Bland-White-Garland syndrome
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Abnormal septation of the conotruncus into the aorta and pulmonary artery; Anomalous origin of left coronary artery from pulmonary artery; ALCAPA; BWG; Persistence of the pulmonary buds together with involution of the aortic buds that form the coronary arteries
Overview
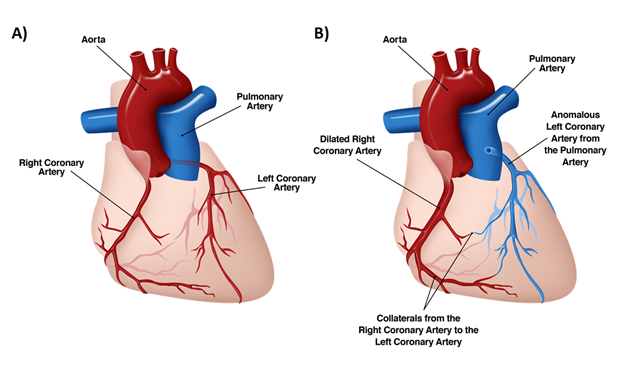
This syndrome is a rare congenital abnormality of coronary artery and refers to origin of the left coronary artery from the pulmonary artery. Normally both right and left coronary artery originate from the aorta. Classified under the Anomalous Pulmonary Origin of Coronaries(APOC) by the Society of Thoracic Surgeons-Congenital Heart Surgery database it is amongst the 3 most common clinically significant congenital coronary anomalies treated surgically, the other two being Anomalous Coronary Origin of Coronaries(AAOC) and Coronary Arteriovenous fistula(CAVF)[1]
Historical Perspective
The Bland-White-Garland Syndrome was first described as an autopsy report by a Russian pathologist Aleksei Ivanovich Abrikossoff in 1911. There was no any clinical correlation in this report. The subject of his report was “a left ventricular aneurysm with abnormal originated left coronary artery from pulmonary artery in a five months old child”.
The first comprehensive clinical description of this congenital syndrome was published in 1933 by three American physicians; Edward Bland, Paul Dudley White and Joseph Garland.
An American surgeon, David Coston Sabiston described the most important diagnostic and hemodynamic components of this syndrome in 1960. His findings and hemodynamic descriptions became a cornerstone of the diagnosis and treatment in this syndrome.
In 1962, Fontana and Edwards reported a series of 58 postmortem specimens that demonstrated that most patients had died at a young age.
Anatomy
Developmentally, failure of the normal connection of the left coronary artery bud to the aorta results in an abnormal connection to the pulmonary artery. The abnormal origin can be situated in the main pulmonary artery or proximal branches. Associated abnormalities are rare but important to recognize because lowering of the pulmonary artery pressure by ligation of patent ductus arteriosus or closure of a ventricular septal defect can be fatal if the Bland-White-Garland Syndrome or ALCAPA is not noted.
Other extremely rare variations of anomalous origin of the coronary arteries listed below:
- The left anterior descending artery or left circumflex branches originate from the main pulmonary artery,
- The right coronary artery originates from main pulmonary trunk; more often this is an incidental autopsy finding,
- Both of the right and left coronary arteries originate from the pulmonary artery; this circumstance is not compatible with survival.
Classification of Bland-White-Garland Syndrome (ALCAPA, BWG Syndrome)
Infantile Syndrome Form
This is the most common form. Patient develops acute episode of respiratory insufficiency, cyanosis, irritability and profuse sweating. Most patients die within two years of life.
Mitral Valve Regurgitation Form
This form is characterized by mitral regurgitation, congestive heart failure, cardiomegaly and atrial arrythmias in children, adolescent and adults.
Continuous Murmur Syndrome Form
This form occurs in asymptomatic patients with angina pectoris. A continuous heart murmur results from great volume of blood flowing through collateral branches between left and right coronary arteries.
Sudden Death in Adolescents or Adults Form
Most of the patients are asymptomatic, but some may experience exertional angina, cardiac arrhythmias and sudden death.
Pathophysiology
Anomalous origin of the left coronary artery from pulmonary artery (ALCAPA or Bland-White-Garland Syndrome) is not considered as an inheritable congenital cardiac defect and there are no known additional risk factors regarding the occurrence of this syndrome. It has no any known relation with any non-cardiac and/or genetic disorders.In utero exposure to teratogens, chromosomal abnormalities or other risk factors are unrelated to anomalous origin of the left coronary artery arising from the pulmonary artery (Bland-White-Garland Syndrome).
The clinical expression of ALCAPA (anomalous origin of left coronary artery from pulmonary artery) or Bland-White-Garland Syndrome results from morphological changes, as well as functional and dynamic alterations in pulmonary circulation that occur immediately after birth.
Fetal Stage
- By the reason of two favorable fetal physiologic mechanisms as relatively equivalent oxygen concentrations in coronary and pulmonary vascular bed (due to parallel circulations) and equivalent pressures in the main pulmonary artery and aorta (secondary to a non restrictive patent ductus arteriosus), symptoms of BGW syndrome do not present during the prenatal term.Therefore myocardial perfusion is in the normal range and no stimulus exists for collateral vessel formation between the right and left coronary artery systems.
Neonatal Stage
- In a newborn; the resistance in pulmonary artery is so high it permits antegrade blood flow to left coronary artery (LCA), which perfuses the entire left ventricle.
- As pulmonary vascular resistance and pulmonary artery pressure gradually reduce in following days and weeks, and flow from pulmonary artery fails to supply left coronary artery, thus collaterals from right coronary artery to the left one becomes the only resources of left ventricular perfusion.However,this results in the left ventricular myocardium being perfused by relatively desaturated blood flow under low pressure, leading to myocardial ischemia.
- Frequently this causes papillary muscle dysfunction and therefore variable degrees of mitral insufficiency.
- The improvements in collateral circulation between right and left coronary arteries and markedly reduced pulmonary vascular resistance results in coronary steal phenomenon.
- Instead of supplying left ventricular myocardium, oxygenated blood from left coronary artery (which has acquired from the right coronary artery through collateral vessels) goes to pulmonary trunk and results in significant myocardial perfusion failure. Consequently, the combination of left ventricular dysfunction and significant mitral valve insufficiency leads to congestive heart failure (CHF).
- Prolonged myocardial ischemia results in the development of patchy area of fibrosis in the left myocardium leading to ventricular dysfunction, large ventricular aneurysms or mitral regurgitation.
Adult Stage
Although, insufficient collateral development may result decompensation and death in this stage, improvement of coronary collateral circulation supplies left ventricular myocardium and may help to survive.[2] [3] [4].
- Factors influencing survival into adulthood include [5]
- Increased physical or mental stress in this group may exacerbate the coronary steal phenomena from LCA to Pulmonary artery leading to ventricular arrhythmias and death.[8] [9]
Bland-White-Garland Syndrome (ALCAPA) is usually an isolated congenital cardiac abnormality but rarely has been reported with occurrence of patent ductus arteriosus (PDA), ventricular septal defect (VSD), tetralogy of Fallot, and coarctation of the aorta.
Genetics
Bland-White-Garland Syndrome is not considered as an inheritable congenital cardiac defect.
Epidemiology and Demographics
The incidence of this rare, congenital cardiac anomaly does not vary geographically, and has no inheritance. Occurrence is generally similar between males and females. There is no race difference in its prevalence. The frequency of Bland-White-Garland Syndrome is approximately 0.25 - 0.5% of all congenital heart diseases. It occurs 1/300,000 births.
In adults it is twice as common in females than males [10]
Differentiating the Disorder from other Diseases
One key disorder to distinguish ALCAPA from is dilated cardiomyopathy. This disorder also presents with moderate to severe congestive heart failure,cardiomegaly on chest roentgenogram, ischemic signs on the electrocardiogram and a systolic murmur of mitral insufficiency.
Johnsrude and associates defined electrocardiographic criteria distinguishing ALCAPA from myocarditis or dilated cardiomyopathy. They found a Q wave depth of >3 mm, a Q wave width >30 ms, and a QR pattern in at least one of leads I, aVL, V5–V7, to be present in 100% of the ECGs of patients with ALCAPA. The absence of Q waves in leads II, III, and aVF was also universal.
In a model relying on the Q wave depth in aVL, the ST segment amplitude in aVL, and the Q wave width in lead I, ALCAPA was correctly diagnosed in 98% of their patients, conferring a sensitivity of 100%, a specificity of 96%, and a positive predictive value of 85%.
Other disorder in the differential diagnosis include:
Diagnosis
In initial period, there is a transient myocardial ischemia. It depends on myocardial oxygen demands and occurs during feeding and/or crying. Further increase in myocardial oxygen consumption may lead to myocardial infarction. Frequently this causes papillary muscle dysfunction and therefore variable degrees of mitral insufficiency and congestive heart failure (CHF)
The rapidity of this functional sequence led investigators to classify patients on the basis of their respective survival patterns into two subsets of coronary circulations: the infantile or the Adult type.
- The infantile type of circulation has little or no coronary collateral development, a condition leading to the early onset of severe myocardial ischemia, left ventricular dysfunction and dilatation, and mitral regurgitation due to papillary muscle ischemia, dilatation of the annulus or both.
- The Adult type has well developed collateral circulations between the RCA and LCA.Symptoms often occur at times of increased myocardial oxygen demand.
In general, approximately 85% of patients present with clinical symptoms of CHF within the first 1-2 months of life. In unusual cases, the clinical presentation with symptoms of myocardial ischemia may be delayed into early childhood.
History and Symptoms
Infants usually do well for a short period then gradually become restless and irritable. Characteristic symptoms include
- Diaphoresis after breast feeding
- Failure to thrive.
- Irritability
- Infantile colic (The moderate chest pain and discomfort due to inadequate myocardial perfusion frequently misinterpreted as colic)
- Tachypnea
A subset of patient with good collaterals might be asymptomatic into adulthood.ALCAPA often manifests in Adult population as
- Acute myocardial Infarction
- congestive heart failure (CHF) (due to combination of mitral valve regurgitation and left ventricular dysfunction)
- Malignant arrhythmias
- Sudden cardiac death
Physical Examination
Appearance of the Patient
Pallor is common
Heart
A systolic (due to mitral valve regurgitation) murmur and a diastolic rumble (relative mitral valve stenosis) may occur. Rarely, a soft continuous murmur (coronary artery fistula or a small patent ductus arteriosus) might be detected at upper left sternal border. The left ventricular apex may palpable (usually shifted to lateral side and to inferior). There is a splitting of second heart sound (a narrow splitting) and pulmonary component is getting harder in patient with pulmonary artery hypertension (PAH).
Lungs
Findings of Congestive Heart failure may occur.
Abdomen
Hepatomegaly is present if congestive heart failure occurs.
Electrolyte and Biomarker Studies
Blood tests have not definitive role in the diagnosis of Bland-White-Garland Syndrome (anomalous origin of the left coronary artery arising from the pulmonary artery). Elevation of cardiac enzymes can only be used in diagnosis of periprocedural myocardial injury or infarction.
Chest X Ray
Although, chest radiography is not diagnostic tool for ALCAPA, it usually shows cardiomegaly with or without pulmonary venous congestion.
Electrocardiography
There is an old anterolateral myocardial infarction pattern with abnormal deep (>3 mm) and wide (>30 msec) Q waves in leads I, aVL, V5, and V6. Q waves are absent in leads II, III, and aVF. There is poor R wave progression in precordial leads, with a quick qR pattern.
The electrocardiogram (ECG) may detect ventricular repolarization abnormalities (ST segment depression or elevation) in both inferior and lateral area.
The QRS axis is typically in normal range. Undetermined axis may seen in some cases.
Echocardiography
Two dimensional echocardiography with Doppler color flow mapping is helpful for diagnosis and may replace the need for cardiac catheterization and angiography.
- Echo without Doppler may identify abnormal origin of the left coronary artery from the main pulmonary artery.
- Color flow velocity mapping may be a helpful diagnostic tool. It shows retrograde flow (from left coronary artery) to pulmonary trunk. This finding is important to distinguish from patent ductus arteriosus.
- In unusual circumstances, echocardiographic examinations and therefore diagnosis is difficult if the coronary artery arise from a pulmonary artery branch.
- Doppler mapping of an abnormal color flow jet will usually identify abnormal retrograde flow within the main pulmonary artery in both late systole and diastole.
- The mapping image is partially dependent on pulmonary artery pressure. The presence of retrograde flow is dependent on collateral development. If collaterals are not present this finding may be absent.
- Abnormal dilation of proximal right coronary artery; when present, it reflects extensive collateral development in patients in infancy or in childhood.
- Abnormal "brightness" of left ventricular papillary muscles not sensitive but highly specific.
- Variable degrees of mitral valve regurgitation, left ventricular dysfunction, and wall motion abnormalities may be identified.
Chang and Allada described a scoring system based on logistic regression which allowed them to distinguish between dilated cardiomyopathy and Bland-White-Garland Syndrome = ALCAPA.
Diagnosis of Bland-White-Garland Syndrome = ALCAPA was achieved with 100% sensitivity and 91% specificity; when including QT patterns in aVL, echocardiographic evidence of a right coronary artery (RCA) to aortic annulus ratio >0.14, increased papillary muscle echogenicity, and Doppler color flow through the left coronary artery.
CT
Coronary CT and MRI angiography allows a non-invasive method for diagnosis . Additionally, it offers a three-dimensional assessment of the anatomic relations between coronary arteries and adjacent structures, useful for surgical planning.[11]
MRI
MRI has the additional advantage of demonstrating communication and flow from the LCA into the PA, is useful in assessing mitral valvular function, and delayed gadolinium enhancement may help determine myocardial viability[12]
Coronary Angiography Findings
Coronary angiography or ventriculograms are not routinely necessary in the current era. Aortic root injection is a valuable diagnostic tool if echocardiography fails to diagnose.
Coronary angiogram should be performed despite a negative echocardiogram if either the history or ECG is strongly suggestive.
Hemodynamic measurements are usually consistent with low cardiac output and elevated left atrial pressures secondary to reduced left ventricular compliance or significant mitral valve insufficiency.
Oximetry may show a small left-to-right shunt into the pulmonary arteries.
Aortography or selective right coronary arteriography usually demonstrates an enlarged right coronary artery system with collateralization to the left coronary artery and eventual reflux of contrast into the pulmonary arterial system. If there is no collateralization, identification of the anomalous left coronary artery may not be evident by aortography or selective right coronary angiography.
Stop flow angiography
After a balloon occlusion in distal pulmonary trunk, the forceful injection of large amount of contrast is an alternative approach to perform an angiogram to see the retrograde filling. Incomplete occlusion of the pulmonary artery or balloon malapposition may cause a false negative result.
All three criteria listed below required for diagnosis:
- Retrograde filling of left coronary artery
- Absence of left coronary arterial origin in aortic root
- Pulmonary arterial connection to left coronary.
Although Bland-White-Garland Syndrome (ALCAPA) is very rare, a high index of suspicion is required during the workup of any infant or child with global myocardial dysfunction.
Treatment
- If left untreated (without surgical correction), the mortality rate in the first year of life is 90% secondary to myocardial ischemia or infarction and mitral valve insufficiency leading to CHF.
- Sudden death may occur within weeks to months after birth because of inadequate collateral circulation between the left and right coronary artery systems.
- In the adult type, accounting for only 10% to 15% of patients, intermediate to long-term survival is aided by a large dominant RCA with extensive inter coronary collaterals, as well as a restrictive opening between the ALCAPA and the PA which reduces the coronary steal phenomenon.
- These patients can remain asymptomatic until adulthood, despite ongoing sub clinical myocardial ischemia.
- In this subset of patients, there is an estimated 80% to 90% incidence of sudden death at a mean age of 35 years
Presently, the prognosis for patients with ALCAPA is dramatically improved as a result of both early diagnosis utilizing echocardiography with color Doppler flow mapping and improvements in surgical techniques, including myocardial preservation.
Pharmacotherapy
Acute Pharmacotherapies
- Inotropic agents - These agents are used to improve myocardial systolic function and increase preoperative or postoperative systemic blood flow..
- Diuretics - These agents promote excretion of water and electrolytes by the kidneys. They are used to treat heart failure or hepatic, renal, or pulmonary disease when sodium and water retention has resulted in edema or ascites.
- Afterload reducing agents - These agents improve preoperative or postoperative cardiac output by reducing systemic vascular resistance and increasing systemic blood flow resulting from myocardial dysfunction and/or significant mitral valve insufficiency.
- Nitrates are peripheral and coronary vasodilators used in the management of angina pectoris, heart failure, and myocardial infarction.
- ACE inhibitors are beneficial in all stages of chronic heart failure. Pharmacologic effects result in a decrease in systemic vascular resistance, reducing blood pressure, preload, and afterload. Dyspnea and exercise tolerance are improved.
Surgery and Device Based Therapy
- Simple ligation of anomalously originated left coronary artery at its origin was historically the first definitive surgical correction for this condition, with operative mortality rates ranging between 20% and 50%
- Direct re-implantation of the anomalously originated left coronary artery into the aorta is the most frequently adopted surgical technique, and it has gained popularity through increased experience with coronary artery transfer techniques adapted from the arterial switch operation. The reported mortality rate in direct r-implantation ranges between 0% and 16%.
- The Takeuchi procedure
- It involves creation of an aortopulmonary window and an intrapulmonary tunnel that baffles the aorta to the ostium of the anomalous left coronary artery.[13]
- Often routine mitral valve repair is performed at the time of coronary artery revascularization on the grounds that early postoperative cardiac output is improved with a resultant decrease in morbidity.
- Saphenous vein bypass grafting has yielded operative mortality rates of 0% to 38%. Disadvantages of this procedure in infants are the scarcity of vein grafts, both at initial and at redo operations, small vein caliber, and most importantly, late graft occlusion.
- Bilateral internal thoracic artery grafting to the left anterior descending and circumflex coronary arteries
References
- ↑ Surgical Treatment of Coronary Artery Anomalies Report of a 371⁄2-Year Experience at theTexas Heart Institute Tex Heart Inst J. 2002; 29(4): 299–307
- ↑ Cowles R, Berdon WE, Bland-White-Garland syndrome of anomalous left coronary artery arising from the pulmonary artery (ALCAPA): a historical review, Pediatric Radiology, Volume 37, Number 9, September 2007 , pp. 890-95.
- ↑ Mancini CM, Weber HS, Anomalous Left Coronary Artery from the Pulmonary Artery, e-medicine (http://www.emedicine.com/ped/topic2484.htm)
- ↑ Dodge-Khatami A, Mavroudis C, Backer CL, Anomalous origin of the left coronary artery from the pulmonary artery: collective review of surgical therapy, Ann Thorac Surg 2002;74:946–55.
- ↑ ALCAPA Syndrome: Not Just a Pediatric Disease1 Elena Peña, MD • Elsie T. Nguyen, MD • Naeem Merchant, MD • Carole Dennie, MD
- ↑ An adult case of Bland-White-Garland syndrome with collaterals from giant right coronary artery and bronchial artery 10.1016/j.jccase.2017.04.006
- ↑ An adult case of Bland-White-Garland syndrome with collaterals from the bronchial artery. Heart Vessels. 1994;9(4):218-22.
- ↑ J Cardiol Cases. 2016 Mar 31;14(1):1-3. doi: 10.1016/j.jccase.2016.03.006. eCollection 2016 Jul.
- ↑ J Cardiol Cases. 2016 Aug 3;14(5):145-148. doi: 10.1016/j.jccase.2016.07.001. eCollection 2016 Nov.
- ↑ Clin Cardiol. 2011 Apr;34(4):204-10. doi: 10.1002/clc.20848.
- ↑ BMJ Case Rep doi:10.1136/ bcr-2018-224307
- ↑ Clin Cardiol. 2011 Apr;34(4):204-10. doi: 10.1002/clc.20848.
- ↑ Pediatr Cardiol. 2012 Oct;33(7):1115-23