Tuberculosis CT: Difference between revisions
Jump to navigation
Jump to search
Mashal Awais (talk | contribs) |
Mohamed riad (talk | contribs) |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Pulmonary tuberculosis]] often presents with abnormal findings in a chest [[CT]], which include micronodules, interlobular septal thickening, consolidation, and [[cavitation]]. [[Computed tomography|CT scan]] is more sensitive than an [[X-ray]] to reveal [[lymphadenopathy|lymphadenopathies]]. | |||
==Computed Tomography== | ==Computed Tomography== | ||
===Pulmonary Tuberculosis=== | ===Pulmonary Tuberculosis=== | ||
* | *Abnormal findings on chest CT are seen in most patients with active [[pulmonary tuberculosis.]] | ||
*CT findings include:<ref>{{Cite journal | *[[CT-scans|CT]] findings include:<ref>{{Cite journal | ||
| author = [[Jeong Min Ko]], [[Hyun Jin Park]] & [[Chi Hong Kim]] | | author = [[Jeong Min Ko]], [[Hyun Jin Park]] & [[Chi Hong Kim]] | ||
| title = Pulmonary Changes of Pleural Tuberculosis: Up-to-Date CT Imaging | | title = Pulmonary Changes of Pleural Tuberculosis: Up-to-Date CT Imaging | ||
| Line 20: | Line 20: | ||
}}</ref> | }}</ref> | ||
:*Micronodules | :*[[Micronodules]] | ||
::* | ::*Often present in the [[subpleural]] region and [[peribronchovascular interstitium]]. | ||
::*CT scan | ::*CT scan is helpful for early and accurate detection of [[micronodules.]] | ||
:*Interlobular septal thickening | :*[[Interlobular arteries|Interlobular]] [[septal]] [[thickening]] | ||
:*Cavitation is the most | :*[[Cavitation]] is the most common abnormal finding in secondary [[Tuberculosis/CT|tuberculosis]] | ||
::* | ::*It has thick walls and irregular margins. | ||
::*It may be observed in almost 50% of patients. | ::*It may be observed in almost 50% of patients. | ||
::* | ::*Usually observed in the [[upper]] lung. | ||
::*Cavities in the lower lung | ::*[[Cavity|Cavities]] in the lower [[lung]] may be seen in [[HIV]] [[HIV AIDS|infection]] and [[diabetes]].<ref name="PatelRami2011">{{cite journal|last1=Patel|first1=AnandK|last2=Rami|first2=KiranC|last3=Ghanchi|first3=FerozD|title=Radiological presentation of patients of pulmonary tuberculosis with diabetes mellitus|journal=Lung India|volume=28|issue=1|year=2011|pages=70|issn=0970-2113|doi=10.4103/0970-2113.76308}}</ref><ref name="PadyanaBhat2012">{{cite journal|last1=Padyana|first1=Mahesha|last2=Bhat|first2=RaghavendraV|last3=Dinesha|first3=M|last4=Nawaz|first4=Alam|title=HIV-Tuberculosis: A Study of Chest X-Ray Patterns in Relation to CD4 Count|journal=North American Journal of Medical Sciences|volume=4|issue=5|year=2012|pages=221|issn=1947-2714|doi=10.4103/1947-2714.95904}}</ref> | ||
::* | ::*Despite being rare, [[superinfected|superinfection]] of the [[cavities]] may occur and an air-fluid level is seen inside the [[cavity]]. | ||
::* | ::*Following the [[resolution]] the active [[infection]], small cavities with may persist as a [[residual]] [[finding]]. | ||
:*Homogeneous and dense consolidation | :*Homogeneous and dense consolidation | ||
*CT is more sensitive to detect hilar lymphadenopathy. | *CT is more sensitive to detect hilar lymphadenopathy. | ||
*The "tree-in-bud" sign is | *The "tree-in-bud" [[Sign (medicine)|sign]] is an abnormal characteristic finding on [[Computed tomography|CT scan]] that may be observed in [[pulmonary tuberculosis]] due to [[mucus]] or [[pus]] [[impaction]] into the small [[Airway|airways]] which accentuates the branching course of [[peripheral]] [[Airway|airways]].<ref name="Eisenhuber2002">{{cite journal|last1=Eisenhuber|first1=Edith|title=The Tree-in-Bud Sign1|journal=Radiology|volume=222|issue=3|year=2002|pages=771–772|issn=0033-8419|doi=10.1148/radiol.2223991980}}</ref> | ||
{| | {| | ||
Revision as of 23:02, 26 March 2021
|
Tuberculosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberculosis CT On the Web |
|
American Roentgen Ray Society Images of Tuberculosis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2]; Alejandro Lemor, M.D. [3]
Overview
Pulmonary tuberculosis often presents with abnormal findings in a chest CT, which include micronodules, interlobular septal thickening, consolidation, and cavitation. CT scan is more sensitive than an X-ray to reveal lymphadenopathies.
Computed Tomography
Pulmonary Tuberculosis
- Abnormal findings on chest CT are seen in most patients with active pulmonary tuberculosis.
- CT findings include:[1]
-
- Often present in the subpleural region and peribronchovascular interstitium.
- CT scan is helpful for early and accurate detection of micronodules.
- Interlobular septal thickening
- Cavitation is the most common abnormal finding in secondary tuberculosis
- It has thick walls and irregular margins.
- It may be observed in almost 50% of patients.
- Usually observed in the upper lung.
- Cavities in the lower lung may be seen in HIV infection and diabetes.[2][3]
- Despite being rare, superinfection of the cavities may occur and an air-fluid level is seen inside the cavity.
- Following the resolution the active infection, small cavities with may persist as a residual finding.
- Homogeneous and dense consolidation
- CT is more sensitive to detect hilar lymphadenopathy.
- The "tree-in-bud" sign is an abnormal characteristic finding on CT scan that may be observed in pulmonary tuberculosis due to mucus or pus impaction into the small airways which accentuates the branching course of peripheral airways.[4]
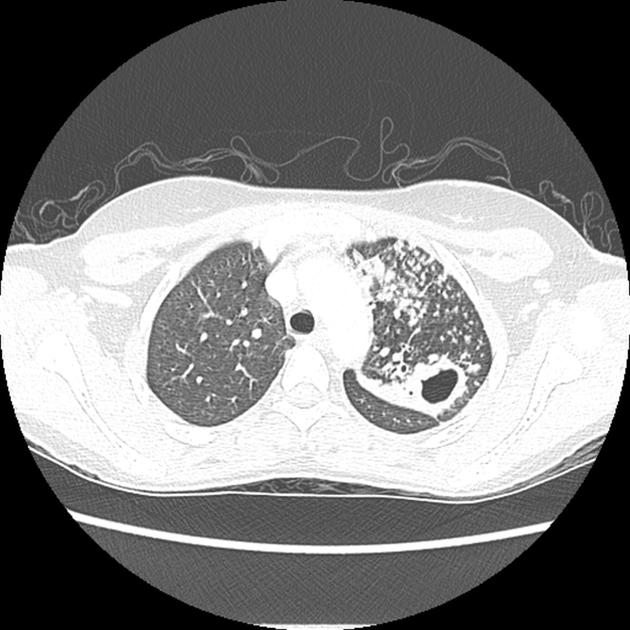 Image courtesy of Dr Natalie Yang, Radiopedia. (original file here) Creative Commons BY-SA-NC |
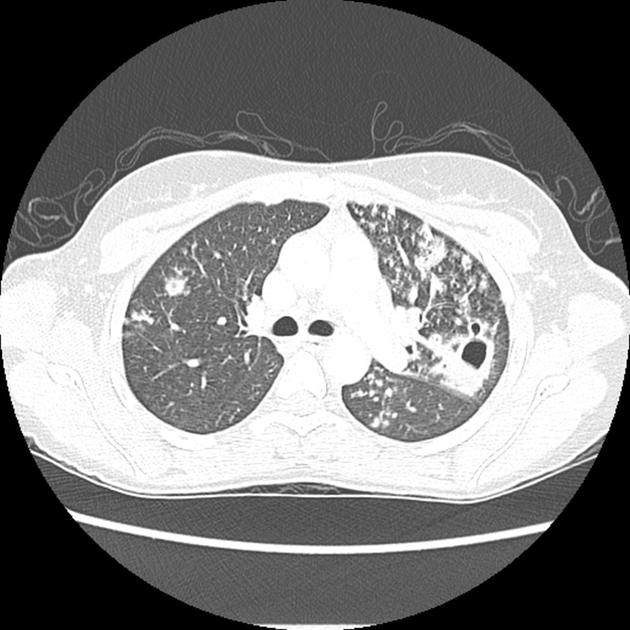 Image courtesy of Dr Natalie Yang, Radiopedia. (original file here) Creative Commons BY-SA-NC |
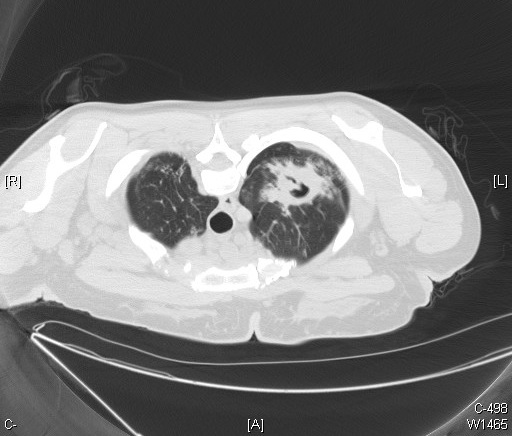 Image courtesy of Wikimedia Commons. |
Extrapulmonary Tuberculosis
Cardiac Tuberculosis
- Pericardial thickening may be seen on a CT scan, specially if it is more than 3 mm.[5]
- Lymph node enlargement is also a common CT finding in cardiac tuberculosis.[5]
- Pericardial effusion is rare and is seen in less than 20% of patients.[5]
Miliary Tuberculosis
CT findings include multiple pulmonary nodules with a diameter of 1-2mm, distributed in a random pattern sometimes presenting with pleural effusion as well.
 Image courtesy of Dr Frank Gaillard, Radiopedia. (original file here) Creative Commons BY-SA-NC |
 Image courtesy of Dr Frank Gaillard, Radiopedia. (original file here) Creative Commons BY-SA-NC |
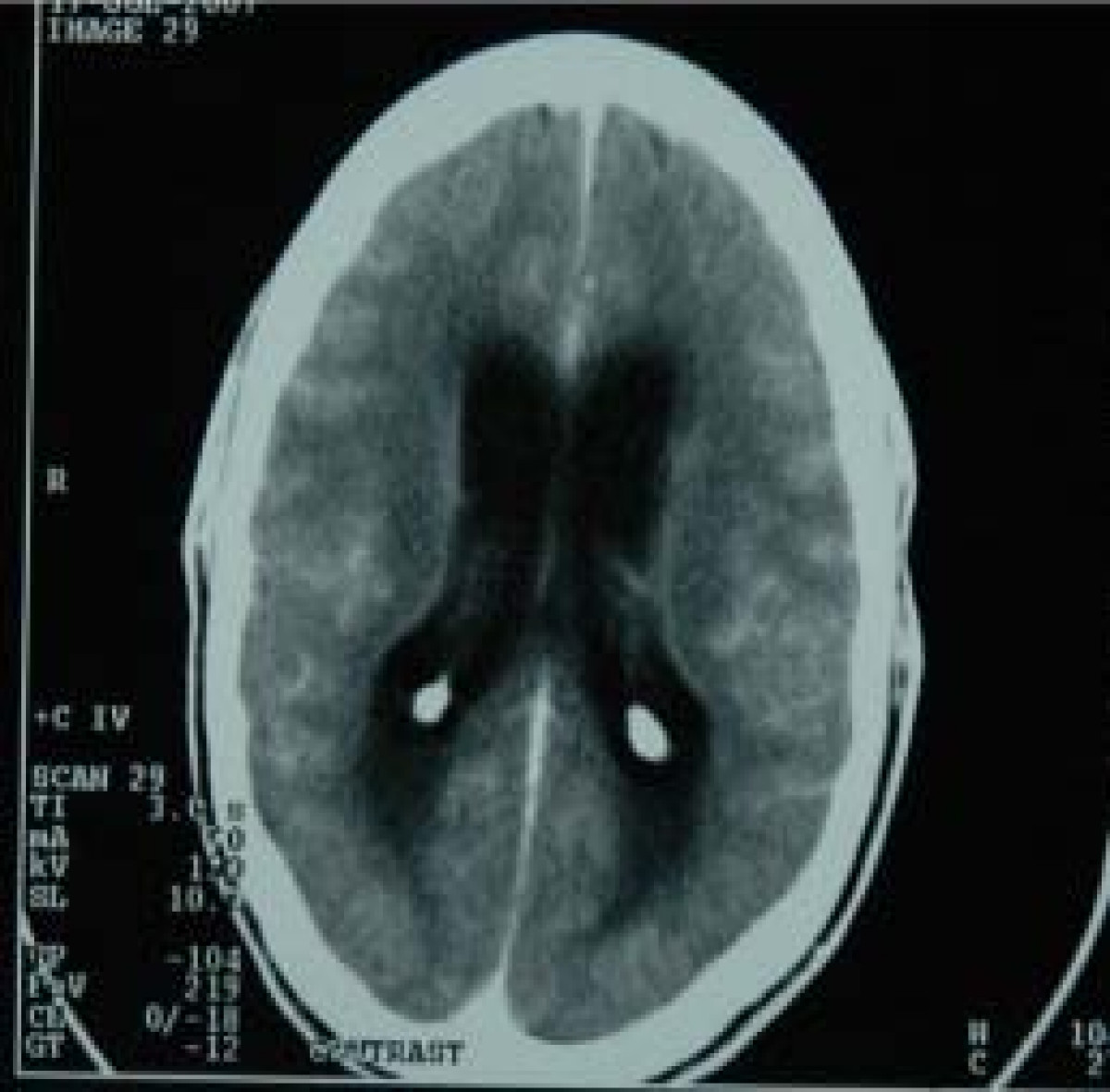
Tuberculous Meningitis
- Head CT findings in tuberculous meningitis include meningeal enhancement indicating meningeal inflammation and choroidal calcifications.[6]
- Areas of infarction and hemorrhage may also be seen in cases of miliary tuberculosis.
- Patients with late complications may show hydrocephalus.
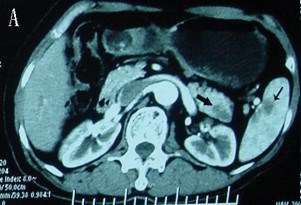
Abdominal Tuberculosis
- CT findings in a pancreatic and spleen infection with tuberculosis may mimic a pancreatic cancer.[7]
- Shown below there is a CT scan of the pancreas demonstrating a mass in the pancreatic tail and metastasizes in the spleen.
 |
 |
References
- ↑ Jeong Min Ko, Hyun Jin Park & Chi Hong Kim (2014). "Pulmonary Changes of Pleural Tuberculosis: Up-to-Date CT Imaging". Chest. doi:10.1378/chest.14-0196. PMID 25086249. Unknown parameter
|month=ignored (help) - ↑ Patel, AnandK; Rami, KiranC; Ghanchi, FerozD (2011). "Radiological presentation of patients of pulmonary tuberculosis with diabetes mellitus". Lung India. 28 (1): 70. doi:10.4103/0970-2113.76308. ISSN 0970-2113.
- ↑ Padyana, Mahesha; Bhat, RaghavendraV; Dinesha, M; Nawaz, Alam (2012). "HIV-Tuberculosis: A Study of Chest X-Ray Patterns in Relation to CD4 Count". North American Journal of Medical Sciences. 4 (5): 221. doi:10.4103/1947-2714.95904. ISSN 1947-2714.
- ↑ Eisenhuber, Edith (2002). "The Tree-in-Bud Sign1". Radiology. 222 (3): 771–772. doi:10.1148/radiol.2223991980. ISSN 0033-8419.
- ↑ 5.0 5.1 5.2 Burrill, Joshua; Williams, Christopher J.; Bain, Gillian; Conder, Gabriel; Hine, Andrew L.; Misra, Rakesh R. (2007). "Tuberculosis: A Radiologic Review1". RadioGraphics. 27 (5): 1255–1273. doi:10.1148/rg.275065176. ISSN 0271-5333.
- ↑ Komolafe, Morenikeji A; Sunmonu, Taofiki A; Esan, Olufunmi A (2008). "Tuberculous meningitis presenting with unusual clinical features in Nigerians: Two case reports". Cases Journal. 1 (1): 180. doi:10.1186/1757-1626-1-180. ISSN 1757-1626.
- ↑ Rong, YF; Lou, WH; Jin, DY (2008). "Pancreatic tuberculosis with splenic tuberculosis mimicking advanced pancreatic cancer with splenic metastasizes: a case report". Cases Journal. 1 (1): 84. doi:10.1186/1757-1626-1-84. ISSN 1757-1626.