Wolff-Parkinson-White syndrome EKG: Difference between revisions
| (38 intermediate revisions by 5 users not shown) | |||
| Line 2: | Line 2: | ||
{{Wolff-Parkinson-White syndrome}} | {{Wolff-Parkinson-White syndrome}} | ||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{Sara.Zand}} {{CZ}} | ||
== | ==Overview== | ||
[[Wolff-Parkinson-White]] ([[WPW]]) pattern is characterized by [[ECG]] findings such as a short [[PR interval]] and a [[delta wave]] and wide [[QRS]] complex.[[ WPW syndrome]] is the occurrence of [[tachycardia]] with or without associated symptoms in a subject with existing [[WPW]] pattern. [[WPW syndrome]] can present as an orthodromic or antidromic [[AVRT]] during which the [[delta wave]] no longer appears. [[Atrial fibrillation]] in a patient with [[WPW]] should be suspected when there is [[ECG]] findings of an irregularly irregular [[rhythm]] and absent [[P wave]]s suggestive of [[atrial fibrillation]] in the context of a [[heart rate]] higher than 240 beats per minute. | |||
==[[WPW]] Pattern== | |||
*[[WPW]] pattern is characterized by the following typical [[EKG]] findings: | |||
** Short [[PR interval]]: The [[PR interval]] is short because the [[ventricles]] begins to contract earlier than usual because of the electrical signal travels through the [[accessory pathway]] faster than the [[AV node]]. | |||
**[[Wide QRS]] | |||
**[[delta wave]] | |||
**[[QRS alternans]] | |||
**[[ST segment depression]]. | |||
*Preexcitation and presence of [[delta wave]]s typical of [[WPW syndrome]] or [[WPW pattern]] may either mimic [[myocardial infarction]] or may mask it.<ref name="pmid18602643">{{cite journal| author=Smolders L, Majidi M, Krucoff MW, Crijns HJ, Wellens HJ, Gorgels AP| title=Preexcitation and myocardial infarction: conditions with confusing electrocardiographic manifestations. | journal=J Electrocardiol | year= 2008 | volume= 41 | issue= 6 | pages= 679-82 | pmid=18602643 | doi=10.1016/j.jelectrocard.2008.05.005 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18602643 }} </ref><br> | |||
**Abolishment of [[delta waves]] may be necessary for the diagnosis of [[myocardial infarction]] on [[EKG]].<ref name="pmid23157811">{{cite journal| author=Liu R, Chang Q| title=The diagnosis of myocardial infarction in the Wolff-Parkinson-White syndrome. | journal=Int J Cardiol | year= 2013 | volume= 167 | issue= 3 | pages= 1083-4 | pmid=23157811 | doi=10.1016/j.ijcard.2012.10.055 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23157811 }} </ref><br> | |||
**Left posterolateral or lateral [[accessory pathways]] may mask inferior or anteroseptal [[ myocardial infarction ]].<ref name="pmid7942468">{{cite journal| author=Preminger MW, Callans DJ, Gottlieb CD, Marchlinski FE| title=Radiofrequency catheter ablation used to unmask infarction Q waves in Wolff-Parkinson-White syndrome. | journal=Am Heart J | year= 1994 | volume= 128 | issue= 5 | pages= 1040-2 | pmid=7942468 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7942468 }} </ref><br> | |||
**Posteroseptal accessory pathways may mask an [[anterior MI]].<ref name="pmid7942468">{{cite journal| author=Preminger MW, Callans DJ, Gottlieb CD, Marchlinski FE| title=Radiofrequency catheter ablation used to unmask infarction Q waves in Wolff-Parkinson-White syndrome. | journal=Am Heart J | year= 1994 | volume= 128 | issue= 5 | pages= 1040-2 | pmid=7942468 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7942468 }} </ref><br> | |||
**Right anteroseptal and anterolateral [[accessory pathways]] may mask inferior or [[anterolateral MI]].<ref name="pmid7942468">{{cite journal| author=Preminger MW, Callans DJ, Gottlieb CD, Marchlinski FE| title=Radiofrequency catheter ablation used to unmask infarction Q waves in Wolff-Parkinson-White syndrome. | journal=Am Heart J | year= 1994 | volume= 128 | issue= 5 | pages= 1040-2 | pmid=7942468 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7942468 }} </ref> | |||
== Determining the location of the accessory pathway== | == Determining the location of the accessory pathway== | ||
{| | {{Family tree/start}} | ||
| | {{Family tree | | | | | | | | | | | | | | | | B01 | | | |B01= V1}} | ||
|- | {{Family tree | | | | | | | | | | | | | |,|-|-|^|-|-|-|-|-|-|-|-|-|-|-|-|-|-|.| | | | | |}} | ||
| | {{Family tree | | | | | | | | | | | | | C01 | | | | | | | | | | | | | | | | |C02 |C01=_ | C02=+|}} | ||
|| | {{Family tree | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | |}} | ||
| | {{Family tree | | | | | | | | | | | | | D1| | | | | | | | | | | | | | | | | D1 | | | | | | | | | | | | | | | D1= Positive inferior leads| | | |}} | ||
|- | {{Family tree | | | | | | | | | | |,|-|-|-|+|-|-|-|.| | | | | | | | | |,|-|-|-|+|-|-|-|.| | | | | | | | | | | | | |}} | ||
| | {{Family tree | | | | | | | | | | |D2 | |D3 | |D4 | | | | | | | |K2 | |K3 | |K4 | | | | | | | | | | |K4=0 |K3=1,2 |D4=3 | D3=1,2|D2=0 | K2=3|}} | ||
|- | {{Family tree | | | | | | | | | | |!| | | |!| | | |!| | | | | | | | | |!| | | |!| | | |!| | | | | | | | | | | | | | |}} | ||
| | {{Family tree | | | | | | | | | | |F1 | |F1 | |F1 | | | | | | |L1 | | |L2 | |L3 | | | | | | | | | | | | | | | | |F1=V3 |L1=Left lateral |L2= Left posterolateral | L3= V1/1 ratio| | |}} | ||
|- | {{Family tree | | | | | | | | |,|-|^|.| | | |:| | | | |:| | | | | | | | | | | | | | | | |:| | | | | | | | | | | | |}} | ||
{{Family tree | | | | | | | | G1| | G2| |:| | | | |:| | | | | | | | | | | | | | | | |:| | | | | | | | | | | |G2=+ |G1=_ |}} | |||
{{Family tree | | | | | | | | |!| | |!| | | |:| | | | |:| | | | | | | | | | | | | | |,|-|^|-|.| | | | | | | | | | | | | | | |}} | |||
{{Family tree | | | | | | | |H1 | |H2 | |:| | | | |:| | | | | | | | | | | | | | |J1 | | J2| | | | | | | | | | | |J1= <1 |J2=≥1 | H2=Right paraseptal|H1=Right posterior| |}} | |||
{{Family tree | | | | | | | | | | | | |,|-|-|^|.| | | |:| | | | | | | | | | | | | | |!| | | | |!| | | | | | | | | |}} | |||
{{Family tree | | | | | | | | | | | | H3| | |H4 | |:| | | | | | | | | | | | | | | M1| | |N1 | | | | | | | | | | | |M1=Lead 2, Notched QS | N1=Left posterolateral| H3=_|H4=+ |}} | |||
{{Family tree | | | | | | | | | | | | |!| | | |!| | | |:| | | | | | | | | | | | |,|-|^|-|.| | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | |H5 | |H6 | | |:| | | | | | | | | | | | | Y1| | Y2| | | | | | | | | |Y2=NO |Y1= Yes |H6=[[Nodo-Hisian]] |H5=Right lateral |}} | |||
{{Family tree | | | | | | | | | | | | | | | | |,|-|-|-|^|.| | | | | | | | | | | |!| | | |!| | | | | | | | | | | | |}} | |||
{{Family tree | | | | | | | | | | | | | | | | |j1 | | |j2 | | | | | | | | | |Y3 | |Y4 | | | | | | | | | |Y4=Left paraseptal |Y3=Deep coronary sinus | j1=_| j2=+| }} | |||
{{Family tree | | | | | | | | | | | | | | | | |!| | | | |!| | | | | | | | | | | | | | | | | | | | | | | | | | | | |}} | |||
{{Family tree | | | | | | | | | | | | | | | | |J3 | | | J4| | | | | | | | | | | | | | | | | | | | | | | | | | |J3=[[Nodo-Hisian]] | |J4=[[Right atrium]] | |}} | |||
{{Family tree/end}} | |||
{| | |||
! colspan="2" style="background: PapayaWhip;" align="center" + |The above algorithm adopted from 2019 ESC Guideline<ref name="pmid31504425">{{cite journal |vauthors=Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, Calkins H, Corrado D, Deftereos SG, Diller GP, Gomez-Doblas JJ, Gorenek B, Grace A, Ho SY, Kaski JC, Kuck KH, Lambiase PD, Sacher F, Sarquella-Brugada G, Suwalski P, Zaza A |title=2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC) |journal=Eur Heart J |volume=41 |issue=5 |pages=655–720 |date=February 2020 |pmid=31504425 |doi=10.1093/eurheartj/ehz467 |url=}}</ref> | |||
|- | |||
|} | |} | ||
== | ==[[WPW Syndrome]]== | ||
*[[WPW syndrome]] is the occurrence of [[tachycardia]] with or without associated symptoms in a subject with existing [[WPW]] pattern.<ref>{{Cite web | last = | first = | title = Wolff-Parkinson-White Syndrome and Accessory Pathways | url = http://circ.ahajournals.org/content/122/15/e480.full | publisher = | date = | accessdate = 1 April 2014 }}</ref> | |||
*Several types of [[ arrhythmia]] can occur in [[WPW syndrome]] such as [[AV reentrant tachycardia]] (AVRT), [[atrial fibrillation]],or [[atrial flutter]] | |||
the most common type of [[tachyarrhythmia]] is [[AVRT]].<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref> | |||
====[[Orthodromic AVRT]]==== | |||
*In orthodromic AVRT, the anterograde conduction (from the [[atrium]] to the [[ventricle]]) passes through the[[ AV node]] and the retrograde conduction (from the [[ventricle]] to the [[atrium]]) passes through the [[accessory pathway]]. | |||
* Orthodromic [[AVRT]] occurs in approximately 90 to 95% of [[WPW]]. | |||
The [[EKG]] findings include the following: | |||
* Regular [[rhythm]]<br> | |||
* Narrow [[QRS complex]]es <br> | |||
* Retrograde [[P wave]] following the [[QRS]] complex <br> | |||
* Long RP, short PR tachycardia | |||
[[File:SVT.jpg|800px|center]] | |||
====Antidromic AVRT==== | |||
*The [[anterograde conduction]] (from the [[atrium]] to the [[ventricle]]) passes through the [[accessory pathway]] and the [[retrograde conduction]] (from the [[ventricle]] to the [[atrium]]) passes through the [[AV node]]. | |||
* It apprears in less than 10% of [[WPW]].<br> | |||
*The [[EKG]] findings may include the following: | |||
* Regular [[rhythm]]<br> | |||
* [[Wide QRS complexes]] [[tachycardia]] <br> | |||
[[File:Wide complex tachy.jpg|800px|center]] | |||
== | ==[[Atrial Fibrillation]] in [[WPW]]== | ||
*[[Atrial fibrillation]] in [[WPW]] syndrome is life-threatening because it might lead to [[ventricular tachycardia]]. | |||
* The suggestive findings of [[antidromic AVRT] and rapid [[atrial fibrillation]] on the [[ECG]] may include the following: | |||
* Irregularly irregular [[ rhythm]] | |||
* Absent of [[P wave]] | |||
* [[Wide WRS]] | |||
* [[Ventricular rate]] >240 beats per minute<ref name="KleinBashore1979">{{cite journal|last1=Klein|first1=George J.|last2=Bashore|first2=Thomas M.|last3=Sellers|first3=T. D.|last4=Pritchett|first4=Edward L. C.|last5=Smith|first5=William M.|last6=Gallagher|first6=John J.|title=Ventricular Fibrillation in the Wolff-Parkinson-White Syndrome|journal=New England Journal of Medicine|volume=301|issue=20|year=1979|pages=1080–1085|issn=0028-4793|doi=10.1056/NEJM197911153012003}}</ref> | |||
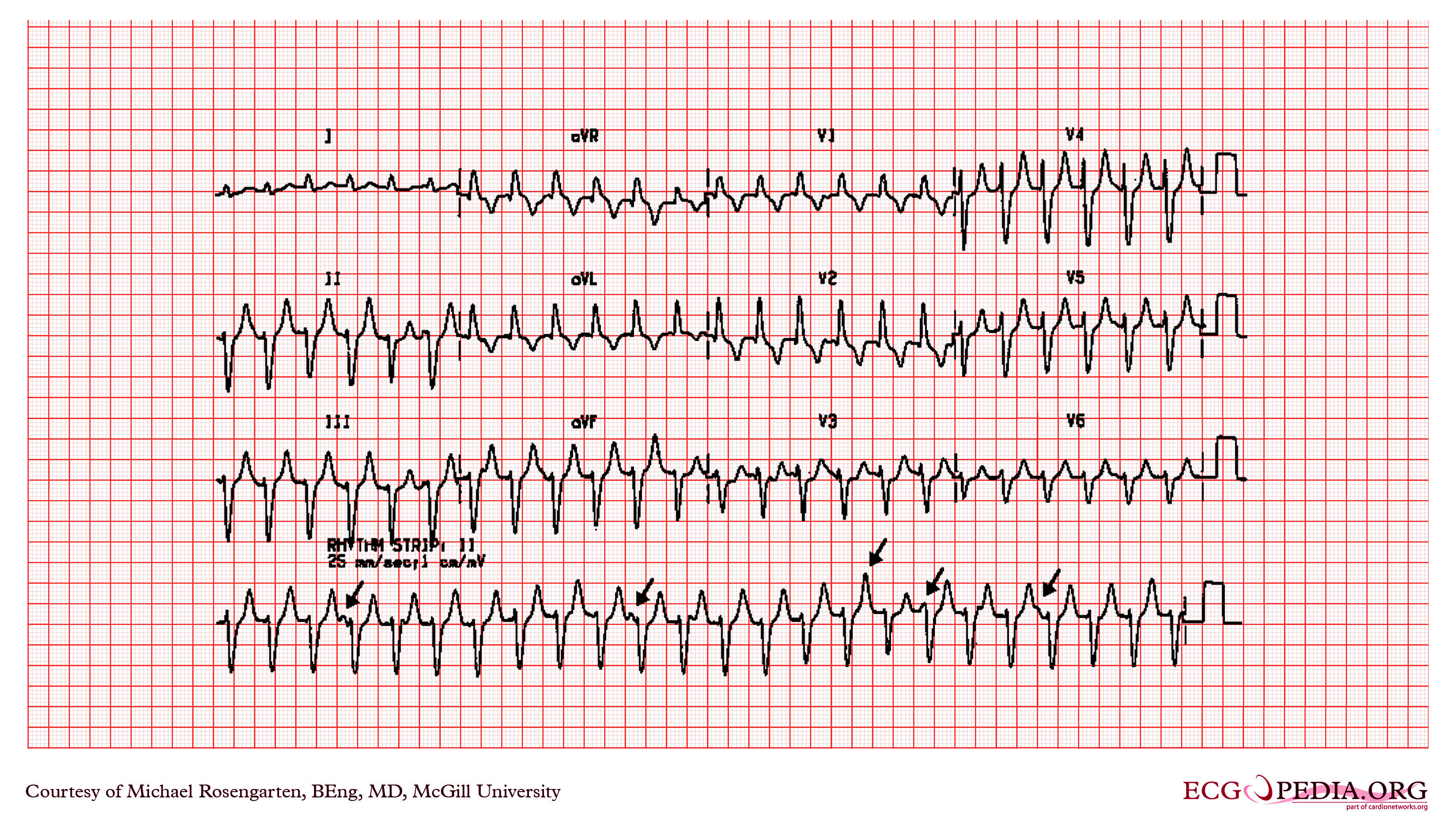
Shown below is an [[ECG]] depicting an irregularly irregular rhythm with [[wide QRS]] and absent [[P waves]] suggestive of [[atrial fibrillation]] in [[WPW syndrome]]. | |||
[[File:Wpw with afib.PNG|center|300px]] | |||
==Examples== | ==Examples== | ||
Shown below is an EKG of [[Wolff-Parkinson-White syndrome]] demonstrating slurred upstroke of the [[QRS complex]] (>110 milli sec), resulting in a [[delta-wave]] (arrow). The EKG also shows a [[short PR interval]].[[File:Rhythm_WPW.png|center|800px]] | Shown below is an [[EKG]] of [[Wolff-Parkinson-White syndrome]] demonstrating slurred upstroke of the [[QRS complex]] (>110 milli sec), resulting in a [[delta-wave]] (arrow). The EKG also shows a [[short PR interval]].[[File:Rhythm_WPW.png|center|800px]] | ||
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | ||
---- | ---- | ||
Shown below is an EKG showing a slurred upstroke [[QRS]] complex which is best appreciated in the [[precordial leads]] and a [[PR interval]] of less than 120 ms ([[short PR interval]]) suggesting WPW syndrome. | Shown below is an [[EKG]] showing a slurred upstroke [[QRS]] complex which is best appreciated in the [[precordial leads]] and a [[PR interval]] of less than 120 ms ([[short PR interval]]) suggesting [[WPW syndrome]]. | ||
[[Image:Wolf_Parkinson_White_syndrome.png|center|800px]] | [[Image:Wolf_Parkinson_White_syndrome.png|center|800px]] | ||
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | ||
| Line 102: | Line 98: | ||
---- | ---- | ||
Shown below is an EKG demonstrating a [[delta wave]] in | Shown below is an [[EKG]] demonstrating a [[delta wave]] in leads [[Precordial leads|V<sub>2</sub>]], I, aVL, with [[wide QRS complexes]] and [[left axis deviation]] suggesting [[WPW syndrome]]. | ||
[[Image:WPW_syndrome_1.jpg|center|800px]] | [[Image:WPW_syndrome_1.jpg|center|800px]] | ||
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | ||
| Line 108: | Line 104: | ||
---- | ---- | ||
Shown below is an | Shown below is an [[EKG]] showing a [[short PR interval]] of less than 120 ms, delta waves in leads [[Limb lead|I]], [[Augmented limb lead|aVF]], [[Augmented limb lead|aVL]] and [[chest]] leads with [[wide QRS]] complexes indicating [[WPW syndrome]]. | ||
[[Image:WPW_syndrome_2.jpg|center|800px]] | [[Image:WPW_syndrome_2.jpg|center|800px]] | ||
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page | ||
| Line 114: | Line 110: | ||
---- | ---- | ||
;For more EKG examples of Wolff-Parkinson-White syndrome click [[Wolff-Parkinson-White syndrome EKG examples | ; For more [[EKG]] examples of [[Wolff-Parkinson-White syndrome]] click [[Wolff-Parkinson-White syndrome]] [[EKG]] examples here. | ||
==References== | ==References== | ||
| Line 123: | Line 119: | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Disease]] | |||
[[Category:Needs overview]] | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 11:33, 19 August 2022
|
Wolff-Parkinson-White syndrome Microchapters |
|
Differentiating Wolff-Parkinson-White syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wolff-Parkinson-White syndrome EKG On the Web |
|
Risk calculators and risk factors for Wolff-Parkinson-White syndrome EKG |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Sara Zand, M.D.[2] Cafer Zorkun, M.D., Ph.D. [3]
Overview
Wolff-Parkinson-White (WPW) pattern is characterized by ECG findings such as a short PR interval and a delta wave and wide QRS complex.WPW syndrome is the occurrence of tachycardia with or without associated symptoms in a subject with existing WPW pattern. WPW syndrome can present as an orthodromic or antidromic AVRT during which the delta wave no longer appears. Atrial fibrillation in a patient with WPW should be suspected when there is ECG findings of an irregularly irregular rhythm and absent P waves suggestive of atrial fibrillation in the context of a heart rate higher than 240 beats per minute.
WPW Pattern
- WPW pattern is characterized by the following typical EKG findings:
- Short PR interval: The PR interval is short because the ventricles begins to contract earlier than usual because of the electrical signal travels through the accessory pathway faster than the AV node.
- Wide QRS
- delta wave
- QRS alternans
- ST segment depression.
- Preexcitation and presence of delta waves typical of WPW syndrome or WPW pattern may either mimic myocardial infarction or may mask it.[1]
- Abolishment of delta waves may be necessary for the diagnosis of myocardial infarction on EKG.[2]
- Left posterolateral or lateral accessory pathways may mask inferior or anteroseptal myocardial infarction .[3]
- Posteroseptal accessory pathways may mask an anterior MI.[3]
- Right anteroseptal and anterolateral accessory pathways may mask inferior or anterolateral MI.[3]
- Abolishment of delta waves may be necessary for the diagnosis of myocardial infarction on EKG.[2]
Determining the location of the accessory pathway
| V1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| _ | + | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Positive inferior leads | Positive inferior leads | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 0 | 1,2 | 3 | 3 | 1,2 | 0 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| V3 | V3 | V3 | Left lateral | Left posterolateral | V1/1 ratio | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| _ | + | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Right posterior | Right paraseptal | <1 | ≥1 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| _ | + | Lead 2, Notched QS | Left posterolateral | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Right lateral | Nodo-Hisian | Yes | NO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| _ | + | Deep coronary sinus | Left paraseptal | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Nodo-Hisian | Right atrium | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| The above algorithm adopted from 2019 ESC Guideline[4] |
|---|
WPW Syndrome
- WPW syndrome is the occurrence of tachycardia with or without associated symptoms in a subject with existing WPW pattern.[5]
- Several types of arrhythmia can occur in WPW syndrome such as AV reentrant tachycardia (AVRT), atrial fibrillation,or atrial flutter
the most common type of tachyarrhythmia is AVRT.[6]
Orthodromic AVRT
- In orthodromic AVRT, the anterograde conduction (from the atrium to the ventricle) passes through theAV node and the retrograde conduction (from the ventricle to the atrium) passes through the accessory pathway.
- Orthodromic AVRT occurs in approximately 90 to 95% of WPW.
The EKG findings include the following:
- Regular rhythm
- Narrow QRS complexes
- Retrograde P wave following the QRS complex
- Long RP, short PR tachycardia

Antidromic AVRT
- The anterograde conduction (from the atrium to the ventricle) passes through the accessory pathway and the retrograde conduction (from the ventricle to the atrium) passes through the AV node.
- It apprears in less than 10% of WPW.
- The EKG findings may include the following:
- Regular rhythm
- Wide QRS complexes tachycardia
Atrial Fibrillation in WPW
- Atrial fibrillation in WPW syndrome is life-threatening because it might lead to ventricular tachycardia.
- The suggestive findings of [[antidromic AVRT] and rapid atrial fibrillation on the ECG may include the following:
- Irregularly irregular rhythm
- Absent of P wave
- Wide WRS
- Ventricular rate >240 beats per minute[7]
Shown below is an ECG depicting an irregularly irregular rhythm with wide QRS and absent P waves suggestive of atrial fibrillation in WPW syndrome.

Examples
Shown below is an EKG of Wolff-Parkinson-White syndrome demonstrating slurred upstroke of the QRS complex (>110 milli sec), resulting in a delta-wave (arrow). The EKG also shows a short PR interval.

Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG showing a slurred upstroke QRS complex which is best appreciated in the precordial leads and a PR interval of less than 120 ms (short PR interval) suggesting WPW syndrome.

Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating a delta wave in leads V2, I, aVL, with wide QRS complexes and left axis deviation suggesting WPW syndrome.

Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG showing a short PR interval of less than 120 ms, delta waves in leads I, aVF, aVL and chest leads with wide QRS complexes indicating WPW syndrome.

Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
- For more EKG examples of Wolff-Parkinson-White syndrome click Wolff-Parkinson-White syndrome EKG examples here.
References
- ↑ Smolders L, Majidi M, Krucoff MW, Crijns HJ, Wellens HJ, Gorgels AP (2008). "Preexcitation and myocardial infarction: conditions with confusing electrocardiographic manifestations". J Electrocardiol. 41 (6): 679–82. doi:10.1016/j.jelectrocard.2008.05.005. PMID 18602643.
- ↑ Liu R, Chang Q (2013). "The diagnosis of myocardial infarction in the Wolff-Parkinson-White syndrome". Int J Cardiol. 167 (3): 1083–4. doi:10.1016/j.ijcard.2012.10.055. PMID 23157811.
- ↑ 3.0 3.1 3.2 Preminger MW, Callans DJ, Gottlieb CD, Marchlinski FE (1994). "Radiofrequency catheter ablation used to unmask infarction Q waves in Wolff-Parkinson-White syndrome". Am Heart J. 128 (5): 1040–2. PMID 7942468.
- ↑ Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, Calkins H, Corrado D, Deftereos SG, Diller GP, Gomez-Doblas JJ, Gorenek B, Grace A, Ho SY, Kaski JC, Kuck KH, Lambiase PD, Sacher F, Sarquella-Brugada G, Suwalski P, Zaza A (February 2020). "2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC)". Eur Heart J. 41 (5): 655–720. doi:10.1093/eurheartj/ehz467. PMID 31504425.
- ↑ "Wolff-Parkinson-White Syndrome and Accessory Pathways". Retrieved 1 April 2014.
- ↑ "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ Klein, George J.; Bashore, Thomas M.; Sellers, T. D.; Pritchett, Edward L. C.; Smith, William M.; Gallagher, John J. (1979). "Ventricular Fibrillation in the Wolff-Parkinson-White Syndrome". New England Journal of Medicine. 301 (20): 1080–1085. doi:10.1056/NEJM197911153012003. ISSN 0028-4793.