TIMI frame count (TFC)
|
Coronary Angiography | |
|
General Principles | |
|---|---|
|
Anatomy & Projection Angles | |
|
Normal Anatomy | |
|
Anatomic Variants | |
|
Projection Angles | |
|
Epicardial Flow & Myocardial Perfusion | |
|
Epicardial Flow | |
|
Myocardial Perfusion | |
|
Lesion Complexity | |
|
ACC/AHA Lesion-Specific Classification of the Primary Target Stenosis | |
|
Lesion Morphology | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Rim Halaby, M.D. [3]; Hilda Mahmoudi M.D., M.P.H.[4]
Synonyms and keywords: TFC
Overview
TIMI frame count is defined as the number of cineframes required for contrast to reach a standardized distal coronary landmark in the culprit vessel. The number is expressed based upon a cinefilming rate of 30 frames/second. Thus, a frame count of 30 would mean that 1 second was required for dye to traverse the artery.[1][2][3]
The TIMI Frame Count is counted using an electronic frame counter. Selected anatomic landmarks are used for the analysis.
History
The frame count was invented by C. Michael Gibson MS. MD. It was originally referred to as the "frames to opacification" [4] but was later renamed the TIMI frame count.
Clinical Importance
There are several limitations to the TFG classification scheme.[2] To overcome these limitations, Gibson developed a more objective and precise index of coronary blood flow called the corrected TIMI frame count (CTFC). In this method, the number of cineframes required for dye to reach standardized distal landmarks are counted. Each frame is 1/30th of a second, and the angiogram is therefore essentially a measure of the time for dye to go down the artery.[2][5][6] In the first frame used for TIMI frame counting, a column of dye touches both borders of the coronary artery and moves forward.[2] In the last frame, dye begins to enter (but does not necessarily fill) a standard distal landmark in the artery. These standard distal landmarks are as follows: in the RCA, the first branch of the posterolateral artery; in the circumflex system, the most distal branch of the obtuse marginal branch, which includes the culprit lesion in the dye path; and in the LAD, the distal bifurcation, which is also known as the "moustache," "pitchfork" or "whale’s tail". These frame counts are corrected for the longer length of the LAD by dividing by 1.7 to arrive at the CTFC.[2] Knowing the time for dye to go down the artery from the CTFC (CTFC/30=seconds), and length of the artery (either from an angioplasty guide wire or by planimetry), dye velocity (cm/s) can also be calculated in a more refined fashion.[7] This refined measure allows calculation of the velocity proximal and distal to the lesion.[7]
Some of the advantages of the TIMI frame count method are as follows. In contrast to the TFG classification scheme, the CTFC is quantitative rather than qualitative, it is objective rather than subjective, it is a continuous rather than a categorical variable, and it is reproducible.[2] The CTFC demonstrates that flow is not divided into arbitrary slow and fast categories, but rather coronary blood flow is unimodally distributed as a continuous variable.[2] The CTFC has been shown to be quite reproducible with a 1- to 2-frame difference between observers.[8][9][10][11][12][13][14][15][14][16][17][18][19] The CTFC is also highly correlated with other measures of flow such as Doppler velocity wire measures of coronary flow reserve, distal velocity, average peak velocity, and volumetric flow,[9][10][11] as well as fractional flow reserve (r=0.85).[12]
Several technical and physiological variables may impact the CTFC:[8][20][21][22][23]
1. Injection force: A power injector to change the force of injection (cc/sec) from the 10th to the 90th percentile of human injection rates lowers the CTFC by only 2 frames.[20]
2. Nitrate administration significantly increases the CTFC by 6 frames (P<0.001).[8]
3. Dye injection at the beginning of diastole decreases the CTFC by 3 to 6 frames.[8]
4. Increasing the heart rate by 20 beats per minute significantly decreases the CTFC by 5 frames (P<0.001).[8]
Association of the CTFC with Clinical Outcomes
Following fibrinolytic administration as well as PCI, the CTFC is related to a variety of clinical outcomes.[2] [5][6][24] [14][15][25][26][17] Flow in the infarct-related artery in survivors is significantly faster than in patients who die (49.5 versus 69.6 frames; P=0.0003).[5] In NSTEMI and STEMI, the post-PCI culprit flow among survivors is significantly faster than among those patients who died (CTFCs 20.4 versus 33.4 frames, P=0.017).[27] Among patients undergoing PCI, the CTFC has demonstrated greater sensitivity in detecting improvements in epicardial flow compared with the use of TIMI grade 3 flow among patients treated with new device interventions and in the detection of transplant rejection.[28][29][30][31][32][33]
Landmarks for TIMI Frame Count
Anatomic Landmark in Right Coronary Artery (RCA)
The landmark used in the right coronary artery is the first branch arising from the posterior lateral extension of the right coronary artery after the origin of the posterior descending artery, regardless of the size of this branch. [1] [2] [3]
This branch will often be located just distal to the bifurcation, and may be oriented either superiorly (R4U) or inferiorly (R4L).
In some cases this branch will lie further along the extension of the distal right coronary artery and will course either superiorly as the AV nodal artery (AV) or will be oriented inferiorly as the right inferior branch (RI). In the event that a very proximal posterior descending stenosis is the culprit lesion, the first branch off the posterior descending after the stenosis is the landmark.
Infrequently, the distal portion of the posterior descending artery is supplied by a proximally arising acute marginal branch and the proximal portion of the posterior descending artery arises at the base of the heart. In these cases, it is the extension of the distal right coronary past the posterior descending at the base of the heart and not the proximal acute marginal branch that is used for determining the TIMI frame count landmark.
In patients with left dominant anatomy, the TIMI frame count landmark is the distal-most branch off the right coronary artery once it is no longer in the AV groove.
Shown below is an image depicting the TIMI frame count landmark for the RCA.
R1= Proximal right coronary artery; R2= Mid right coronary artery; R3= Distal right coronary artery; R4= Right posterolateral artery; A1, A2, A3= Acute marginal arteries; PDA= Posterior descending artery.
Anatomic Landmark in Left Circumflex Artery (Cx)
The branch of the circumflex artery used for TIMI Frame Counting is determined as follows. The artery used for TIMI Frame Counting is the artery with the longest total distance along which dye travels in the left circumflex system and yet passes through the culprit lesion. [1] [2] [3]
When the culprit lesion is proximal to two arteries with equal total dye path distances, the artery which arises more distally from the left circumflex is used.
For example when the culprit lesion is located in the proximal left circumflex, the marginal branch with the longest total dye path distance is used, regardless of whether it is the first, second or third marginal. If these second and third marginals have equal total dye path distances, the third marginal is the target artery.
The target artery is always the first marginal when the culprit lesion is in the first marginal and, likewise, always the second marginal when the culprit lesion is in the second marginal.
In left and balanced dominant systems, the target artery is no further distal than the marginal branch which lies at the border of the inferior and lateral walls, usually the 3rd or 4th marginal; inferior wall vessels are never target arteries (i.e. “wrap around” LCx). The anatomic landmark is the distal-most branch in the target artery, regardless of the size of the branch. Usually this landmark branch can be found at approximately the mid-point of the distal third of the artery (5/6ths the distance down the vessel from its origin), but occasionally it is just prior to the termination of the artery.
Shown below are images depicting the TIMI frame count landmarks for the left circumflex artery.
Anatomic Landmark in Left Anterior Descending Artery (LAD)
The landmark in the LAD is the distal-most branch in the left anterior descending artery (referred to as the "pitchfork", "moustache" or "whale’s tail") usually occurs at the apex of the heart. [1] [2] [3]
In a "wrap around" left anterior descending artery, the branch closest to the apex of the heart is used.
In the event that a proximal diagonal stenosis is the culprit lesion, the distal branch off the diagonal after the stenosis is the landmark.
Shown below is an image depicting the TIMI frame count landmark for the LAD. The encircled part in the image is the distal-most branch in the left anterior descending artery (referred to as the "pitchfork", "moustache" or "whale’s tail") and is considered the TIMI frame count landmark for the LAD.
Definitions of the First and Last Frames Used for TIMI Frame Counting
The first frame used for TIMI Frame Counting is the first frame in which dye fully enters the artery, marked by dye touching both borders of the left main or right coronary artery. Dye may initially track down a single wall of the artery as dye leaks from the catheter prior to the injection and these frames are not included in the TIMI frame count. [1] [2] [3]
In the infrequent situation in which the left anterior descending artery is subselectively engaged and the left circumflex artery is the culprit vessel, the TIMI frame count begins when dye first touches both borders at the origin of the left circumflex artery. The last frame counted occurs when dye first enters the landmark branch off the target artery.
Note that complete opacification of the target artery is not required, just initial entry of dye into the culprit artery. Often the last frame is best determined by running the cinefilm past the initial opacification of the landmark branch and then moving frame-by-frame in reverse until the landmark branch disappears and then advance one more frame.
The Corrected TIMI Frame Count vs the TIMI Frame Count
The raw TIMI Frame Count is the number of cineframes required for contrast to reach a standardized distal coronary landmark in the culprit vessel normalized to 30 frames/second. This value is not the “Corrected TIMI Frame Count (CTFC),” which adjusts for vessel length as well. A 1.7 correction factor is used to correct the TIMI frame counts for the average shorter length of the LCx or RCA, as compared with the LAD. When this correction is applied, this is called the corrected TIMI Frame Count (CTFC). A 1.6 correction factor is used to correct the TIMI frame counts for the average greater length of SVG’s, as compared with the LCx or the RCA.
For example, if dye reached fully entered the Left Main Coronary Artery at frame 8 of a 15 frames per second cinefilm and reached the distal landmark of the LAD at frame 28, the unadjusted frame count would be 20, the raw TIMI Frame Count would be 40, and the Corrected TIMI Frame Count would be 68.
| Type of Frame Count | Step Performed | Result |
|---|---|---|
| Unadjusted Frame Count | Subtract initial frame from final frame number Unadjusted Frame Count = 8 - 8 = 20 |
20 |
| Raw TIMI Frame Count | Adjust for filming speed. Raw TIMI Frame Count = 20 * (30 fps)/(15 fps) = 40 |
40 |
| Corrected TIMI Frame Count | Correct for vessel length. Corrected TIMI Frame Count = 40 / (1.6) = 25 |
25 |
Adjusting for Different Film Speeds
30 frames/second is the standard film speed used in U.S. cardiac catheterization laboratories (more recently 30 frames/sec filming rates are widely available at international catheterization laboratories). Alternatives include 15 frames/second and 60 frames/second. The European equivalents of U.S. 30 frames/second and 15 frames/second are 25 frames/second and 12.5 frames/second, respectively. If the frame count was collected at a rate of 15 frames/second, then the frame count is multiplied by 2 to arrive at the CTFC.
Insights into the Pathophysiology of STEMI and UA/NSTEMI Based Upon the CTFC
One of the more interesting observations learned with the use of the CTFC is the fact that flow in nonculprit arteries in the setting of acute coronary syndromes is "abnormal." For instance, the CTFC in uninvolved arteries in acute STEMI (30.5 frames) is in fact 40% slower than normal (21 frames, P<0.001)[2] [34] [35] [36] Adjunctive and rescue PCI following fibrinolysis restores flow in culprit vessels that is nearly identical to that of nonculprit arteries in the STEMI setting (30.5 versus 30.5 frames, p=NS)[34], but this flow remains slower than normal (21 frames). It is notable that PCI of the culprit lesion is also associated with improvements in the nonculprit artery after the intervention in both the STEMI and UA/NSTEMI settings [34] [35]. Slower flow throughout all 3 arteries in STEMI is associated with a higher risk of adverse outcomes [34], poorer wall motion in remote territories[34], poorer tissue perfusion on digital subtraction angiography (DSA)[35], and a greater magnitude of ST depression in remote territories such as the anterior precordium in inferior MI [37]. The basis of slowed flow in non-culprit arteries is not clear. It has been speculated that the delayed flow in the non-culprit artery may be the result of spasm in shared territories of microvasculature, or a result of global vasoconstriction mediated through either a local neurohumoral or paracrine mechanism. Gregorini et al[38] have highlighted the importance of sympathetic storm. Consistent with this hypothesis, they have demonstrated that the CTFC and fractional wall shortening is improved in both the culprit and nonculprit arteries after administration of alpha-blockers. Willerson and others [39][40][41][42][43][44][45] have also demonstrated that a wide range of vasoconstrictors including thromboxane A2, serotonin, endothelin, oxygen-derived free radicals, and thrombin are all released in the setting of vessel injury, thrombosis and reperfusion. While a residual stenosis following PCI in the setting of STEMI may be responsible for the delay in flow, it is important to note that despite a minimal 13% residual stenosis and the relief of intraluminal obstruction with stent placement, flow remains persistently abnormal in 34% of stented vessels.[3]
Washout TIMI Frame Count
The washout TIMI Frame Count is the number of frames required for dye to exit the infarct related artery (clearance of dye from the ostium to the standardized distal TIMI landmark).
In the first frame, unopacified blood occupies at least 70% of the ostium of the artery with antegrade motion down the artery. In the last frame, unopacified blood first enters (but does not completely fill) the standard distal TIMI landmark
TIMI Myocardial Frame Count (TMFC) = frame when blush is the brightest minus frame when blush first appears.
Tips for TIMI Frame Count Evaluations
How do I pick the first frame?
In frame zero, dye touches either none of the borders or only one of the borders as shown below:
We find that in some injections dye will dribble down on border of the artery and these frames are not selected as the first frame. In frame number one, dye extends across at least 70% of the artery and moves forward as shown below:
How do I pick the last frame?
In the last frame, the dye first enters the distal landmark. This frame is included in the frame count. For example, in frame 20 in the RCA shown below, dye has not yet entered the first branch off of the posterolateral:
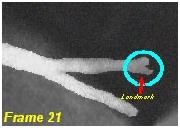
In frame 21 shown below, the dye has begun to enter the first branch off of the posterolateral artery. This is the last frame counted:
In frame 22, dye begins to fill more completely the distal landmark as shown below:
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Gibson CM, Ryan KA, Kelley M; et al. (1999). "Methodologic drift in the assessment of TIMI grade 3 flow and its implications with respect to the reporting of angiographic trial results. The TIMI Study Group". Am. Heart J. 137 (6): 1179–84. PMID 10347349. Unknown parameter
|month=ignored (help) - ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Gibson CM, Cannon CP, Daley WL; et al. (1996). "TIMI frame count: a quantitative method of assessing coronary artery flow". Circulation. 93 (5): 879–88. PMID 8598078. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Gibson CM, Murphy S, Menown IB; et al. (1999). "Determinants of coronary blood flow after thrombolytic administration. TIMI Study Group. Thrombolysis in Myocardial Infarction". J. Am. Coll. Cardiol. 34 (5): 1403–12. PMID 10551685. Unknown parameter
|month=ignored (help) - ↑ Piana RN, Paik GY, Moscucci M; et al. (1994). "Incidence and treatment of 'no-reflow' after percutaneous coronary intervention". Circulation. 89 (6): 2514–8. PMID 8205658. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 5.2 Gibson CM, Murphy SA, Rizzo MJ; et al. (1999). "Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group". Circulation. 99 (15): 1945–50. PMID 10208996. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E (2002). "Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction". Circulation. 105 (16): 1909–13. PMID 11997276. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 Gibson CM, Dodge JT, Goel M; et al. (1997). "Angioplasty guidewire velocity: a new simple method to calculate absolute coronary blood velocity and flow". Am. J. Cardiol. 80 (12): 1536–9. PMID 9416931. Unknown parameter
|month=ignored (help) - ↑ 8.0 8.1 8.2 8.3 8.4 Abaci A, Oguzhan A, Eryol NK, Ergin A (1999). "Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility". Circulation. 100 (22): 2219–23. PMID 10577994. Unknown parameter
|month=ignored (help) - ↑ 9.0 9.1 Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV (1999). "Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method". Am. J. Cardiol. 83 (11): 1562–5, A7. PMID 10363873. Unknown parameter
|month=ignored (help) - ↑ 10.0 10.1 Stankovic G, Manginas A, Voudris V; et al. (2000). "Prediction of restenosis after coronary angioplasty by use of a new index: TIMI frame count/minimal luminal diameter ratio". Circulation. 101 (9): 962–8. PMID 10704161. Unknown parameter
|month=ignored (help) - ↑ 11.0 11.1 Barcin C, Denktas AE, Garratt KN, Higano ST, Holmes DR, Lerman A (2003). "Relation of Thrombolysis in Myocardial Infarction (TIMI) frame count to coronary flow parameters". Am. J. Cardiol. 91 (4): 466–9. PMID 12586269. Unknown parameter
|month=ignored (help) - ↑ 12.0 12.1 Umman B, Nisanci Y, Sezer M; et al. (2002). "The relationship between corrected TIMI frame count and myocardial fractional flow reserve". J Invasive Cardiol. 14 (3): 125–8. PMID 11870267. Unknown parameter
|month=ignored (help) - ↑ French JK, Hyde TA, Amos DJ, et al. Corrected TIMI frame count at 3 weeks influences survival at 5 years but not 10 years after myocardial infarction. Eur Heart J. 1998; 19: 630.
- ↑ 14.0 14.1 14.2 French JK, Straznicky IT, Webber BJ; et al. (1999). "Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction". Heart. 81 (2): 128–33. PMC 1728934. PMID 9922346. Unknown parameter
|month=ignored (help) - ↑ 15.0 15.1 French JK, Ellis CJ, Webber BJ; et al. (1998). "Abnormal coronary flow in infarct arteries 1 year after myocardial infarction is predicted at 4 weeks by corrected Thrombolysis in Myocardial Infarction (TIMI) frame count and stenosis severity". Am. J. Cardiol. 81 (6): 665–71. PMID 9527071. Unknown parameter
|month=ignored (help) - ↑ French JK, Hyde TA, Straznicky IT; et al. (2000). "Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction". J. Am. Coll. Cardiol. 35 (6): 1516–24. PMID 10807455. Unknown parameter
|month=ignored (help) - ↑ 17.0 17.1 Amos DJ, French JK, Andrews J; et al. (2001). "Corrected TIMI frame counts correlate with stenosis severity and infarct zone wall motion after thrombolytic therapy". Am. Heart J. 141 (4): 586–91. doi:10.1067/mhj.2001.113393. PMID 11275924. Unknown parameter
|month=ignored (help) - ↑ Sahin M, Basoglu T, Canbaz F, Elcik M, Kosus A (2002). "The value of the TIMI frame count method in the diagnosis of coronary no-reflow: a comparison with myocardial perfusion SPECT in patients with acute myocardial infarction". Nucl Med Commun. 23 (12): 1205–10. doi:10.1097/01.mnm.0000046213.83338.9e. PMID 12464786. Unknown parameter
|month=ignored (help) - ↑ Moliterno D, Antman EM, Ohman M, et al. Concordance between core labs in trial results using TIMI flow grades and frame counts. Circulation. 2000; 102 (suppl II): II–590.
- ↑ 20.0 20.1 Dodge JT, Rizzo M, Nykiel M; et al. (1998). "Impact of injection rate on the Thrombolysis in Myocardial Infarction (TIMI) trial frame count". Am. J. Cardiol. 81 (10): 1268–70. PMID 9604968. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Anshelevich M, Murphy S; et al. (2000). "Impact of injections during diagnostic coronary arteriography on coronary patency in the setting of acute myocardial infarction from the TIMI trials. Thrombolysis In Myocardial Infarction". Am. J. Cardiol. 86 (12): 1378–9, A5. PMID 11113418. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Kirtane AJ, Murphy SA; et al. (2001). "Impact of contrast agent type (ionic versus nonionic) used for coronary angiography on angiographic, electrocardiographic, and clinical outcomes following thrombolytic administration in acute myocardial infarction". Catheter Cardiovasc Interv. 53 (1): 6–11. doi:10.1002/ccd.1121. PMID 11329210. Unknown parameter
|month=ignored (help) - ↑ Faile BA, Guzzo JA, Tate DA, Nichols TC, Smith SC, Dehmer GJ (2000). "Effect of sex, hemodynamics, body size, and other clinical variables on the corrected thrombolysis in myocardial infarction frame count used as an assessment of coronary blood flow". Am. Heart J. 140 (2): 308–14. doi:10.1067/mhj.2000.108003. PMID 10925348. Unknown parameter
|month=ignored (help) - ↑ French JK, Hyde TA, Amos DJ, et al. Corrected TIMI frame count at 3 weeks influences survival at 5 years but not 10 years after myocardial infarction. Eur Heart J. 1998; 19: 630.
- ↑ French JK, Straznicky IT, Webber BJ, et al. Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction. Heart. 1999; 81: 128–133.
- ↑ French JK, Hyde TA, Straznicky IT, et al. Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction. J Am Coll Cardiol. 2000; 35: 1516–1524.
- ↑ Gibson CM, Dotani MI, Murphy SA; et al. (2002). "Correlates of coronary blood flow before and after percutaneous coronary intervention and their relationship to angiographic and clinical outcomes in the RESTORE trial. Randomized Efficacy Study of Tirofiban for Outcomes and REstenosis". Am. Heart J. 144 (1): 130–5. PMID 12094199. Unknown parameter
|month=ignored (help) - ↑ Edep ME, Guarneri EM, Teirstein PS, Phillips PS, Brown DL (1999). "Differences in TIMI frame count following successful reperfusion with stenting or percutaneous transluminal coronary angioplasty for acute myocardial infarction". Am. J. Cardiol. 83 (9): 1326–9. PMID 10235089. Unknown parameter
|month=ignored (help) - ↑ Vrachatis AD, Alpert MA, Georgulas VP; et al. (2001). "Comparative efficacy of primary angioplasty with stent implantation and thrombolysis in restoring basal coronary artery flow in acute ST segment elevation myocardial infarction: quantitative assessment using the corrected TIMI frame count". Angiology. 52 (3): 161–6. PMID 11269778. Unknown parameter
|month=ignored (help) - ↑ Hamada S, Nishiue T, Nakamura S; et al. (2001). "TIMI frame count immediately after primary coronary angioplasty as a predictor of functional recovery in patients with TIMI 3 reperfused acute myocardial infarction". J. Am. Coll. Cardiol. 38 (3): 666–71. PMID 11527614. Unknown parameter
|month=ignored (help) - ↑ Capozzolo C, Piscione F, De Luca G; et al. (2001). "Direct coronary stenting: effect on coronary blood flow, immediate and late clinical results". Catheter Cardiovasc Interv. 53 (4): 464–73. PMID 11514995. Unknown parameter
|month=ignored (help) - ↑ Bickel C, Rupprecht HJ, Maimaitiming A; et al. (2002). "The superiority of TIMI frame count in detecting coronary flow changes after coronary stenting compared to TIMI Flow Classification". J Invasive Cardiol. 14 (10): 590–6. PMID 12368511. Unknown parameter
|month=ignored (help) - ↑ Fang JC, Kinlay S, Wexberg P; et al. (2000). "Use of the thrombolysis in myocardial infarction frame count for the quantitative assessment of transplant-associated arteriosclerosis". Am. J. Cardiol. 86 (8): 890–2. PMID 11024410. Unknown parameter
|month=ignored (help) - ↑ 34.0 34.1 34.2 34.3 34.4 Gibson CM, Ryan KA, Murphy SA; et al. (1999). "Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction". J. Am. Coll. Cardiol. 34 (4): 974–82. PMID 10520778. Unknown parameter
|month=ignored (help) - ↑ 35.0 35.1 35.2 Gibson CM, Goel M, Murphy SA; et al. (2000). "Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis". Am. J. Cardiol. 86 (12): 1375–7, A5. PMID 11113417. Unknown parameter
|month=ignored (help) - ↑ Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O'Neill WW (2000). "Multiple complex coronary plaques in patients with acute myocardial infarction". N. Engl. J. Med. 343 (13): 915–22. PMID 11006367. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Chen M, Angeja BG; et al. (2002). "Precordial ST-segment depression in inferior myocardial infarction is associated with slow flow in the non-culprit left anterior descending artery" (PDF). J. Thromb. Thrombolysis. 13 (1): 9–12. PMID 11994554. Unknown parameter
|month=ignored (help) - ↑ Gregorini L, Marco J, Kozàkovà M; et al. (1999). "Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction". Circulation. 99 (4): 482–90. PMID 9927393. Unknown parameter
|month=ignored (help) - ↑ Hirsh PD, Hillis LD, Campbell WB, Firth BG, Willerson JT (1981). "Release of prostaglandins and thromboxane into the coronary circulation in patients with ischemic heart disease". N. Engl. J. Med. 304 (12): 685–91. PMID 6894016. Unknown parameter
|month=ignored (help) - ↑ Bush LR, Campbell WB, Kern K; et al. (1984). "The effects of alpha 2-adrenergic and serotonergic receptor antagonists on cyclic blood flow alterations in stenosed canine coronary arteries". Circ. Res. 55 (5): 642–52. PMID 6488486. Unknown parameter
|month=ignored (help) - ↑ Willerson JT, Campbell WB, Winniford MD; et al. (1984). "Conversion from chronic to acute coronary artery disease: speculation regarding mechanisms". Am. J. Cardiol. 54 (10): 1349–54. PMID 6391133. Unknown parameter
|month=ignored (help) - ↑ Apprill P, Schmitz JM, Campbell WB; et al. (1985). "Cyclic blood flow variations induced by platelet-activating factor in stenosed canine coronary arteries despite inhibition of thromboxane synthetase, serotonin receptors, and alpha-adrenergic receptors". Circulation. 72 (2): 397–405. PMID 2988822. Unknown parameter
|month=ignored (help) - ↑ Ashton JH, Golino P, McNatt JM, Buja LM, Willerson JT (1989). "Serotonin S2 and thromboxane A2-prostaglandin H2 receptor blockade provide protection against epinephrine-induced cyclic flow variations in severely narrowed canine coronary arteries". J. Am. Coll. Cardiol. 13 (3): 755–63. PMID 2521875. Unknown parameter
|month=ignored (help) - ↑ Eidt JF, Allison P, Noble S; et al. (1989). "Thrombin is an important mediator of platelet aggregation in stenosed canine coronary arteries with endothelial injury". J. Clin. Invest. 84 (1): 18–27. doi:10.1172/JCI114138. PMC 303947. PMID 2661588. Unknown parameter
|month=ignored (help) - ↑ Willerson JT, Golino P, Eidt J, Campbell WB, Buja LM (1989). "Specific platelet mediators and unstable coronary artery lesions. Experimental evidence and potential clinical implications". Circulation. 80 (1): 198–205. PMID 2661053. Unknown parameter
|month=ignored (help)