Influenza future or investigational therapies
Jump to navigation
Jump to search
|
Influenza Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Influenza future or investigational therapies On the Web |
|
American Roentgen Ray Society Images of Influenza future or investigational therapies |
|
Risk calculators and risk factors for Influenza future or investigational therapies |
For more information about non-human (variant) influenza viruses that may be transmitted to humans, see Zoonotic influenza
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Overview
Other antiviral drugs are being developed to treat influenza infection, such as peramivir. Vaccines are manufactured every year according to the subtype of influenza virus that causes the outbreak in that specific year.
Future or Investigational Therapies
Antiviral Medication
- Peramivir is being developed by BioCryst Pharmaceuticals, but has not yet been approved for sale in the United States.[1]
- Peramivir is a pharmaceutical drug used to treat viral infections.
- Like zanamivir and oseltamivir, peramivir is a neuraminidase inhibitor, acting as a transition-state analogue inhibitor of influenza neuraminidase and thereby preventing new viruses from emerging from infected cells.
- Experimental data indicate that peramivir may have useful activity against many viruses of interest, including H5N1 (avian bird flu) ,hepatitis B, polio, measles and smallpox.
- HHS Secretary Mike Leavitt announced on January 4, 2007 that the Department has awarded a $102.6 million, four-year contract to BioCryst Pharmaceuticals, Inc. for advanced development of their influenza antiviral drug, peramivir.[3]
Vaccine Development
- One important basic research program is the Influenza Genome Sequencing Project, which is creating a library of influenza sequences; this library should help clarify which factors make one strain more lethal than another, which genes most affect immunogenicity, and how the virus evolves over time.[2]
- Research into new vaccines is particularly important: as current vaccines are slow and expensive to produce and must be reformulated every year. The sequencing of the influenza genome and recombinant DNA technology may accelerate the generation of new vaccine strains by allowing scientists to substitute new antigens into a previously-developed vaccine strain.[3]
- New technologies are also being developed to grow virus in cell culture; which promises higher yields, less cost, better quality and surge capacity.[4]
- The potential H5N1 pandemic has motivated a huge increase in flu research. At least 12 companies and 17 governments are developing pre-pandemic influenza vaccines in 28 different clinical trials that, if successful, could turn a deadly pandemic infection into a nondeadly pandemic infection.
- A vaccine that could prevent any illness at all from the not-yet-existing pandemic influenza strain will take at least three months from the virus's emergence until full-scale vaccine production could begin; with vaccine production hoped to increase until one billion doses are produced by one year after the virus is first identified.[5]
- It is estimated that, in a best scenario situation, 750 million doses could be produced each year, whereas it is likely that each individual would need two doses of the vaccine in order to become immuno-competent.[6].
Problems with Vacccine Develpment against H5N1
- There are two serious technical problems associated with the development of a vaccine against H5N1.
- The first problem is that seasonal influenza vaccines require a single injection of 15 μg haemagluttinin in order to give protection; H5 seems to evoke only a weak immune response and a large multicentre trial found that two injections of 90 µg H5 given 28 days apart provided protection in only 54% of people Template:Harv.
- Even if it is considered that 54% is an acceptable level of protection, the world is currently capable of producing only 900 million doses at a strength of 15 μg (assuming that all production were immediately converted to manufacturing H5 vaccine); if two injections of 90 μg are needed then this capacity drops to only 70 million Template:Harv.
- Trials using adjuvants such as alum or MF59 to try and lower the dose of vaccine are urgently needed.
- The second problem is that there are two circulating clades of virus, clade 1 is the virus originally isolated in Vietnam, clade 2 is the virus isolated in Indonesia.
- Current vaccine research is focussed on clade 1 viruses, but the clade 2 virus is antigenically distinct and a clade 1 vaccine will probably not protect against a pandemic caused by clade 2 virus.
Reverse genetics
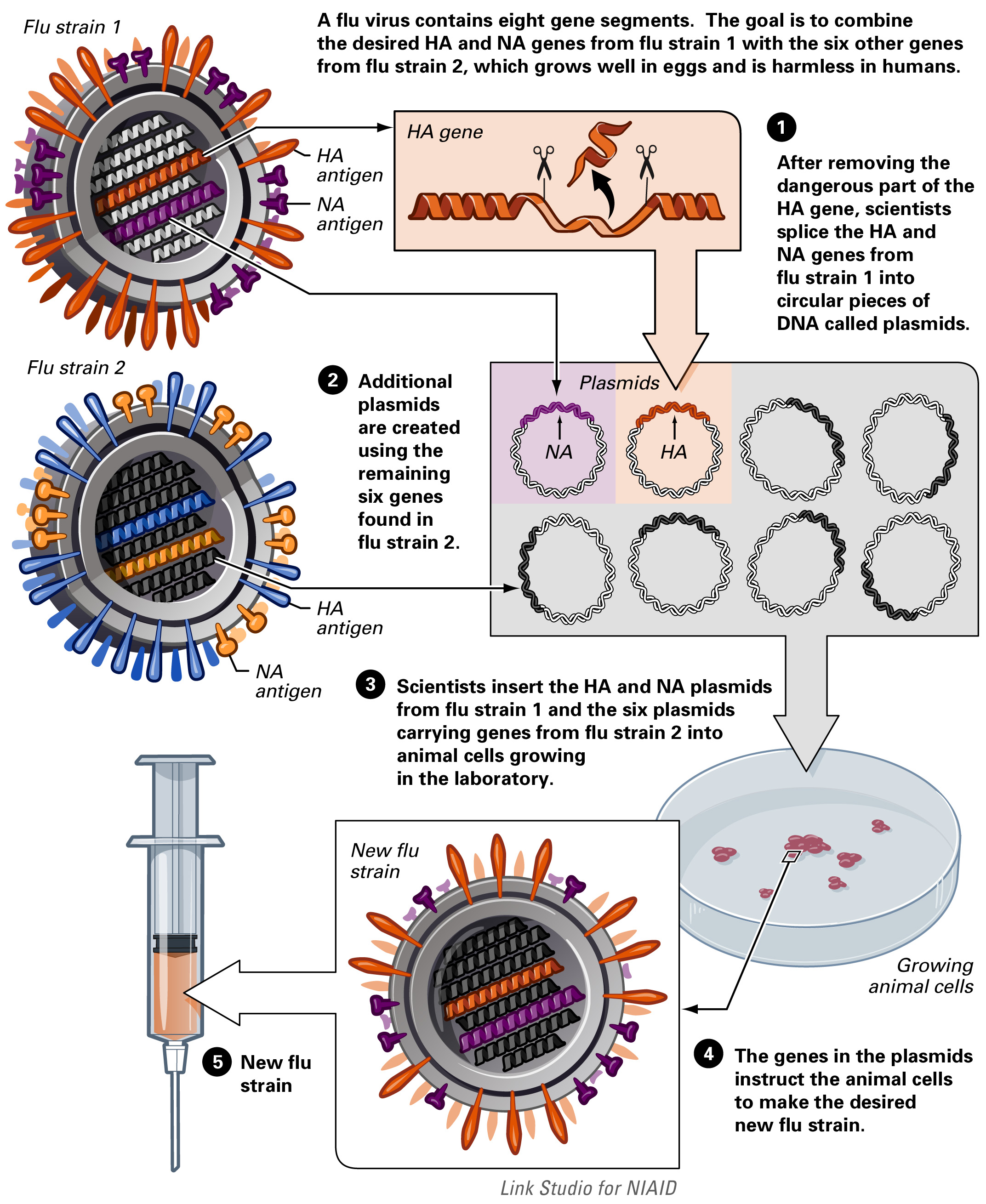
- A technique called reverse genetics allows scientists to manipulate the genomes of influenza viruses and to transfer genes between viral strains.
- The technique allows the rapid generation of seed viruses for vaccine candidates that exactly match the anticipated epidemic strain.
- By removing or modifying certain virulence genes, reverse genetics also can be used to convert highly pathogenic influenza viruses into vaccine candidates that are safer for vaccine manufacturers to handle.
 |
Reassortment
- A flu virus contains eight gene segments. One of the gene segments codes for the surface antigen hemagglutinin (HA), and another codes for the surface antigen neuraminidase (NA).
- Each year, researchers predict which flu strains will be most prevalent and select three—two influenza A strains and an influenza B strain—to be included in that year’s vaccine.
- The goal of reassortment is to combine the desired HA and NA antigens from the target strain (flu strain 1) with genes from a harmless strain that grows well in an egg (flu strain 2).
 |
References
- ↑ "Peramivir Fact Sheet" (pdf). BioCryst Pharmaceuticals Inc. Retrieved 2007-05-25.
- ↑ Influenza A Virus Genome Project at The Institute of Genomic Research. Accessed 19 Oct 06
- ↑ Subbarao K, Katz J. "Influenza vaccines generated by reverse genetics". Curr Top Microbiol Immunol. 283: 313–42. PMID 15298174.
- ↑ Bardiya N, Bae J (2005). "Influenza vaccines: recent advances in production technologies". Appl Microbiol Biotechnol. 67 (3): 299–305. PMID 15660212.
- ↑ Science and Development Network article Pandemic flu: fighting an enemy that is yet to exist published May 3, 2006.
- ↑ phacilitate.co.uk