Subependymal giant cell astrocytoma MRI: Difference between revisions
(→MRI) |
No edit summary |
||
| (30 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Subependymal giant cell astrocytoma}} | {{Subependymal giant cell astrocytoma}} | ||
{{CMG}}{{AE}}{{SR}} | {{CMG}}, {{AE}}{{IO}}, {{SR}} | ||
==Overview== | ==Overview== | ||
On brain [[Magnetic resonance imaging|MRI]], some of the findings that are suggestive of subependymal giant cell astrocytoma include T1 isointense and hypointense signal enhancement, T2 isointense and hyperintense signal enhancement, and enlargement of ventricles. | |||
==MRI== | ==MRI== | ||
Brain [[Magnetic resonance imaging|MRI]] may be helpful in the diagnosis of subependymal giant cell astrocytoma. Findings on [[Magnetic resonance imaging|MRI]] suggestive of/diagnostic of subependymal giant cell astrocytoma include:<ref name="pmid26942030">{{cite journal| author=Stein JR, Reidman DA| title=Imaging Manifestations of a Subependymal Giant Cell Astrocytoma in Tuberous Sclerosis. | journal=Case Rep Radiol | year= 2016 | volume= 2016 | issue= | pages= 3750450 | pmid=26942030 | doi=10.1155/2016/3750450 | pmc=4752974 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26942030 }} </ref><ref name="BeaumontGodzik2015">{{cite journal|last1=Beaumont|first1=Thomas L.|last2=Godzik|first2=Jakub|last3=Dahiya|first3=Sonika|last4=Smyth|first4=Matthew D.|title=Subependymal giant cell astrocytoma in the absence of tuberous sclerosis complex: case report|journal=Journal of Neurosurgery: Pediatrics|volume=16|issue=2|year=2015|pages=134–137|issn=1933-0707|doi=10.3171/2015.1.PEDS13146}}</ref> | |||
*Well circumscribed [[mass]] | |||
*Perilesional [[edema]] | |||
*T1 isointense and hypointense signal enhancement | |||
*T2 isointense and hyperintense signal enhancement | |||
*[[Calcification]] | |||
*[[Cyst]] | |||
*Enlargement of ventricles | |||
*Homogenous postcontrast enhancement | |||
Serial [[Magnetic resonance imaging|MRI's]] every 1-3 years is recommended in [[asymptomatic]] patients younger than 25 as [[tumor]] growth is more common in these patients.<ref name="pmid26942030">{{cite journal| author=Stein JR, Reidman DA| title=Imaging Manifestations of a Subependymal Giant Cell Astrocytoma in Tuberous Sclerosis. | journal=Case Rep Radiol | year= 2016 | volume= 2016 | issue= | pages= 3750450 | pmid=26942030 | doi=10.1155/2016/3750450 | pmc=4752974 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26942030 }} </ref> | |||
| | |||
| | |||
| | |||
| | |||
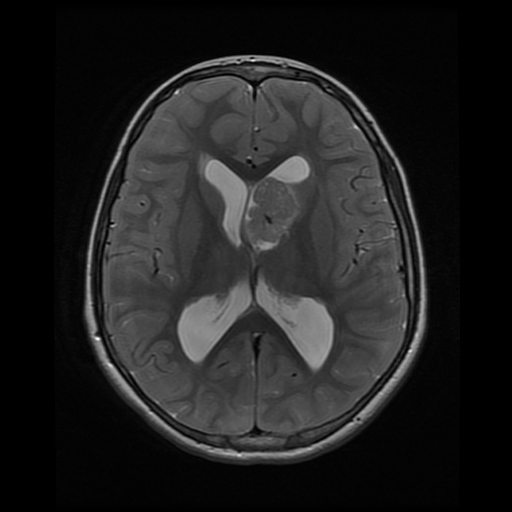
[[File:SEGA MRI.jpg|400px|thumb|left|Axial T2 MRI showing a large lobulated intensely enhancing mass arising from the left foramen of Monro causing mild hydrocephalus. [https://radiopaedia.org/articles/subependymal-giant-cell-astrocytoma?lang=us source:Case courtesy of Dr Amro Omar, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/36589">rID: 36589</a>]]] | |||
<br style="clear:left" /> | |||
</ | |||
==References== | |||
{{reflist|2}} | {{reflist|2}} | ||
| Line 52: | Line 32: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Neurology]] | |||
[[Category:Neurosurgery]] | |||
Latest revision as of 21:04, 5 November 2019
|
Subependymal giant cell astrocytoma Microchapters |
|
Differentiating Subependymal Giant Cell Astrocytoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Subependymal giant cell astrocytoma MRI On the Web |
|
American Roentgen Ray Society Images of Subependymal giant cell astrocytoma MRI |
|
Risk calculators and risk factors for Subependymal giant cell astrocytoma MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: Ifeoma Odukwe, M.D. [2], Sujit Routray, M.D. [3]
Overview
On brain MRI, some of the findings that are suggestive of subependymal giant cell astrocytoma include T1 isointense and hypointense signal enhancement, T2 isointense and hyperintense signal enhancement, and enlargement of ventricles.
MRI
Brain MRI may be helpful in the diagnosis of subependymal giant cell astrocytoma. Findings on MRI suggestive of/diagnostic of subependymal giant cell astrocytoma include:[1][2]
- Well circumscribed mass
- Perilesional edema
- T1 isointense and hypointense signal enhancement
- T2 isointense and hyperintense signal enhancement
- Calcification
- Cyst
- Enlargement of ventricles
- Homogenous postcontrast enhancement
Serial MRI's every 1-3 years is recommended in asymptomatic patients younger than 25 as tumor growth is more common in these patients.[1]
References
- ↑ 1.0 1.1 Stein JR, Reidman DA (2016). "Imaging Manifestations of a Subependymal Giant Cell Astrocytoma in Tuberous Sclerosis". Case Rep Radiol. 2016: 3750450. doi:10.1155/2016/3750450. PMC 4752974. PMID 26942030.
- ↑ Beaumont, Thomas L.; Godzik, Jakub; Dahiya, Sonika; Smyth, Matthew D. (2015). "Subependymal giant cell astrocytoma in the absence of tuberous sclerosis complex: case report". Journal of Neurosurgery: Pediatrics. 16 (2): 134–137. doi:10.3171/2015.1.PEDS13146. ISSN 1933-0707.