Eprosartan
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: FETAL TOXICITY
See full prescribing information for complete Boxed Warning.
* When pregnancy is detected, discontinue eprosartan as soon as possible.
|
Overview
Eprosartan is an angiotensin II receptor blocker that is FDA approved for the {{{indicationType}}} of hypertension. There is a Black Box Warning for this drug as shown here. Common adverse reactions include abdominal pain, myalgia, dizziness, upper respiratory infection and fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Hypertension
- May be used alone or in combination with other antihypertensives such as diuretics and calcium channel blockers.
- Discontinuation of treatment with eprosartan does not lead to a rapid rebound increase in blood pressure.
- Initial dosage:
- 600 mg/day, in patients who are not volume depleted.
- May be administered once or twice daily with total daily doses ranging from 400 - 800 mg.
- There is limited experience with doses beyond 800 mg/day.
- If the antihypertensive effect measured at trough using once-daily dosing is inadequate, a twice-a-day regimen at the same total daily dose or an increase in dose may give a more satisfactory response.
- Achievement of maximum blood pressure reduction in most patients may take 2 to 3 weeks.
- Elderly, Hepatically Impaired or Renally Impaired Patients
- No initial dosing adjustment is generally necessary for elderly or hepatically impaired patients or those with renal impairment.
- No initial dosing adjustment is generally necessary in patients with moderate and severe renal impairment, with maximum dose not exceeding 600 mg daily.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of eprosartan in adult patients.
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Label Guideline-Supported Use of eprosartan in children.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of eprosartan in children.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Nonguideline-Supported Use of eprosartan in children.
Contraindications
- Hypersensitivity to eprosartan mesylate or any of its components.
Warnings
|
WARNING: FETAL TOXICITY
See full prescribing information for complete Boxed Warning.
* When pregnancy is detected, discontinue eprosartan as soon as possible.
|
Fetal Toxicity
- Pregnancy Category D
- Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue eprosartan mesylate as soon as possible. These adverse outcomes are usually associated with use of these drugs in the second and third trimester of pregnancy. Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. Appropriate management of maternal hypertension during pregnancy is important to optimize outcomes for both mother and fetus.
- In the unusual case that there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system for a particular patient, apprise the mother of the potential risk to the fetus. Perform serial ultrasound examination to assess the intra-amniotic environment. If oligohydramnios is observed, discontinue eprosartan, unless it is considered lifesaving for the mother. Fetal testing may be appropriate, based on the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. Closely observe infants with histories of in utero exposure to eprosartan for hypotension, oliguria, and hyperkalemia.
- Eprosartan mesylate has been shown to produce maternal and fetal toxicities (maternal and fetal mortality, low maternal body weight and food consumption, resorptions, abortions and litter loss) in pregnant rabbits given oral doses as low as 10 mg eprosartan/kg/day. No maternal or fetal adverse effects were observed at 3 mg/kg/day; this oral dose yielded a systemic exposure (AUC) to unbound eprosartan 0.8 times that achieved in humans given 400 mg b.i.d. No adverse effects on in utero or postnatal development and maturation of offspring were observed when eprosartan mesylate was administered to pregnant rats at oral doses up to 1000 mg eprosartan/kg/day (the 1000 mg eprosartan/kg/day dose in non-pregnant rats yielded systemic exposure to unbound eprosartan approximately 0.6 times the exposure achieved in humans given 400 mg b.i.d.).
Hypotension in Volume- and/or Salt-Depleted Patients
- In patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with diuretics), symptomatic hypotension may occur. These conditions should be corrected prior to administration of eprosartan mesylate, or the treatment should start under close medical supervision. If hypotension occurs, the patient should be placed in the supine position and, if necessary, given an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
Adverse Reactions
Clinical Trials Experience
- Eprosartan has been evaluated for safety in more than 3,300 healthy volunteers and patients worldwide, including more than 1,460 patients treated for more than 6 months, and more than 980 patients treated for 1 year or longer. Eprosartan was well tolerated at doses up to 1200 mg daily. Most adverse events were of mild or moderate severity and did not require discontinuation of therapy. The overall incidence of adverse experiences and the incidences of specific adverse events reported with eprosartan were similar to placebo.
- Adverse experiences were similar in patients regardless of age, gender, or race.
- Adverse experiences were not dose-related.
- In placebo-controlled clinical trials, about 4% of 1,202 patients treated with eprosartan discontinued therapy due to clinical adverse experiences, compared to 6.5% of 352 patients given placebo.
- Adverse events occurring at an Incidence of 1% or more among eprosartan-treated patients.
- The following table lists adverse events that occurred at an incidence of 1% or more among eprosartan-treated patients who participated in placebo-controlled trials of 8 to 13 weeks' duration, using doses of 25 mg to 400 mg twice daily, and 400 mg to 1200 mg once daily.
- The overall incidence of adverse events reported with eprosartan (54.4%) was similar to placebo (52.8%).
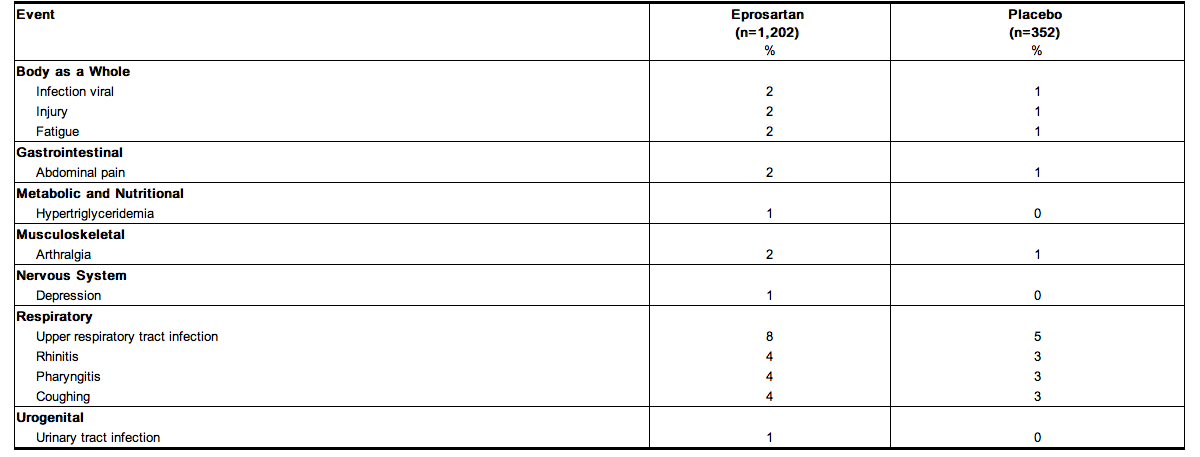
- The following adverse events were also reported at a rate of 1% or greater in patients treated with eprosartan, but were as, or more, frequent in the placebo group:
- Facial edema was reported in 5 patients receiving eprosartan.
- Angioedema has been reported with other angiotensin II antagonists.
- Rare cases of rhabdomyolysis have been reported in patients receiving angiotensin II receptor blockers.
- In addition to the adverse events above, potentially important events that occurred in at least two patients/subjects exposed to eprosartan or other adverse events that occurred in <1% of patients in clinical studies are listed below. It cannot be determined whether events were causally related to eprosartan:
Body as a Whole
- Alcohol intolerance
- Asthenia
- Substernal chest pain
- Peripheral edema
- Fatigue
- Fever
- Hot flushes
- Influenza-like symptoms
- Malaise
- Rigors
- Pain
Cardiovascular
- Angina pectoris
- Bradycardia
- Abnormal ECG,
- Extrasystoles
- Atrial fibrillation
- Hypotension and orthostatic hypotension
- Tachycardia
- Palpitations
Gastrointestinal
- Anorexia
- Constipation
- Dry mouth
- Esophagitis
- Flatulence
- Gastritis
- Gastroenteritis
- Gingivitis
- Nausea
- Periodontitis
- Toothache
- Vomiting
Hematologic
Liver and Biliary
Metabolic and Nutritional
- Increased creatine phosphokinase
- Diabetes mellitus
- Glycosuria
- Gout
- Hypercholesterolemia
- Hyperglycemia
- Hyperkalemia
- Hypokalemia
- Hyponatremia
Musculoskeletal
- Arthritis
- Aggravated arthritis
- Arthrosis
- Skeletal pain
- Tendinitis
- Back pain
Nervous System/Psychiatric
Resistance Mechanism
Respiratory
Skin and Appendages
Special Senses
Urinary
Vascular
Laboratory Test Findings
- In placebo-controlled studies, clinically important changes in standard laboratory parameters were rarely associated with administration of eprosartan. Patients were rarely withdrawn from eprosartan because of laboratory test results.
- Creatinine, Blood Urea Nitrogen
- Minor elevations in creatinine and in BUN occurred in 0.6% and 1.3%, respectively, of patients taking eprosartan and 0.9% and 0.3%, respectively, of patients given placebo in controlled clinical trials. Two patients were withdrawn from clinical trials for elevations in serum creatinine and BUN, and three additional patients were withdrawn for increases in serum creatinine.
- Liver Function Tests
- Minor elevations of ALAT, ASAT, and alkaline phosphatase occurred for comparable percentages of patients taking eprosartan or placebo in controlled clinical trials. An elevated ALAT of >3.5 x ULN occurred in 0.1% of patients taking eprosartan (one patient) and in no patient given placebo in controlled clinical trials. Four patients were withdrawn from clinical trials for an elevation in liver function tests.
- A greater than 20% decrease in hemoglobin was observed in 0.1% of patients taking eprosartan (one patient) and in no patient given placebo in controlled clinical trials. Two patients were withdrawn from clinical trials for anemia.
- Leukopenia
- A WBC count of ≤3.0 x 103/mm3 occurred in 0.3% of patients taking eprosartan and in 0.3% of patients given placebo in controlled clinical trials. One patient was withdrawn from clinical trials for leukopenia.
- Neutropenia
- A neutrophil count of ≤1.5 x 103/mm3 occurred in 1.3% of patients taking eprosartan and in 1.4% of patients given placebo in controlled clinical trials. No patient was withdrawn from any clinical trial for neutropenia.
- A platelet count of ≤100 x 109/L occurred in 0.3% of patients taking eprosartan (one patient) and in no patient given placebo in controlled clinical trials. Four patients receiving eprosartan in clinical trials were withdrawn for thrombocytopenia. In one case, thrombocytopenia was present prior to dosing with eprosartan.
- A potassium value of ≥5.6 mmol/L occurred in 0.9% of patients taking eprosartan and 0.3% of patients given placebo in controlled clinical trials. One patient was withdrawn from clinical trials for hyperkalemia and three for hypokalemia.
Postmarketing Experience
There is limited data regarding adverse reactions reported from post marketing experience.
Drug Interactions
- Digoxin - concomitant administration of eprosartan and digoxin had no effect on single oral-dose digoxin pharmacokinetics.
- Warfarin - concomitant administration of eprosartan and warfarin had no effect on steady-state prothrombin time ratios (INR) in healthy volunteers.
- Glyburide - concomitant administration of eprosartan and glyburide in diabetic patients did not affect 24-hour plasma glucose profiles.
- Ranitidine - eprosartan pharmacokinetics were not affected by concomitant administration of ranitidine.
- Eprosartan did not inhibit human cytochrome P450 enzymes CYP1A, 2A6, 2C9/8, 2C19, 2D6, 2E and 3A in vitro.
- Eprosartan is not metabolized by the cytochrome P450 system.
- Ketoconazole and fluconazole - Eprosartan steady-state concentrations were not affected by concomitant administration of ketoconazole or fluconazole, potent inhibitors of CYP3A and 2C9, respectively.
- Dual Blockade of the Renin-Angiotensin System (RAS):
- Dual blockade of the RAS with angiotensin receptor blockers, ACE inhibitors, or aliskiren is associated with increased risks of hypotension, hyperkalemia, and changes in renal function (including acute renal failure) compared to monotherapy. Closely monitor blood pressure, renal function and electrolytes in patients on eprosartan mesylate and other agents that affect the RAS.
- Do not co-administer aliskiren with eprosartan mesylate in patients with diabetes. Avoid use of aliskiren with eprosartan mesylate in patients with renal impairment (GFR <60 ml/min).
- Eprosartan has been shown to have no effect on the pharmacokinetics of digoxin and the pharmacodynamics of warfarin and glyburide. Thus, no dosing adjustments are necessary during concomitant use with these agents. Because eprosartan is not metabolized by the cytochrome P450 system, inhibitors of CYP450 enzyme would not be expected to affect its metabolism, and ketoconazole and fluconazole, potent inhibitors of CYP3A and 2C9, respectively, have been shown to have no effect on eprosartan pharmacokinetics. Ranitidine also has no effect on eprosartan pharmacokinetics.
- Eprosartan (up to 400 mg b.i.d. or 800 mg q.d.) doses have been safely used concomitantly with a thiazide diuretic (hydrochlorothiazide).
- Eprosartan doses of up to 300 mg b.i.d. have been safely used concomitantly with sustained-release calcium channel blockers (sustained-release nifedipine) with no clinically significant adverse interactions.
- Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 inhibitors (COX-2 Inhibitors):
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, co-administration of NSAIDs, including selective COX-2 inhibitors, with angiotensin II receptor antagonists, including eprosartan, may result in deterioration of renal function, including possible acute renal failure.
- These effects are usually reversible.
- Monitor renal function periodically in patients receiving eprosartan and NSAID therapy.
- The antihypertensive effect of angiotensin II receptor antagonists, including eprosartan may be attenuated by NSAIDs including selective COX-2 inhibitors.
Use in Specific Populations
Pregnancy
- Female patients of childbearing age should be told about the consequences of exposure to eprosartan during pregnancy.
- Discuss treatment options with women planning to become pregnant. Patients should be asked to report pregnancies to their physicians as soon as possible.
- Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue eprosartan mesylate as soon as possible. These adverse outcomes are usually associated with use of these drugs in the second and third trimester of pregnancy. Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. Appropriate management of maternal hypertension during pregnancy is important to optimize outcomes for both mother and fetus.
- In the unusual case that there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system for a particular patient, apprise the mother of the potential risk to the fetus. Perform serial ultrasound examination to assess the intra-amniotic environment. If oligohydramnios is observed, discontinue eprosartan, unless it is considered lifesaving for the mother. Fetal testing may be appropriate, based on the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. Closely observe infants with histories of in utero exposure to eprosartan for hypotension, oliguria, and hyperkalemia.
- Eprosartan mesylate has been shown to produce maternal and fetal toxicities (maternal and fetal mortality, low maternal body weight and food consumption, resorptions, abortions and litter loss) in pregnant rabbits given oral doses as low as 10 mg eprosartan/kg/day. No maternal or fetal adverse effects were observed at 3 mg/kg/day; this oral dose yielded a systemic exposure (AUC) to unbound eprosartan 0.8 times that achieved in humans given 400 mg b.i.d. No adverse effects on in utero or postnatal development and maturation of offspring were observed when eprosartan mesylate was administered to pregnant rats at oral doses up to 1000 mg eprosartan/kg/day (the 1000 mg eprosartan/kg/day dose in non-pregnant rats yielded systemic exposure to unbound eprosartan approximately 0.6 times the exposure achieved in humans given 400 mg b.i.d.).
Pregnancy Category (AUS): D
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of eprosartan in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Eprosartan during labor and delivery.
Nursing Mothers
- Eprosartan is excreted in animal milk; it is not known whether eprosartan is excreted in human milk.
- Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from eprosartan, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Eprosartan pharmacokinetics have not been investigated in patients younger than 18 years of age.
- Neonates with a history of in utero exposure to eprosartan:
- If oliguria or hypotension occurs, direct attention toward support of blood pressure and renal perfusion.
- Exchange transfusions or dialysis may be required as a means of reversing hypotension and/or substituting for disordered renal function.
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- Following single oral dose administration of eprosartan to healthy elderly men (aged 68 to 78 years), AUC, Cmax, and Tmax eprosartan values increased, on average by approximately twofold, compared to healthy young men (aged 20 to 39 years) who received the same dose.
- The extent of plasma protein binding was not influenced by age.
- Of the total number of patients receiving eprosartan in clinical studies, 29% (681 of 2,334) were 65 years and over, while 5% (124 of 2,334) were 75 years and over.
- Based on the pooled data from randomized trials, the decrease in diastolic blood pressure and systolic blood pressure with eprosartan was slightly less in patients ≥65 years of age compared to younger patients.
- In a study of only patients over the age of 65, eprosartan at 200 mg twice daily (and increased optionally up to 300 mg twice daily) decreased diastolic blood pressure on average by 3 mmHg (placebo corrected).
- Adverse experiences were similar in younger and older patients.
Gender
- There was no difference in the pharmacokinetics and plasma protein binding between men and women following single oral dose administration of eprosartan.
Race
- A pooled population pharmacokinetic analysis of 442 Caucasian and 29 non-Caucasian hypertensive patients showed that oral clearance and steady-state volume of distribution were not influenced by race.
Renal Impairment
- As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function have been reported in susceptible individuals treated with angiotensin II antagonists; in some patients, these changes in renal function were reversible upon discontinuation of therapy.
- In patients whose renal function may depend on the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure), treatment with angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists has been associated with oliguria and/or progressive azotemia and (rarely) with acute renal failure and/or death. Eprosartan mesylate would be expected to behave similarly.
- In studies of ACE inhibitors in patients with unilateral or bilateral renal artery stenosis, increases in serum creatinine or BUN have been reported. Similar effects have been reported with angiotensin II antagonists; in some patients, these effects were reversible upon discontinuation of therapy.
Hepatic Impairment
- Eprosartan AUC (but not Cmax) values increased, on average, by approximately 40% in men with decreased hepatic function compared to healthy men after a single 100 mg oral dose of eprosartan. Hepatic disease was defined as a documented clinical history of chronic hepatic abnormality diagnosed by liver biopsy, liver/spleen scan or clinical laboratory tests.
- The extent of eprosartan plasma protein binding was not influenced by hepatic dysfunction.
- No dosage adjustment is necessary for patients with hepatic impairment.
Females of Reproductive Potential and Males
- Eprosartan mesylate was not carcinogenic in dietary restricted rats or ad libitum fed mice dosed at 600 mg and 2000 mg eprosartan/kg/day, respectively, for up to 2 years. In male and female rats, the systemic exposure (AUC) to unbound eprosartan at the dose evaluated was only approximately 20% of the exposure achieved in humans given 400 mg b.i.d. In mice, the systemic exposure (AUC) to unbound eprosartan was approximately 25 times the exposure achieved in humans given 400 mg b.i.d.
- Eprosartan mesylate was not mutagenic in vitro in bacteria or mammalian cells (mouse lymphoma assay). Eprosartan mesylate also did not cause structural chromosomal damage in vivo (mouse micronucleus assay).
- In human peripheral lymphocytes in vitro , eprosartan mesylate was equivocal for clastogenicity with metabolic activation, and was negative without metabolic activation. In the same assay, eprosartan mesylate was positive for polyploidy with metabolic activation and equivocal for polyploidy without metabolic activation.
- Eprosartan mesylate had no adverse effects on the reproductive performance of male or female rats at oral doses up to 1000 mg eprosartan/kg/day. This dose provided systemic exposure (AUC) to unbound eprosartan approximately 0.6 times the exposure achieved in humans given 400 mg b.i.d.
Immunocompromised Patients
There is no FDA guidance one the use of Eprosartan in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
Monitoring
Hypertension
- Dual Blockade of the Renin-Angiotensin System:
- Monitor blood pressure, renal function and electrolytes in patients on eprosartan and other agents that affect the RAS.
- Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 inhibitors (COX-2 Inhibitors)
- Monitor renal function periodically in patients receiving eprosartan and NSAID therapy.
IV Compatibility
There is limited information regarding the compatibility of eprosartan and IV administrations.
Overdosage
- Limited data are available regarding overdosage.
- Appropriate symptomatic and supportive therapy should be given if overdosage should occur.
- There was no mortality in rats and mice receiving oral doses of up to 3000 mg eprosartan/kg and in dogs receiving oral doses of up to 1000 mg eprosartan/kg.
Pharmacology
| |
Eprosartan
| |
| Systematic (IUPAC) name | |
| 4-({2-Butyl-5-[2-carboxy-2-(thiophen-2-ylmethyl)eth-1-en-1-yl]-1H-imidazol-1-yl}methyl)benzoic acid | |
| Identifiers | |
| CAS number | |
| ATC code | C09 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | Eprosartan mesylate: 520.625 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 15% (Eprosartan mesylate) |
| Metabolism | not metabolized |
| Half life | 5 to 9 hours |
| Excretion | Renal 10%, biliary 90% |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | Oral |
Mechanism of Action
- Angiotensin II (formed from angiotensin I in a reaction catalyzed by angiotensin-converting enzyme [kininase II]), a potent vasoconstrictor, is the principal pressor agent of the renin-angiotensin system. Angiotensin II also stimulates aldosterone synthesis and secretion by the adrenal cortex, cardiac contraction, renal resorption of sodium, activity of the sympathetic nervous system, and smooth muscle cell growth.
- Eprosartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT1 receptor found in many tissues (e.g., vascular smooth muscle, adrenal gland). There is also an AT2 receptor found in many tissues but it is not known to be associated with cardiovascular homeostasis.
- Eprosartan does not exhibit any partial agonist activity at the AT1 receptor. Its affinity for the AT1 receptor is 1,000 times greater than for the AT2 receptor. In vitro binding studies indicate that eprosartan is a reversible, competitive inhibitor of the AT1 receptor.
- Blockade of the AT1 receptor removes the negative feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and circulating angiotensin II do not overcome the effect of eprosartan on blood pressure.
- Eprosartan mesylate does not inhibit kininase II, the enzyme that converts angiotensin I to angiotensin II and degrades bradykinin; whether this has clinical relevance is not known. It does not bind to or block other hormone receptors or ion channels known to be important in cardiovascular regulation.
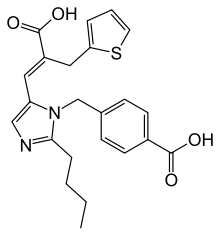
Structure
- Eprosartan mesylate is a non-biphenyl non-tetrazole angiotensin II receptor (AT1) antagonist. A selective non-peptide molecule, eprosartan mesylate is chemically described as the monomethanesulfonate of (E )-2-butyl-1-(p-carboxybenzyl)-α-2-thienylmethylimid-azole-5-acrylic acid.
- Its empirical formula is C23H24N2O4S•CH4O3S and molecular weight is 520.625. Its structural formula is:
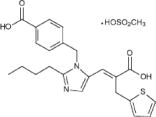
- Eprosartan mesylate is a white to off-white free-flowing crystalline powder that is insoluble in water, freely soluble in ethanol, and melts between 248°C and 250°C.
- Eprosartan mesylate is available as aqueous film-coated tablets containing eprosartan mesylate equivalent to 400 mg or 600 mg eprosartan zwitterion (pink, oval, non-scored tablets or white, non-scored, capsule-shaped tablets, respectively).
- Inactive Ingredients:
- The 400 mg tablet contains the following: croscarmellose sodium, hypromellose, iron oxide red, iron oxide yellow, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate 80, pregelatinized starch, and titanium dioxide. The 600 mg tablet contains crospovidone, hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate 80, pregelatinized starch, and titanium dioxide.
Pharmacodynamics
- Eprosartan inhibits the pharmacologic effects of angiotensin II infusions in healthy adult men. Single oral doses of eprosartan from 10 mg to 400 mg have been shown to inhibit the vasopressor, renal vasoconstrictive and aldosterone secretory effects of infused angiotensin II with complete inhibition evident at doses of 350 mg and above. Eprosartan inhibits the pressor effects of angiotensin II infusions. A single oral dose of 350 mg of eprosartan inhibits pressor effects by approximately 100% at peak, with approximately 30% inhibition persisting for 24 hours. The absence of angiotensin II AT1 agonist activity has been demonstrated in healthy adult men. In hypertensive patients treated chronically with eprosartan, there was a twofold rise in angiotensin II plasma concentration and a twofold rise in plasma renin activity, while plasma aldosterone levels remained unchanged. Serum potassium levels also remained unchanged in these patients.
- Achievement of maximal blood pressure response to a given dose in most patients may take 2 to 3 weeks of treatment. Onset of blood pressure reduction is seen within 1 to 2 hours of dosing with few instances of orthostatic hypotension. Blood pressure control is maintained with once- or twice-daily dosing over a 24-hour period. Discontinuing treatment with eprosartan does not lead to a rapid rebound increase in blood pressure.
- There was no change in mean heart rate in patients treated with eprosartan in controlled clinical trials.
- Eprosartan increases mean effective renal plasma flow (ERPF) in salt-replete and salt-restricted normal subjects. A dose-related increase in ERPF of 25% to 30% occurred in salt-restricted normal subjects, with the effect plateauing between the 200 mg and 400 mg doses. There was no change in ERPF in hypertensive patients and patients with renal insufficiency on normal salt diets. Eprosartan did not reduce glomerular filtration rate in patients with renal insufficiency or in patients hypertension, after 7 days and 28 days of dosing, respectively. In hypertensive patients and patients with chronic renal insufficiency, eprosartan did not change fractional excretion of sodium and potassium.
- Eprosartan (1200 mg once daily for 7 days or 300 mg twice daily for 28 days) had no effect on the excretion of uric acid in healthy men, patients with essential hypertension or those with varying degrees of renal insufficiency.
- There were no effects on mean levels of fasting triglycerides, total cholesterol, HDL cholesterol, LDL cholesterol or fasting glucose.
Pharmacokinetics
- General:
- Absolute bioavailability following a single 300 mg oral dose of eprosartan is approximately 13%.
- Eprosartan plasma concentrations peak at 1 to 2 hours after an oral dose in the fasted state.
- Administering eprosartan with food delays absorption, and causes variable changes (<25%) in Cmax and AUC values which do not appear clinically important. Plasma concentrations of eprosartan increase in a slightly less than dose-proportional manner over the 100 mg to 800 mg dose range. The mean terminal elimination half-life of eprosartan following multiple oral doses of 600 mg was approximately 20 hours.
- Eprosartan does not significantly accumulate with chronic use.
- Metabolism and Excretion:
- Eprosartan is eliminated by biliary and renal excretion, primarily as unchanged compound.
- Less than 2% of an oral dose is excreted in the urine as a glucuronide.
- There are no active metabolites following oral and intravenous dosing with [14C] eprosartan in human subjects.
- Eprosartan was the only drug-related compound found in the plasma and feces. Following intravenous [14C] eprosartan, about 61% of the material is recovered in the feces and about 37% in the urine. Following an oral dose of [14C] eprosartan, about 90% is recovered in the feces and about 7% in the urine. Approximately 20% of the radioactivity excreted in the urine was an acyl glucuronide of eprosartan with the remaining 80% being unchanged eprosartan.
- Distribution:
- Plasma protein binding of eprosartan is high (approximately 98%) and constant over the concentration range achieved with therapeutic doses.
- The pooled population pharmacokinetic analysis from two Phase 3 trials of 299 men and 172 women with mild to moderate hypertension (aged 20 to 93 years) showed that eprosartan exhibited a population mean oral clearance (CL/F) for an average 60-year-old patient of 48.5 L/hr. The population mean steady-state volume of distribution (Vss/F) was 308 L. Eprosartan pharmacokinetics were not influenced by weight, race, gender or severity of hypertension at baseline. Oral clearance was shown to be a linear function of age with CL/F decreasing 0.62 L/hr for every year increase.
Nonclinical Toxicology
There is limited information regarding the nonclinical toxicology of eprosartan.
Clinical Studies
- The safety and efficacy of eprosartan mesylate have been evaluated in controlled clinical trials worldwide that enrolled predominantly hypertensive patients with sitting DBP ranging from 95 mmHg to ≤115 mmHg.
- There is also some experience with use of eprosartan together with other antihypertensive drugs in more severe hypertension.
- The antihypertensive effects of eprosartan mesylate were demonstrated principally in five placebo-controlled trials (4 to 13 weeks' duration) including dosages of 400 mg to 1200 mg given once daily (two studies), 25 mg to 400 mg twice daily (two studies), and one study comparing total daily doses of 400 mg to 800 mg given once daily or twice daily. The five studies included 1,111 patients randomized to eprosartan and 395 patients randomized to placebo. The studies showed dose-related antihypertensive responses.
- At study endpoint, patients treated with eprosartan mesylate at doses of 600 mg to 1200 mg given once daily experienced significant decreases in sitting systolic and diastolic blood pressure at trough, with differences from placebo of approximately 5-10/3-6 mmHg. Limited experience is available with the dose of 1200 mg administered once daily. In a direct comparison of 200 mg to 400 mg b.i.d. with 400 mg to 800 mg q.d. of eprosartan mesylate, effects at trough were similar. Patients treated with eprosartan mesylate at doses of 200 mg to 400 mg given twice daily experienced significant decreases in sitting systolic and diastolic blood pressure at trough, with differences from placebo of approximately 7-10/4-6 mmHg.
- Peak (1 to 3 hours) effects were uniformly, but moderately, larger than trough effects with b.i.d. dosing, with the trough-to-peak ratio for diastolic blood pressure 65% to 80%. In the once-daily dose-response study, trough-to-peak responses of ≤50% were observed at some doses (including 1200 mg), suggesting attenuation of effect at the end of the dosing interval.
The antihypertensive effect of eprosartan mesylate was similar in men and women, but was somewhat smaller in patients over 65. There were too few black subjects to determine whether their response was similar to Caucasians. In general, blacks (usually a low renin population) have had smaller responses to ACE inhibitors and angiotensin II inhibitors than caucasian populations.
- Angiotensin-converting enzyme inhibitor-induced cough (a dry, persistent cough) can lead to discontinuation of ACE inhibitor therapy. In one study, patients who had previously coughed while taking an ACE inhibitor were treated with eprosartan, an ACE inhibitor (enalapril) or placebo for six weeks. The incidence of dry, persistent cough was 2.2% on eprosartan, 4.4% on placebo, and 20.5% on the ACE inhibitor; p=0.008 for the comparison of eprosartan with enalapril. In a second study comparing the incidence of cough in 259 patients treated with eprosartan to 261 patients treated with the ACE inhibitor enalapril, the incidence of dry, persistent cough in eprosartan-treated patients (1.5%) was significantly lower (p=0.018) than that observed in patients treated with the ACE inhibitor (5.4%). In addition, analysis of overall data from six double-blind clinical trials involving 1,554 patients showed an incidence of spontaneously reported cough in patients treated with eprosartan of 3.5%, similar to placebo (2.6%).
How Supplied
- TEVETEN® is available as aqueous film-coated tablets as follows:
- 400 mg pink, non-scored, oval tablets, debossed with “5044” on one side.
- NDC 0074–3025–11 (bottles of 100)
- 600 mg white, non-scored, capsule-shaped tablets, debossed with “5046” on one side.
- NDC 0074–3040–11 (bottles of 100)
Storage
Store at controlled room temperature 20 to 25°C (68 to 77°F) [see USP Controlled Room Temperature].
Images
Drug Images
{{#ask: Page Name::Eprosartan |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Eprosartan |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Pregnancy
- Female patients of childbearing age should be told about the consequences of exposure to eprosartan mesylate during pregnancy.
- Discuss treatment options with women planning to become pregnant.
- Patients should be asked to report pregnancies to their physicians as soon as possible.
Precautions with Alcohol
- Some patients previously exposed to eprosartan showed signs of alcohol intolerance, however, it is not possible to confirm if eprosartan was directly involved in the adverse reaction.
Brand Names
Teveten®
Look-Alike Drug Names
N/A
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Eprosartan |Pill Name=Eprosartan pill.jpg |Drug Name=Eprosartan mesylate |Pill Ingred=crospovidone, lactose monohydrate, magnesium stearate, cellulose, microcrystalline, polysorbate 80, starch, corn, titanium dioxide and polyethylene glycols|+sep=; |Pill Imprint=SOLVAY;5046 |Pill Dosage=600 mg |Pill Color=White|+sep=; |Pill Shape=Oval |Pill Size (mm)=20 |Pill Scoring=1 |Pill Image= |Drug Author=Abbott Laboratories |NDC=00074-3040--11
}}
{{#subobject:
|Label Page=Eprosartan |Label Name=TEVETEN 1.jpg
}}
{{#subobject:
|Label Page=Eprosartan |Label Name=TEVETEN copy.jpg
}}
{{#subobject:
|Label Page=Eprosartan |Label Name=TEVETEN copy 2.jpg
}}