Tuberculosis epidemiology and demographics: Difference between revisions
Tarek Nafee (talk | contribs) |
Mohamed riad (talk | contribs) (→Gender) |
||
| (13 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Tuberculosis}} | {{Tuberculosis}} | ||
{{CMG}}; {{AE}} {{JS}}, {{DN}}, {{TarekNafee}} | {{CMG}}; {{AE}} {{Mashal Awais}}; {{JS}}, {{DN}}, {{TarekNafee}} | ||
==Overview== | ==Overview== | ||
In 2015, about 10.4 million people developed symptomatic TB and 1.8 million died from the disease. In 2014 | In 2019, about 8,920 [[TB]] cases were documented in the US with an [[Incidence (epidemiology)|incidence]] of 2.7 cases/100,000 persons. This represented a decrease by 1.1% from 2018. In 2015, about 10.4 million people developed [[symptomatic]] [[Tuberculosis|TB]] and 1.8 million died from the disease. In 2014, approximately 9,421 cases were documented in the United States, with an [[incidence]] of 3.0 cases/100 000 persons. Since 1990, there has been a decrease in the [[mortality rate]] . [[Tuberculosis|TB]] is more [[prevalent]] in older men. Racial and [[Ethnic group|ethnic]] minorities have a higher [[prevalence]] of TB than non-Hispanic whites. [[coinfection|Coinfection]] with [[HIV]] is an important leading cause of death in [[Tuberculosis|TB]]. In 2015, 60% of the worldwide TB cases were in 6 countries: South Africa, Indonesia, China, Pakistan, India, and Nigeria. The WHO reported 24 other high-burden TB countries including Bangladesh, Korea, Columbia, Cambodia, Congo, Brazil, Ethiopia, Myanmar, Philippines, Thailand, Liberia, Vietnam, Kenya, Central Africa, Russia, Angola, Zimbabwe, Namibia, Mozambique, Tanzania, Sierra Leone, Zambia, Papua New Guinea, and Lesotho.<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref> | ||
==Epidemiology== | ==Epidemiology== | ||
* Worldwide, in 2015, | |||
:* 1.17 million of these cases occurred | *Worldwide, in 2018, there were approximately 10 million individuals with incident TB and about 1.5 million TB-related deaths. | ||
* Worldwide, in 2015, about 1.8 million people died from TB.<ref name=CDC>{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name=WHO>{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | **Approximately 862,000 of these cases were in patients [[coinfected]] with [[Human Immunodeficiency Virus (HIV)|HIV]] <sup>[https://stacks.cdc.gov/view/cdc/99462 <nowiki>[12]</nowiki>]</sup> | ||
:* 400,000 of these cases | *Worldwide, in 2015, approximately 10.4 million people had symptomatic [[Tuberculosis|TB]].<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | ||
*In the United States, | |||
:*1.17 million of these cases occurred were in patients [[coinfected]] with [[HIV]].<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | |||
*Worldwide, in 2015, about 1.8 million people died from [[Tuberculosis|TB]].<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | |||
:*400,000 of these cases were in patients [[coinfected]] with [[HIV]].<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | |||
*In the United States, in 2014, approximately 9,421 cases were reported with an [[incidence]] of 3.0 cases/100 000 persons.<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | |||
==Incidence and Mortality== | ==Incidence and Mortality== | ||
===Worldwide Tuberculosis=== | ===Worldwide Tuberculosis=== | ||
*Over 95% of TB deaths occur in low- and middle-income countries, and it is among the top three causes of death for women aged 15 to 44. | |||
*The TB death rate dropped 45% between 1990 and 2012. | *Over 95% of [[TB]] deaths occur in low- and middle-income countries, and it is among the top three causes of death for women aged 15 to 44. | ||
*The [[Tuberculosis|TB]] death rate dropped 45% between 1990 and 2012. | |||
*In 2015, 3 million lives were saved by the global TB response. | *In 2015, 3 million lives were saved by the global TB response. | ||
<gallery> | <gallery> | ||
File:TB incidence all forms.jpg|Incidence of All Forms of TB in 2015. <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:TB incidence trends.jpg|Trend in TB incidence from 2000 to 2015. <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:TB mortality trends.jpg|TB mortality trends (2000-2015) <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:TBmortality2015.jpg|TB Global Mortality in 2015. <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:Topworldwidecauseofdeath.jpg|''Image 5'' - TB is in the top 10 causes of death in 2015. <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:Screen Shot 2021-01-19 at 8.30.45 PM.png|Trends in Estimated Incident Tuberculosis 2000-2018 (TB)[https://stacks.cdc.gov/view/cdc/99462] | |||
</gallery> | </gallery> | ||
====Global Regional Incidence & Mortality==== | ====Global Regional Incidence & Mortality==== | ||
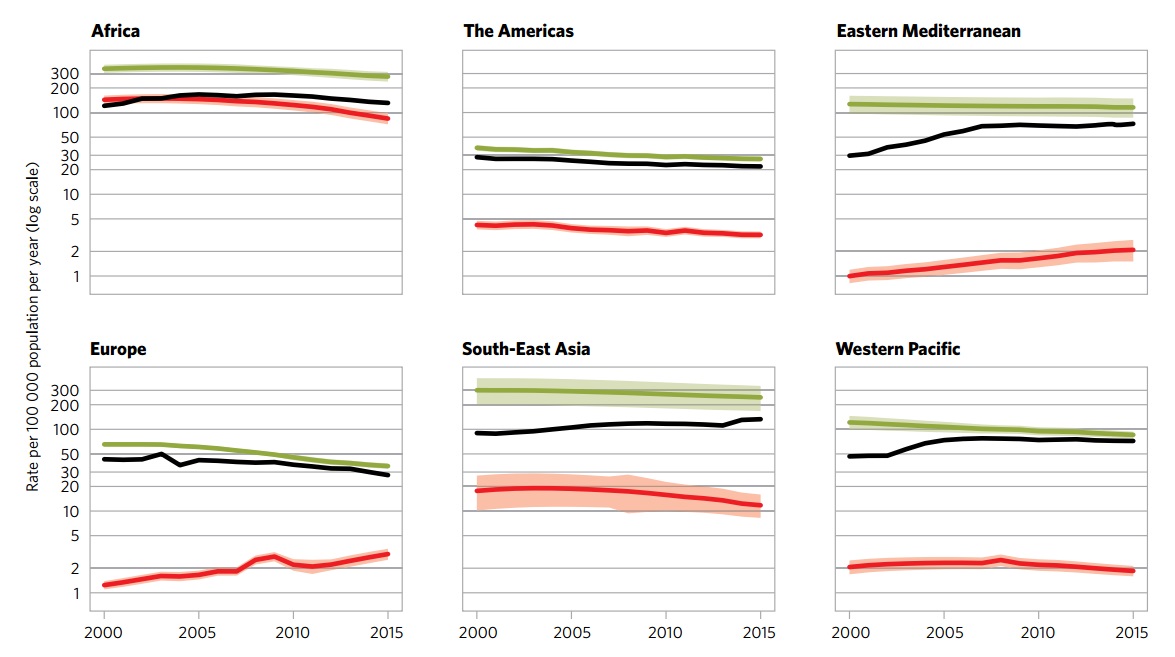
The following global regional trends in TB incidence are observed from 2000 to 2015:<br> | The following global regional trends in TB incidence are observed from 2000 to 2015:<br> | ||
[[Image:Regional incidence trends.jpg|600px]] | [[Image:Regional incidence trends.jpg|600px]] | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 900px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 900px;" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ style="background: #4479BA; color:#FFF | '''Global Incidence and Mortality of Tuberculosis and HIV, By Region''' | |+ style="background: #4479BA; color:#FFF " |'''Global Incidence and Mortality of Tuberculosis and HIV, By Region (2015)''' | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | | ! style="background: #4479BA; color:#FFF; width: 200px;" | | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | African Region | ! style="background: #4479BA; color:#FFF; width: 200px;" |African Region | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | American Region | ! style="background: #4479BA; color:#FFF; width: 200px;" |American Region | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | Eastern Mediterranean Region | ! style="background: #4479BA; color:#FFF; width: 200px;" |Eastern Mediterranean Region | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | European Region | ! style="background: #4479BA; color:#FFF; width: 200px;" |European Region | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | South-East Asian Region | ! style="background: #4479BA; color:#FFF; width: 200px;" |South-East Asian Region | ||
! style="background: #4479BA; color:#FFF; width: 200px;" | Western-Pacific Region | ! style="background: #4479BA; color:#FFF; width: 200px;" |Western-Pacific Region | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Incidence <br> <small>(per 100 000)</small> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Incidence <br> <small>(per 100 000)</small> | ||
| style="padding: 5px 5px; background: #F5F5F5; text-align:right" | 275 | | style="padding: 5px 5px; background: #F5F5F5; text-align:right" |275 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 27 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |27 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 116 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |116 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 36 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |36 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 246 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |246 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 86 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |86 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Incidence of Multi-Drug Resistant TB <br> <small>(per 100 000)</small> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Incidence of Multi-Drug Resistant TB <br> <small>(per 100 000)</small> | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 11 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |11 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 1.1 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |1.1 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 6 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |6 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 14 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |14 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 10 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |10 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 5.5 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |5.5 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Mortality (excluding HIV-TB coinfection) <br> <small>(per 100 000)</small> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Mortality (excluding HIV-TB coinfection) <br> <small>(per 100 000)</small> | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 45 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |45 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 1.9 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |1.9 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 12 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |12 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 3.5 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |3.5 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 37 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |37 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 4.8 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |4.8 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Mortality (only HIV-TB coinfection) <br> <small>(per 100 000)</small> | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 30 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |30 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 0.59 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |0.59 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 0.46 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |0.46 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 0.54 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |0.54 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 3.9 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |3.9 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 0.31 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |0.31 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Total new cases in 2016 | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Total new cases in 2016 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 1 333 504 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |1 333 504 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 230 519 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |230 519 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 484 733 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |484 733 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 297 448 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |297 448 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 2 656 560 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |2 656 560 | ||
| style="padding: 5px 5px; background: #F5F5F5;text-align:right" | 1 361 430 | | style="padding: 5px 5px; background: #F5F5F5;text-align:right" |1 361 430 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | colspan="7" style="padding: 5px 5px; background: #F5F5F5;" |<small> Table adapted from WHO Global Report 2016 <ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref> | ||
|} | |} | ||
| Line 91: | Line 95: | ||
Immunosuppression secondary to HIV is strongly associated with incidence of TB and its subsequent complications. Tuberculosis contributes to a considerable proportion of HIV/AIDS related deaths. | Immunosuppression secondary to HIV is strongly associated with incidence of TB and its subsequent complications. Tuberculosis contributes to a considerable proportion of HIV/AIDS related deaths. | ||
<gallery> | <gallery> | ||
File:TB HIV incidence.jpg|Incidence of TB and HIV in 2015 <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:TrendinTBandHIVdeath.jpg|Trend in TB and HIV mortality (2000-2015) <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
File:HIVandTBdeath2015.jpg|Estimated TB and HIV deaths in 2015 <SMALL><SMALL>''[http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1} - WHO 2016 TB Report)]''<ref name="CDC2">{{Cite web | title = WHO 2016 TB Report | url =http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1}}</ref></SMALL></SMALL> | |||
</gallery> | </gallery> | ||
===Tuberculosis in Endemic Countries=== | ===Tuberculosis in Endemic Countries=== | ||
In 2015, 60% of TB cases | In 2015, 60% of the worldwide TB cases were reported in six countries: | ||
====South Africa==== | ====South Africa==== | ||
*The incidence of tuberculosis | |||
*The mortality of tuberculosis (excluding HIV-TB coinfection) | *The [[Incidence (epidemiology)|incidence]] of [[tuberculosis]] was reported as '''834''' per 100,000 of the general population.<ref name="CDC2"></ref> | ||
*The [[mortality rate]] of [[tuberculosis]] (excluding HIV-TB coinfection) was reported as '''46''' per 100,000 of the general population.<ref name="CDC2"></ref> | |||
====Indonesia==== | ====Indonesia==== | ||
*The incidence of tuberculosis | |||
*The mortality of tuberculosis (excluding HIV-TB coinfection) | *The [[Incidence (epidemiology)|incidence]] of tuberculosis was reported as '''395''' per 100,000 of the overall population.<ref name="CDC2"></ref> | ||
*The [[mortality]] rate of [[tuberculosis]] (excluding [[Human Immunodeficiency Virus (HIV)|HIV]]-[[Tuberculosis|TB]] [[coinfection]]) was reported as '''40''' per 100,000 of the overall population.<ref name="CDC2"></ref> | |||
====Nigeria==== | ====Nigeria==== | ||
*The incidence of tuberculosis | |||
*The mortality of tuberculosis (excluding HIV-TB coinfection) | *The [[incidence]] of [[tuberculosis]] was reported as '''322''' per 100,000 of the general population.<ref name="CDC2"></ref> | ||
*The [[mortality rate]] of [[tuberculosis]] (excluding [[Human Immunodeficiency Virus (HIV)|HIV]]-[[TB coinfection]]) was reported as '''99''' per 100,000 of the general population.<ref name="CDC2"></ref> | |||
====Pakistan==== | ====Pakistan==== | ||
*The incidence of tuberculosis | |||
*The mortality of tuberculosis (excluding HIV-TB coinfection) | *The [[Incidence (epidemiology)|incidence]] of [[tuberculosis]] was reported as '''270''' per 100,000 of the general population.<ref name="CDC2"></ref> | ||
*The [[mortality rate]] of [[tuberculosis]] (excluding [[Human Immunodeficiency Virus (HIV)|HIV]]-TB coinfection) was reported as '''23''' per 100,000 of the general population.<ref name="CDC2"></ref> | |||
====India==== | ====India==== | ||
*The incidence of tuberculosis | |||
*The mortality of tuberculosis (excluding HIV-TB coinfection) | *The [[Incidence (epidemiology)|incidence]] of [[tuberculosis]] was reported as '''217''' per 100,000 of the general population.<ref name="CDC2"></ref> | ||
*The [[mortality rate]] of tuberculosis (excluding [[Human Immunodeficiency Virus (HIV)|HIV]]-TB [[coinfection]]) was reported as '''36''' per 100,000 of the general population.<ref name="CDC2"></ref> | |||
====China==== | ====China==== | ||
*The incidence of tuberculosis | |||
*The mortality of tuberculosis (excluding HIV-TB coinfection) | *The [[Incidence (epidemiology)|incidence]] of tuberculosis was reported as '''67''' per 100,000 of the general population.<ref name="CDC2"></ref> | ||
*The [[mortality rate]] of [[tuberculosis]] (excluding [[Human Immunodeficiency Virus (HIV)|HIV-]]TB [[coinfection]]) was reported as '''2.6''' per 100,000 of the general population.<ref name="CDC2"></ref> | |||
===Tuberculosis in the United States=== | ===Tuberculosis in the United States=== | ||
[[Tuberculosis|TB]] [[resurge]] occurred in the mid-1980s since when the number of [[cases]] steadily increased with a peak occurred in 1992. Following this peak, the number of reported [[Tuberculosis|TB]] cases has decreased annually. The year of 2014 represented the twenty-second year of decline in the [[reported]] [[Tuberculosis|TB]] [[cases]] in the [[United States]] since that peak. In 2014, approximately a total number of 9,421 cases were reported in the 50 states and the District of Columbia (DC). This was considered a [[Decline in amphibian populations|decline]] of 1.5% from 2013. The number of [[Tuberculosis|TB]] cases per 100,000 in 2013 and 2014 was at a stable [[Rate (mathematics)|rate]] of 3.0.<ref name="CDC2">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm}}</ref> | |||
{| | {| | ||
| valign=top | | | valign="top" | | ||
[[Image:US_trend.png|thumb|center|400 px|''Image 1'' - Reported TB Cases United States, 1982–2014<SMALL><SMALL>''[http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm} | [[Image:US_trend.png|thumb|center|400 px|''Image 1'' - Reported TB Cases United States, 1982–2014<SMALL><SMALL>''[http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm} - Center for Disease Control and Prevention(CDC)]''<ref name="CDC2">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm}}</ref></SMALL></SMALL>]] | ||
|style="width: 300px"| | | style="width: 300px" | | ||
| [[Image:US2014.png|thumb|center|400 px|''Image 2'' - TB Case Rates,* United States, 2014<SMALL><SMALL>''[https://http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm} | |[[Image:US2014.png|thumb|center|400 px|''Image 2'' - TB Case Rates,* United States, 2014<SMALL><SMALL>''[https://http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm} - Center for Disease Control and Prevention(CDC)]''<ref name="CDC2">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =http://www.cdc.gov/tb/publications/factsheets/statistics/tbtrends.htm}}</ref></SMALL></SMALL>]] | ||
|} | |} | ||
==Demographics== | ==Demographics== | ||
===Age=== | ===Age=== | ||
In 2014, | In 2014, TB cases in most age groups decreased by approximately 70% from the 1993 values. Below is the comparison between the case rates (per 100 000 persons) of these two years, according to different ages:<ref name="CDC 2014 age"> Center for Disease Control and Prevention http://www.cdc.gov/tb/statistics/reports/2014/pdfs/2014-surveillance-report_table4.pdf </ref> | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Age}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Age}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Case rate in 1993}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Case rate in 1993}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Case rate in 2014}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Case rate in 2014}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |>65 years | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |>65 years | ||
| Line 170: | Line 176: | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |< 15 years | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |< 15 years | ||
| style="padding: 5px 5px; background: #F5F5F5;" |2.9 | | style="padding: 5px 5px; background: #F5F5F5;" |2.9 | ||
| style="padding: 5px 5px; background: #F5F5F5;" |0.8 | | style="padding: 5px 5px; background: #F5F5F5;" |0.8 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5; | | colspan="3" style="padding: 5px 5px; background: #F5F5F5;" |Data provided by the CDC<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref><ref name="CDC 2014 age"> Center for Disease Control and Prevention http://www.cdc.gov/tb/statistics/reports/2014/pdfs/2014-surveillance-report_table4.pdf </ref> | ||
|} | |} | ||
{| | {| | ||
| valign=top | | | valign="top" | | ||
[[Image:age1.png|thumb|center|400 px|''Image 4'' - TB Case Rates* by Age Group United States, 1993–2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf | [[Image:age1.png|thumb|center|400 px|''Image 4'' - TB Case Rates* by Age Group United States, 1993–2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf - Center for Disease Control and Prevention(CDC)]''<ref name="CDC1">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf}}</ref></SMALL></SMALL>]] | ||
|style="width: 300px"| | | style="width: 300px" | | ||
| | |[[Image:age2.png|thumb|center|400 px|''Image 5'' - Reported TB Cases by Age Group, United States, 2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf - Center for Disease Control and Prevention(CDC)]''<ref name="CDC1">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf}}</ref></SMALL></SMALL>]] | ||
|} | |} | ||
Depending on the age of the patient, tuberculosis may have different clinical manifestations, progression, and prognosis:<ref name="pmid3990748">{{cite journal| author=Stead WW, Lofgren JP, Warren E, Thomas C| title=Tuberculosis as an endemic and nosocomial infection among the elderly in nursing homes. | journal=N Engl J Med | year= 1985 | volume= 312 | issue= 23 | pages= 1483-7 | pmid=3990748 | doi=10.1056/NEJM198506063122304 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3990748 }} </ref><ref name="pmid13007533">{{cite journal| author=DAHL RH| title=[The first appearance of a pulmonary cavity after primary infection with relation to time and age]. | journal=Acta Tuberc Scand | year= 1952 | volume= 27 | issue= 1-2 | pages= 140-9 | pmid=13007533 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13007533 }} </ref><ref name="pmid4960690">{{cite journal| author=Stead WW| title=Pathogenesis of a first episode of chronic pulmonary tuberculosis in man: recrudescence of residuals of the primary infection or exogenous reinfection? | journal=Am Rev Respir Dis | year= 1967 | volume= 95 | issue= 5 | pages= 729-45 | pmid=4960690 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4960690 }} </ref><ref name="pmid10764341">{{cite journal| author=| title=Targeted tuberculin testing and treatment of latent tuberculosis infection. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. This is a Joint Statement of the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC). This statement was endorsed by the Council of the Infectious Diseases Society of America. (IDSA), September 1999, and the sections of this statement. | journal=Am J Respir Crit Care Med | year= 2000 | volume= 161 | issue= 4 Pt 2 | pages= S221-47 | pmid=10764341 | doi=10.1164/ajrccm.161.supplement_3.ats600 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10764341 }} </ref><ref name="pmid13007533">{{cite journal| author=DAHL RH| title=[The first appearance of a pulmonary cavity after primary infection with relation to time and age]. | journal=Acta Tuberc Scand | year= 1952 | volume= 27 | issue= 1-2 | pages= 140-9 | pmid=13007533 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13007533 }} </ref><ref name="pmid5642961">{{cite journal| author=Stead WW, Kerby GR, Schlueter DP, Jordahl CW| title=The clinical spectrum of primary tuberculosis in adults. Confusion with reinfection in the pathogenesis of chronic tuberculosis. | journal=Ann Intern Med | year= 1968 | volume= 68 | issue= 4 | pages= 731-45 | pmid=5642961 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5642961 }} </ref> | Depending on the age of the patient, tuberculosis may have different clinical manifestations, progression, and prognosis:<ref name="pmid3990748">{{cite journal| author=Stead WW, Lofgren JP, Warren E, Thomas C| title=Tuberculosis as an endemic and nosocomial infection among the elderly in nursing homes. | journal=N Engl J Med | year= 1985 | volume= 312 | issue= 23 | pages= 1483-7 | pmid=3990748 | doi=10.1056/NEJM198506063122304 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3990748 }} </ref><ref name="pmid13007533">{{cite journal| author=DAHL RH| title=[The first appearance of a pulmonary cavity after primary infection with relation to time and age]. | journal=Acta Tuberc Scand | year= 1952 | volume= 27 | issue= 1-2 | pages= 140-9 | pmid=13007533 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13007533 }} </ref><ref name="pmid4960690">{{cite journal| author=Stead WW| title=Pathogenesis of a first episode of chronic pulmonary tuberculosis in man: recrudescence of residuals of the primary infection or exogenous reinfection? | journal=Am Rev Respir Dis | year= 1967 | volume= 95 | issue= 5 | pages= 729-45 | pmid=4960690 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4960690 }} </ref><ref name="pmid10764341">{{cite journal| author=| title=Targeted tuberculin testing and treatment of latent tuberculosis infection. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. This is a Joint Statement of the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC). This statement was endorsed by the Council of the Infectious Diseases Society of America. (IDSA), September 1999, and the sections of this statement. | journal=Am J Respir Crit Care Med | year= 2000 | volume= 161 | issue= 4 Pt 2 | pages= S221-47 | pmid=10764341 | doi=10.1164/ajrccm.161.supplement_3.ats600 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10764341 }} </ref><ref name="pmid13007533">{{cite journal| author=DAHL RH| title=[The first appearance of a pulmonary cavity after primary infection with relation to time and age]. | journal=Acta Tuberc Scand | year= 1952 | volume= 27 | issue= 1-2 | pages= 140-9 | pmid=13007533 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13007533 }} </ref><ref name="pmid5642961">{{cite journal| author=Stead WW, Kerby GR, Schlueter DP, Jordahl CW| title=The clinical spectrum of primary tuberculosis in adults. Confusion with reinfection in the pathogenesis of chronic tuberculosis. | journal=Ann Intern Med | year= 1968 | volume= 68 | issue= 4 | pages= 731-45 | pmid=5642961 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5642961 }} </ref> | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 750px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 750px;" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF|Factor}} | ! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF|Factor}} | ||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|Influence}} | ! style="background: #4479BA; width: 400px;" |{{fontcolor|#FFF|Influence}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | Infants and Children | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |Infants and Children | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* Younger age (< 5 years) is associated with higher risk of developing progressive disease. | *Younger age (< 5 years) is associated with a higher risk of developing progressive disease. | ||
* Infants are more prone to the development of tuberculosis following infection with ''M. tuberculosis''. | *Infants are more prone to the development of tuberculosis following infection with ''M. tuberculosis''. | ||
* | *Higher risk of [[miliary tuberculosis]]. | ||
* Common involvement of: | *Common involvement of: | ||
:* [[Lymph nodes]] | |||
:* [[Bones]] | :*[[Lymph nodes]] | ||
:* Extrapulmonary foci | :*[[Bones]] | ||
* | :*Extrapulmonary foci | ||
* Cavitary tuberculosis has | |||
*Usually have a good prognosis; spontaneous healing occurs even in the absence of therapy. | |||
*Cavitary tuberculosis has a higher risk of relapse. | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | Adolescents | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |Adolescents | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *The lower regions of the lungs are usually affected with the presentation of [[hilar]] [[adenitis]] | ||
* [[Hilar]] calcification is rare | *[[Hilar]] calcification is rare | ||
* Common in [[immunocompromised]] and dark-skinned patients | *Common in [[immunocompromised]] and dark-skinned patients | ||
* | *In young adults, the disease tends to affect the apical regions of the lung. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | Midadulthood | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |Midadulthood | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* If infection | *If the infection occurs during mid-adulthood, the disease carries a better prognosis, possibly due to the presence of less [[necrotic]] tissue. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | Elderly | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |Elderly | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* Elderly patients have a weaker [[immune system]]. | *Elderly patients have a weaker [[immune system]]. Consequently, latent disease, acquired at younger ages, has a higher risk f progression to active tuberculosis with posterior-apical predominance. | ||
* A | *A lot of elderly patients are [[TST]] negative because they have no prior TB infection; they have lost the immune/hypersensitivity reaction; or because they have completely cleared previous infections. These patients are at risk of reinfection. | ||
* Tuberculosis in | *Tuberculosis in those patients usually presents as middle or lower lobe [[pneumonitis]], rarely with [[pleural effusion]]. | ||
* Similar to childhood | *Similar to tuberculosis in childhood, with less degree of [[lymphadenopathy]] | ||
* Higher death rate | *Higher death rate | ||
|- | |- | ||
|} | |} | ||
===Gender=== | ===Gender=== | ||
In 2012, 410,000 women | In 2012, there were 410,000 total deaths in women as a result of TB in the United States, 160,000 of them were [[HIV]]-positive. Out of the total TB deaths among [[HIV]]-positive people, 50% were women.<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> TB rates tend to increase with age, ranging from a low rate of less than 1 per 100,000 in children aged 5 - 14 to a high rate of 6.9 per 100,000 in men aged 65 years and older. With age increasing, the case rate increases faster in men than in women; the rates in men aged 45 years and older were approximately more than double the case rate in women of the same age.<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/surv/surv2013/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref> | ||
[[Image:ags.png|thumb|right|400 px|''Image 6'' - TB Case Rates by Age Group and Sex, United States, 2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf | [[Image:ags.png|thumb|right|400 px|''Image 6'' - TB Case Rates by Age Group and Sex, United States, 2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf - Center for Disease Control and Prevention(CDC)]''<ref name="CDC1">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url = https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf}}</ref></SMALL></SMALL>]] | ||
===Race=== | ===Race=== | ||
The highest TB rates was | The highest TB rates was reported in Asians, a decline from 29.9 per 100,000 persons in 2003 to 17.8 in 2014.<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/surv/surv2013/default.htm }}</ref><ref name="CDC ethnicity"> Center for Disease Control and Prevention http://www.cdc.gov/tb/statistics/reports/2014/pdfs/2014-surveillance-report_table17.pdf </ref> | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Racial/ethnic groups}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Racial/ethnic groups}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Case rate in 2003}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Case rate in 2003}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Case rate in 2014}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Case rate in 2014}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Non-Hispanic blacks or African-Americans | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Non-Hispanic blacks or African-Americans | ||
| Line 248: | Line 256: | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |American Indians and Alaska Natives | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |American Indians and Alaska Natives | ||
| style="padding: 5px 5px; background: #F5F5F5;" |8.2 | | style="padding: 5px 5px; background: #F5F5F5;" |8.2 | ||
| style="padding: 5px 5px; background: #F5F5F5;" |5.0 | | style="padding: 5px 5px; background: #F5F5F5;" |5.0 | ||
|- | |- | ||
| Line 259: | Line 267: | ||
| style="padding: 5px 5px; background: #F5F5F5;" |16.9 | | style="padding: 5px 5px; background: #F5F5F5;" |16.9 | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5; | | colspan="3" style="padding: 5px 5px; background: #F5F5F5;" |Data provided by the CDC<ref name="CDC">{{cite web | title = Tuberculosis (TB) | url = http://www.cdc.gov/tb/statistics/default.htm }}</ref><ref name="WHO">{{cite web | title = Tuberculosis | url = http://www.who.int/tb/en/ }}</ref><ref name="CDC ethnicity"> Center for Disease Control and Prevention http://www.cdc.gov/tb/statistics/reports/2014/pdfs/2014-surveillance-report_table17.pdf </ref> | ||
|} | |} | ||
The disproportionate burden of [[Tuberculosis|TB]] in minorities is due to many factors. In persons who were born in countries where TB is [[Endemic (epidemiology)|endemic]], the disease can be a result of an acquired [[infection]] in their country of origin. Unequal [[Distribution (pharmacology)|distribution]] of [[Tuberculosis|TB]] [[Risk factor|risk factors]], such as [[HIV]] infection, leads to increased [[Tuberculosis|TB]] exposure or to an increased risk of developing TB after [[infection]] with with [[M. tuberculosis]].<ref name="CDC"> Tuberculosis (TB) http://www.cdc.gov/tb/statistics/surv/surv2013/default.htm</ref> | |||
*Image 7 shows | *Image 7 shows that [[TB]] rates are decreasing by race/ethnicity in the last 12 years.<ref name="CDC1"> Center for Disease Control and Prevention (CDC) https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf</ref> | ||
*Image 8 shows that above the age of 5, there is an increased risk of TB with age across all racial and ethnic groups. | *Image 8 shows that above the age of 5, there is an increased risk of TB with age across all racial and ethnic groups. The case rates were higher in minority racial and ethnic groups than in non-Hispanic whites and were highest in Asians, Native Hawaiians and Other Pacific Islanders, especially in the adult age groups.<ref name="CDC1"> Center for Disease Control and Prevention (CDC) https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf</ref> | ||
*Image 9 shows that in 2014, 85% of all reported TB cases occurred in racial and ethnic minorities, whereas 13% of cases occurred in non-Hispanic whites. Persons reporting two or more races accounted for 2% of all cases<ref name="CDC1">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf}}</ref> | *Image 9 shows that in 2014, 85% of all reported TB cases occurred in racial and ethnic minorities, whereas 13% of cases occurred in non-Hispanic whites. Persons reporting two or more races accounted for 2% of all cases<ref name="CDC1">{{Cite web | title = Center for Disease Control and Prevention (CDC) | url =https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf}}</ref> | ||
{| | {| | ||
| valign=top | | | valign="top" | | ||
[[Image:race_ethnicity.png|thumb|center|400 px|''Image 7'' - TB Case Rates by Race/Ethnicity, United States, 2003–2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf | [[Image:race_ethnicity.png|thumb|center|400 px|''Image 7'' - TB Case Rates by Race/Ethnicity, United States, 2003–2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf - Center for Disease Control and Prevention(CDC)]''<ref name="CDC1"> Center for Disease Control and Prevention (CDC) https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf</ref></SMALL></SMALL>]] | ||
|style="width: 40px"| | | style="width: 40px" | | ||
| | |[[Image:race_ethnicity1.png|thumb|center|400 px|''Image 8'' - TB Case Rates by Age Group and Race/Ethnicity, United States, 2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf - Center for Disease Control and Prevention(CDC)]''<ref name="CDC1"> Center for Disease Control and Prevention (CDC) https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf</ref></SMALL></SMALL>]] | ||
|style="width: 40px"| | | style="width: 40px" | | ||
|[[Image:race_ethnicity2.png|thumb|center|400 px|''Image 9'' - Reported TB Cases by Race/Ethnicity, United States, 2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf | |[[Image:race_ethnicity2.png|thumb|center|400 px|''Image 9'' - Reported TB Cases by Race/Ethnicity, United States, 2014<SMALL><SMALL>''[https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf - Center for Disease Control and Prevention(CDC)]''<ref name="CDC1"> Center for Disease Control and Prevention (CDC) https://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf</ref></SMALL></SMALL>]] | ||
|} | |} | ||
Latest revision as of 05:57, 22 March 2021
|
Tuberculosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberculosis epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Tuberculosis epidemiology and demographics |
|
Risk calculators and risk factors for Tuberculosis epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[3]; João André Alves Silva, M.D. [4], Dima Nimri, M.D. [5], Tarek Nafee, M.D. [6]
Overview
In 2019, about 8,920 TB cases were documented in the US with an incidence of 2.7 cases/100,000 persons. This represented a decrease by 1.1% from 2018. In 2015, about 10.4 million people developed symptomatic TB and 1.8 million died from the disease. In 2014, approximately 9,421 cases were documented in the United States, with an incidence of 3.0 cases/100 000 persons. Since 1990, there has been a decrease in the mortality rate . TB is more prevalent in older men. Racial and ethnic minorities have a higher prevalence of TB than non-Hispanic whites. Coinfection with HIV is an important leading cause of death in TB. In 2015, 60% of the worldwide TB cases were in 6 countries: South Africa, Indonesia, China, Pakistan, India, and Nigeria. The WHO reported 24 other high-burden TB countries including Bangladesh, Korea, Columbia, Cambodia, Congo, Brazil, Ethiopia, Myanmar, Philippines, Thailand, Liberia, Vietnam, Kenya, Central Africa, Russia, Angola, Zimbabwe, Namibia, Mozambique, Tanzania, Sierra Leone, Zambia, Papua New Guinea, and Lesotho.[1]
Epidemiology
- Worldwide, in 2018, there were approximately 10 million individuals with incident TB and about 1.5 million TB-related deaths.
- Approximately 862,000 of these cases were in patients coinfected with HIV [12]
- Worldwide, in 2015, approximately 10.4 million people had symptomatic TB.[2][3]
- 1.17 million of these cases occurred were in patients coinfected with HIV.[2][3]
- 400,000 of these cases were in patients coinfected with HIV.[2][3]
- In the United States, in 2014, approximately 9,421 cases were reported with an incidence of 3.0 cases/100 000 persons.[2][3]
Incidence and Mortality
Worldwide Tuberculosis
- Over 95% of TB deaths occur in low- and middle-income countries, and it is among the top three causes of death for women aged 15 to 44.
- The TB death rate dropped 45% between 1990 and 2012.
- In 2015, 3 million lives were saved by the global TB response.
-
Incidence of All Forms of TB in 2015. - WHO 2016 TB Report)[1]
-
Trend in TB incidence from 2000 to 2015. - WHO 2016 TB Report)[1]
-
TB mortality trends (2000-2015) - WHO 2016 TB Report)[1]
-
TB Global Mortality in 2015. - WHO 2016 TB Report)[1]
-
Image 5 - TB is in the top 10 causes of death in 2015. - WHO 2016 TB Report)[1]
-
Trends in Estimated Incident Tuberculosis 2000-2018 (TB)[1]
Global Regional Incidence & Mortality
The following global regional trends in TB incidence are observed from 2000 to 2015:
| African Region | American Region | Eastern Mediterranean Region | European Region | South-East Asian Region | Western-Pacific Region | |
|---|---|---|---|---|---|---|
| Incidence (per 100 000) |
275 | 27 | 116 | 36 | 246 | 86 |
| Incidence of Multi-Drug Resistant TB (per 100 000) |
11 | 1.1 | 6 | 14 | 10 | 5.5 |
| Mortality (excluding HIV-TB coinfection) (per 100 000) |
45 | 1.9 | 12 | 3.5 | 37 | 4.8 |
| Mortality (only HIV-TB coinfection) (per 100 000) |
30 | 0.59 | 0.46 | 0.54 | 3.9 | 0.31 |
| Total new cases in 2016 | 1 333 504 | 230 519 | 484 733 | 297 448 | 2 656 560 | 1 361 430 |
| Table adapted from WHO Global Report 2016 [1] | ||||||
TB and HIV
Immunosuppression secondary to HIV is strongly associated with incidence of TB and its subsequent complications. Tuberculosis contributes to a considerable proportion of HIV/AIDS related deaths.
-
Incidence of TB and HIV in 2015 - WHO 2016 TB Report)[1]
-
Trend in TB and HIV mortality (2000-2015) - WHO 2016 TB Report)[1]
-
Estimated TB and HIV deaths in 2015 - WHO 2016 TB Report)[1]
Tuberculosis in Endemic Countries
In 2015, 60% of the worldwide TB cases were reported in six countries:
South Africa
- The incidence of tuberculosis was reported as 834 per 100,000 of the general population.[1]
- The mortality rate of tuberculosis (excluding HIV-TB coinfection) was reported as 46 per 100,000 of the general population.[1]
Indonesia
- The incidence of tuberculosis was reported as 395 per 100,000 of the overall population.[1]
- The mortality rate of tuberculosis (excluding HIV-TB coinfection) was reported as 40 per 100,000 of the overall population.[1]
Nigeria
- The incidence of tuberculosis was reported as 322 per 100,000 of the general population.[1]
- The mortality rate of tuberculosis (excluding HIV-TB coinfection) was reported as 99 per 100,000 of the general population.[1]
Pakistan
- The incidence of tuberculosis was reported as 270 per 100,000 of the general population.[1]
- The mortality rate of tuberculosis (excluding HIV-TB coinfection) was reported as 23 per 100,000 of the general population.[1]
India
- The incidence of tuberculosis was reported as 217 per 100,000 of the general population.[1]
- The mortality rate of tuberculosis (excluding HIV-TB coinfection) was reported as 36 per 100,000 of the general population.[1]
China
- The incidence of tuberculosis was reported as 67 per 100,000 of the general population.[1]
- The mortality rate of tuberculosis (excluding HIV-TB coinfection) was reported as 2.6 per 100,000 of the general population.[1]
Tuberculosis in the United States
TB resurge occurred in the mid-1980s since when the number of cases steadily increased with a peak occurred in 1992. Following this peak, the number of reported TB cases has decreased annually. The year of 2014 represented the twenty-second year of decline in the reported TB cases in the United States since that peak. In 2014, approximately a total number of 9,421 cases were reported in the 50 states and the District of Columbia (DC). This was considered a decline of 1.5% from 2013. The number of TB cases per 100,000 in 2013 and 2014 was at a stable rate of 3.0.[1]
 |
 |
Demographics
Age
In 2014, TB cases in most age groups decreased by approximately 70% from the 1993 values. Below is the comparison between the case rates (per 100 000 persons) of these two years, according to different ages:[4]
| Age | Case rate in 1993 | Case rate in 2014 |
|---|---|---|
| >65 years | 17.7 | 4.8 |
| 45 - 64 years | 12.4 | 3.5 |
| 25 - 44 years | 11.5 | 3.4 |
| 15 - 24 years | 5.0 | 2.2 |
| < 15 years | 2.9 | 0.8 |
| Data provided by the CDC[2][3][4] | ||
 |
 |
Depending on the age of the patient, tuberculosis may have different clinical manifestations, progression, and prognosis:[6][7][8][9][7][10]
| Factor | Influence |
|---|---|
| Infants and Children |
|
| Adolescents |
|
| Midadulthood |
|
| Elderly |
|
Gender
In 2012, there were 410,000 total deaths in women as a result of TB in the United States, 160,000 of them were HIV-positive. Out of the total TB deaths among HIV-positive people, 50% were women.[2][3] TB rates tend to increase with age, ranging from a low rate of less than 1 per 100,000 in children aged 5 - 14 to a high rate of 6.9 per 100,000 in men aged 65 years and older. With age increasing, the case rate increases faster in men than in women; the rates in men aged 45 years and older were approximately more than double the case rate in women of the same age.[2][3]

Race
The highest TB rates was reported in Asians, a decline from 29.9 per 100,000 persons in 2003 to 17.8 in 2014.[2][11]
| Racial/ethnic groups | Case rate in 2003 | Case rate in 2014 |
|---|---|---|
| Non-Hispanic blacks or African-Americans | 11.7 | 5.1 |
| Hispanics | 10.3 | 5.0 |
| American Indians and Alaska Natives | 8.2 | 5.0 |
| Non-Hispanic whites | 1.4 | 0.6 |
| Native Hawaiian or Other Pacific Islanders | 16.2 | 16.9 |
| Data provided by the CDC[2][3][11] | ||
The disproportionate burden of TB in minorities is due to many factors. In persons who were born in countries where TB is endemic, the disease can be a result of an acquired infection in their country of origin. Unequal distribution of TB risk factors, such as HIV infection, leads to increased TB exposure or to an increased risk of developing TB after infection with with M. tuberculosis.[2]
- Image 8 shows that above the age of 5, there is an increased risk of TB with age across all racial and ethnic groups. The case rates were higher in minority racial and ethnic groups than in non-Hispanic whites and were highest in Asians, Native Hawaiians and Other Pacific Islanders, especially in the adult age groups.[5]
- Image 9 shows that in 2014, 85% of all reported TB cases occurred in racial and ethnic minorities, whereas 13% of cases occurred in non-Hispanic whites. Persons reporting two or more races accounted for 2% of all cases[5]
 |
 |
 |
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 "WHO 2016 TB Report" (PDF).
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 "Tuberculosis (TB)".
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 "Tuberculosis".
- ↑ 4.0 4.1 Center for Disease Control and Prevention http://www.cdc.gov/tb/statistics/reports/2014/pdfs/2014-surveillance-report_table4.pdf
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 "Center for Disease Control and Prevention (CDC)" (PDF).
- ↑ Stead WW, Lofgren JP, Warren E, Thomas C (1985). "Tuberculosis as an endemic and nosocomial infection among the elderly in nursing homes". N Engl J Med. 312 (23): 1483–7. doi:10.1056/NEJM198506063122304. PMID 3990748.
- ↑ 7.0 7.1 DAHL RH (1952). "[The first appearance of a pulmonary cavity after primary infection with relation to time and age]". Acta Tuberc Scand. 27 (1–2): 140–9. PMID 13007533.
- ↑ Stead WW (1967). "Pathogenesis of a first episode of chronic pulmonary tuberculosis in man: recrudescence of residuals of the primary infection or exogenous reinfection?". Am Rev Respir Dis. 95 (5): 729–45. PMID 4960690.
- ↑ "Targeted tuberculin testing and treatment of latent tuberculosis infection. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. This is a Joint Statement of the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC). This statement was endorsed by the Council of the Infectious Diseases Society of America. (IDSA), September 1999, and the sections of this statement". Am J Respir Crit Care Med. 161 (4 Pt 2): S221–47. 2000. doi:10.1164/ajrccm.161.supplement_3.ats600. PMID 10764341.
- ↑ Stead WW, Kerby GR, Schlueter DP, Jordahl CW (1968). "The clinical spectrum of primary tuberculosis in adults. Confusion with reinfection in the pathogenesis of chronic tuberculosis". Ann Intern Med. 68 (4): 731–45. PMID 5642961.
- ↑ 11.0 11.1 Center for Disease Control and Prevention http://www.cdc.gov/tb/statistics/reports/2014/pdfs/2014-surveillance-report_table17.pdf
![Incidence of All Forms of TB in 2015. - WHO 2016 TB Report)[1]](/images/0/05/TB_incidence_all_forms.jpg)
![Trend in TB incidence from 2000 to 2015. - WHO 2016 TB Report)[1]](/images/d/dd/TB_incidence_trends.jpg)
![TB mortality trends (2000-2015) - WHO 2016 TB Report)[1]](/images/9/94/TB_mortality_trends.jpg)
![TB Global Mortality in 2015. - WHO 2016 TB Report)[1]](/images/3/3d/TBmortality2015.jpg)
![Image 5 - TB is in the top 10 causes of death in 2015. - WHO 2016 TB Report)[1]](/images/6/65/Topworldwidecauseofdeath.jpg)
![Trends in Estimated Incident Tuberculosis 2000-2018 (TB)[1]](/images/c/c2/Screen_Shot_2021-01-19_at_8.30.45_PM.png)
![Incidence of TB and HIV in 2015 - WHO 2016 TB Report)[1]](/images/b/b0/TB_HIV_incidence.jpg)
![Trend in TB and HIV mortality (2000-2015) - WHO 2016 TB Report)[1]](/images/c/c7/TrendinTBandHIVdeath.jpg)
![Estimated TB and HIV deaths in 2015 - WHO 2016 TB Report)[1]](/images/b/b6/HIVandTBdeath2015.jpg)