Pressure volume diagram: Difference between revisions
Jump to navigation
Jump to search
Rim Halaby (talk | contribs) |
|||
| (63 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} | {{CMG}}; '''Assistant Editor(s)-in-Chief:''' [[User:Rim Halaby|Rim Halaby]] | ||
{{SK}} Pressure-volume loop; P-V diagram; volume-pressure loop | {{SK}} Pressure-volume loop; P-V diagram; volume-pressure loop | ||
==Overview== | ==Overview== | ||
A plot of a system's pressure versus volume has long been used to measure the work done by the system and its efficiency. This analysis can be applied to heat engines and pumps, including the heart. | *A plot of a system's pressure versus volume has long been used to measure the work done by the system and its efficiency. This analysis can be applied to heat engines and pumps, including the heart. | ||
*Real time left ventricular (LV) pressure-volume loops provide a framework for understanding cardiac mechanics; in fact, a considerable amount of information on cardiac performance can be determined from the pressure versus volume plot (also known as [[pressure volume diagram]]). | |||
*Several physiologically relevant hemodynamic parameters such as [[stroke volume]], [[cardiac output]], [[ejection fraction]], myocardial contractility can be determined from these loops. | |||
*To generate a [[pressure volume loop]] for the left [[ventricle]], the left ventricular pressure is plotted against left ventricular volume at multiple time points during a single [[cardiac cycle]]. | |||
== Cardiac Pressure-Volume Loop== | |||
*The left ventricular pressure-volume loop (PV loop) represents the different events of the [[cardiac cycle]]. | |||
*To generate a PV loop for the left [[ventricle]], the left ventricular pressure is plotted against the left ventricular volume at multiple time points during a single cardiac cycle. | |||
*The left ventricular pressure-volume illustrates the four phases of the [[cardiac cycle]] with respect to pressure and volume changes: | |||
**'''Phase I: Diastolic ventricular filling''' | |||
***The [[mitral valve]] is open while the [[aortic valve]] is closed. | |||
***The volume increases to reach the maximal ventricular capacity known as end diastolic volume '''EDV'''. | |||
***The pressure slightly increases. | |||
**'''Phase II: Isovolumetric contraction''' | |||
***The mitral and aortic valves are both closed. | |||
***The volume of the blood is unchanged as the [[ventricles]] are contracting. | |||
***The pressure inside the ventricles significantly increases. | |||
**'''Phase III: Ventricular ejection''' | |||
***The [[aortic valve]] opens as the pressure inside the ventricles exceeds that of the [[aorta]]. | |||
***The blood volume inside the left [[ventricle]] decreases because it is pumped into the systemic circulation. | |||
**'''Phase IV: Isovolumetric relaxation''' | |||
***The aortic and mitral valves are closed. | |||
***The volume inside the left [[ventricle]] is unchanged and it corresponds to the volume remaining in the ventricle after systole, known as end systolic volume '''ESV'''. | |||
***The pressure inside the ventricle tremendously decreases as the ventricles are relaxing. | |||
[[Image: | ; Below is an image showing idealized pressure-volume diagram featuring cardiac cycle events. | ||
[[Image:Normal_Pressure_Volume_Loop.png|600px|Normal pressure volume loop]] | |||
== | == Pressure-Volume Parameters == | ||
=== Stroke Volume === | |||
*[[Stroke volume]] (SV) is the amount of blood pumped by the left [[ventricle]] in a single cardiac cycle. | |||
**At the start of systole, the left [[ventricle]] is filled with blood to the capacity known as end diastolic volume EDV. | |||
**During systole, the left [[ventricle]] contracts and ejects blood until it reaches its minimum capacity known as end systolic volume ESV. | |||
**'''Stroke Volume (SV) = EDV – ESV''' | |||
* The stroke volume is an indicator the left ventricular function which is mainly affected by the preload, afterload and contractility of the heart. | |||
=== Stroke Work === | |||
*Ventricular stroke work (SW) is defined as the work performed by the left or right ventricle to eject the stroke volume into the aorta or pulmonary artery, respectively. | |||
*The area enclosed by the PV loop is a measure of the ventricular stroke work, which is a product of the stroke volume and the mean aortic or pulmonary artery pressure (afterload), depending on whether one is considering the left or the right ventricle. | |||
=== Cardiac Output === | |||
[[ | *[[Cardiac output]] (CO) is defined as the amount of blood pumped by the left [[ventricle]] in unit time. | ||
** '''CO = Stroke Volume x Heart Rate''' | |||
**The normal cardiac output is '''5-6L/min''' and it can increase up to 5 times during exercise. | |||
**CO is an indicator of the left ventricular function. | |||
== | === Ejection Fraction === | ||
*[[Ejection fraction]] (EF) is defined as the fraction of end diastolic volume that is ejected out of the ventricle during each contraction. | |||
[[ | *'''Ejection Fraction = Stroke volume/end diastolic volume''' | ||
* Healthy ventricles typically have ejection fractions greater than 0.55. | |||
* [[Myocardial infarction]] or cardiomyopathy causes damage to the myocardium, which impairs the heart's ability to eject blood and therefore reduces ejection fraction. This reduction in the ejection fraction can manifest itself as heart failure. | |||
**Low EF usually indicates [[systolic dysfunction]] and severe heart failure can result in EF lower than 0.2. | |||
=== dP/dt<sub>min</sub> and dP/dt<sub>max</sub> === | |||
*These represent the minimum and maximum rate of pressure change in the ventricle. Peak dP/dt has historically been used as an index of ventricular performance. However, it is known to be load dependent and inferior to hemodynamic parameters defined by the PV plane. | |||
*An increase in contractility is manifested as an increase in dP/dtmax during isovolumic contraction. However, dP/dtmax is also influenced by preload, afterload, heart rate and myocardial hypertrophy. Hence the relationship between ventricular end-diastolic volume and dP/dt is a more accurate index of contractility than dP/dt alone. | |||
*Similarly, an increase in diastolic function or an increase in relaxation ([[lusitropy]]) causes increased dP/dtmin during isovolumic relaxation. Hence, dP/dtmin has been used as a valuable tool in the analysis of isovolumic relaxation. However, studies have shown that this parameter may not be a valid measure of LV relaxation rate, especially during acute alterations in contractility or afterload. | |||
[[ | |||
=== Isovolumic Relaxation Constant (Τau) === | |||
*Tau represents the exponential decay of the ventricular pressure during isovolumic relaxation. Several studies have shown that Tau is a preload independent measure of isovolumic relaxation. | |||
*Calculation of Tau (Glantz method) | |||
Tau represents the exponential decay of the ventricular pressure during isovolumic relaxation. Several studies have shown that Tau is a preload independent measure of isovolumic relaxation. | |||
Calculation of Tau (Glantz method) | |||
P(t)= P<sub>0</sub>e<sup>-t⁄τ<sub>E</sub></sup> +P<sub>α</sub> | P(t)= P<sub>0</sub>e<sup>-t⁄τ<sub>E</sub></sup> +P<sub>α</sub> | ||
| Line 98: | Line 79: | ||
:* P<sub>α</sub> = non zero asymptote due to pleural and pericardial pressure | :* P<sub>α</sub> = non zero asymptote due to pleural and pericardial pressure | ||
; Below is an image | ; Below is an image showing the calculation of Tau using Glantz Method. | ||
[[File:Calculation of Tau.jpg|center]] | [[File:Calculation of Tau.jpg|center]] | ||
== | ==Determinants of Left Ventricular Function== | ||
*'''1- Preload:''' | |||
**The preload is the '''volume''' that fills in the [[heart]] during diastole, and it is referred to as the end diastolic volume (EDV). | |||
**According to '''Frank Starling's law''', the larger the blood volume filling the heart is, the larger the degree of cardiac stretching is and consequently more [[blood]] is pumped. | |||
**The Frank–Starling mechanism can be explained on the basis of preload. As the heart fills with more blood than usual, there is an increase in the load experienced by each myocyte. This stretches the muscle fibers, increasing the affinity of troponin C to Ca2+ ions causing a greater number of cross-bridges to form within the muscle fibers. This increases the contractile force of the cardiac muscle, resulting in increased stroke volume. | |||
;Below is an image showing Frank Starling's law according to which the left ventricular function increases as the preload increases. | |||
[[Image:Frank_Starling_Law_of_the_Heart.png|350px|Frank starling law of the heart: as the preload increases, the cardiac output increases]] | |||
*'''2- Afterload:''' | |||
**The afterload is the '''pressure''' corresponding to the mean arterial pressure that the heart needs to overcome when pumping blood. | |||
**When the afterload increases, it makes it harder for the heart to pump the [[blood]], and thus the volume remaining in the ventricles after ventricular contraction (end systolic volume) will increase and the stroke volume will be low. | |||
*'''3- Contractility:''' | |||
**The contractility of the heart is defined as the intrinsic force with which the heart contracts. | |||
**Factors that increase the contractility of the heart (positive '''ionotropy''') are: [[catecholamines]], xanthines (caffeine), medications ([[Digitalis]]). | |||
**Factors that decrease the contractlity of the heart (negative '''ionotropy''') are: hypercapnea, hypoxia, acidosis, medications ([[quinidine]], [[procainamide]], barbiturates), heart failure.<ref ="Ganong">Barrett KE, Barman SM, Boitano S, Brooks HL. Chapter 30. The Heart as a Pump. In: Barrett KE, Barman SM, Boitano S, Brooks HL, eds. Ganong's Review of Medical Physiology. 24th ed. New York: McGraw-Hill; 2012.</ref> | |||
;Below is an image showing various curves illustrating different states of contractlity of the heart. | |||
[[Image:Variation_in_the_Contractility_of_the_Heart.png|400px|Variation in the contractility of the heart: note that each curve represents a state of contractility of the heart but any point on each curve represents the same state of contractility.]] | |||
=== | == Pressure-Volume Loop Analysis == | ||
=== End Systolic Pressure Volume Relationship ESPVR=== | |||
End systolic pressure volume relationship (ESPVR) describes the maximal pressure that can be developed by the ventricle at any given LV volume. This implies that the PV loop cannot cross over the line defining ESPVR for any given contractile state. | *End systolic pressure volume relationship ('''ESPVR''') describes the maximal pressure that can be developed by the ventricle at any given LV volume. This implies that the PV loop cannot cross over the line defining ESPVR for any given contractile state. | ||
*The slope of ESPVR represents the '''end-systolic elastance''', which provides an index of '''myocardial contractility'''. | |||
*The ESPVR is relatively insensitive to changes in preload, afterload and heart rate. This makes it an improved index of '''systolic function''' over other hemodynamic parameters like ejection fraction, cardiac output and stroke volume. | |||
**The ESPVR becomes steeper and shifts to the left as inotropy (contractility) increases. | |||
**The ESPVR becomes flatter and shifts to the right as inotropy decreases. | |||
;Below is an image showing a pressure-volume loop with a steeper ESPVR that shifts to the left in the case of increased inotropy or contractility. | |||
[[Image:Increased_Contractility.png|250px|Pressure- Volume loop showing a steeper ESPVR that shifts to the left as inotropy (contractility) increases. Note that the normal pressure volume diagram is in dotted line.]] | |||
The | === End Diastolic Pressure Volume Relationship EDPVR=== | ||
*End diastolic pressure volume relationship (EDPVR) describes the passive filling curve for the ventricle and thus the passive properties of the myocardium. | |||
*The slope of the EDPVR at any point along this curve is the reciprocal of ventricular compliance (or ventricular stiffness). | |||
**If ventricular compliance is decreased (such as in ventricular hypertrophy): | |||
***The ventricle is stiffer. | |||
***This results in higher ventricular end-diastolic pressures (EDP) at any given end-diastolic volume (EDV). | |||
***Alternatively, for a given EDP, a less compliant ventricle would have a smaller EDV due to impaired filling. | |||
**If ventricular compliance increases (such as in dilated cardiomyopathy): | |||
***The EDV may be very high but the EDP may not be greatly elevated. | |||
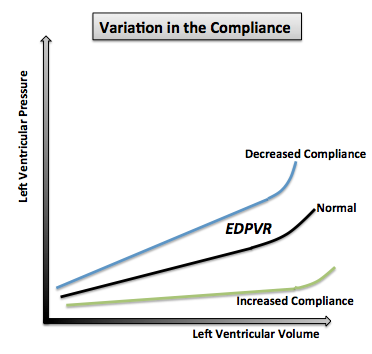
;Below is an image showing a pressure volume loop with changes in the EDPVR's part resulting from variations in the ventricular compliance. | |||
[[Image:Variation_in_the_compliance.png|300px|Changes in the EDPVR's part of pressure-volume loop with variations in the ventricular compliance.]] | |||
[[ | |||
=== Pressure Volume Area === | |||
*The Pressure-volume area (PVA) represents the total mechanical energy generated by ventricular contraction. | |||
*This is equal to the sum of the stroke work (SW), encompassed within the PV loop, and the elastic potential energy (PE). | |||
**PVA = PE + SW | |||
== Pressure- Volume Loop Changes in Cardiac Abnormalities == | |||
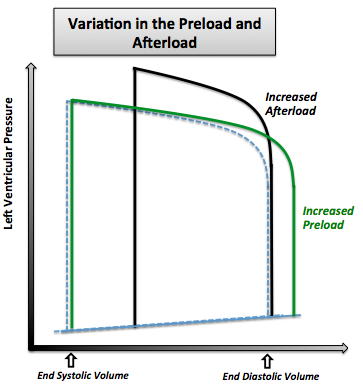
===Variation in Preload and Afterload=== | |||
*When preload increases the following changes are observed: | |||
**Increased end diastolic volume | |||
**Increased stroke volume | |||
**No changes in pressure | |||
*When afterload increases the following changes are observed: | |||
**Increased end systolic volume | |||
**Decreased stroke volume | |||
**Increased ventricular pressure because the ventricles need to contract more in order to overcome the afterload | |||
The | ;Below is an image showing the pressure volume graph in case of changes in preload and afterload. | ||
[[Image:Variation_in_the_Preload_and_Afterload.png|300px|The variation in the pressure volume loop in case of increased preload and in the case of increased afterload. Note that the normal pressure volume diagram is in dotted line.]] | |||
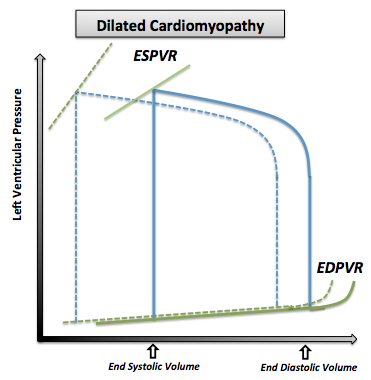
=== Dilated Cardiomyopathy === | |||
*In [[dilated cardiomyopathy]], the ventricle becomes dilated without compensatory thickening of the wall and consequently the following changes are observed: | |||
**Decreased contractility of the left ventricle that is illustrated by a shift to the right of the ESPVR curve | |||
**Decreased ventricular compliance illustrated by the shift to the right of the EDPVR curve | |||
**Decreased stroke volume leading to an increase in the end systolic volume | |||
**Increased end diastolic volume due to the dilatation of the ventricles | |||
**Decreased cardiac output | |||
**No change in the ventricular pressures accompanies the changes in the volume. | |||
;Below is an image showing the pressure volume graph in case of dilated cardiomyopathy. | |||
[[Image:Dilated_Cardiomyopathy.png|300px|The pressure volume loop in dilated cardiomyopathy. Note that the normal pressure volume diagram is in dotted line]] | |||
<br clear=left> | |||
=== Left Ventricular Hypertrophy === | |||
*[[Left ventricular hypertrophy]] (LVH) is an increase in the thickness and mass of the myocardium. | |||
*The thickening of the ventricular muscle results in decreased chamber compliance and consequently the following changes are observed: | |||
* | **Elevated left ventricular pressures | ||
* | **Increased ESV | ||
* | **Decreased EDV | ||
* | **Decreased cardiac output | ||
;Below is an image showing the pressure volume curve in case of left ventricular hypertrophy (LVH) with associated reduced stroke volume (SV), end diastolic volume (EDV) and increased left ventricular pressure (LVP). | |||
[[Image:Left_Ventricular_Hypertrophy.png|300px|The pressure volume loop in left ventricular hypertrophy. Note that the normal pressure volume diagram is in dotted line.]] | |||
== | *There are two exceptions to these changes, where moderate hypertrophy allows for a lower heart rate, increased diastolic volume, and thus higher stroke volume: | ||
**Increased left ventricular hypertrophy with increased EDV and SV seen with athletes<ref>{{cite web|last=Scharhag|first=J.ürgen|title=Athlete’s heart|url=http://content.onlinejacc.org/cgi/content/figsonly/40/10/1856|work=Athlete’s heart}}</ref> | |||
**Increased left ventricular hypertrophy in healthy normal elderly individuals. | |||
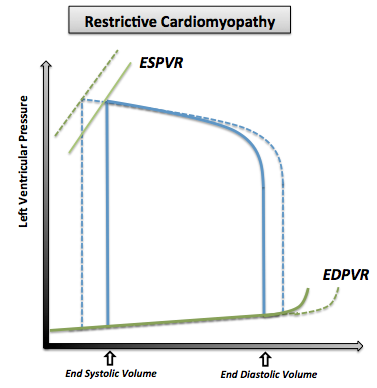
=== | === Restrictive Cardiomyopathy === | ||
*[[Restrictive cardiomyopathy]] includes a group of heart disorders in which the walls of the ventricles become stiff (but not necessarily thickened) and resist normal filling with blood between heartbeats. | |||
*This condition occurs when heart muscle is gradually infiltrated or replaced by scar tissue or when abnormal substances accumulate in the heart muscle and consequently the following changes are observed: | |||
**Normal ventricular systolic pressure | |||
**Elevated diastolic pressure | |||
**Reduced cardiac output | |||
;Below is an image showing the pressure volume curve in case of restrictive cardiomyopathy with associated reduced stroke volume. | |||
[[Image:Restrictive_Cardiomyopathy.png|300px|The pressure volume curve in restrictive cardiomyopathy. Note that the normal pressure volume diagram is in dotted line.]] | |||
==== | === Valvular Diseases === | ||
[[ | ==== Aortic Stenosis ==== | ||
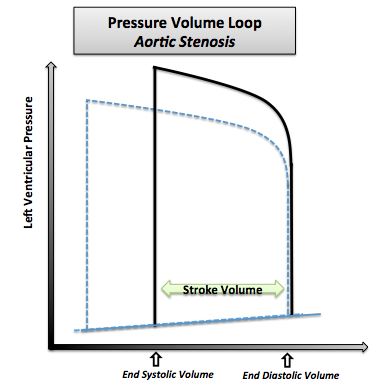
*[[Aortic valve stenosis]] is the abnormal narrowing of the aortic valve. | |||
*This results in the left ventricle pressures being much greater than the aortic pressures during left ventricular ejection. The magnitude of the pressure gradient is determined by the severity of the stenosis and the flow rate across the valve. | |||
*The following changes are observed in severe aortic stenosis: | |||
** Reduced ventricular stroke volume due to increased afterload (which decreases ejection velocity) | |||
** Increased end-systolic volume | |||
** Compensatory increase in end-diastolic volume and pressure | |||
; Below is an image showing a pressure volume diagram in case of aortic stenosis depicting increased end systolic pressure and reduced stroke volume. | |||
[[Image:Pressure_Volume_Loop_Aortic_Stenosis.png|300px|Pressure-volume loop in aortic stenosis. Note that the normal pressure volume diagram is in dotted line.]] | |||
==== Mitral Stenosis ==== | |||
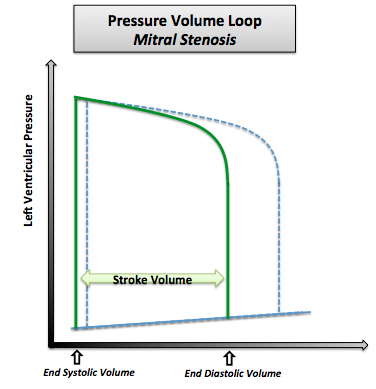
*Mitral stenosis is the abnormal narrowing of the mitral valve orifice. | |||
*The following changes are observed in[[mitral stenosis]]: | |||
**Decreased end-diastolic volume (preload) due to impaired left ventricular filling | |||
**Decreased stroke volume resulting from the decreased preload according to the Frank–Starling mechanism | |||
**Decreased cardiac output and aortic pressure (afterload) as the stroke volume is decreased | |||
**Slightly decreased end-systolic volume due to the decrease in the afterload | |||
;Below is an image showing a pressure volume curve in case of mitral stenosis depicting reduced end diastolic volume and reduced stroke volume. | |||
[[Image:Pressure_Volume_Loop_Mitral_Stenosis.png|300px|Pressure-volume loop in mitral stenosis. Note that the normal pressure volume loop is in dotted line.]] | |||
=== | ==== Aortic Regurgitation ==== | ||
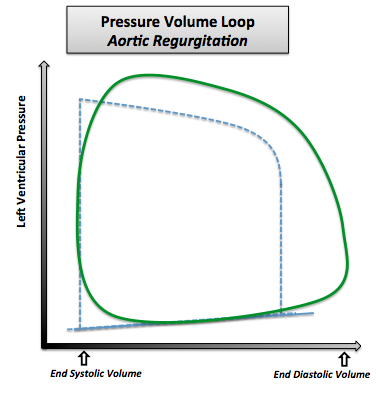
[[ | *[[Aortic insufficiency]] (AI) or regurgitation is the failure of the valve to close completely at the end of systolic ejection, causing leakage of blood back through the valve during LV diastole. | ||
*The following changes are observed in aortic regurgitation: | |||
**Increased end diastolic volume (preload) because the LV volume is greatly increased due to the enhanced ventricular filling from the constant backflow of blood through the leaky valve | |||
**Increased systolic pressure and stroke volume due to the elevated preload according to the Frank–Starling mechanism | |||
* Not that when the LV begins to contract and develop pressure, blood is still entering the LV from the aorta (since aortic pressure is higher than LV pressure), implying that there is no true isovolumic contraction. Once the LV pressure exceeds the aortic diastolic pressure, the LV begins to eject blood into the aorta. | |||
;Below is an image showing the pressure volume curve in case of aortic regurgitation depicting increased end diastolic volume, increased stroke volume and increased LV systolic pressure. | |||
[[Image:Pressure_Volume_Loop_Aortic_Regurgitation.png|300px|Pressure-volume loop in aortic regurgitation. Note that the normal pressure-volume diagram is in dotted line.]] | |||
==== Mitral Regurgitation ==== | |||
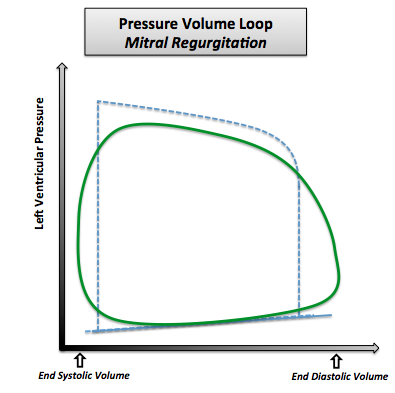
*[[Mitral regurgitation]] (MR) is the failure of the mitral valve to close completely, causing blood to flow back into the left atrium during ventricular systole. | |||
*The increased ventricular | |||
*The following changes are observed in mitral regurgitation: | |||
**Decreased end systolic volume due to the constant back flow of blood through the leaky valve | |||
**Increased left ventricular end diastolic volume as the volume and pressure of atria are higher than normal | |||
**Increased stroke volume in such a way that the ejection into the aorta (forward flow) is reduced as the stroke volume in this case includes the volume of blood ejected into the aorta as well as the volume ejected back into the left atrium | |||
;Below is an image showing the pressure volume curve in case of mitral regurgitation depicting increased end diastolic volume and increased stroke voume. | |||
[[Image:Pressure_Volume_Loop_Mitral_Regurgitation.png|300px|Pressure volume loop in case of mitral regurgitation. Note that the normal pressure volume loop is in dotted line.]] | |||
[[ | |||
==References== | |||
{{reflist|2}} | |||
== | |||
{{Cardiovascular physiology}} | {{Cardiovascular physiology}} | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Physiology]] | |||
{{WH}} | |||
{{WS}} | |||
== | ==Related Chapters== | ||
* [[ | * [[Stroke volume]] | ||
* [[cyclic process]] | * [[cyclic process]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
Latest revision as of 15:00, 26 October 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Assistant Editor(s)-in-Chief: Rim Halaby
Synonyms and keywords: Pressure-volume loop; P-V diagram; volume-pressure loop
Overview
- A plot of a system's pressure versus volume has long been used to measure the work done by the system and its efficiency. This analysis can be applied to heat engines and pumps, including the heart.
- Real time left ventricular (LV) pressure-volume loops provide a framework for understanding cardiac mechanics; in fact, a considerable amount of information on cardiac performance can be determined from the pressure versus volume plot (also known as pressure volume diagram).
- Several physiologically relevant hemodynamic parameters such as stroke volume, cardiac output, ejection fraction, myocardial contractility can be determined from these loops.
- To generate a pressure volume loop for the left ventricle, the left ventricular pressure is plotted against left ventricular volume at multiple time points during a single cardiac cycle.
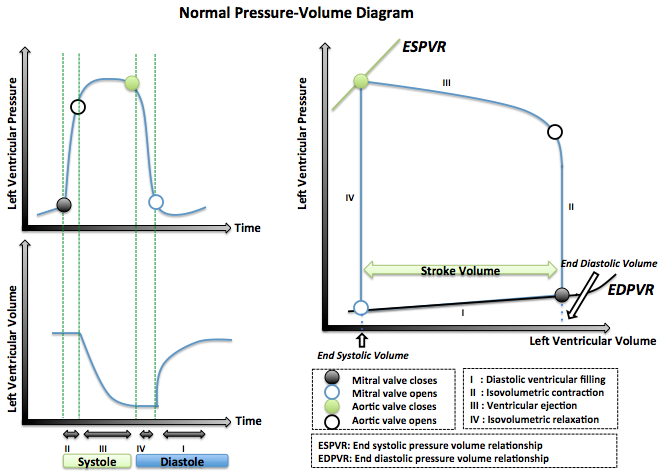
Cardiac Pressure-Volume Loop
- The left ventricular pressure-volume loop (PV loop) represents the different events of the cardiac cycle.
- To generate a PV loop for the left ventricle, the left ventricular pressure is plotted against the left ventricular volume at multiple time points during a single cardiac cycle.
- The left ventricular pressure-volume illustrates the four phases of the cardiac cycle with respect to pressure and volume changes:
- Phase I: Diastolic ventricular filling
- The mitral valve is open while the aortic valve is closed.
- The volume increases to reach the maximal ventricular capacity known as end diastolic volume EDV.
- The pressure slightly increases.
- Phase II: Isovolumetric contraction
- The mitral and aortic valves are both closed.
- The volume of the blood is unchanged as the ventricles are contracting.
- The pressure inside the ventricles significantly increases.
- Phase III: Ventricular ejection
- The aortic valve opens as the pressure inside the ventricles exceeds that of the aorta.
- The blood volume inside the left ventricle decreases because it is pumped into the systemic circulation.
- Phase IV: Isovolumetric relaxation
- The aortic and mitral valves are closed.
- The volume inside the left ventricle is unchanged and it corresponds to the volume remaining in the ventricle after systole, known as end systolic volume ESV.
- The pressure inside the ventricle tremendously decreases as the ventricles are relaxing.
- Phase I: Diastolic ventricular filling
- Below is an image showing idealized pressure-volume diagram featuring cardiac cycle events.
Pressure-Volume Parameters
Stroke Volume
- Stroke volume (SV) is the amount of blood pumped by the left ventricle in a single cardiac cycle.
- The stroke volume is an indicator the left ventricular function which is mainly affected by the preload, afterload and contractility of the heart.
Stroke Work
- Ventricular stroke work (SW) is defined as the work performed by the left or right ventricle to eject the stroke volume into the aorta or pulmonary artery, respectively.
- The area enclosed by the PV loop is a measure of the ventricular stroke work, which is a product of the stroke volume and the mean aortic or pulmonary artery pressure (afterload), depending on whether one is considering the left or the right ventricle.
Cardiac Output
- Cardiac output (CO) is defined as the amount of blood pumped by the left ventricle in unit time.
- CO = Stroke Volume x Heart Rate
- The normal cardiac output is 5-6L/min and it can increase up to 5 times during exercise.
- CO is an indicator of the left ventricular function.
Ejection Fraction
- Ejection fraction (EF) is defined as the fraction of end diastolic volume that is ejected out of the ventricle during each contraction.
- Ejection Fraction = Stroke volume/end diastolic volume
- Healthy ventricles typically have ejection fractions greater than 0.55.
- Myocardial infarction or cardiomyopathy causes damage to the myocardium, which impairs the heart's ability to eject blood and therefore reduces ejection fraction. This reduction in the ejection fraction can manifest itself as heart failure.
- Low EF usually indicates systolic dysfunction and severe heart failure can result in EF lower than 0.2.
dP/dtmin and dP/dtmax
- These represent the minimum and maximum rate of pressure change in the ventricle. Peak dP/dt has historically been used as an index of ventricular performance. However, it is known to be load dependent and inferior to hemodynamic parameters defined by the PV plane.
- An increase in contractility is manifested as an increase in dP/dtmax during isovolumic contraction. However, dP/dtmax is also influenced by preload, afterload, heart rate and myocardial hypertrophy. Hence the relationship between ventricular end-diastolic volume and dP/dt is a more accurate index of contractility than dP/dt alone.
- Similarly, an increase in diastolic function or an increase in relaxation (lusitropy) causes increased dP/dtmin during isovolumic relaxation. Hence, dP/dtmin has been used as a valuable tool in the analysis of isovolumic relaxation. However, studies have shown that this parameter may not be a valid measure of LV relaxation rate, especially during acute alterations in contractility or afterload.
Isovolumic Relaxation Constant (Τau)
- Tau represents the exponential decay of the ventricular pressure during isovolumic relaxation. Several studies have shown that Tau is a preload independent measure of isovolumic relaxation.
- Calculation of Tau (Glantz method)
P(t)= P0e-t⁄τE +Pα
where
- P = pressure at time t
- P0 = amplitude constant
- τE = Glantz relaxation constant
- Pα = non zero asymptote due to pleural and pericardial pressure
- Below is an image showing the calculation of Tau using Glantz Method.

Determinants of Left Ventricular Function
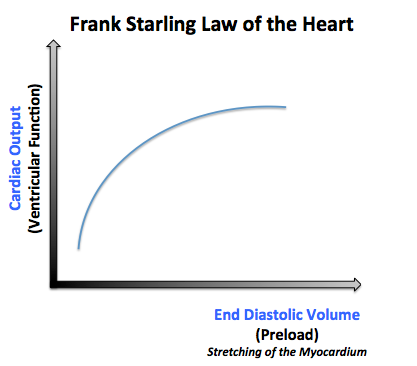
- 1- Preload:
- The preload is the volume that fills in the heart during diastole, and it is referred to as the end diastolic volume (EDV).
- According to Frank Starling's law, the larger the blood volume filling the heart is, the larger the degree of cardiac stretching is and consequently more blood is pumped.
- The Frank–Starling mechanism can be explained on the basis of preload. As the heart fills with more blood than usual, there is an increase in the load experienced by each myocyte. This stretches the muscle fibers, increasing the affinity of troponin C to Ca2+ ions causing a greater number of cross-bridges to form within the muscle fibers. This increases the contractile force of the cardiac muscle, resulting in increased stroke volume.
- Below is an image showing Frank Starling's law according to which the left ventricular function increases as the preload increases.
- 2- Afterload:
- The afterload is the pressure corresponding to the mean arterial pressure that the heart needs to overcome when pumping blood.
- When the afterload increases, it makes it harder for the heart to pump the blood, and thus the volume remaining in the ventricles after ventricular contraction (end systolic volume) will increase and the stroke volume will be low.
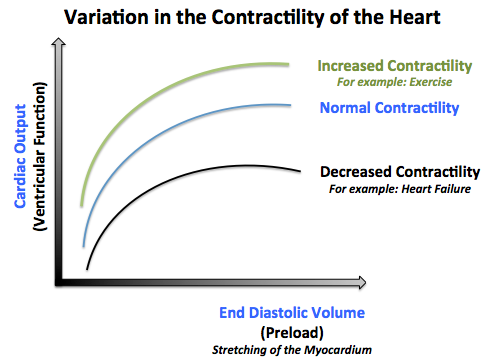
- 3- Contractility:
- The contractility of the heart is defined as the intrinsic force with which the heart contracts.
- Factors that increase the contractility of the heart (positive ionotropy) are: catecholamines, xanthines (caffeine), medications (Digitalis).
- Factors that decrease the contractlity of the heart (negative ionotropy) are: hypercapnea, hypoxia, acidosis, medications (quinidine, procainamide, barbiturates), heart failure.[1]
- Below is an image showing various curves illustrating different states of contractlity of the heart.
Pressure-Volume Loop Analysis
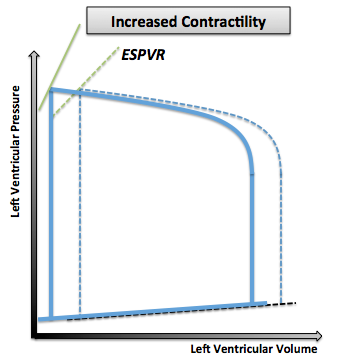
End Systolic Pressure Volume Relationship ESPVR
- End systolic pressure volume relationship (ESPVR) describes the maximal pressure that can be developed by the ventricle at any given LV volume. This implies that the PV loop cannot cross over the line defining ESPVR for any given contractile state.
- The slope of ESPVR represents the end-systolic elastance, which provides an index of myocardial contractility.
- The ESPVR is relatively insensitive to changes in preload, afterload and heart rate. This makes it an improved index of systolic function over other hemodynamic parameters like ejection fraction, cardiac output and stroke volume.
- The ESPVR becomes steeper and shifts to the left as inotropy (contractility) increases.
- The ESPVR becomes flatter and shifts to the right as inotropy decreases.
- Below is an image showing a pressure-volume loop with a steeper ESPVR that shifts to the left in the case of increased inotropy or contractility.
End Diastolic Pressure Volume Relationship EDPVR
- End diastolic pressure volume relationship (EDPVR) describes the passive filling curve for the ventricle and thus the passive properties of the myocardium.
- The slope of the EDPVR at any point along this curve is the reciprocal of ventricular compliance (or ventricular stiffness).
- If ventricular compliance is decreased (such as in ventricular hypertrophy):
- The ventricle is stiffer.
- This results in higher ventricular end-diastolic pressures (EDP) at any given end-diastolic volume (EDV).
- Alternatively, for a given EDP, a less compliant ventricle would have a smaller EDV due to impaired filling.
- If ventricular compliance increases (such as in dilated cardiomyopathy):
- The EDV may be very high but the EDP may not be greatly elevated.
- If ventricular compliance is decreased (such as in ventricular hypertrophy):
- Below is an image showing a pressure volume loop with changes in the EDPVR's part resulting from variations in the ventricular compliance.
Pressure Volume Area
- The Pressure-volume area (PVA) represents the total mechanical energy generated by ventricular contraction.
- This is equal to the sum of the stroke work (SW), encompassed within the PV loop, and the elastic potential energy (PE).
- PVA = PE + SW
Pressure- Volume Loop Changes in Cardiac Abnormalities
Variation in Preload and Afterload
- When preload increases the following changes are observed:
- Increased end diastolic volume
- Increased stroke volume
- No changes in pressure
- When afterload increases the following changes are observed:
- Increased end systolic volume
- Decreased stroke volume
- Increased ventricular pressure because the ventricles need to contract more in order to overcome the afterload
- Below is an image showing the pressure volume graph in case of changes in preload and afterload.
Dilated Cardiomyopathy
- In dilated cardiomyopathy, the ventricle becomes dilated without compensatory thickening of the wall and consequently the following changes are observed:
- Decreased contractility of the left ventricle that is illustrated by a shift to the right of the ESPVR curve
- Decreased ventricular compliance illustrated by the shift to the right of the EDPVR curve
- Decreased stroke volume leading to an increase in the end systolic volume
- Increased end diastolic volume due to the dilatation of the ventricles
- Decreased cardiac output
- No change in the ventricular pressures accompanies the changes in the volume.
- Below is an image showing the pressure volume graph in case of dilated cardiomyopathy.
Left Ventricular Hypertrophy
- Left ventricular hypertrophy (LVH) is an increase in the thickness and mass of the myocardium.
- The thickening of the ventricular muscle results in decreased chamber compliance and consequently the following changes are observed:
- Elevated left ventricular pressures
- Increased ESV
- Decreased EDV
- Decreased cardiac output
- Below is an image showing the pressure volume curve in case of left ventricular hypertrophy (LVH) with associated reduced stroke volume (SV), end diastolic volume (EDV) and increased left ventricular pressure (LVP).
- There are two exceptions to these changes, where moderate hypertrophy allows for a lower heart rate, increased diastolic volume, and thus higher stroke volume:
- Increased left ventricular hypertrophy with increased EDV and SV seen with athletes[2]
- Increased left ventricular hypertrophy in healthy normal elderly individuals.
Restrictive Cardiomyopathy
- Restrictive cardiomyopathy includes a group of heart disorders in which the walls of the ventricles become stiff (but not necessarily thickened) and resist normal filling with blood between heartbeats.
- This condition occurs when heart muscle is gradually infiltrated or replaced by scar tissue or when abnormal substances accumulate in the heart muscle and consequently the following changes are observed:
- Normal ventricular systolic pressure
- Elevated diastolic pressure
- Reduced cardiac output
- Below is an image showing the pressure volume curve in case of restrictive cardiomyopathy with associated reduced stroke volume.
Valvular Diseases
Aortic Stenosis
- Aortic valve stenosis is the abnormal narrowing of the aortic valve.
- This results in the left ventricle pressures being much greater than the aortic pressures during left ventricular ejection. The magnitude of the pressure gradient is determined by the severity of the stenosis and the flow rate across the valve.
- The following changes are observed in severe aortic stenosis:
- Reduced ventricular stroke volume due to increased afterload (which decreases ejection velocity)
- Increased end-systolic volume
- Compensatory increase in end-diastolic volume and pressure
- Below is an image showing a pressure volume diagram in case of aortic stenosis depicting increased end systolic pressure and reduced stroke volume.
Mitral Stenosis
- Mitral stenosis is the abnormal narrowing of the mitral valve orifice.
- The following changes are observed inmitral stenosis:
- Decreased end-diastolic volume (preload) due to impaired left ventricular filling
- Decreased stroke volume resulting from the decreased preload according to the Frank–Starling mechanism
- Decreased cardiac output and aortic pressure (afterload) as the stroke volume is decreased
- Slightly decreased end-systolic volume due to the decrease in the afterload
- Below is an image showing a pressure volume curve in case of mitral stenosis depicting reduced end diastolic volume and reduced stroke volume.
Aortic Regurgitation
- Aortic insufficiency (AI) or regurgitation is the failure of the valve to close completely at the end of systolic ejection, causing leakage of blood back through the valve during LV diastole.
- The following changes are observed in aortic regurgitation:
- Increased end diastolic volume (preload) because the LV volume is greatly increased due to the enhanced ventricular filling from the constant backflow of blood through the leaky valve
- Increased systolic pressure and stroke volume due to the elevated preload according to the Frank–Starling mechanism
- Not that when the LV begins to contract and develop pressure, blood is still entering the LV from the aorta (since aortic pressure is higher than LV pressure), implying that there is no true isovolumic contraction. Once the LV pressure exceeds the aortic diastolic pressure, the LV begins to eject blood into the aorta.
- Below is an image showing the pressure volume curve in case of aortic regurgitation depicting increased end diastolic volume, increased stroke volume and increased LV systolic pressure.
Mitral Regurgitation
- Mitral regurgitation (MR) is the failure of the mitral valve to close completely, causing blood to flow back into the left atrium during ventricular systole.
- The increased ventricular
- The following changes are observed in mitral regurgitation:
- Decreased end systolic volume due to the constant back flow of blood through the leaky valve
- Increased left ventricular end diastolic volume as the volume and pressure of atria are higher than normal
- Increased stroke volume in such a way that the ejection into the aorta (forward flow) is reduced as the stroke volume in this case includes the volume of blood ejected into the aorta as well as the volume ejected back into the left atrium
- Below is an image showing the pressure volume curve in case of mitral regurgitation depicting increased end diastolic volume and increased stroke voume.
References
- ↑ Barrett KE, Barman SM, Boitano S, Brooks HL. Chapter 30. The Heart as a Pump. In: Barrett KE, Barman SM, Boitano S, Brooks HL, eds. Ganong's Review of Medical Physiology. 24th ed. New York: McGraw-Hill; 2012.
- ↑ Scharhag, J.ürgen. "Athlete's heart". Athlete’s heart.