One observer wrote, "One of the most striking of the complications was hemorrhage from mucous membranes, especially from the nose, stomach, and intestine. Bleeding from the ears and petechial hemorrhages in the skin also occurred."[28] The majority of deaths were from bacterial pneumonia, a secondary infection caused by influenza, but the virus also killed people directly, causing massive hemorrhages and edema in the lung.[26]
The Spanish flu pandemic was truly global, spreading even to the Arctic and remote Pacific islands. The unusually severe disease killed between 2 and 20% of those infected, as opposed to the more usual flu epidemic mortality rate of 0.1%.[26][28] Another unusual feature of this pandemic was that it mostly killed young adults, with 99% of pandemic influenza deaths occurring in people under 65, and more than half in young adults 20 to 40 years old.[30] This is unusual since influenza is normally most deadly to the very young (under age 2) and the very old (over age 70). The total mortality of the 1918–1919 pandemic is not known, but it is estimated that 2.5% to 5% of the world's population was killed. As many as 25 million may have been killed in the first 25 weeks; in contrast, HIV/AIDS has killed 25 million in its first 25 years.[28]
Asian Flu (1957–1958)
The "Asian Flu" was a category 2 flu pandemic outbreak of avian influenza that originated in China in early 1956 lasting until 1958. It originated from mutation in wild ducks combining with a pre-existing human strain.[31] The virus was first identified in Guizhou.[32] It spread to Singapore in February 1957, reached Hong Kong by April, and US by June. Death toll in the US was approximately 69,800.[31] Estimates of worldwide infection rate varies widely depending on source, ranging from 1 million to 4 million.
Hong Kong Flu (1968–1969)
The Hong Kong Flu was a category 2 flu pandemic caused by a strain of H3N2 descended from H2N2 by antigenic shift, in which genes from multiple subtypes reassorted to form a new virus. The Hong Kong Flu pandemic of 1968 and 1969 infected an estimate 500,000 with a low death rate[33][34]. In the US, 50 million were infected with an estimated 33,000 deaths[35].
H5N1
Influenza A virus subtype H5N1, also known as A(H5N1) or simply H5N1, is a subtype of the Influenza A virus which can cause illness in humans and many other animal species.[36] A bird-adapted strain of H5N1, called HPAI A(H5N1) for "highly pathogenic avian influenza virus of type A of subtype H5N1", is the causative agent of H5N1 flu, commonly known as "avian influenza" or "bird flu". It is endemic in many bird populations, especially in Southeast Asia. One strain of HPAI A(H5N1) is spreading globally after first appearing in Asia. It is epizootic (an epidemic in nonhumans) and panzootic (affecting animals of many species, especially over a wide area), killing tens of millions of birds and spurring the culling of hundreds of millions of others to stem its spread. Most mentions of "bird flu" and H5N1 in the media refer to this strain.[37]
HPAI A(H5N1) is an avian disease. There is no evidence of efficient human-to-human transmission or of airborne transmission of HPAI A(H5N1) to humans. In almost all cases, those infected with H5N1 had extensive physical contact with infected birds. Still, around 60% of humans known to have been infected with the current Asian strain of HPAI A(H5N1) have died from it, and H5N1 may mutate or reassort into a strain capable of efficient human-to-human transmission.[38][39][40][41][42][43][44]
In 2003, world-renowned virologist Robert Webster published an article titled "The world is teetering on the edge of a pandemic that could kill a large fraction of the human population" in American Scientist. He called for adequate resources to fight what he sees as a major world threat to possibly billions of lives.[45] On September 29, 2005, David Nabarro, the newly-appointed Senior United Nations System Coordinator for Avian and Human Influenza, warned the world that an outbreak of avian influenza could kill anywhere between 5 million and 150 million people.[46] Experts have identified key events (creating new clades, infecting new species, spreading to new areas) marking the progression of an avian flu virus towards becoming pandemic, and many of those key events have occurred more rapidly than expected.
Due to the high lethality and virulence of HPAI A(H5N1), its endemic presence, its increasingly large host reservoir, and its significant ongoing mutations, the H5N1 virus is the world's largest current pandemic threat, and billions of dollars are being spent researching H5N1 and preparing for a potential influenza pandemic.[47] At least 12 companies and 17 governments are developing pre-pandemic influenza vaccines in 28 different clinical trials that, if successful, could turn a deadly pandemic infection into a nondeadly one. Full-scale production of a vaccine that could prevent any illness at all from the strain would require at least three months after the virus's emergence to begin, but it is hoped that vaccine production could increase until one billion doses were produced by one year after the initial identification of the virus.[48]
H5N1 may cause more than one influenza pandemic as it is expected to continue mutating in birds regardless of whether humans develop herd immunity to a future pandemic strain.[49] Influenza pandemics from its genetic offspring may include influenza A virus subtypes other than H5N1.[50] While genetic analysis of the H5N1 virus shows that influenza pandemics from its genetic offspring can easily be far more lethal than the Spanish Flu pandemic[51], planning for a future influenza pandemic is based on what can be done and there is no higher Pandemic Severity Index level than a Category 5 pandemic which, roughly speaking, is any pandemic as bad the Spanish flu or worse; and for which all intervention measures are to be used.[52]
To have a flu pandemic several distinct phases must happen. H5N1's next phase is easy person to person transmission. After that occurs, it is theoretically possible to stop it before it becomes an epidemic, or if that opportunity is missed, to stop the epidemic before it becomes a pandemic. It is widely believed by the experts that it will not be possible to prevent any of these phases from occurring with H5N1, but if we are lucky enough to delay it for a few years, we might come up with a solution such as a influenza vaccine.
H5N1 is just one of the many subtypes of the species Influenza A virus. Any one of them can combine with each other or with different variant genotypes within its own subtype creating new variants, any one of which could become a pandemic strain. We know enough about the genetics to know what strains to fear most (example: only H5 and H7 subtypes are "highly pathogenic") and we know what genetic factors make a flu virus a human virus (i.e. easily passed human to human); so we know H5N1 is the biggest pandemic threat of all the strains in circulation and we know it is only a few antigenic shift mutations or antigenic drift mutations from being an avian influenza virus to being a human flu virus. If it does this it may or may not still be in the H5N1 subtype. Both the drift and the shift can happen in any infected animal and then be passed to a human and spread like wildfire. Possible shift scenarios include the shift occurring in humans, pigs, or cats. To acquire the needed mutation through drift, it simply has to continue being an epidemic in birds long enough for the mutations to occur and then be passed to a human.
Other pandemic threat subtypes
"Human influenza virus" usually refers to those subtypes that spread widely among humans. H1N1, H1N2, and H3N2 are the only known Influenza A virus subtypes currently circulating among humans. [53]
Genetic factors in distinguishing between "human flu viruses" and "avian influenza viruses" include:
- PB2: (RNA polymerase): Amino acid (or residue) position 627 in the PB2 protein encoded by the PB2 RNA gene. Until H5N1, all known avian influenza viruses had a Glu at position 627, while all human influenza viruses had a lysine.
- HA: (hemagglutinin): Avian influenza HA bind alpha 2-3 sialic acid receptors while human influenza HA bind alpha 2-6 sialic acid receptors. Swine influenza viruses have the ability to bind both types of sialic acid receptors.
"About 52 key genetic changes distinguish avian influenza strains from those that spread easily among people, according to researchers in Taiwan, who analyzed the genes of more than 400 A type flu viruses."[54] "How many mutations would make an avian virus capable of infecting humans efficiently, or how many mutations would render an influenza virus a pandemic strain, is difficult to predict. We have examined sequences from the 1918 strain, which is the only pandemic influenza virus that could be entirely derived from avian strains. Of the 52 species-associated positions, 16 have residues typical for human strains; the others remained as avian signatures. The result supports the hypothesis that the 1918 pandemic virus is more closely related to the avian influenza A virus than are other human influenza viruses."[55]
Human flu symptoms usually include fever, cough, sore throat, muscle aches, conjunctivitis and, in severe cases, severe breathing problems and pneumonia that may be fatal. The severity of the infection will depend to a large part on the state of the infected person's immune system and if the victim has been exposed to the strain before, and is therefore partially immune.
Highly pathogenic H5N1 avian influenza in a human is far worse, killing 50% of humans that catch it. In one case, a boy with H5N1 experienced diarrhea followed rapidly by a coma without developing respiratory or flu-like symptoms. [56]
The Influenza A virus subtypes that have been confirmed in humans, ordered by the number of known human pandemic deaths, are:
- H1N1 caused "Spanish Flu"
- H2N2 caused "Asian Flu"
- H3N2 caused "Hong Kong Flu"
- H5N1 is the world's major influenza pandemic threat
- H7N7 has unusual zoonotic potential
- H1N2 is currently endemic in humans and pigs
- H9N2, H7N2, H7N3, H10N7.
- H1N1
- H1N1 is currently endemic in both human and pig populations. A variant of H1N1 was responsible for the Spanish flu pandemic that killed some 50 million to 100 million people worldwide over about a year in 1918 and 1919. [57] Controversy arose in October, 2005, after the H1N1 genome was published in the journal, Science. Many fear that this information could be used for bioterrorism.
- "When he compared the 1918 virus with today's human flu viruses, Dr. Taubenberger noticed that it had alterations in just 25 to 30 of the virus's 4,400 amino acids. Those few changes turned a bird virus into a killer that could spread from person to person." [58]
- H2N2
- The Asian Flu was a pandemic outbreak of H2N2 avian influenza that originated in China in 1957, spread worldwide that same year during which a influenza vaccine was developed, lasted until 1958 and caused between one and four million deaths.
- H3N2
- H3N2 is currently endemic in both human and pig populations. It evolved from H2N2 by antigenic shift and caused the Hong Kong Flu pandemic of 1968 and 1969 that killed up to 750,000. [59] "An early-onset, severe form of influenza A H3N2 made headlines when it claimed the lives of several children in the United States in late 2003." [60]
- The dominant strain of annual flu in January 2006 is H3N2. Measured resistance to the standard antiviral drugs amantadine and rimantadine in H3N2 has increased from 1% in 1994 to 12% in 2003 to 91% in 2005. [61]
- "[C]ontemporary human H3N2 influenza viruses are now endemic in pigs in southern China and can reassort with avian H5N1 viruses in this intermediate host." [62]
- H7N7
- H7N7 has unusual zoonotic potential. In 2003 in Netherlands 89 people were confirmed to have H7N7 influenza virus infection following an outbreak in poultry on several farms. One death was recorded.
- H1N2
- H1N2 is currently endemic in both human and pig populations. The new H1N2 strain appears to have resulted from the reassortment of the genes of the currently circulating influenza H1N1 and H3N2 subtypes. The hemagglutinin protein of the H1N2 virus is similar to that of the currently circulating H1N1 viruses and the neuraminidase protein is similar to that of the current H3N2 viruses.
Strategies to prevent a flu pandemic
This section contains strategies to prevent a flu pandemic by a Council on Foreign Relations panel consisting of:
- James F. Hoge, who is Peter G. Peterson chair, editor, Foreign Affairs
- Nancy E. Roman, who is vice president and director, Washington Program, Council on Foreign Relations
- Rita Colwell, who is chair, Royal Institution World Science Assembly's Pandemic Preparedness Project
- Anthony Fauci, who is director of the National Institute of Allergy and Infectious Diseases at the National Institute of Health
- Laurie Garrett, who is the senior fellow for global health, Council on Foreign Relations
- Michael Osterholm, who is director of the Center for Infectious Disease Research and Policy, University of Minnesota; also, associate director, National Center for Food Protection and Defense, Department of Homeland Defense; also a professor at the University of Minnesota School of Public Health.[63]
If influenza remains an animal problem with limited human-to-human transmission it is not a pandemic, though it continues to pose a risk. To prevent the situation from progressing to a pandemic, the following short-term strategies have been put forward:
- Culling and vaccinating livestock
- Vaccinating poultry workers against common flu
- Limiting travel in areas where the virus is found[63]
The rationale for vaccinating poultry workers against common flu is that it reduces the probability of common influenza virus recombining with avian H5N1 virus to form a pandemic strain. Longer term strategies proposed for regions where highly pathogenic H5N1 is endemic in wild birds have included:
- changing local farming practices to increase farm hygiene and reduce contact between livestock and wild birds.
- altering farming practices in regions where animals live in close, often unsanitary quarters with people, and changing the practices of open-air "wet markets" where birds. A challenge to implementing these measures is widespread poverty, frequently in rural areas, coupled with a reliance upon raising fowl for purposes of subsistence farming or income without measures to prevent propagation of the disease.
- changing local shopping practices from purchase of live fowl to purchase of slaughtered, pre-packaged fowl.
- improving veterinary vaccine availability and cost.[63]
Strategies to slow down a flu pandemic
Vaccines
A vaccine probably would not be available in the initial stages of population infection [64]. A vaccine cannot be developed to protect against a virus which does not exist yet, and the influenza virus capable of generating the next pandemic has not been identified yet. The Avian Flu virus H5N1 has the potential to mutate into a pandemic strain, but so do other types of flu virus. Once a potential virus is identified, it normally takes at least several months before a vaccine becomes widely available, as it must be developed, tested and authorized. The capability to produce vaccines varies widely from country to country; in fact, only 19 countries are listed as "Influenza vaccine manufacturers" according to the World Health Organization.[65] It is estimated that, in a best scenario situation, 750 million doses could be produced each year, whereas it is likely that each individual would need two doses of the vaccine in order to become immuno-competent. Distribution to and inside countries would probably be problematic.[66] Several countries, however, have well-developed plans for producing large quantities of vaccine. For example, Canadian health authorities say that they are developing the capacity to produce 32 million doses within four months, enough vaccine to inoculate every person in the country.[67]
Another concern is whether countries which do not manufacture vaccines themselves, including those where a pandemic strain is likely to originate, will be able to purchase vaccine to protect their population. Cost considerations aside, they fear that the countries with vaccine-manufacturing capability, will reserve production to protect their own populations, and not release vaccines to other countries until their own population is protected. Indonesia has refused to share samples of H5N1 strains which have infected and killed its citizens until it receives assurances that it will have access to vaccines produced with those samples. So far, it has not received those assurances..[68]
There are two serious technical problems associated with the development of a vaccine against H5N1. The first problem is this: seasonal influenza vaccines require a single injection of 15 μg haemagluttinin in order to give protection; H5 seems to evoke only a weak immune response and a large multicentre trial found that two injections of 90 µg H5 given 28 days apart provided protection in only 54% of people Template:Harv. Even if it is considered that 54% is an acceptable level of protection, the world is currently capable of producing only 900 million doses at a strength of 15 μg (assuming that all production were immediately converted to manufacturing H5 vaccine); if two injections of 90 μg are needed then this capacity drops to only 70 million Template:Harv. Trials using adjuvants such as alum or MF59 to try and lower the dose of vaccine are urgently needed. The second problem is this: there are two circulating clades of virus, clade 1 is the virus originally isolated in Vietnam, clade 2 is the virus isolated in Indonesia. Current vaccine research is focused on clade 1 viruses, but the clade 2 virus is antigenically distinct and a clade 1 vaccine will probably not protect against a pandemic caused by clade 2 virus.
Anti-viral drugs
Many nations, as well as the World Health Organization, are working to stockpile anti-viral drugs in preparation for a possible pandemic. Oseltamivir (trade name Tamiflu) is the most commonly sought drug, since it is available in pill form. Zanamivir (trade name Relenza) is also considered for use, but it must be inhaled. Other anti-viral drugs are less likely to be effective against pandemic influenza.
Both Tamiflu and Relenza are in short supply, and production capabilities are limited in the medium term. Some doctors say that co-administration of Tamiflu with probenecid could double supplies [69].
There also is the potential of viruses to evolve drug resistance. Some H5N1-infected persons treated with oseltamivir have developed resistant strains of that virus.
Tamiflu was originally discovered by Gilead Sciences and licensed to Roche for late-phase development and marketing.
Global response
- the establishment and maintenance of high standards of poultry biosecurity
- national veterinary services upgraded to OIE standards
- early detection of H5N1
- early warning system
- adequate surveillance
- rapid reporting
- data-sharing systems
- web-based
- facilitate integrated responses and risk management
- report associated meta-data that allow full analysis of the results
- facilitate timely and effective risk management
- standardization of national-level reporting
- transparent, structured and science-based risk assessments
- better HPAI field surveillance worldwide
- better veterinary services worldwide
- improved, contemporary and international analysis of existing waterbird ringing and count data at the species level and also in months other than January
- better consolidated information on national trade in poultry and poultry products
- rapid reporting and control measures
- data collection on trade issues
- the development of compensation policies for agricultural losses and impacts on protected areas
- effective communication with the media
- the public and policy makers using scientific facts
- additional research on:
- the prevalence of H5N1 in wild bird populations
- existing ringing data to assess migratory systems
- the ecology of the virus in the environment
- natural mortality levels in wild bird populations
- wild bird susceptibility to H5N1
- effective measures to reduce transmission of H5N1 between wild birds and poultry
- build programmes of sustainable financial measures
- support to ensure the sustainability of short-term measures
- development of mechanisms to restructure agricultural production systems with the goal of reducing stresses on ecosystems and risks to human health
- better information on cultural practices that have the potential to either help or hinder the control of H5N1.
- develop and maintain collaborative approaches and partnerships that integrate wetland and wildlife management expertise with expertise on human health and zoonoses
- better integration of existing data on trade in poultry and other birds and the establishment of a web-based clearing-house mechanism on the spread of H5N1.
Source:SCIENTIFIC SEMINAR ON AVIAN INFLUENZA, THE ENVIRONMENT AND MIGRATORY BIRDS ON 10-11 APRIL 2006 published 14 April 2006.[70]
Individual response
(The World Health Organization published a compendium of non-pharmaceutical interventions in November 2005. The following list is not identical to the WHO recommendations.)[71]
- Social distance. By travelling less, working from home or closing schools there is less opportunity for the virus to spread.
- Respiratory hygiene. Populations should be repeatedly informed of the need for "respiratory hygiene" (covering mouth when coughing or sneezing, careful disposal of soiled tissues or other materials).
- Masks. No mask can provide a perfect barrier but products that meet or exceed the NIOSH N95 standard recommended by the World Health Organization are thought to provide good protection. WHO recommends that health-care workers wear N95 masks and that patients wear surgical masks (which may prevent respiratory secretions from becoming airborne).[71] Any mask may be useful to remind the wearer not to touch his face. This can reduce infection due to contact with contaminated surfaces, especially in crowded public places where coughing or sneezing people have no way of washing their hands. The mask itself can become contaminated and must be handled as medical waste when removed.
- Hygiene. Frequent handwashing, especially when there has been contact with other people or with potentially contaminated surfaces can be very helpful. Alcohol-based hand sanitizers also kill both bacteria and viruses.[72]
Phases of an influenza pandemic
The World Health Organization (WHO) has developed a global influenza preparedness plan, which defines the stages of a pandemic, outlines WHO's role and makes recommendations for national measures before and during a pandemic. [73]
Investigations of small clusters of cases are currently ongoing in southeast Asia, particularly Vietnam, to rule out limited human-to-human spread (which would signify Phase 4). The phases are defined as:
Interpandemic period
- Phase 1: Low risk No new influenza virus subtypes dangerous to humans detected in humans or animals.
- Phase 2: New virus A new circulating animal influenza virus subtype poses a substantial risk of human disease but no new influenza virus subtypes have been detected in humans.
Pandemic alert period
- Phase 3: Self limiting Human infection(s) with a new subtype, but no human-to-human spread, or at most rare instances of spread to a close contact. Even without human intervention it would be self limiting among humans.
- Phase 4: Person to person: Small cluster(s) with limited human-to-human transmission but spread is highly localized, suggesting that the virus is not well adapted to humans. An epidemic is possible but has not yet happened.
- Phase 5: Epidemic: Larger cluster(s) but human-to-human spread still localized, suggesting that the virus is becoming increasingly well adapted to humans, but may not yet be fully transmissible (substantial pandemic risk).
Pandemic period
- Phase 6: Pandemic: increased and sustained transmission in general population.
Notes
The distinction between phase 1 and phase 2 is based on the risk of human infection or disease resulting from circulating strains in animals. The distinction is based on various factors and their relative importance according to current scientific knowledge. Factors may include pathogenicity in animals and humans, occurrence in domesticated animals and livestock or only in wildlife, whether the virus is enzootic or epizootic, geographically localized or widespread, and/or other scientific parameters.
The distinction between phase 3, phase 4 and phase 5 is based on an assessment of the risk of a pandemic. Various factors and their relative importance according to current scientific knowledge may be considered. Factors may include rate of transmission, geographical location and spread, severity of illness, presence of genes from human strains (if derived from an animal strain), and/or other scientific parameters.
CIDRAP provides a thoroughgoing overview, which has its roots in materials from the U.S. HHS National Vaccine Program Office. CIDRAP's overview originally set forth a model listing five numbered stages for the pandemic itself, preceded by four additional pre-pandemic stages, each numbered as zero, that overlapped the WHO's first five stages of a pandemic. CIDRAP's overview has since adopted the WHO's 6-stage model. [74]
Preparations for a potential influenza pandemic
According to The New York Times as of March 2006, "governments worldwide have spent billions planning for a potential influenza pandemic: buying medicines, running disaster drills, [and] developing strategies for tighter border controls" due to the H5N1 threat.[75]
"[T]he United States is collaborating closely with eight international organizations, including the World Health Organization (WHO), the Food and Agriculture Organization of the United Nations (FAO), the World Organization for Animal Health (OIE), and 88 foreign governments to address the situation through planning, greater monitoring, and full transparency in reporting and investigating avian influenza occurrences. The United States and these international partners have led global efforts to encourage countries to heighten surveillance for outbreaks in poultry and significant numbers of deaths in migratory birds and to rapidly introduce containment measures. The U.S. Agency for International Development (USAID) and the U.S. Departments of State, Health and Human Services (HHS), and Agriculture (USDA) are coordinating future international response measures on behalf of the White House with departments and agencies across the federal government."[76]
Together steps are being taken to "minimize the risk of further spread in animal populations", "reduce the risk of human infections", and "further support pandemic planning and preparedness".[76]
Ongoing detailed mutually coordinated onsite surveillance and analysis of human and animal H5N1 avian flu outbreaks are being conducted and reported by the USGS National Wildlife Health Center, the Centers for Disease Control and Prevention, the World Health Organization, the European Commission, the National Influenza Centers, and others.[77]
United Nations
In September 2005, David Nabarro, a lead UN health official warned that a bird flu outbreak could happen anytime and had the potential to kill 5-150 million people.[78]
United States
"[E]fforts by the federal government to prepare for pandemic influenza at the national level include a $100 million DHHS initiative in 2003 to build U.S. vaccine production. Several agencies within Department of Health and Human Services (DHHS) — including the Office of the Secretary, the Food and Drug Administration (FDA), CDC, and the National Institute of Allergy and Infectious Diseases (NIAID) — are in the process of working with vaccine manufacturers to facilitate production of pilot vaccine lots for both H5N1 and H9N2 strains as well as contracting for the manufacturing of 2 million doses of an H5N1 vaccine. This H5N1 vaccine production will provide a critical pilot test of the pandemic vaccine system; it will also be used for clinical trials to evaluate dose and immunogenicity and can provide initial vaccine for early use in the event of an emerging pandemic."[79]
On August 26, 2004, Secretary of Health and Human Services, Tommy Thompson released a draft Pandemic Influenza Response and Preparedness Plan[80], which outlined a coordinated national strategy to prepare for and respond to an influenza pandemic. Public comments were accepted for 60 days.
In a speech before the United Nations General Assembly on September 14, 2005, President George W. Bush announced the creation of the International Partnership on Avian and Pandemic Influenza. The Partnership brings together nations and international organizations to improve global readiness by:
- elevating the issue on national agendas;
- coordinating efforts among donor and affected nations;
- mobilizing and leveraging resources;
- increasing transparency in disease reporting and surveillance; and
- building capacity to identify, contain and respond to a pandemic influenza.
On October 5, 2005, Democratic Senators Harry Reid, Evan Bayh, Dick Durbin, Ted Kennedy, Barack Obama, and Tom Harkin introduced the Pandemic Preparedness and Response Act as a proposal to deal with a possible outbreak.[81]
On October 27, 2005, the Department of Health and Human Services awarded a $62.5 million contract to Chiron Corporation to manufacture an avian influenza vaccine designed to protect against the H5N1 influenza virus strain. This followed a previous awarded $100 million contract to sanofi pasteur, the vaccines business of the sanofi-aventis Group, for avian flu vaccine.
In October 2005, President Bush urged bird flu vaccine manufacturers to increase their production.[82]
On November 1, 2005 President Bush unveiled the National Strategy To Safeguard Against The Danger of Pandemic Influenza[83]. He also submitted a request to Congress for $7.1 billion to begin implementing the plan. The request includes $251 million to detect and contain outbreaks before they spread around the world; $2.8 billion to accelerate development of cell-culture technology; $800 million for development of new treatments and vaccines; $1.519 billion for the Departments of Health and Human Services (HHS) and Defense to purchase influenza vaccines; $1.029 billion to stockpile antiviral medications; and $644 million to ensure that all levels of government are prepared to respond to a pandemic outbreak.[84]
On 6 March 2006, Mike Leavitt, Secretary of Health and Human Services, said U.S. health agencies are continuing to develop vaccine alternatives that will protect against the evolving avian influenza virus.[85]
The U.S. government, bracing for the possibility that migrating birds could carry a deadly strain of bird flu to North America, plans to test nearly eight times as many wild birds starting in April 2006 as have been tested in the past decade.[86]
On 8 March 2006, Dr. David Nabarro, senior U.N. coordinator for avian and human influenza, said that given the flight patterns of wild birds that have been spreading avian influenza (bird flu) from Asia to Europe and Africa, birds infected with the H5N1 virus could reach the Americas within the next six to 12 months.[87]
"Jul 5, 2006 (CIDRAP News) – In an update on pandemic influenza preparedness efforts, the federal government said last week it had stockpiled enough vaccine against H5N1 avian influenza virus to inoculate about 4 million people and enough antiviral medication to treat about 6.3 million."[88]
China
In 1982, Kennedy F. Shortridge and Charles Stuart-Harris proposed that China, particularly southern China, is an epicentre for the emergence of pandemic influenza viruses[89]. This hypothesis was based on three observations:
1. The occurrence of a large number of viruses in domestic poultry notably ducks in the region.
2. The dense populations and proximity of humans, poultry and pigs in villages and farms there.
3. The historical records associating China with epidemics and pandemics and, in the last century, the association of southern China with the emergence of the 1957 Asian and 1968 Hong Kong pandemic strains and the re-emergence of the 1977 H1N1 virus [90]. These records have been reinforced by the 1997 H5N1 incident that is considered by some to have been an incipient pandemic and a pandemic averted by the slaughter of poultry across Hong Kong SAR in late 1997.
See also
Further reading
- United States Influenza pandemic plan Draft 2004 Final 2005
- European Commission
- The official U.S. government website for information on pandemic flu and avian flu
- The Flu Wiki dedicated to sharing information about pandemic flu and how to prepare for it
- Nature Magazine: Avian flu special: The flu pandemic: were we ready? Fictional account of flu epidemic from Nature magazine
- World Health Organisation pandemic alert page
- Public Healthy.com - Flu pandemic planning Regularly updated information on flu pandemic preparedness
- California pandemic flu information
- Center for Biosecurity (an independent, nonprofit organization of the University of Pittsburgh Medical Center) page on Avian/Pandemic Influenza
References
- ↑ Klenk; et al. (2008). "Avian Influenza: Molecular Mechanisms of Pathogenesis and Host Range". Animal Viruses: Molecular Biology. Caister Academic Press. ISBN 978-1-904455-22-6.
- ↑ Kawaoka Y (editor). (2006). Influenza Virology: Current Topics. Caister Academic Press. ISBN 978-1-904455-06-6 .
- ↑ CIDRAP article Sanofi tests H7N1 flu vaccine for pandemic readiness published September 19, 2006
- ↑ 4.0 4.1 Merck Manual Home Edition. "Influenza: Viral Infections".
- ↑ Eccles, R (2005). "Understanding the symptoms of the common cold and influenza". Lancet Infect Dis. 5 (11): 718–25. doi:10.1016/S1473-3099(05)70270-X. PMID 16253889.
- ↑ Seasonal Flu vs. Stomach Flu by Kristina Duda, R.N.; accessed March 12, 2007 (Website: "About, Inc., A part of The New York Times Company")
- ↑ Suarez, D (2003). "The effect of various disinfectants on detection of avian influenza virus by real time RT-PCR". Avian Dis. 47 (3 Suppl): 1091–5. PMID 14575118. Unknown parameter
|coauthors=ignored (help) - ↑ Avian Influenza (Bird Flu): Implications for Human Disease. Physical characteristics of influenza A viruses. UMN CIDRAP.
- ↑ Flu viruses 'can live for decades' on ice, NZ Herald, November 30, 2006.
- ↑ "Avian influenza ("bird flu") fact sheet". WHO. February 2006. Retrieved 2006-10-20.
- ↑ WHO position paper: influenza vaccines WHO weekly Epidemiological Record 19 August 2005, vol. 80, 33, pp. 277–288.
- ↑ Villegas, P (1998). "Viral diseases of the respiratory system". Poult Sci. 77 (8): 1143–5. PMID 9706079.
- ↑ Horwood, F. "Pneumococcal and influenza vaccination: current situation and future prospects" (PDF). Thorax. 57 Suppl 2: II24–II30. PMID 12364707. Unknown parameter
|coauthors=ignored (help) - ↑ 14.0 14.1 Harder, T. C. and Werner, O. (2006). "Avian Influenza". In Kamps, B. S., Hoffman, C. and Preiser, W. (ed.). Influenza Report 2006. Paris, France: Flying Publisher. ISBN 3-924774-51-X. Retrieved 2006-04-18.
This e-book is under constant revision and is an excellent guide to Avian Influenza - ↑ See the articles for references that use these names.
- ↑ CIDRAP - Center for Infectious Disease Research And Policy Pandemic Influenza Overview
- ↑ Roos, Robert (February 1, 2007). "HHS ties pandemic mitigation advice to severity". University of Minnesota Center for Infectious Disease Research and Policy (CIDRAP). Retrieved 2007-02-03. Unknown parameter
|coauthors=ignored (help) - ↑ McNeil Jr., Donald (2006-05-02). "Turning to Chickens in Fight With Bird Flu". The New York Times. Retrieved 2006-09-13. Check date values in:
|date=(help)"Desperate times call for desperate measures. In the worst months of the 1918 Spanish flu pandemic, doctors failing to save patients tried all sorts of outlandish 'cures'. Cupping and bleeding made comebacks. Intravenous hydrogen peroxide was tried, sometimes fatally. One doctor injected a mix of blister fluid, morphine, strychnine and caffeine. Typhoid vaccine was given, since it prompts immune reactions; so was quinine, because it breaks malarial fevers." - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 62. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 66. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 59. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 60. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 63. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 61. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ Hilleman M (2002). "Realities and enigmas of human viral influenza: pathogenesis, epidemiology and control". Vaccine. 20 (25–26): 3068–87. doi:10.1016/S0264-410X(02)00254-2. PMID 12163258. Unknown parameter
|month=ignored (help) - ↑ 26.0 26.1 26.2 Taubenberger, J (2006). "1918 Influenza: the mother of all pandemics". Emerg Infect Dis. 12 (1): 15–22. PMID 16494711. Unknown parameter
|coauthors=ignored (help) - ↑ 27.0 27.1 Patterson, KD (1991). "The geography and mortality of the 1918 influenza pandemic". Bull Hist Med. 65 (1): 4–21. PMID 2021692. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ 28.0 28.1 28.2 28.3 Knobler S, Mack A, Mahmoud A, Lemon S (ed.). "1: The Story of Influenza". The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005). Washington, D.C.: The National Academies Press. pp. 60–61.
- ↑ Potter, CW (2006). "A History of Influenza". J Appl Microbiol. 91 (4): 572–579. doi:10.1046/j.1365-2672.2001.01492.x. PMID 11576290. Unknown parameter
|month=ignored (help) - ↑ Simonsen, L (1998). "Pandemic versus epidemic influenza mortality: a pattern of changing age distribution". J Infect Dis. 178 (1): 53–60. PMID 9652423. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ 31.0 31.1 Greene Jeffrey. Moline, Karen. [2006] (2006) The Bird Flu Pandemic. ISBN 0312360568.
- ↑ Goldsmith, Connie. [2007] (2007) Influenza: The Next Pandemic? 21st century publishing. ISBN 0761394575
- ↑ Starling, Arthur. [2006] (2006) Plague, SARS, and the Story of Medicine in Hong Kong. HK University Press. ISBN 9622098053
- ↑ (Detailed chart of its evolution here.)
- ↑ Digitized Editorial Research Reports By Congressional Quarterly, inc 1986
- ↑ International Committee on Taxonomy of Viruses (2002). "46.0.1. Influenzavirus A". Retrieved 2006-04-17.
- ↑
Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. (2004). "Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia". Nature. 430 (6996): 209–213. doi:10.1038/nature02746. PMID doi:[https://doi.org/10.1038%2Fnature02746 10.1038/nature02746 15241415[[Digital object identifier|doi]]:[https://doi.org/10.1038%2Fnature02746 '"`UNIQ--nowiki-00000081-QINU`"']] Check
|pmid=value (help).
This was reprinted in 2005:
Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. (2005). "Today's Pandemic Threat: Genesis of a Highly Pathogenic and Potentially Pandemic H5N1 Influenza Virus in Eastern Asia,". In Forum on Microbial Threats Board on Global Health: Knobler SL, Mack A, Mahmoud A, Lemon SM. (ed.). The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005). Washington DC: The National Academies Press. pp. 116–130. - ↑ "Avian influenza strains are those well adapted to birds"EUROPEAN CENTRE FOR DISEASE PREVENTION AND CONTROL.
- ↑ Chapter Two : Avian Influenza by Timm C. Harder and Ortrud Werner from excellent free on-line Book called Influenza Report 2006 which is a medical textbook that provides a comprehensive overview of epidemic and pandemic influenza.
- ↑ Large-scale sequencing of human influenza reveals the dynamic nature of viral genome evolution Nature magazine presents a summary of what has been discovered in the Influenza Genome Sequencing Project.
- ↑ Full HTML text of Avian Influenza A (H5N1) Infection in Humans by The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 in the September 29, 2005 New England Journal of Medicine
- ↑ The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) Full text of online book by INSTITUTE OF MEDICINE OF THE NATIONAL ACADEMIES
- ↑ Here is the tree showing evolution by antigenic drift since 2002 that created dozens of highly pathogenic varieties of the Z genotype of avian flu virus H5N1, some of which are increasingly adapted to mammals.
- ↑ Evolutionary characterization of the six internal genes of H5N1 human influenza A virus
- ↑ Webster, R. G. and Walker, E. J. (2003). "The world is teetering on the edge of a pandemic that could kill a large fraction of the human population". American Scientist. 91 (2): 122. doi:10.1511/2003.2.122.
- ↑
United Nations (2005-09-29). "Press Conference by UN System Senior Coordinator for Avian, Human Influenza". UN News and Media Division, Department of Public Information, New York. Retrieved 2006-04-17. Check date values in:
|date=(help) - ↑
Rosenthal, E. and Bradsher, K. (2006-03-16). "Is Business Ready for a Flu Pandemic?". The New York Times. Retrieved 2006-04-17. Check date values in:
|date=(help) - ↑ Science and Development Network article Pandemic flu: fighting an enemy that is yet to exist published May 3, 2006.
- ↑ Robert G. Webster, Ph.D., and Elena A. Govorkova, M.D., Ph.D. (November 23, 2006). "H5N1 Influenza — Continuing Evolution and Spread". NEJM. 355 (21): 2174–2177. doi:10.1056/NEJMp068205.
- ↑ CDC ARTICLE 1918 Influenza: the Mother of All Pandemics by Jeffery K. Taubenberger published January 2006
- ↑ Informaworld article Why is the world so poorly prepared for a pandemic of hypervirulent avian influenza? published December 2006
- ↑ Roos, Robert (February 1, 2007). "HHS ties pandemic mitigation advice to severity". University of Minnesota Center for Infectious Disease Research and Policy (CIDRAP). Retrieved 2007-02-03. Unknown parameter
|coauthors=ignored (help) - ↑ CDC Key Facts About Avian Influenza (Bird Flu) and Avian Influenza A (H5N1) Virus
- ↑ Bloomberg News article Scientists Move Closer to Understanding Flu Virus Evolution published August 28, 2006
- ↑ CDC Emerging Infectious Diseases Journal Volume 12, Number 9 – September 2006 - Genomic Signatures of Human versus Avian Influenza A Viruses article by Chen G-W, Chang S-C, Mok C-K, Lo Y-L, Kung Y-N, Huang J-H, et al. posted August 23, 2006
- ↑ New England Journal of Medicine Volume 352:686-691 - February 17, 2005 - Number 7 - Fatal Avian Influenza A (H5N1) in a Child Presenting with Diarrhea Followed by Coma
- ↑ NAP Books National Academies Press Books - The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) - page 7.
- ↑ New York Times Published: November 8, 2005 - Hazard in Hunt for New Flu: Looking for Bugs in All the Wrong Places
- ↑ Detailed chart of its evolution here at PDF called Ecology and Evolution of the Flu
- ↑ NAP Books National Academies Press Books - The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) - page 115 - "There is particular pressure to recognize and heed the lessons of past influenza pandemics in the shadow of the worrisome 2003–2004 flu season. An early-onset, severe form of influenza A H3N2 made headlines when it claimed the lives of several children in the United States in late 2003. As a result, stronger than usual demand for annual flu inactivated vaccine outstripped the vaccine supply, of which 10 to 20 percent typically goes unused. Because statistics on pediatric flu deaths had not been collected previously, it is unknown if the 2003–2004 season witnessed a significant change in mortality patterns."
- ↑ Reason New York Times This Season's Flu Virus Is Resistant to 2 Standard Drugs By Altman Published: January 15, 2006
- ↑ NAP Books National Academies Press Books - The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) - page 126
- ↑ 63.0 63.1 63.2 Council on Foreign Relations (2005-06-16). "The Threat of Global Pandemics". Washington, DC: Council on Foreign Relations. Retrieved 2006-09-13. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ CDC
- ↑ "Influenza vaccine manufacturers". World Health Organization. Retrieved 2006-09-13.
- ↑ "The clock is ticking". Phacilitate. Retrieved 2006-09-13.
- ↑ "Canada to launch avian flu vaccine trial". CTV.ca. 2005-04-20. Retrieved 2006-09-13. Check date values in:
|date=(help) - ↑ [http://www.cidrap.umn.edu/cidrap/content/influenza/panflu/news/
jan2308gao.html "GAO cites barriers to antiviral, vaccine roles in pandemic"] Check
|url=value (help). CIDRAP. Retrieved 2007-02-06. line feed character in|url=at position 64 (help) - ↑ Nature
- ↑ "Avian Influenza & Wild Birds Bulletin, Vol. 123 No. 1". International Institute for Sustainable Development. 2006-04-14. Retrieved 2006-09-13. Check date values in:
|date=(help) - ↑ 71.0 71.1 "Non-pharmaceutical interventions: their role in reducing transmission and spread". World Health Organization. November 2006. Retrieved 2006-09-13.
- ↑ "Stop Germs, Stay Healthy!". King County, Washington web site. Retrieved 2006-09-13.
- ↑ The World Health Organization announces the current phase of the pandemic alert here.
See "Assessing the pandemic threat" at [1]. WHO published a first edition of the Global Influenza Preparedness Plan in 1999, and updated it in April 2005. See [2] and [3] which define the responsibilities of WHO and national authorities in case of an influenza pandemic. This is the first time a pandemic has been anticipated and is being prepared for.
The aims of such plans are, broadly speaking, the following:
- Before a pandemic, attempt to prevent it and prepare for it in case prevention fails.
- If a pandemic does occur, to slow its spread and allow societies to function as normally as possible.
- ↑ CIDRAP's Pandemic Influenza
- ↑ Rosenthal, Elisabeth (2006-03-16). "Is Business Ready for a Flu Pandemic?". The New York Times. Retrieved 2006-09-13. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ 76.0 76.1 "Avian Influenza Response: Key Actions to Date". USAID. Retrieved 2006-09-16.
- ↑ "Monitoring Outbreaks". PandemicFlu.gov web site. Retrieved 2006-09-16.
- ↑ "Bird flu 'could kill 150m people'". BBC News. 2005-09-30. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ U.S. Institute of Medicine (2005). The Threat of Pandemic Influenza: Are We Ready?. National Academies Press. p. 23. ISBN 0-309-09504-2. Unknown parameter
|coauthors=ignored (help) - ↑ "HHS Pandemic Influenza Plan". United States Department of Health and Human Services. 2006-03-20. Check date values in:
|date=(help) - ↑ "Democrats Work to Protect Americans From Avian Flu" (Press release). Senate Democratic Communications Center. 2005-10-5. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ "Bush focuses on bird flu vaccines". BBC News. 2005-10-08. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ "National Strategy for Pandemic Influenza". The White House. 2005-11-01. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ "Bush Outlines $7 Billion Pandemic Flu Preparedness Plan". usinfo.state.gov web site. 2005-11-01. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ "U.S. Health Secretary Says More Bird Flu Vaccines Coming". usinfo.state.gov web site. 2006-03-07. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ Manning, Anita (2006-03-07). "With avian flu spreading, U.S. to expand its testing". USA Today. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ Aita, Judy (2006-03-09). "United Nations Predicts Bird Flu in the Americas within a Year". usinfo.state.gov web site. Retrieved 2006-09-16. Check date values in:
|date=(help) - ↑ "HHS has enough H5N1 vaccine for 4 million people". Center for Infectious Disease Research & Policy. 2006-07-05. Check date values in:
|date=(help) article HHS has enough H5N1 vaccine for 4 million people published July 5, 2006 - ↑ Shortridge, K. F., and Stuart-Harris, C. H. (1982). An influenza epicentre? Lancet 2, 812-813.
- ↑ Potter, C. W. (1998). Chronicle of influenza pandemics. In Nicholson, K. G., Webster, R. G., and Hay, A. J. (eds.) Textbook of influenza. Blackwell Science Ltd. Oxford, UK. pp. 3-18.
Additional Resources
|
Influenza Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Influenza pandemic On the Web |
|
American Roentgen Ray Society Images of Influenza pandemic |
- Pages with reference errors
- CS1 maint: Explicit use of et al.
- Pages with citations using unsupported parameters
- CS1 maint: Multiple names: authors list
- CS1 maint: Extra text: editors list
- CS1 errors: dates
- CS1 maint: Multiple names: editors list
- CS1 errors: PMID
- CS1 errors: invisible characters
- Pages with URL errors
- Pandemics
- Prevention
- Influenza pandemic
- H5N1
- Influenza