Tisagenlecleucel: Difference between revisions
No edit summary |
No edit summary |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
|genericName=generic name | |genericName=generic name | ||
|aOrAn=a | |aOrAn=a | ||
|drugClass= | |drugClass=[[CD19]]-directed genetically modified autologous [[T-cell]] [[immunotherapy]] | ||
|indicationType= | |indicationType=treatment | ||
|indication= | |indication=patients up to 25 years of age with [[B-cell]] precursor [[acute lymphoblastic leukemia]] (ALL) that is refractory or in second or later relapse and adult patients with relapsed or refractory (r/r) large B-cell [[lymphoma]] after two or more lines of [[systemic therapy]] including [[diffuse large B-cell lymphoma]] (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from [[follicular lymphoma]]. | ||
|hasBlackBoxWarning=Yes | |hasBlackBoxWarning=Yes | ||
|adverseReactions= | |adverseReactions=[[cytokine release syndrome]], [[hypogammaglobulinemia]], [[infection]]s-[[pathogen]] unspecified, [[pyrexia]], decreased appetite, [[headache]], [[encephalopathy]], [[hypotension]], [[bleeding]] episodes, [[tachycardia]], [[nausea]], [[diarrhea]], [[vomiting]], [[viral]] [[infectious]] [[disorder]]s, [[hypoxia]], [[fatigue]], [[acute kidney injury]], [[edema]], [[cough]], [[delirium]] | ||
|blackBoxWarningTitle=CYTOKINE RELEASE SYNDROME AND NEUROLOGICAL TOXICITIES | |blackBoxWarningTitle=CYTOKINE RELEASE SYNDROME AND NEUROLOGICAL TOXICITIES | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;"> | |blackBoxWarningBody=<i><span style="color:#FF0000;"> | ||
*Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving | *Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving Tisagenlecleucel. Do not administer Tisagenlecleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids. | ||
*Neurological toxicities, which may be severe or life-threatening, can occur following treatment with | *Neurological toxicities, which may be severe or life-threatening, can occur following treatment with Tisagenlecleucel, including concurrently with CRS. Monitor for neurological events after treatment with Tisagenlecleucel. Provide supportive care as needed. | ||
* | *Tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Tisagenlecleucel REMS. | ||
|fdaLIADAdult====== | |fdaLIADAdult======Indications:===== | ||
* | *Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of: | ||
=====Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)===== | |||
*Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. | |||
=====Adult Relapsed or Refractory (r/r) Diffuse Large B-Cell Lymphoma (DLBCL)===== | |||
*Adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma. | |||
=====Dosage in Adult Relapsed or Refractory (r/r) Diffuse Large B-cell lymphoma (DLBCL)===== | |||
* | *Tisagenlecleucel is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells. | ||
* | :*For adult patients: administer 0.6 to 6.0 x 108 CAR-positive viable T cells. | ||
|offLabelAdultGuideSupport=There is limited information regarding Tisagenlecleucel ''Off-Label Guideline-Supported Use and Dosage (Adult)'' in the drug label. | |||
|offLabelAdultNoGuideSupport=There is limited information regarding Tisagenlecleucel ''Off-Label Non-Guideline-Supported Use and Dosage (Adult)'' in the drug label. | |||
===== | |fdaLIADPed======Indications:===== | ||
* | *Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of: | ||
=====Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)===== | |||
* | *Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. | ||
=====Adult Relapsed or Refractory (r/r) Diffuse Large B-Cell Lymphoma (DLBCL)===== | |||
*Adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma. | |||
=====Dosage in Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)===== | |||
*Tisagenlecleucel is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells. | |||
*Based on the patient weight reported at the time of leukapheresis: | |||
* | :*Patients 50 kg or less: administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight. | ||
:* | :*Patients above 50 kg: administer 0.1 to 2.5 x 108 CAR-positive viable T cells. | ||
= | |offLabelPedGuideSupport=There is limited information regarding Tisagenlecleucel ''Off-Label Guideline-Supported Use and Dosage (Pediatric)'' in the drug label. | ||
|offLabelPedNoGuideSupport=There is limited information regarding Tisagenlecleucel ''Off-Label Non-Guideline-Supported Use and Dosage (Pediatric)'' in the drug label. | |||
|contraindications=*None | |||
| | |warnings======Cytokine Release Syndrome (CRS)===== | ||
* | *CRS, including fatal or life-threatening reactions, occurred following treatment with Tisagenlecleucel. CRS occurred in 54 (79%) of the 68 pediatric and young adult patients with r/r ALL and 78 (74%) of the 106 adult patients with r/r DLBCL receiving Tisagenlecleucel, including ≥ Grade 3 (Penn grading system1) in 49% of patients with r/r ALL and in 23% of patients with r/r DLBCL. The median time to onset was 3 days (range: 1-51), and in only two patients was onset after Day 10. The median time to resolution of CRS was 8 days (range: 1-36). | ||
*Of the 54 patients with r/r ALL who had CRS, 27 (50%) received tocilizumab. Seven (13%) patients received two doses of tocilizumab, 3 (6%) patients received three doses of tocilizumab, and 14 (26%) patients received addition of corticosteroids (e.g., methylprednisolone). Of the 78 patients with r/r DLBCL who had CRS, 16 (21%) received systemic tocilizumab or corticosteroids. Six (8%) patients received a single dose of tocilizumab, 10 (13%) patients received two doses of tocilizumab, and 10 (13%) patients received corticosteroids in addition to tocilizumab. Two patients with r/r DLBCL received corticosteroids for CRS without concomitant tocilizumab, and two patients received corticosteroids for persistent neurotoxicity after resolution of CRS. | |||
*Five deaths occurred within 30 days of Tisagenlecleucel infusion. One patient with r/r ALL died with CRS and progressive leukemia, and one patient had resolving CRS with abdominal compartment syndrome, coagulopathy, and renal failure when an intracranial hemorrhage occurred. Of the 3 r/r DLBCL patients who died within 30 days of infusion, all had CRS in the setting of stable to progressive underlying disease, one of whom developed bowel necrosis. Among patients with CRS, key manifestations include fever (92% in r/r ALL and r/r DLBCL), hypotension (67% in r/r ALL; 47% in r/r DLBCL), hypoxia (20% in r/r ALL; 35% in r/r DLBCL) and tachycardia (30% in r/r ALL; 14% in r/r DLBCL). CRS may be associated with hepatic, renal, and cardiac dysfunction, and coagulopathy. | |||
* | *Delay the infusion of Tisagenlecleucel after lymphodepleting chemotherapy if the patient has unresolved serious adverse reactions from preceding chemotherapies (including pulmonary toxicity, cardiac toxicity, or hypotension), active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden. | ||
*Ensure that two doses of tocilizumab are available on site prior to infusion of Tisagenlecleucel. Monitor patients for signs or symptoms of CRS for at least 4 weeks after treatment with Tisagenlecleucel. Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time. At the first sign of CRS, immediately evaluate patient for hospitalization and institute treatment with supportive care, tocilizumab and/or corticosteroids as indicated. | |||
* | *Risk factors for severe CRS in the pediatric and young adult r/r B-cell ALL population are high pre-infusion tumor burden (greater than 50% blasts in bone marrow), uncontrolled or accelerating tumor burden following lymphodepleting chemotherapy, active infections, and/or inflammatory processes. Risk factors for developing severe CRS in adult r/r DLBCL are not known. | ||
=====Neurological Toxicities===== | |||
* | *Neurological toxicities including severe or life-threatening reactions, occurred in 49 (72%) of the 68 patients with r/r ALL and 62 (58%) of the 106 patients with r/r DLBCL following treatment with Tisagenlecleucel, including ≥ Grade 3 in 21% of patients with r/r ALL and 18% of patients with r/r DLBCL. Among patients who had a neurological toxicity, 88% occurred within 8 weeks following Tisagenlecleucel infusion. | ||
* | *Median time to the first event was 6 days from infusion (range: 1-359), and the median duration was 6 days for patients with r/r ALL and 14 days for patients with r/r DLBCL. Resolution occurred within 3 weeks in 79% of patients with r/r ALL and 61% of patients with r/r DLBCL. Encephalopathy lasting up to 50 days was noted. | ||
*The onset of neurological toxicity can be concurrent with CRS, following resolution of CRS or in the absence of CRS. | |||
*The most common neurological toxicities observed with Tisagenlecleucel include headache (37% in r/r ALL; 21% in r/r DLBCL), encephalopathy (34% in r/r ALL; 16% in r/r DLBCL), delirium (21% in r/r ALL; 6% in r/r DLBCL), anxiety (13% in r/r ALL; 9% in r/r DLBCL), sleep disorders (10% in r/r ALL; 9% in r/r DLBCL), dizziness (6% in r/r ALL; 11% in r/r DLBCL), tremor (9% in r/r ALL; 7% r/r DLBCL) and peripheral neuropathy (4% in r/r ALL; 8% in r/r DLBCL). Other manifestations included seizures, mutism and aphasia. | |||
* | *Monitor patients for neurological events and exclude other causes for neurological symptoms. Provide supportive care as needed for Tisagenlecleucel-associated neurological events. | ||
=====Tisagenlecleucel REMS to Mitigate Cytokine Release Syndrome and Neurological Toxicities===== | |||
* | *Because of the risk of CRS and neurological toxicities, Tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Tisagenlecleucel REMS. The required components of the Tisagenlecleucel REMS are: | ||
* | :*Healthcare facilities that dispense and administer Tisagenlecleucel must be enrolled and comply with the REMS requirements. Certified healthcare facilities must have on-site, immediate access to tocilizumab, and ensure that a minimum of two doses of tocilizumab are available for each patient for administration within 2 hours after Tisagenlecleucel infusion, if needed for treatment of CRS. | ||
:* | :*Certified healthcare facilities must ensure that healthcare providers who prescribe, dispense or administer Tisagenlecleucel are trained about the management of CRS and neurological toxicities. | ||
=====Hypersensitivity Reactions===== | |||
*Allergic reactions may occur with infusion of Tisagenlecleucel. Serious hypersensitivity reactions, including anaphylaxis, may be due to the dimethyl sulfoxide (DMSO) or dextran 40 in Tisagenlecleucel. | |||
===== | =====Serious Infections===== | ||
* | *Infections, including life-threatening or fatal infections, occurred in 95 (55%) of 174 patients with r/r ALL or r/r DLBCL after Tisagenlecleucel infusion. Fifty eight patients (33%) experienced Grade ≥ 3 infections, including fatal infections in 2 patients (3%) with r/r ALL and 1 patient (1%) with r/r DLBCL. Prior to Tisagenlecleucel infusion, infection prophylaxis should follow local guidelines. Patients with active uncontrolled infection should not start Tisagenlecleucel treatment until the infection is resolved. Monitor patients for signs and symptoms of infection after treatment with Tisagenlecleucel and treat appropriately. | ||
*Febrile neutropenia (≥ Grade 3) was also observed in 37% of patients with r/r ALL and 17% of patients with r/r DLBCL after Tisagenlecleucel infusion and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage with broad spectrum antibiotics, fluids and other supportive care as medically indicated. | |||
''Viral Reactivation'' | |||
* | *Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure and death, can occur in patients treated with drugs directed against B cells. | ||
*Perform screening for HBV, HCV, and HIV in accordance with clinical guidelines before collection of cells for manufacturing. | |||
=====Prolonged Cytopenias===== | |||
*Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and Tisagenlecleucel infusion. | |||
( | *In the ELIANA study (Study 1), ≥ Grade 3 cytopenias not resolved by Day 28 following Tisagenlecleucel treatment included neutropenia (40%), and thrombocytopenia (27%) among 52 responding patients. At 56 days following Tisagenlecleucel, 17% and 12% of responding patients had ≥ Grade 3 neutropenia or thrombocytopenia respectively. | ||
*In the JULIET study (Study 2), ≥ Grade 3 cytopenias not resolved by Day 28 following Tisagenlecleucel treatment included thrombocytopenia (40%) and neutropenia (25%) among 106 treated patients. | |||
*Prolonged neutropenia has been associated with increased risk of infection. Myeloid growth factors, particularly GM-CSF, are not recommended during the first 3 weeks after Tisagenlecleucel infusion or until CRS has resolved. | |||
=====Hypogammaglobulinemia===== | |||
*Hypogammaglobulinemia and agammaglobulinemia (IgG) related to B-cell aplasia can occur in patients with a complete remission (CR) after Tisagenlecleucel infusion. | |||
*Hypogammaglobulinemia was reported in 43% of patients treated with Tisagenlecleucel for r/r ALL and 14% of patients with r/r DLBCL. | |||
*Monitor immunoglobulin levels after treatment with Tisagenlecleucel and manage using infection precautions, antibiotic prophylaxis and immunoglobulin replacement standard guidelines. | |||
''Immunization with Live Vaccine'' | |||
*The safety of immunization with live viral vaccines during or following Tisagenlecleucel treatment has not been studied. Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during Tisagenlecleucel treatment, and until immune recovery following treatment with Tisagenlecleucel. | |||
*Pregnant women who have received Tisagenlecleucel may have hypogammaglobulinemia. Assess immunoglobulin levels in newborns of mothers treated with Tisagenlecleucel. | |||
===== | =====Secondary Malignancies===== | ||
*Patients treated with Tisagenlecleucel may develop secondary malignancies or recurrence of their cancer. Monitor life-long for secondary malignancies. | |||
=====Effects on Ability to Drive and Use Machines===== | |||
*Due to the potential for neurological events, including altered mental status or seizures, patients receiving Tisagenlecleucel are at risk for altered or decreased consciousness or coordination in the 8 weeks following Tisagenlecleucel infusion. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, during this initial period. | |||
|clinicalTrials=*Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |||
*The safety data described in the WARNINGS AND PRECAUTIONS and in this section reflect exposure to Tisagenlecleucel in two non-randomized, single-arm studies in which 68 pediatric and young adult patients with relapsed/refractory (r/r) B-cell ALL (ELIANA Study) and 106 adults with r/r diffuse large B-cell lymphoma (JULIET Study) received a single dose of CAR-positive viable T cells. | |||
''Pediatric and Young Adult r/r B-cell Acute Lymphoblastic Leukemia (ALL) (up to 25 years of age)'' | |||
*Based on a recommended dose which was weight-based, all 68 patients in the ELIANA study (Study 1) received a single intravenous dose of Tisagenlecleucel [see Clinical Studies (14.1)]. The most common adverse reactions (> 20%) were cytokine release syndrome (79%), hypogammaglobulinemia (43%), infections-pathogen unspecified (41%), pyrexia (40%), decreased appetite (37%), headache (37%), encephalopathy (34%), hypotension (31%), bleeding episodes (31%), tachycardia (26%), nausea (26%), diarrhea (26%), vomiting (26%), viral infectious disorders (26%), hypoxia (24%), fatigue (25%), acute kidney injury (24%), edema (21%), cough (21%), and delirium (21%). | |||
*The adverse reactions with greater or equal to 10% incidence for any Grade are summarized in Table 2. | |||
: | [[image:Tisagenlecleucel_Adverse_Reactions_Tables_1_and_2.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
Laboratory Abnormalities | |||
*Selected laboratory abnormalities worsening from baseline Grade 0-2 to Grade 3-4 are shown in Table 3. | |||
[[image:Tisagenlecleucel_Adverse_Reactions_Table_3.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
*All patients experienced neutropenia, anemia and thrombocytopenia. See Table 4 for the incidences of ≥ Grade 3 prolonged thrombocytopenia and prolonged neutropenia in responding patients. | |||
[[image:Tisagenlecleucel_Adverse_Reactions_Table_4.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
''Adult r/r Diffuse Large B-cell Lymphoma (DLBCL)'' | |||
*In the JULIET study (Study 2) 106 adults with r/r DLBCL received a single intravenous dose of Tisagenlecleucel. The most common adverse reactions (incidence > 20%) were cytokine release syndrome, infections-pathogen unspecified, diarrhea, nausea, pyrexia, fatigue, hypotension, edema and headache. | |||
: ( | *The study population characteristics were: median age of 56 years (range: 22 to 76 years), 79% DLBCL; a median of 3 prior lines of therapy (range: 1-6), 49% had a prior autologous hematopoietic stem cell transplantation, and 33% had received prior radiation therapy. Ninety-nine patients (93%) received lymphodepleting chemotherapy prior to Tisagenlecleucel, that included fludarabine (n = 77) or bendamustine (n = 22). | ||
*The adverse reactions with greater than or equal to 10% incidence for any Grade are summarized in Table 5 below. | |||
[[image:Tisagenlecleucel_Adverse_Reactions_Tables_5_and_6.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
Laboratory Abnormalities | |||
*Selected laboratory abnormalities worsening from baseline Grade 0-2 to Grade 3-4 are shown in Table 6. | |||
[[image:Tisagenlecleucel_Adverse_Reactions_Table_7.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
=====Immunogenicity===== | |||
*In clinical studies, humoral immunogenicity of Tisagenlecleucel was measured by determination of anti-murine CAR19 antibodies (anti-mCAR19) in serum pre- and post-administration. The majority of patients, 86% in ELIANA (Study 1) and 91.4% in JULIET (Study 2) tested positive for pre-dose anti-mCAR19 antibodies prior to Tisagenlecleucel infusion; Treatment induced anti-mCAR19 antibodies were detected in 5% of the patients in JULIET. However, the preexisting and treatment-induced antibodies were not associated with an impact on clinical response and did not have an impact on the initial expansion and persistence of Tisagenlecleucel. Persistence of Tisagenlecleucel was similar between patients with positive post-infusion anti-mCAR19 antibodies compared with patients with negative post-infusion anti-mCAR19 antibodies. There is no evidence that the presence of preexisting and treatment-induced anti-mCAR19 antibodies impact the safety or effectiveness of Tisagenlecleucel. | |||
*T cell immunogenicity responses were not observed in adult r/r DLBCL patients. | |||
|postmarketing= | |||
|drugInteractions=*HIV and the lentivirus used to make Tisagenlecleucel have limited, short spans of identical genetic material (RNA). Therefore, some commercial HIV nucleic acid test (NATs) tests may yield false-positive results in patients who have received Tisagenlecleucel. | |||
| | |||
|useInPregnancyFDA=Risk Summary | |||
*There are no available data with Tisagenlecleucel use in pregnant women. No animal reproductive and developmental toxicity studies have been conducted with Tisagenlecleucel to assess whether it can cause fetal harm when administered to a pregnant woman. It is not known if Tisagenlecleucel has the potential to be transferred to the fetus. Based on the mechanism of action, if the transduced cells cross the placenta, they may cause fetal toxicity, including B-cell lymphocytopenia. Therefore, Tisagenlecleucel is not recommended for women who are pregnant, and pregnancy after Tisagenlecleucel administration should be discussed with the treating physician. Report pregnancies to Novartis Pharmaceuticals Corporation at 1-888-669-6682. | |||
*In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively. | |||
== | |useInLaborDelivery= | ||
|useInNursing=Risk Summary | |||
*There is no information regarding the presence of Tisagenlecleucel in human milk, the effect on the breastfed infant, and the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Tisagenlecleucel and any potential adverse effects on the breastfed infant from Tisagenlecleucel or from the underlying maternal condition. | |||
| | |useInPed=*The safety and efficacy of Tisagenlecleucel have been established in pediatric patients with r/r B-cell ALL. Use of Tisagenlecleucel is supported by a single-arm trial [see Clinical Studies (14.1)] that included 52 pediatric patients with r/r B-cell precursor ALL in the following age groups: 33 children (age 3 years to less than 12 years) and 19 adolescents (age 12 years to less than 17 years). No differences in efficacy or safety were observed between the different age subgroups or in comparison to the young adults in the trial. | ||
*The safety and efficacy of Tisagenlecleucel in pediatric patients with relapsed or refractory DLBCL has not been established. | |||
|useInGeri=*The safety and effectiveness of Tisagenlecleucel have not been established in geriatric patients with r/r B-cell ALL. Clinical studies of Tisagenlecleucel did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. | |||
==== | |useInGender= | ||
|useInRace= | |||
|useInRenalImpair= | |||
|useInHepaticImpair= | |||
|useInReproPotential=Pregnancy Testing | |||
*Pregnancy status of females with reproductive potential should be verified. Sexually-active females of reproductive potential should have a pregnancy test prior to starting treatment with Tisagenlecleucel. | |||
Contraception | |||
*See the prescribing information for fludarabine and cyclophosphamide for information on the need for effective contraception in patients who receive the lymphodepleting chemotherapy. | |||
*There are insufficient exposure data to provide a recommendation concerning duration of contraception following treatment with Tisagenlecleucel. | |||
==== | Infertility | ||
*There are no data on the effect of Tisagenlecleucel on fertility. | |||
|useInImmunocomp= | |||
|administration======Intravenous===== | |||
*Match patient identity with patient identifiers on infusion bag (patient name, date of birth, and DIN or Aph ID) prior to preparation. | |||
*A Tisagenlecleucel dose may be contained in up to 3 cryopreserved patient-specific infusion bags. Verify the number of bags received for the dose of Tisagenlecleucel with the Certificate of Analysis (CoA). | |||
*Coordinate thaw with timing of infusion; confirm infusion time and adjust thaw start time to ensure that product is available for infusion when recipient is ready as thawed product may only be stored for up to 30 minutes at room temperature (20 to 25 degrees C). If more than 1 bag has been received for the treatment dose, thaw 1 bag at a time. Wait to thaw or infuse the next bag until it is determined that the previous bag has been safely administered. | |||
*Do not use if bag is compromised (eg, breaks or cracks in bag). | |||
*Place infusion bag inside a second, sterile bag to protect ports from contamination or in case of a leak. | |||
*Thaw infusion bag in water bath or by dry thaw method at 37 degrees C until no visible ice is present. | |||
*Do not resuspend in new media, wash, or spin down before infusing. | |||
*Inspect thawed infusion bag for visible clumps and gently manually mix to disperse; do not infuse if clumps do not disperse. | |||
*May be stored for up to 30 minutes at room temperature (20 to 25 degrees C) after thawing; infuse within 30 minutes of thawing. | |||
*Prime tubing with NS prior to infusion. | |||
*Do not administer through a leukocyte-depleting filter. | |||
*Infuse entire contents of bag (10 to 50 mL) at 10 to 20 mL/min; adjust rate for smaller children and volumes. | |||
*Cells from all bags must be infused to complete a single dose. | |||
*While maintaining a closed tubing system, rinse infusion bag with 10 to 30 mL NS to ensure infusion of as many cells as possible into patient. | |||
|monitoring=*Resolution or improvement of disease-related signs (reduction of blasts in the bone marrow and peripheral blood, recovery of blood counts, and resolution of extra medullary disease) may indicate efficacy. | |||
*Immunoglobulin levels: After treatment. | |||
*Signs and symptoms of cytokine release syndrome: 2 to 3 times during the first week after the infusion at a certified healthcare facility for at least 4 weeks after infusion. | |||
*Signs and symptoms of neurologic toxicities: 2 to 3 times during the first week at a certified healthcare facility; majority of cases occurred within 8 weeks of infusion. | |||
*Hypersensitivity reaction: During infusion. | |||
*Signs and symptoms of infection. | |||
*Secondary malignancies: Life-long. | |||
|overdose= | |||
|drugBox= | |drugBox= | ||
| Line 309: | Line 336: | ||
| molecular_weight = | | molecular_weight = | ||
}} | }} | ||
|mechAction=* | |mechAction=*Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy which involves reprogramming a patient’s own T cells with a transgene encoding a chimeric antigen receptor (CAR) to identify and eliminate CD19-expressing malignant and normal cells. The CAR is comprised of a murine single-chain antibody fragment which recognizes CD19 and is fused to intracellular signaling domains from 4-1BB (CD137) and CD3 zeta. The CD3 zeta component is critical for initiating T-cell activation and antitumor activity, while 4-1BB enhances the expansion and persistence of Tisagenlecleucel. Upon binding to CD19-expressing cells, the CAR transmits a signal to promote T-cell expansion, activation, target cell elimination, and persistence of the Tisagenlecleucel cells. | ||
|structure= | |structure= | ||
|PD= | |PD= | ||
|PK=*Following infusion, | |PK=*Following infusion, Tisagenlecleucel exhibited an initial rapid expansion followed by a bi-exponential decline in both pediatric and young adult relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) patients, and adult relapsed/refractory diffuse large B-cell lymphoma patients. | ||
*A summary of pharmacokinetic parameters of | *A summary of pharmacokinetic parameters of Tisagenlecleucel is provided in Table 7 below. | ||
[[image:Tisagenlecleucel_Pharmacokinetics_Table_1.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | [[image:Tisagenlecleucel_Pharmacokinetics_Table_1.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
| Line 323: | Line 350: | ||
*The Cmax and AUC0-28d were approximately 2-fold higher in CR/CRi patients compared with non-responding (NR) patients. | *The Cmax and AUC0-28d were approximately 2-fold higher in CR/CRi patients compared with non-responding (NR) patients. | ||
* | *Tisagenlecleucel was present in the blood as well as bone marrow and was measurable beyond 2 years. Blood to bone marrow partitioning suggested that Tisagenlecleucel distribution in bone marrow was 44% of that present in blood at Day 28 while at Months 3 and 6 Tisagenlecleucel distributed at 67% and 69%, respectively, indicating high distribution to bone marrow. | ||
*Children < 10 years and between 10-18 years of age had 1.5- to 2-fold higher Cmax and AUC0-28d than adults. Due to small sample size and high variability, it is difficult to assess the impact of age on the pharmacokinetics of | *Children < 10 years and between 10-18 years of age had 1.5- to 2-fold higher Cmax and AUC0-28d than adults. Due to small sample size and high variability, it is difficult to assess the impact of age on the pharmacokinetics of Tisagenlecleucel. | ||
''Description of Pharmacokinetics in Adult r/r DLBCL'' | ''Description of Pharmacokinetics in Adult r/r DLBCL'' | ||
| Line 331: | Line 358: | ||
*The Cmax and AUC0-28d were similar between responding and non-responding (NR) patients. | *The Cmax and AUC0-28d were similar between responding and non-responding (NR) patients. | ||
* | *Tisagenlecleucel was present in adult r/r DLBCL patients up to 18 months in peripheral blood and up to 9 months in the bone marrow for patients having a complete response. The median time of maximal expansion of transgene levels (Tmax) in peripheral blood occurred at 9-10 days in both responding and non-responding patients. | ||
''Tocilizumab and Corticosteroid use'' | ''Tocilizumab and Corticosteroid use'' | ||
*Some patients required tocilizumab and corticosteroids for the management of CRS. | *Some patients required tocilizumab and corticosteroids for the management of CRS. Tisagenlecleucel continues to expand and persist following tocilizumab administration. Patients who have higher expansion tended to have higher CRS Grades [see Warnings and Precautions (5.1)]. | ||
*Pediatric and young adult r/r B-cell ALL patients (n = 18) treated with tocilizumab had 265% and 183% higher | *Pediatric and young adult r/r B-cell ALL patients (n = 18) treated with tocilizumab had 265% and 183% higher Tisagenlecleucel AUC0-28d and Cmax, respectively, as compared to patients (n = 44) who did not receive tocilizumab. In addition, patients who received corticosteroids had 89% higher AUC0-28d compared with patients who did not receive corticosteroids. | ||
*Adult /r/r DLBCL patients treated with tocilizumab (N = 15) had 199% (n = 11) and 257% (n = 13) higher | *Adult /r/r DLBCL patients treated with tocilizumab (N = 15) had 199% (n = 11) and 257% (n = 13) higher Tisagenlecleucel AUC0-28d and Cmax, respectively, as compared to patients (N = 90) who did not receive tocilizumab. In addition, patients who received corticosteroids (N = 11) had 122% and 161% higher AUC0-28d and Cmax, respectively, as compared with patients who did not receive corticosteroids (N = 94). Hepatic and renal impairment studies of Tisagenlecleucel were not conducted. | ||
|nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | |nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | ||
*Genotoxicity assays and carcinogenicity assessment in rodent models were not performed for | *Genotoxicity assays and carcinogenicity assessment in rodent models were not performed for Tisagenlecleucel. In vitro expansion studies with transduced T cells (Tisagenlecleucel) from healthy donors and patients showed no evidence for transformation and/or immortalization of T cells. In vivo studies in immunocompromised mice did not show signs of abnormal cell growth or signs of clonal cell expansion for up to 7 months after cell injection. A genomic insertion site analysis was performed on Tisagenlecleucel products from 14 individual donors (12 patients and 2 healthy volunteers). There was no evidence for preferential integration near genes of concern, or preferential outgrowth of cells harboring integration sites of concern. | ||
*No studies on the effects of | *No studies on the effects of Tisagenlecleucel on fertility have been conducted. | ||
|clinicalStudies======Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)===== | |clinicalStudies======Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)===== | ||
*The efficacy of | *The efficacy of Tisagenlecleucel in pediatric and young adults with r/r B-cell precursor ALL was evaluated in an open-label, multicenter single-arm trial (ELIANA, NCT02228096). In total, 107 patients were screened, 88 were enrolled, 68 were treated, and 63 were evaluable for efficacy. Nine percent of the enrolled patients did not receive the product due to manufacturing failure. The 63 evaluable patients included 35 males and 28 females of median age 12 years (range: 3-23 years). Seventy-three percent of patients were White, 10% were Asian, and 17% were of other races. Six (10%) had primary refractory disease, 30 (48%) had one prior stem cell transplantation, 5 patients (8%) had two stem cell transplantations. Treatment consisted of lymphodepleting chemotherapy (fludarabine 30 mg/m2 daily for 4 days and cyclophosphamide 500 mg/m2 daily for 2 days) followed by a single dose of Tisagenlecleucel. Of the 22 patients who had a WBC count < 1000/µL, 20 received lymphodepleting chemotherapy prior to Tisagenlecleucel while 2 received Tisagenlecleucel infusion without lymphodepleting chemotherapy. Fifty-three patients received bridging chemotherapy between time of enrollment and lymphodepleting chemotherapy. | ||
*The efficacy of | *The efficacy of Tisagenlecleucel was established on the basis of complete remission (CR) within 3 months after infusion, the duration of CR, and proportion of patients with CR and minimal residual disease (MRD) < 0.01% by flow cytometry (MRD-negative) (Table 8). Among the 63 infused patients, 52 (83%) achieved CR/CRi, all of which were MRD-negative. With a median follow-up of 4.8 months from response, the median duration of CR/CRi was not reached (range: 1.2 to 14.1+ months). Median time to onset of CR/CRi was 29 days with onset of CR/CRi between 26 and 31 days for 50/52 (96%) responders. The stem cell transplantation rate among those who achieved CR/CRi was 12% (6/52). Table 8 shows the efficacy results from this study. | ||
[[image:Tisagenlecleucel_Clinical_Studies_Table_1.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | [[image:Tisagenlecleucel_Clinical_Studies_Table_1.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
| Line 357: | Line 384: | ||
=====Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL)===== | =====Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL)===== | ||
*The efficacy and safety of | *The efficacy and safety of Tisagenlecleucel was evaluated in an open-label, multicenter, single-arm trial (JULIET; NCT02445248). Eligible patients were ≥ 18 years of age with relapsed or refractory DLBCL, who received ≥ 2 lines of chemotherapy, including rituximab and anthracycline, or relapsed following autologous hematopoietic stem cell transplantation (HSCT). The study excluded patients with active central nervous system malignancy, prior allogenic HSCT, an ECOG performance status ≥ 2, a creatinine clearance < 60, alanine aminotransferase > 5 times normal, cardiac ejection fraction < 45%, or absolute lymphocyte concentration less than 300/µL. | ||
*Following 2 to 11 days after completion of lymphodepleting (LD) chemotherapy consisting of either fludarabine (25 mg/m2 i.v. daily for 3 days) and cyclophosphamide (250 mg/m2 i.v. daily for 3 days starting with the first dose of fludarabine) or bendamustine (90 mg/m2 i.v. daily for 2 days), | *Following 2 to 11 days after completion of lymphodepleting (LD) chemotherapy consisting of either fludarabine (25 mg/m2 i.v. daily for 3 days) and cyclophosphamide (250 mg/m2 i.v. daily for 3 days starting with the first dose of fludarabine) or bendamustine (90 mg/m2 i.v. daily for 2 days), Tisagenlecleucel was administered as a single intravenous infusion. Bridging chemotherapy between leukapheresis and LD chemotherapy was permitted to control disease burden. LD chemotherapy could be omitted if the white blood cell count was < 1000 cells/µL. The major efficacy outcome measures were objective response rate per Lugano criteria [2014] as assessed by an independent review committee and duration of response. | ||
*Of the 160 patients enrolled, 106 patients received | *Of the 160 patients enrolled, 106 patients received Tisagenlecleucel, including 92 patients who received product manufactured in the U.S. and were followed for at least 3 months or discontinued earlier. Eleven out of 160 patients enrolled did not receive Tisagenlecleucel due to manufacturing failure. Thirty-eight other patients did not receive Tisagenlecleucel, primarily due to death (n = 16), physician decision (n = 16), and adverse events (n = 3). | ||
*Of the 92 patients receiving | *Of the 92 patients receiving Tisagenlecleucel, 90% received physician’s choice of bridging chemotherapy in the interval between start of screening and Tisagenlecleucel infusion, among whom the median number of bridging chemotherapy regimens was 1 (range: 1 to 5) with 83% of patients receiving ≤ 2 regimens. A retrospectively identified sub-group of 68 patients was evaluable for the major efficacy outcome measures. Patients included in this sub-group had either had no bridging chemotherapy, or had imaging that showed measurable disease after completion of bridging chemotherapy, prior to Tisagenlecleucel infusion. Of the 24 patients not included, 8 had no evidence of disease at baseline prior to Tisagenlecleucel infusion, 15 did not have baseline imaging following bridging chemotherapy, and 1 was excluded because of initial misclassification of a neuroendocrine tumor as DLBCL. | ||
*Among the efficacy evaluable population of 68 patients, the baseline characteristics were: median age 56 years (range: 22 to 74 years); 71% male; 90% White, 4% Asian, and 3% Black or African American; 78% had primary DLBCL not otherwise specified (NOS) and 22% had DLBCL following transformation from follicular lymphoma, of whom 17% were identified as high grade; and 44% had undergone prior autologous HSCT. The median number of prior therapies was 3 (range: 1 to 6), 56% had refractory disease and 44% relapsed after their last therapy. Ninety percent of patients received lymphodepleting chemotherapy (66% of patients received fludarabine and 24% received bendamustine) and 10% did not receive any LD chemotherapy. The median time from leukapheresis and cryopreservation to | *Among the efficacy evaluable population of 68 patients, the baseline characteristics were: median age 56 years (range: 22 to 74 years); 71% male; 90% White, 4% Asian, and 3% Black or African American; 78% had primary DLBCL not otherwise specified (NOS) and 22% had DLBCL following transformation from follicular lymphoma, of whom 17% were identified as high grade; and 44% had undergone prior autologous HSCT. The median number of prior therapies was 3 (range: 1 to 6), 56% had refractory disease and 44% relapsed after their last therapy. Ninety percent of patients received lymphodepleting chemotherapy (66% of patients received fludarabine and 24% received bendamustine) and 10% did not receive any LD chemotherapy. The median time from leukapheresis and cryopreservation to Tisagenlecleucel infusion was 113 days (range: 47 to 196 days). The median dose was 3.5 × 108 CAR-positive viable T cells (range: 1.0 to 5.2 × 108 cells). Seventy-three percent of patients received Tisagenlecleucel in the inpatient setting. | ||
*Efficacy was established on the basis of complete response (CR) rate and duration of response (DOR), as determined by an independent review committee (Table 9 and Table 10). The median time to first response to | *Efficacy was established on the basis of complete response (CR) rate and duration of response (DOR), as determined by an independent review committee (Table 9 and Table 10). The median time to first response to Tisagenlecleucel (CR or PR) was 0.9 months (range: 0.7 to 3.3 months). The median duration of response was not reached. Response durations were longer in patients who achieved CR, as compared to patients with a best response of partial response (PR) (Table 12). Of the 22 patients who experienced a CR, 9 achieved this status by 1 month, 12 more by month 3, and the last by month 6 after Tisagenlecleucel infusion. | ||
[[image:Tisagenlecleucel_Clinical_Studies_Table_2.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | [[image:Tisagenlecleucel_Clinical_Studies_Table_2.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
| Line 373: | Line 400: | ||
[[image:Tisagenlecleucel_Clinical_Studies_Table_3.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | [[image:Tisagenlecleucel_Clinical_Studies_Table_3.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
|howSupplied=* | |howSupplied=*Tisagenlecleucel is supplied as a frozen suspension of genetically modified autologous T cells in an infusion bag(s) labeled for the specific recipient. Tisagenlecleucel is shipped directly to the cell lab associated with the infusion center in a liquid nitrogen Dewar. Product and patient-specific labels are located inside the Dewar. | ||
*Ped ALL: NDC 0078-0846-19 | *Ped ALL: NDC 0078-0846-19 | ||
| Line 385: | Line 412: | ||
*Use closed, break-proof, leak-proof containers when transporting infusion bags within the facility. | *Use closed, break-proof, leak-proof containers when transporting infusion bags within the facility. | ||
*Thaw | *Thaw Tisagenlecleucel prior to infusion. | ||
|packLabel=[[image:Tisagenlecleucel_Package_Label_1.jpeg|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |packLabel=[[image:Tisagenlecleucel_Package_Label_1.jpeg|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
| Line 391: | Line 418: | ||
[[image:Tisagenlecleucel_Package_Label_2.jpeg|none|thumb|400px|This image is provided by the National Library of Medicine.]] | [[image:Tisagenlecleucel_Package_Label_2.jpeg|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
|fdaPatientInfo=*Ensure that patients understand the risk of manufacturing failure. This has been reported in up to 9% of manufacturing attempts. In case of a manufacturing failure, a second manufacturing of | |fdaPatientInfo=*Ensure that patients understand the risk of manufacturing failure. This has been reported in up to 9% of manufacturing attempts. In case of a manufacturing failure, a second manufacturing of Tisagenlecleucel may be attempted. In addition, while the patient awaits the product, additional chemotherapy (not the lymphodepletion) may be necessary and may increase the risk of adverse events during the pre-infusion period. | ||
*Prior to infusion, advise patients of the following risks: | *Prior to infusion, advise patients of the following risks: | ||
| Line 399: | Line 426: | ||
:*Neurological Toxicities -- Report altered or decreased consciousness, delirium, confusion, agitation, seizures, difficulty speaking and understanding, or loss of balance to their healthcare professional. | :*Neurological Toxicities -- Report altered or decreased consciousness, delirium, confusion, agitation, seizures, difficulty speaking and understanding, or loss of balance to their healthcare professional. | ||
:*Serious Infections -- | :*Serious Infections -- Tisagenlecleucel may cause serious infections. Advise patients that they will be screened for HBV, HCV, and HIV before collection of cells. | ||
:*Hypogammaglobulinemia -- Patients may need to receive immunoglobulin replacement for an indefinite amount of time following treatment with | :*Hypogammaglobulinemia -- Patients may need to receive immunoglobulin replacement for an indefinite amount of time following treatment with Tisagenlecleucel. Patients should tell their physician about their treatment with Tisagenlecleucel before receiving a live virus vaccine. | ||
:*Driving and Engaging in Hazardous Occupations -- Patients should refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, for at least 8 weeks after treatment. | :*Driving and Engaging in Hazardous Occupations -- Patients should refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, for at least 8 weeks after treatment. | ||
:*Prolonged Cytopenia -- Patient may exhibit signs or symptoms associated with bone marrow suppression (i.e., neutropenia, thrombocytopenia and anemia) for several weeks following lymphodepleting chemotherapy and | :*Prolonged Cytopenia -- Patient may exhibit signs or symptoms associated with bone marrow suppression (i.e., neutropenia, thrombocytopenia and anemia) for several weeks following lymphodepleting chemotherapy and Tisagenlecleucel. | ||
[[image:Tisagenlecleucel_Patient_Counseling_Information.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | [[image:Tisagenlecleucel_Patient_Counseling_Information.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | ||
Latest revision as of 15:02, 1 August 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
CYTOKINE RELEASE SYNDROME AND NEUROLOGICAL TOXICITIES
See full prescribing information for complete Boxed Warning.
|
Overview
Tisagenlecleucel is a CD19-directed genetically modified autologous T-cell immunotherapy that is FDA approved for the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse and adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include cytokine release syndrome, hypogammaglobulinemia, infections-pathogen unspecified, pyrexia, decreased appetite, headache, encephalopathy, hypotension, bleeding episodes, tachycardia, nausea, diarrhea, vomiting, viral infectious disorders, hypoxia, fatigue, acute kidney injury, edema, cough, delirium.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications:
- Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of:
Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
- Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Adult Relapsed or Refractory (r/r) Diffuse Large B-Cell Lymphoma (DLBCL)
- Adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma.
Dosage in Adult Relapsed or Refractory (r/r) Diffuse Large B-cell lymphoma (DLBCL)
- Tisagenlecleucel is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells.
- For adult patients: administer 0.6 to 6.0 x 108 CAR-positive viable T cells.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Tisagenlecleucel Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding Tisagenlecleucel Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Indications:
- Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of:
Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
- Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Adult Relapsed or Refractory (r/r) Diffuse Large B-Cell Lymphoma (DLBCL)
- Adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma.
Dosage in Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
- Tisagenlecleucel is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells.
- Based on the patient weight reported at the time of leukapheresis:
- Patients 50 kg or less: administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight.
- Patients above 50 kg: administer 0.1 to 2.5 x 108 CAR-positive viable T cells.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Tisagenlecleucel Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding Tisagenlecleucel Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- None
Warnings
|
CYTOKINE RELEASE SYNDROME AND NEUROLOGICAL TOXICITIES
See full prescribing information for complete Boxed Warning.
|
Cytokine Release Syndrome (CRS)
- CRS, including fatal or life-threatening reactions, occurred following treatment with Tisagenlecleucel. CRS occurred in 54 (79%) of the 68 pediatric and young adult patients with r/r ALL and 78 (74%) of the 106 adult patients with r/r DLBCL receiving Tisagenlecleucel, including ≥ Grade 3 (Penn grading system1) in 49% of patients with r/r ALL and in 23% of patients with r/r DLBCL. The median time to onset was 3 days (range: 1-51), and in only two patients was onset after Day 10. The median time to resolution of CRS was 8 days (range: 1-36).
- Of the 54 patients with r/r ALL who had CRS, 27 (50%) received tocilizumab. Seven (13%) patients received two doses of tocilizumab, 3 (6%) patients received three doses of tocilizumab, and 14 (26%) patients received addition of corticosteroids (e.g., methylprednisolone). Of the 78 patients with r/r DLBCL who had CRS, 16 (21%) received systemic tocilizumab or corticosteroids. Six (8%) patients received a single dose of tocilizumab, 10 (13%) patients received two doses of tocilizumab, and 10 (13%) patients received corticosteroids in addition to tocilizumab. Two patients with r/r DLBCL received corticosteroids for CRS without concomitant tocilizumab, and two patients received corticosteroids for persistent neurotoxicity after resolution of CRS.
- Five deaths occurred within 30 days of Tisagenlecleucel infusion. One patient with r/r ALL died with CRS and progressive leukemia, and one patient had resolving CRS with abdominal compartment syndrome, coagulopathy, and renal failure when an intracranial hemorrhage occurred. Of the 3 r/r DLBCL patients who died within 30 days of infusion, all had CRS in the setting of stable to progressive underlying disease, one of whom developed bowel necrosis. Among patients with CRS, key manifestations include fever (92% in r/r ALL and r/r DLBCL), hypotension (67% in r/r ALL; 47% in r/r DLBCL), hypoxia (20% in r/r ALL; 35% in r/r DLBCL) and tachycardia (30% in r/r ALL; 14% in r/r DLBCL). CRS may be associated with hepatic, renal, and cardiac dysfunction, and coagulopathy.
- Delay the infusion of Tisagenlecleucel after lymphodepleting chemotherapy if the patient has unresolved serious adverse reactions from preceding chemotherapies (including pulmonary toxicity, cardiac toxicity, or hypotension), active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden.
- Ensure that two doses of tocilizumab are available on site prior to infusion of Tisagenlecleucel. Monitor patients for signs or symptoms of CRS for at least 4 weeks after treatment with Tisagenlecleucel. Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time. At the first sign of CRS, immediately evaluate patient for hospitalization and institute treatment with supportive care, tocilizumab and/or corticosteroids as indicated.
- Risk factors for severe CRS in the pediatric and young adult r/r B-cell ALL population are high pre-infusion tumor burden (greater than 50% blasts in bone marrow), uncontrolled or accelerating tumor burden following lymphodepleting chemotherapy, active infections, and/or inflammatory processes. Risk factors for developing severe CRS in adult r/r DLBCL are not known.
Neurological Toxicities
- Neurological toxicities including severe or life-threatening reactions, occurred in 49 (72%) of the 68 patients with r/r ALL and 62 (58%) of the 106 patients with r/r DLBCL following treatment with Tisagenlecleucel, including ≥ Grade 3 in 21% of patients with r/r ALL and 18% of patients with r/r DLBCL. Among patients who had a neurological toxicity, 88% occurred within 8 weeks following Tisagenlecleucel infusion.
- Median time to the first event was 6 days from infusion (range: 1-359), and the median duration was 6 days for patients with r/r ALL and 14 days for patients with r/r DLBCL. Resolution occurred within 3 weeks in 79% of patients with r/r ALL and 61% of patients with r/r DLBCL. Encephalopathy lasting up to 50 days was noted.
- The onset of neurological toxicity can be concurrent with CRS, following resolution of CRS or in the absence of CRS.
- The most common neurological toxicities observed with Tisagenlecleucel include headache (37% in r/r ALL; 21% in r/r DLBCL), encephalopathy (34% in r/r ALL; 16% in r/r DLBCL), delirium (21% in r/r ALL; 6% in r/r DLBCL), anxiety (13% in r/r ALL; 9% in r/r DLBCL), sleep disorders (10% in r/r ALL; 9% in r/r DLBCL), dizziness (6% in r/r ALL; 11% in r/r DLBCL), tremor (9% in r/r ALL; 7% r/r DLBCL) and peripheral neuropathy (4% in r/r ALL; 8% in r/r DLBCL). Other manifestations included seizures, mutism and aphasia.
- Monitor patients for neurological events and exclude other causes for neurological symptoms. Provide supportive care as needed for Tisagenlecleucel-associated neurological events.
Tisagenlecleucel REMS to Mitigate Cytokine Release Syndrome and Neurological Toxicities
- Because of the risk of CRS and neurological toxicities, Tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Tisagenlecleucel REMS. The required components of the Tisagenlecleucel REMS are:
- Healthcare facilities that dispense and administer Tisagenlecleucel must be enrolled and comply with the REMS requirements. Certified healthcare facilities must have on-site, immediate access to tocilizumab, and ensure that a minimum of two doses of tocilizumab are available for each patient for administration within 2 hours after Tisagenlecleucel infusion, if needed for treatment of CRS.
- Certified healthcare facilities must ensure that healthcare providers who prescribe, dispense or administer Tisagenlecleucel are trained about the management of CRS and neurological toxicities.
Hypersensitivity Reactions
- Allergic reactions may occur with infusion of Tisagenlecleucel. Serious hypersensitivity reactions, including anaphylaxis, may be due to the dimethyl sulfoxide (DMSO) or dextran 40 in Tisagenlecleucel.
Serious Infections
- Infections, including life-threatening or fatal infections, occurred in 95 (55%) of 174 patients with r/r ALL or r/r DLBCL after Tisagenlecleucel infusion. Fifty eight patients (33%) experienced Grade ≥ 3 infections, including fatal infections in 2 patients (3%) with r/r ALL and 1 patient (1%) with r/r DLBCL. Prior to Tisagenlecleucel infusion, infection prophylaxis should follow local guidelines. Patients with active uncontrolled infection should not start Tisagenlecleucel treatment until the infection is resolved. Monitor patients for signs and symptoms of infection after treatment with Tisagenlecleucel and treat appropriately.
- Febrile neutropenia (≥ Grade 3) was also observed in 37% of patients with r/r ALL and 17% of patients with r/r DLBCL after Tisagenlecleucel infusion and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage with broad spectrum antibiotics, fluids and other supportive care as medically indicated.
Viral Reactivation
- Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure and death, can occur in patients treated with drugs directed against B cells.
- Perform screening for HBV, HCV, and HIV in accordance with clinical guidelines before collection of cells for manufacturing.
Prolonged Cytopenias
- Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and Tisagenlecleucel infusion.
- In the ELIANA study (Study 1), ≥ Grade 3 cytopenias not resolved by Day 28 following Tisagenlecleucel treatment included neutropenia (40%), and thrombocytopenia (27%) among 52 responding patients. At 56 days following Tisagenlecleucel, 17% and 12% of responding patients had ≥ Grade 3 neutropenia or thrombocytopenia respectively.
- In the JULIET study (Study 2), ≥ Grade 3 cytopenias not resolved by Day 28 following Tisagenlecleucel treatment included thrombocytopenia (40%) and neutropenia (25%) among 106 treated patients.
- Prolonged neutropenia has been associated with increased risk of infection. Myeloid growth factors, particularly GM-CSF, are not recommended during the first 3 weeks after Tisagenlecleucel infusion or until CRS has resolved.
Hypogammaglobulinemia
- Hypogammaglobulinemia and agammaglobulinemia (IgG) related to B-cell aplasia can occur in patients with a complete remission (CR) after Tisagenlecleucel infusion.
- Hypogammaglobulinemia was reported in 43% of patients treated with Tisagenlecleucel for r/r ALL and 14% of patients with r/r DLBCL.
- Monitor immunoglobulin levels after treatment with Tisagenlecleucel and manage using infection precautions, antibiotic prophylaxis and immunoglobulin replacement standard guidelines.
Immunization with Live Vaccine
- The safety of immunization with live viral vaccines during or following Tisagenlecleucel treatment has not been studied. Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during Tisagenlecleucel treatment, and until immune recovery following treatment with Tisagenlecleucel.
- Pregnant women who have received Tisagenlecleucel may have hypogammaglobulinemia. Assess immunoglobulin levels in newborns of mothers treated with Tisagenlecleucel.
Secondary Malignancies
- Patients treated with Tisagenlecleucel may develop secondary malignancies or recurrence of their cancer. Monitor life-long for secondary malignancies.
Effects on Ability to Drive and Use Machines
- Due to the potential for neurological events, including altered mental status or seizures, patients receiving Tisagenlecleucel are at risk for altered or decreased consciousness or coordination in the 8 weeks following Tisagenlecleucel infusion. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, during this initial period.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety data described in the WARNINGS AND PRECAUTIONS and in this section reflect exposure to Tisagenlecleucel in two non-randomized, single-arm studies in which 68 pediatric and young adult patients with relapsed/refractory (r/r) B-cell ALL (ELIANA Study) and 106 adults with r/r diffuse large B-cell lymphoma (JULIET Study) received a single dose of CAR-positive viable T cells.
Pediatric and Young Adult r/r B-cell Acute Lymphoblastic Leukemia (ALL) (up to 25 years of age)
- Based on a recommended dose which was weight-based, all 68 patients in the ELIANA study (Study 1) received a single intravenous dose of Tisagenlecleucel [see Clinical Studies (14.1)]. The most common adverse reactions (> 20%) were cytokine release syndrome (79%), hypogammaglobulinemia (43%), infections-pathogen unspecified (41%), pyrexia (40%), decreased appetite (37%), headache (37%), encephalopathy (34%), hypotension (31%), bleeding episodes (31%), tachycardia (26%), nausea (26%), diarrhea (26%), vomiting (26%), viral infectious disorders (26%), hypoxia (24%), fatigue (25%), acute kidney injury (24%), edema (21%), cough (21%), and delirium (21%).
- The adverse reactions with greater or equal to 10% incidence for any Grade are summarized in Table 2.

Laboratory Abnormalities
- Selected laboratory abnormalities worsening from baseline Grade 0-2 to Grade 3-4 are shown in Table 3.

- All patients experienced neutropenia, anemia and thrombocytopenia. See Table 4 for the incidences of ≥ Grade 3 prolonged thrombocytopenia and prolonged neutropenia in responding patients.

Adult r/r Diffuse Large B-cell Lymphoma (DLBCL)
- In the JULIET study (Study 2) 106 adults with r/r DLBCL received a single intravenous dose of Tisagenlecleucel. The most common adverse reactions (incidence > 20%) were cytokine release syndrome, infections-pathogen unspecified, diarrhea, nausea, pyrexia, fatigue, hypotension, edema and headache.
- The study population characteristics were: median age of 56 years (range: 22 to 76 years), 79% DLBCL; a median of 3 prior lines of therapy (range: 1-6), 49% had a prior autologous hematopoietic stem cell transplantation, and 33% had received prior radiation therapy. Ninety-nine patients (93%) received lymphodepleting chemotherapy prior to Tisagenlecleucel, that included fludarabine (n = 77) or bendamustine (n = 22).
- The adverse reactions with greater than or equal to 10% incidence for any Grade are summarized in Table 5 below.

Laboratory Abnormalities
- Selected laboratory abnormalities worsening from baseline Grade 0-2 to Grade 3-4 are shown in Table 6.

Immunogenicity
- In clinical studies, humoral immunogenicity of Tisagenlecleucel was measured by determination of anti-murine CAR19 antibodies (anti-mCAR19) in serum pre- and post-administration. The majority of patients, 86% in ELIANA (Study 1) and 91.4% in JULIET (Study 2) tested positive for pre-dose anti-mCAR19 antibodies prior to Tisagenlecleucel infusion; Treatment induced anti-mCAR19 antibodies were detected in 5% of the patients in JULIET. However, the preexisting and treatment-induced antibodies were not associated with an impact on clinical response and did not have an impact on the initial expansion and persistence of Tisagenlecleucel. Persistence of Tisagenlecleucel was similar between patients with positive post-infusion anti-mCAR19 antibodies compared with patients with negative post-infusion anti-mCAR19 antibodies. There is no evidence that the presence of preexisting and treatment-induced anti-mCAR19 antibodies impact the safety or effectiveness of Tisagenlecleucel.
- T cell immunogenicity responses were not observed in adult r/r DLBCL patients.
Postmarketing Experience
There is limited information regarding Tisagenlecleucel Postmarketing Experience in the drug label.
Drug Interactions
- HIV and the lentivirus used to make Tisagenlecleucel have limited, short spans of identical genetic material (RNA). Therefore, some commercial HIV nucleic acid test (NATs) tests may yield false-positive results in patients who have received Tisagenlecleucel.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- There are no available data with Tisagenlecleucel use in pregnant women. No animal reproductive and developmental toxicity studies have been conducted with Tisagenlecleucel to assess whether it can cause fetal harm when administered to a pregnant woman. It is not known if Tisagenlecleucel has the potential to be transferred to the fetus. Based on the mechanism of action, if the transduced cells cross the placenta, they may cause fetal toxicity, including B-cell lymphocytopenia. Therefore, Tisagenlecleucel is not recommended for women who are pregnant, and pregnancy after Tisagenlecleucel administration should be discussed with the treating physician. Report pregnancies to Novartis Pharmaceuticals Corporation at 1-888-669-6682.
- In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Tisagenlecleucel in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Tisagenlecleucel during labor and delivery.
Nursing Mothers
Risk Summary
- There is no information regarding the presence of Tisagenlecleucel in human milk, the effect on the breastfed infant, and the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Tisagenlecleucel and any potential adverse effects on the breastfed infant from Tisagenlecleucel or from the underlying maternal condition.
Pediatric Use
- The safety and efficacy of Tisagenlecleucel have been established in pediatric patients with r/r B-cell ALL. Use of Tisagenlecleucel is supported by a single-arm trial [see Clinical Studies (14.1)] that included 52 pediatric patients with r/r B-cell precursor ALL in the following age groups: 33 children (age 3 years to less than 12 years) and 19 adolescents (age 12 years to less than 17 years). No differences in efficacy or safety were observed between the different age subgroups or in comparison to the young adults in the trial.
- The safety and efficacy of Tisagenlecleucel in pediatric patients with relapsed or refractory DLBCL has not been established.
Geriatic Use
- The safety and effectiveness of Tisagenlecleucel have not been established in geriatric patients with r/r B-cell ALL. Clinical studies of Tisagenlecleucel did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Gender
There is no FDA guidance on the use of Tisagenlecleucel with respect to specific gender populations.
Race
There is no FDA guidance on the use of Tisagenlecleucel with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Tisagenlecleucel in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Tisagenlecleucel in patients with hepatic impairment.
Females of Reproductive Potential and Males
Pregnancy Testing
- Pregnancy status of females with reproductive potential should be verified. Sexually-active females of reproductive potential should have a pregnancy test prior to starting treatment with Tisagenlecleucel.
Contraception
- See the prescribing information for fludarabine and cyclophosphamide for information on the need for effective contraception in patients who receive the lymphodepleting chemotherapy.
- There are insufficient exposure data to provide a recommendation concerning duration of contraception following treatment with Tisagenlecleucel.
Infertility
- There are no data on the effect of Tisagenlecleucel on fertility.
Immunocompromised Patients
There is no FDA guidance one the use of Tisagenlecleucel in patients who are immunocompromised.
Administration and Monitoring
Administration
Intravenous
- Match patient identity with patient identifiers on infusion bag (patient name, date of birth, and DIN or Aph ID) prior to preparation.
- A Tisagenlecleucel dose may be contained in up to 3 cryopreserved patient-specific infusion bags. Verify the number of bags received for the dose of Tisagenlecleucel with the Certificate of Analysis (CoA).
- Coordinate thaw with timing of infusion; confirm infusion time and adjust thaw start time to ensure that product is available for infusion when recipient is ready as thawed product may only be stored for up to 30 minutes at room temperature (20 to 25 degrees C). If more than 1 bag has been received for the treatment dose, thaw 1 bag at a time. Wait to thaw or infuse the next bag until it is determined that the previous bag has been safely administered.
- Do not use if bag is compromised (eg, breaks or cracks in bag).
- Place infusion bag inside a second, sterile bag to protect ports from contamination or in case of a leak.
- Thaw infusion bag in water bath or by dry thaw method at 37 degrees C until no visible ice is present.
- Do not resuspend in new media, wash, or spin down before infusing.
- Inspect thawed infusion bag for visible clumps and gently manually mix to disperse; do not infuse if clumps do not disperse.
- May be stored for up to 30 minutes at room temperature (20 to 25 degrees C) after thawing; infuse within 30 minutes of thawing.
- Prime tubing with NS prior to infusion.
- Do not administer through a leukocyte-depleting filter.
- Infuse entire contents of bag (10 to 50 mL) at 10 to 20 mL/min; adjust rate for smaller children and volumes.
- Cells from all bags must be infused to complete a single dose.
- While maintaining a closed tubing system, rinse infusion bag with 10 to 30 mL NS to ensure infusion of as many cells as possible into patient.
Monitoring
- Resolution or improvement of disease-related signs (reduction of blasts in the bone marrow and peripheral blood, recovery of blood counts, and resolution of extra medullary disease) may indicate efficacy.
- Immunoglobulin levels: After treatment.
- Signs and symptoms of cytokine release syndrome: 2 to 3 times during the first week after the infusion at a certified healthcare facility for at least 4 weeks after infusion.
- Signs and symptoms of neurologic toxicities: 2 to 3 times during the first week at a certified healthcare facility; majority of cases occurred within 8 weeks of infusion.
- Hypersensitivity reaction: During infusion.
- Signs and symptoms of infection.
- Secondary malignancies: Life-long.
IV Compatibility
There is limited information regarding the compatibility of Tisagenlecleucel and IV administrations.
Overdosage
There is limited information regarding Tisagenlecleucel overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Tisagenlecleucel
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | None |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Synonyms | CTL019 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | 16.8 days |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Intravenous infusion |
Mechanism of Action
- Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy which involves reprogramming a patient’s own T cells with a transgene encoding a chimeric antigen receptor (CAR) to identify and eliminate CD19-expressing malignant and normal cells. The CAR is comprised of a murine single-chain antibody fragment which recognizes CD19 and is fused to intracellular signaling domains from 4-1BB (CD137) and CD3 zeta. The CD3 zeta component is critical for initiating T-cell activation and antitumor activity, while 4-1BB enhances the expansion and persistence of Tisagenlecleucel. Upon binding to CD19-expressing cells, the CAR transmits a signal to promote T-cell expansion, activation, target cell elimination, and persistence of the Tisagenlecleucel cells.
Structure
There is limited information regarding Tisagenlecleucel Structure in the drug label.
Pharmacodynamics
There is limited information regarding Tisagenlecleucel Pharmacodynamics in the drug label.
Pharmacokinetics
- Following infusion, Tisagenlecleucel exhibited an initial rapid expansion followed by a bi-exponential decline in both pediatric and young adult relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) patients, and adult relapsed/refractory diffuse large B-cell lymphoma patients.
- A summary of pharmacokinetic parameters of Tisagenlecleucel is provided in Table 7 below.

Description of Pharmacokinetics in Pediatric and Young Adult r/r B-cell ALL (up to 25 years of age)
- The Cmax and AUC0-28d were approximately 2-fold higher in CR/CRi patients compared with non-responding (NR) patients.
- Tisagenlecleucel was present in the blood as well as bone marrow and was measurable beyond 2 years. Blood to bone marrow partitioning suggested that Tisagenlecleucel distribution in bone marrow was 44% of that present in blood at Day 28 while at Months 3 and 6 Tisagenlecleucel distributed at 67% and 69%, respectively, indicating high distribution to bone marrow.
- Children < 10 years and between 10-18 years of age had 1.5- to 2-fold higher Cmax and AUC0-28d than adults. Due to small sample size and high variability, it is difficult to assess the impact of age on the pharmacokinetics of Tisagenlecleucel.
Description of Pharmacokinetics in Adult r/r DLBCL
- The Cmax and AUC0-28d were similar between responding and non-responding (NR) patients.
- Tisagenlecleucel was present in adult r/r DLBCL patients up to 18 months in peripheral blood and up to 9 months in the bone marrow for patients having a complete response. The median time of maximal expansion of transgene levels (Tmax) in peripheral blood occurred at 9-10 days in both responding and non-responding patients.
Tocilizumab and Corticosteroid use
- Some patients required tocilizumab and corticosteroids for the management of CRS. Tisagenlecleucel continues to expand and persist following tocilizumab administration. Patients who have higher expansion tended to have higher CRS Grades [see Warnings and Precautions (5.1)].
- Pediatric and young adult r/r B-cell ALL patients (n = 18) treated with tocilizumab had 265% and 183% higher Tisagenlecleucel AUC0-28d and Cmax, respectively, as compared to patients (n = 44) who did not receive tocilizumab. In addition, patients who received corticosteroids had 89% higher AUC0-28d compared with patients who did not receive corticosteroids.
- Adult /r/r DLBCL patients treated with tocilizumab (N = 15) had 199% (n = 11) and 257% (n = 13) higher Tisagenlecleucel AUC0-28d and Cmax, respectively, as compared to patients (N = 90) who did not receive tocilizumab. In addition, patients who received corticosteroids (N = 11) had 122% and 161% higher AUC0-28d and Cmax, respectively, as compared with patients who did not receive corticosteroids (N = 94). Hepatic and renal impairment studies of Tisagenlecleucel were not conducted.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Genotoxicity assays and carcinogenicity assessment in rodent models were not performed for Tisagenlecleucel. In vitro expansion studies with transduced T cells (Tisagenlecleucel) from healthy donors and patients showed no evidence for transformation and/or immortalization of T cells. In vivo studies in immunocompromised mice did not show signs of abnormal cell growth or signs of clonal cell expansion for up to 7 months after cell injection. A genomic insertion site analysis was performed on Tisagenlecleucel products from 14 individual donors (12 patients and 2 healthy volunteers). There was no evidence for preferential integration near genes of concern, or preferential outgrowth of cells harboring integration sites of concern.
- No studies on the effects of Tisagenlecleucel on fertility have been conducted.
Clinical Studies
Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
- The efficacy of Tisagenlecleucel in pediatric and young adults with r/r B-cell precursor ALL was evaluated in an open-label, multicenter single-arm trial (ELIANA, NCT02228096). In total, 107 patients were screened, 88 were enrolled, 68 were treated, and 63 were evaluable for efficacy. Nine percent of the enrolled patients did not receive the product due to manufacturing failure. The 63 evaluable patients included 35 males and 28 females of median age 12 years (range: 3-23 years). Seventy-three percent of patients were White, 10% were Asian, and 17% were of other races. Six (10%) had primary refractory disease, 30 (48%) had one prior stem cell transplantation, 5 patients (8%) had two stem cell transplantations. Treatment consisted of lymphodepleting chemotherapy (fludarabine 30 mg/m2 daily for 4 days and cyclophosphamide 500 mg/m2 daily for 2 days) followed by a single dose of Tisagenlecleucel. Of the 22 patients who had a WBC count < 1000/µL, 20 received lymphodepleting chemotherapy prior to Tisagenlecleucel while 2 received Tisagenlecleucel infusion without lymphodepleting chemotherapy. Fifty-three patients received bridging chemotherapy between time of enrollment and lymphodepleting chemotherapy.
- The efficacy of Tisagenlecleucel was established on the basis of complete remission (CR) within 3 months after infusion, the duration of CR, and proportion of patients with CR and minimal residual disease (MRD) < 0.01% by flow cytometry (MRD-negative) (Table 8). Among the 63 infused patients, 52 (83%) achieved CR/CRi, all of which were MRD-negative. With a median follow-up of 4.8 months from response, the median duration of CR/CRi was not reached (range: 1.2 to 14.1+ months). Median time to onset of CR/CRi was 29 days with onset of CR/CRi between 26 and 31 days for 50/52 (96%) responders. The stem cell transplantation rate among those who achieved CR/CRi was 12% (6/52). Table 8 shows the efficacy results from this study.

Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL)
- The efficacy and safety of Tisagenlecleucel was evaluated in an open-label, multicenter, single-arm trial (JULIET; NCT02445248). Eligible patients were ≥ 18 years of age with relapsed or refractory DLBCL, who received ≥ 2 lines of chemotherapy, including rituximab and anthracycline, or relapsed following autologous hematopoietic stem cell transplantation (HSCT). The study excluded patients with active central nervous system malignancy, prior allogenic HSCT, an ECOG performance status ≥ 2, a creatinine clearance < 60, alanine aminotransferase > 5 times normal, cardiac ejection fraction < 45%, or absolute lymphocyte concentration less than 300/µL.
- Following 2 to 11 days after completion of lymphodepleting (LD) chemotherapy consisting of either fludarabine (25 mg/m2 i.v. daily for 3 days) and cyclophosphamide (250 mg/m2 i.v. daily for 3 days starting with the first dose of fludarabine) or bendamustine (90 mg/m2 i.v. daily for 2 days), Tisagenlecleucel was administered as a single intravenous infusion. Bridging chemotherapy between leukapheresis and LD chemotherapy was permitted to control disease burden. LD chemotherapy could be omitted if the white blood cell count was < 1000 cells/µL. The major efficacy outcome measures were objective response rate per Lugano criteria [2014] as assessed by an independent review committee and duration of response.
- Of the 160 patients enrolled, 106 patients received Tisagenlecleucel, including 92 patients who received product manufactured in the U.S. and were followed for at least 3 months or discontinued earlier. Eleven out of 160 patients enrolled did not receive Tisagenlecleucel due to manufacturing failure. Thirty-eight other patients did not receive Tisagenlecleucel, primarily due to death (n = 16), physician decision (n = 16), and adverse events (n = 3).
- Of the 92 patients receiving Tisagenlecleucel, 90% received physician’s choice of bridging chemotherapy in the interval between start of screening and Tisagenlecleucel infusion, among whom the median number of bridging chemotherapy regimens was 1 (range: 1 to 5) with 83% of patients receiving ≤ 2 regimens. A retrospectively identified sub-group of 68 patients was evaluable for the major efficacy outcome measures. Patients included in this sub-group had either had no bridging chemotherapy, or had imaging that showed measurable disease after completion of bridging chemotherapy, prior to Tisagenlecleucel infusion. Of the 24 patients not included, 8 had no evidence of disease at baseline prior to Tisagenlecleucel infusion, 15 did not have baseline imaging following bridging chemotherapy, and 1 was excluded because of initial misclassification of a neuroendocrine tumor as DLBCL.
- Among the efficacy evaluable population of 68 patients, the baseline characteristics were: median age 56 years (range: 22 to 74 years); 71% male; 90% White, 4% Asian, and 3% Black or African American; 78% had primary DLBCL not otherwise specified (NOS) and 22% had DLBCL following transformation from follicular lymphoma, of whom 17% were identified as high grade; and 44% had undergone prior autologous HSCT. The median number of prior therapies was 3 (range: 1 to 6), 56% had refractory disease and 44% relapsed after their last therapy. Ninety percent of patients received lymphodepleting chemotherapy (66% of patients received fludarabine and 24% received bendamustine) and 10% did not receive any LD chemotherapy. The median time from leukapheresis and cryopreservation to Tisagenlecleucel infusion was 113 days (range: 47 to 196 days). The median dose was 3.5 × 108 CAR-positive viable T cells (range: 1.0 to 5.2 × 108 cells). Seventy-three percent of patients received Tisagenlecleucel in the inpatient setting.
- Efficacy was established on the basis of complete response (CR) rate and duration of response (DOR), as determined by an independent review committee (Table 9 and Table 10). The median time to first response to Tisagenlecleucel (CR or PR) was 0.9 months (range: 0.7 to 3.3 months). The median duration of response was not reached. Response durations were longer in patients who achieved CR, as compared to patients with a best response of partial response (PR) (Table 12). Of the 22 patients who experienced a CR, 9 achieved this status by 1 month, 12 more by month 3, and the last by month 6 after Tisagenlecleucel infusion.
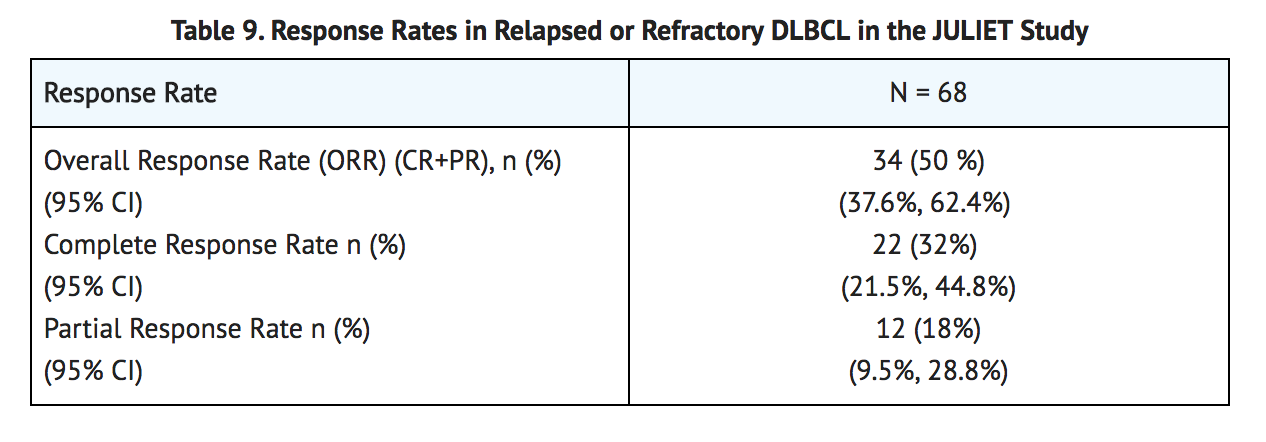
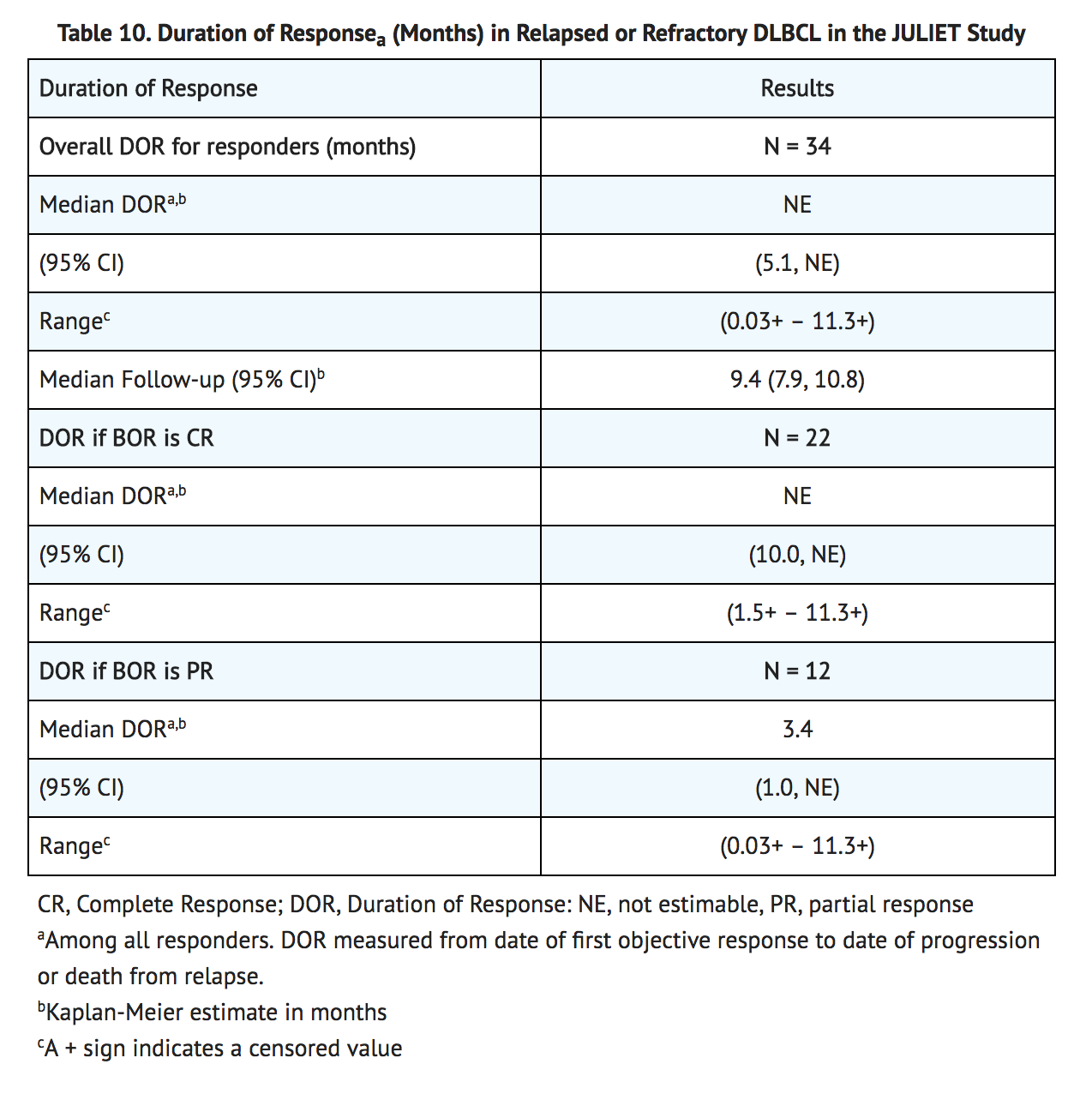
How Supplied
- Tisagenlecleucel is supplied as a frozen suspension of genetically modified autologous T cells in an infusion bag(s) labeled for the specific recipient. Tisagenlecleucel is shipped directly to the cell lab associated with the infusion center in a liquid nitrogen Dewar. Product and patient-specific labels are located inside the Dewar.
- Ped ALL: NDC 0078-0846-19
- DLBCL: NDC 0078-0958-19
Storage
- Confirm patient identity upon receipt.
- Store infusion bag(s) in the vapor phase of liquid nitrogen (less than or equal to minus 120°C) in a temperature-monitored system.
- Use closed, break-proof, leak-proof containers when transporting infusion bags within the facility.
- Thaw Tisagenlecleucel prior to infusion.
Images
Drug Images
{{#ask: Page Name::Tisagenlecleucel |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


{{#ask: Label Page::Tisagenlecleucel |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Ensure that patients understand the risk of manufacturing failure. This has been reported in up to 9% of manufacturing attempts. In case of a manufacturing failure, a second manufacturing of Tisagenlecleucel may be attempted. In addition, while the patient awaits the product, additional chemotherapy (not the lymphodepletion) may be necessary and may increase the risk of adverse events during the pre-infusion period.
- Prior to infusion, advise patients of the following risks:
- Cytokine Release Syndrome (CRS) -- Report signs and symptoms of CRS (high fever, difficulty breathing, chills/shaking chills, severe nausea, severe vomiting, severe diarrhea, severe muscle pain, severe joint pain, very low blood pressure, or dizziness/lightheadedness) to their healthcare professional.
- Neurological Toxicities -- Report altered or decreased consciousness, delirium, confusion, agitation, seizures, difficulty speaking and understanding, or loss of balance to their healthcare professional.
- Serious Infections -- Tisagenlecleucel may cause serious infections. Advise patients that they will be screened for HBV, HCV, and HIV before collection of cells.
- Hypogammaglobulinemia -- Patients may need to receive immunoglobulin replacement for an indefinite amount of time following treatment with Tisagenlecleucel. Patients should tell their physician about their treatment with Tisagenlecleucel before receiving a live virus vaccine.
- Driving and Engaging in Hazardous Occupations -- Patients should refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, for at least 8 weeks after treatment.
- Prolonged Cytopenia -- Patient may exhibit signs or symptoms associated with bone marrow suppression (i.e., neutropenia, thrombocytopenia and anemia) for several weeks following lymphodepleting chemotherapy and Tisagenlecleucel.
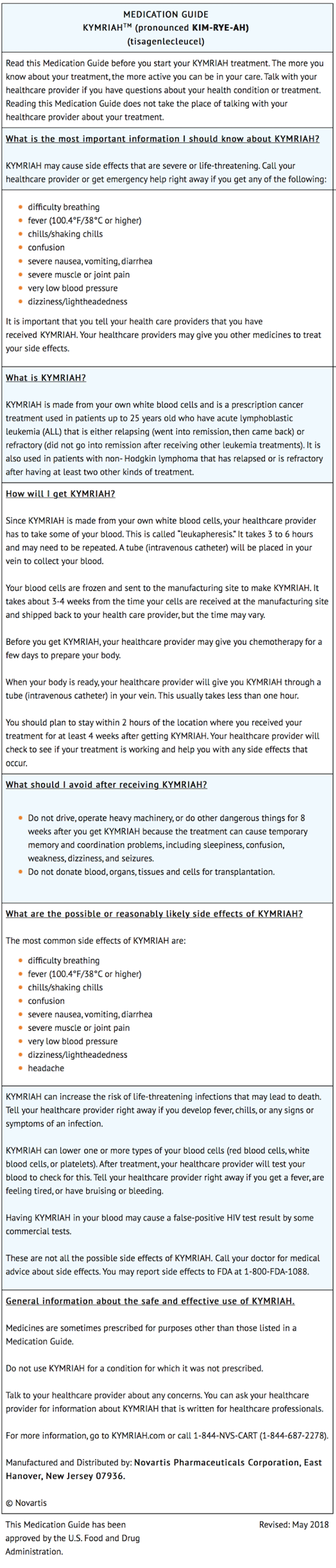
Precautions with Alcohol
Alcohol-Tisagenlecleucel interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Kymriah
Look-Alike Drug Names
There is limited information regarding Tisagenlecleucel Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.