Portal vein thrombosis pathophysiology: Difference between revisions
Farima Kahe (talk | contribs) |
No edit summary |
||
| (23 intermediate revisions by 4 users not shown) | |||
| Line 9: | Line 9: | ||
{{Portal vein thrombosis}} | {{Portal vein thrombosis}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}} {{F.K}} | ||
==Overview== | ==Overview== | ||
It seems portal vein thrombosis is caused by [[Virchow's triad]] which includes: Reduced portal blood flow, [[hypercoagulable state]], and vascular [[endothelial]] injury. There are two mechanisms that contribute in loss of [[portal vein]] blood flow to liver, [[arterial]] rescue and [[venous]] rescue. It is a rapid process and takes a few days to start and 3-5 weeks to complete after [[portal vein]] obstruction. Collateral vessel joins to form [[cavernoma]] which connects the proximal and distal part of thrombosed [[portal vein]]. Finally, the [[portal vein]] becomes a fibrosed and thin cord. All these events leads to low [[systemic vascular resistance]] and high. These are the characterstic findings of hyperkinetic circulation. | |||
It | |||
[ | |||
[ | |||
==Structure== | ==Structure== | ||
* [[Portal vein]] is formed by the union of the [[splenic vein]] and [[superior mesenteric vein]] and divides into a right and a left branch before entering the [[liver]]. | |||
* The [[portal vein]] drains blood into the liver, not from the liver, the blood entering the liver from the [[portal vein]], after being cleaned by the liver, flows into the [[inferior vena cava]] via the [[hepatic vein]]s. | |||
* The [[inferior mesenteric vein]] usually does not directly connect to the hepatic portal vein; it drains into the splenic vein. | |||
*[[ | |||
* [[Portal vein]] branches into many generations of [[vessels]] that open into [[Liver sinusoid|hepatic sinusoids]]. Blood is recollected into the [[hepatic vein]] and enters the [[inferior vena cava]]. | |||
===Tributaries=== | ===Tributaries=== | ||
The tributaries of the hepatic portal vein include: | The tributaries of the hepatic [[portal vein]] include: | ||
* [[Left gastric vein]] and [[right gastric vein]] | * [[Left gastric vein]] and [[right gastric vein]] | ||
* [[Superior mesenteric vein]] | * [[Superior mesenteric vein]] | ||
| Line 59: | Line 30: | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
*It is thought that vein thrombosis is caused by Virchow's triad which includes:<ref name="pmid25941431">{{cite journal |vauthors=Chawla YK, Bodh V |title=Portal vein thrombosis |journal=J Clin Exp Hepatol |volume=5 |issue=1 |pages=22–40 |year=2015 |pmid=25941431 |pmc=4415192 |doi=10.1016/j.jceh.2014.12.008 |url=}}</ref> | *It is thought that [[Venous thrombosis|vein thrombosis]] is caused by [[Virchow's triad]] which includes:<ref name="pmid25941431">{{cite journal |vauthors=Chawla YK, Bodh V |title=Portal vein thrombosis |journal=J Clin Exp Hepatol |volume=5 |issue=1 |pages=22–40 |year=2015 |pmid=25941431 |pmc=4415192 |doi=10.1016/j.jceh.2014.12.008 |url=}}</ref> | ||
**Reduced portal blood flow | **Reduced portal blood flow | ||
**Hypercoagulable state | **[[Hypercoagulable state]] | ||
**Vascular endothelial injury | **Vascular [[endothelial]] injury | ||
*There are two mechanisms that contribute in loss of portal vein blood flow to liver:<ref name="pmid2806552">{{cite journal |vauthors=Zhang WW, Churchill S, Churchill P |title=Developmental regulation of D-beta-hydroxybutyrate dehydrogenase in rat liver and brain |journal=FEBS Lett. |volume=256 |issue=1-2 |pages=71–4 |year=1989 |pmid=2806552 |doi= |url=}}</ref> | |||
**Arterial rescue | <figure-inline><figure-inline><figure-inline><figure-inline>[[File:VTE Pathophysisology Virchow's triad.JPG|639x639px]]</figure-inline></figure-inline></figure-inline></figure-inline> | ||
***Arterial rescue is the phenomenon that occurs after portal vein clamping during liver surgery.<ref name="pmid1505914">{{cite journal |vauthors=Henderson JM, Gilmore GT, Mackay GJ, Galloway JR, Dodson TF, Kutner MH |title=Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows |journal=Hepatology |volume=16 |issue=3 |pages=715–8 |year=1992 |pmid=1505914 |doi= |url=}}</ref> | |||
***It is a vascular reflex present in organs with both arterial and venous supply. | Shown below is a table depicting the elements of Virchow's triad and their modern counterparts. | ||
***It has a role in preserving liver function in the acute stages of portal vein thrombosis. | |||
**Venous rescue | {| | ||
***Venous rescue is the phenomenon of neovascularization by forming collateral vessels. | |- | ||
***It helps to bypass the obstruction. | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Virchow's<ref name="isbn1-4020-6649-X">{{cite book |author=Agutter, Paul S. |title=The Aetiology of Deep Venous Thrombosis: A Critical, Historical and Epistemological Survey |publisher=Springer |location=Berlin |year=2008 |pages=84 |isbn=1-4020-6649-X |oclc= |doi= |accessdate=}}</ref> | ||
***It is a rapid process and takes a few days to start and 3-5 weeks to complete after portal vein obstruction.<ref name="pmid7572494">{{cite journal |vauthors=De Gaetano AM, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K |title=Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography |journal=AJR Am J Roentgenol |volume=165 |issue=5 |pages=1151–5 |year=1995 |pmid=7572494 |doi=10.2214/ajr.165.5.7572494 |url=}}</ref> | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Modern | ||
***Collateral vessel joins to form cavernoma which connects the proximal and distal part of thrombosed portal vein. | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Notes | ||
***Finally, the portal vein becomes fibrosed | |- | ||
*All these events leads to low systemic vascular resistance and high cardiac output. These are the characterstic findings of hyperkinetic circulation.<ref name="pmid16286254">{{cite journal |vauthors=Wang JT, Zhao HY, Liu YL |title=Portal vein thrombosis |journal=HBPD INT |volume=4 |issue=4 |pages=515–8 |year=2005 |pmid=16286254 |doi= |url=}}</ref> | ! style="background:#DCDCDC;" align="center" + |Phenomena of interrupted [[blood]]-flow | ||
| style="background:#DCDCDC;" align="center" + |"Stasis" or "[[venous stasis]]"<ref name="pmid15692260">{{cite journal |author=Lowe GD |title=Virchow's triad revisited: abnormal flow |journal=Pathophysiol. Haemost. Thromb. |volume=33 |issue=5-6 |pages=455–7 |year=2003 |pmid=15692260 |doi=10.1159/000083845 |url=http://content.karger.com/produktedb/produkte.asp?doi=10.1159/000083845&typ=pdf}}</ref> | |||
| style="background:#F5F5F5;" + | | |||
* The first category, alterations in normal [[blood]] flow, refers to several situations. | |||
* These include [[turbulence]], [[stasis (medicine)|stasis]], [[mitral stenosis]], and [[varicose veins]]. | |||
* The equivalence of [[Virchow's triad|Virchow's]] version and the modern version has been disputed.<ref name="urlFurther reflections on Virchows triad. - Free Online Library">{{cite web |url=http://www.thefreelibrary.com/Further+reflections+on+Virchow%27s+triad.(Letter+to+the+Editor)-a0128075135 |title=Further reflections on Virchow's triad. - Free Online Library |format= |work= |accessdate=2009-02-10}}</ref> | |||
|- | |||
! style="background:#DCDCDC;" align="center" + |Phenomena associated with irritation of the [[vessel]] and its vicinity | |||
| style="background:#DCDCDC;" align="center" + |"Endothelial injury" or "vessel wall injury" | |||
| style="background:#F5F5F5;" + | | |||
* The second category, injuries and/or [[trauma]] to [[endothelium]] includes damage to the veins arising from [[shear stress]] or [[hypertension]]. | |||
|- | |||
! style="background:#DCDCDC;" align="center" + |Phenomena of [[blood]]-[[coagulation]] | |||
| style="background:#DCDCDC;" align="center" + |"[[Hypercoagulability]]" | |||
| style="background:#F5F5F5;" + | | |||
* The last category, alterations in the constitution of blood,<ref name="pmid15692259">{{cite journal |author=Chung I, Lip GY |title=Virchow's triad revisited: blood constituents |journal=Pathophysiol. Haemost. Thromb. |volume=33 |issue=5-6 |pages=449–54 |year=2003 |pmid=15692259 |doi=10.1159/000083844 |url=http://content.karger.com/produktedb/produkte.asp?doi=10.1159/000083844&typ=pdf}}</ref> has numerous possible [[risk factors]] such as [[hyperviscosity]], deficiency of [[antithrombin]] III, [[nephrotic syndrome]], changes after severe [[Physical trauma|trauma]] or burn, disseminated [[cancer]], late [[pregnancy]], and [[delivery]], race, age, whether the patient is a smoker or [[obesity|obese]]. | |||
* All of these [[risk factors]] lead to [[hypercoagulability]]. | |||
|} | |||
*There are two mechanisms that contribute in loss of [[portal vein]] blood flow to [[liver]]:<ref name="pmid2806552">{{cite journal |vauthors=Zhang WW, Churchill S, Churchill P |title=Developmental regulation of D-beta-hydroxybutyrate dehydrogenase in rat liver and brain |journal=FEBS Lett. |volume=256 |issue=1-2 |pages=71–4 |year=1989 |pmid=2806552 |doi= |url=}}</ref> | |||
**[[Arterial]] rescue: | |||
***Arterial rescue is the phenomenon that occurs after [[portal vein]] clamping during liver surgery.<ref name="pmid1505914">{{cite journal |vauthors=Henderson JM, Gilmore GT, Mackay GJ, Galloway JR, Dodson TF, Kutner MH |title=Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows |journal=Hepatology |volume=16 |issue=3 |pages=715–8 |year=1992 |pmid=1505914 |doi= |url=}}</ref> | |||
***It is a vascular reflex present in organs with both [[arterial]] and [[venous]] supply. | |||
***It has a role in preserving [[liver function]] in the acute stages of [[portal vein]] thrombosis. | |||
**Venous rescue: | |||
***Venous rescue is the phenomenon of [[neovascularization]] by forming collateral vessels. | |||
***It helps to bypass the [[obstruction]]. | |||
***It is a rapid process and takes a few days to start and 3-5 weeks to complete after [[portal vein]] obstruction.<ref name="pmid7572494">{{cite journal |vauthors=De Gaetano AM, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K |title=Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography |journal=AJR Am J Roentgenol |volume=165 |issue=5 |pages=1151–5 |year=1995 |pmid=7572494 |doi=10.2214/ajr.165.5.7572494 |url=}}</ref> | |||
***Collateral vessel joins to form [[cavernoma]] which connects the proximal and distal part of thrombosed [[portal vein]]. | |||
***Finally, the [[portal vein]] becomes a fibrosed and thin cord.<ref name="pmid19299846">{{cite journal |vauthors=Hoekstra J, Janssen HL |title=Vascular liver disorders (II): portal vein thrombosis |journal=Neth J Med |volume=67 |issue=2 |pages=46–53 |year=2009 |pmid=19299846 |doi= |url=}}</ref> | |||
*All these events leads to low [[systemic vascular resistance]] and high [[cardiac output]]. These are the characterstic findings of hyperkinetic circulation.<ref name="pmid16286254">{{cite journal |vauthors=Wang JT, Zhao HY, Liu YL |title=Portal vein thrombosis |journal=HBPD INT |volume=4 |issue=4 |pages=515–8 |year=2005 |pmid=16286254 |doi= |url=}}</ref> | |||
==Genetics== | ==Genetics== | ||
* | *The development of [[portal vein]] thrombosis is the result of G201210A mutations. | ||
==Associated Conditions== | ==Associated Conditions== | ||
*Conditions associated with [[portal vein]] thrombosis include:<ref name="pmid25941431">{{cite journal |vauthors=Chawla YK, Bodh V |title=Portal vein thrombosis |journal=J Clin Exp Hepatol |volume=5 |issue=1 |pages=22–40 |year=2015 |pmid=25941431 |pmc=4415192 |doi=10.1016/j.jceh.2014.12.008 |url=}}</ref><ref name="pmid11159889">{{cite journal |vauthors=Condat B, Pessione F, Hillaire S, Denninger MH, Guillin MC, Poliquin M, Hadengue A, Erlinger S, Valla D |title=Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy |journal=Gastroenterology |volume=120 |issue=2 |pages=490–7 |year=2001 |pmid=11159889 |doi= |url=}}</ref><ref name="pmid18814081">{{cite journal |vauthors=Garcia-Pagán JC, Hernández-Guerra M, Bosch J |title=Extrahepatic portal vein thrombosis |journal=Semin. Liver Dis. |volume=28 |issue=3 |pages=282–92 |year=2008 |pmid=18814081 |doi=10.1055/s-0028-1085096 |url=}}</ref> | |||
**[[Cirrhosis]] | |||
**[[Hepatocellular carcinoma]] | |||
**Portal [[cavernoma]] | |||
**Gastric or [[esophageal varices]]/bleeding | |||
**[[Hepatic encephalopathy]] | |||
**Portal biliopathy or cholangiopathy | |||
**[[Peritonitis]] | |||
**[[Hypoxia]] or [[pulmonary artery hypertension]] | |||
**[[Portal hypertensive gastropathy]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
* | *There is no finding on [[gross pathology]] of [[portal vein]] thrombosis. | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
* | *There is no finding on microscopic histopathological analysis. | ||
==References== | ==References== | ||
Latest revision as of 14:10, 29 December 2017
| https://www.youtube.com/watch?v=RKxoYs3mDew%7C350}} |
|
Portal vein thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Portal vein thrombosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Portal vein thrombosis pathophysiology |
|
Risk calculators and risk factors for Portal vein thrombosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Farima Kahe M.D. [2]
Overview
It seems portal vein thrombosis is caused by Virchow's triad which includes: Reduced portal blood flow, hypercoagulable state, and vascular endothelial injury. There are two mechanisms that contribute in loss of portal vein blood flow to liver, arterial rescue and venous rescue. It is a rapid process and takes a few days to start and 3-5 weeks to complete after portal vein obstruction. Collateral vessel joins to form cavernoma which connects the proximal and distal part of thrombosed portal vein. Finally, the portal vein becomes a fibrosed and thin cord. All these events leads to low systemic vascular resistance and high. These are the characterstic findings of hyperkinetic circulation.
Structure
- Portal vein is formed by the union of the splenic vein and superior mesenteric vein and divides into a right and a left branch before entering the liver.
- The portal vein drains blood into the liver, not from the liver, the blood entering the liver from the portal vein, after being cleaned by the liver, flows into the inferior vena cava via the hepatic veins.
- The inferior mesenteric vein usually does not directly connect to the hepatic portal vein; it drains into the splenic vein.
- Portal vein branches into many generations of vessels that open into hepatic sinusoids. Blood is recollected into the hepatic vein and enters the inferior vena cava.
Tributaries
The tributaries of the hepatic portal vein include:
Pathophysiology
Pathogenesis
- It is thought that vein thrombosis is caused by Virchow's triad which includes:[1]
- Reduced portal blood flow
- Hypercoagulable state
- Vascular endothelial injury
<figure-inline><figure-inline><figure-inline><figure-inline>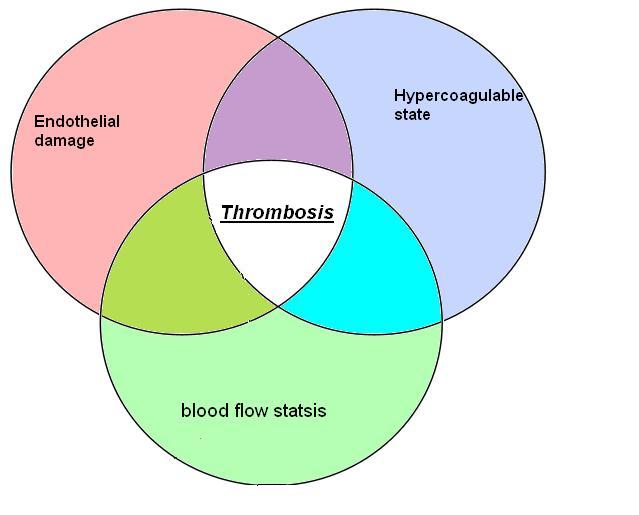
Shown below is a table depicting the elements of Virchow's triad and their modern counterparts.
| Virchow's[2] | Modern | Notes |
|---|---|---|
| Phenomena of interrupted blood-flow | "Stasis" or "venous stasis"[3] |
|
| Phenomena associated with irritation of the vessel and its vicinity | "Endothelial injury" or "vessel wall injury" |
|
| Phenomena of blood-coagulation | "Hypercoagulability" |
|
- There are two mechanisms that contribute in loss of portal vein blood flow to liver:[6]
- Arterial rescue:
- Arterial rescue is the phenomenon that occurs after portal vein clamping during liver surgery.[7]
- It is a vascular reflex present in organs with both arterial and venous supply.
- It has a role in preserving liver function in the acute stages of portal vein thrombosis.
- Venous rescue:
- Venous rescue is the phenomenon of neovascularization by forming collateral vessels.
- It helps to bypass the obstruction.
- It is a rapid process and takes a few days to start and 3-5 weeks to complete after portal vein obstruction.[8]
- Collateral vessel joins to form cavernoma which connects the proximal and distal part of thrombosed portal vein.
- Finally, the portal vein becomes a fibrosed and thin cord.[9]
- Arterial rescue:
- All these events leads to low systemic vascular resistance and high cardiac output. These are the characterstic findings of hyperkinetic circulation.[10]
Genetics
- The development of portal vein thrombosis is the result of G201210A mutations.
Associated Conditions
- Conditions associated with portal vein thrombosis include:[1][11][12]
- Cirrhosis
- Hepatocellular carcinoma
- Portal cavernoma
- Gastric or esophageal varices/bleeding
- Hepatic encephalopathy
- Portal biliopathy or cholangiopathy
- Peritonitis
- Hypoxia or pulmonary artery hypertension
- Portal hypertensive gastropathy
Gross Pathology
- There is no finding on gross pathology of portal vein thrombosis.
Microscopic Pathology
- There is no finding on microscopic histopathological analysis.
References
- ↑ 1.0 1.1 Chawla YK, Bodh V (2015). "Portal vein thrombosis". J Clin Exp Hepatol. 5 (1): 22–40. doi:10.1016/j.jceh.2014.12.008. PMC 4415192. PMID 25941431.
- ↑ Agutter, Paul S. (2008). The Aetiology of Deep Venous Thrombosis: A Critical, Historical and Epistemological Survey. Berlin: Springer. p. 84. ISBN 1-4020-6649-X.
- ↑ Lowe GD (2003). "Virchow's triad revisited: abnormal flow". Pathophysiol. Haemost. Thromb. 33 (5–6): 455–7. doi:10.1159/000083845. PMID 15692260.
- ↑ "Further reflections on Virchow's triad. - Free Online Library". Retrieved 2009-02-10.
- ↑ Chung I, Lip GY (2003). "Virchow's triad revisited: blood constituents". Pathophysiol. Haemost. Thromb. 33 (5–6): 449–54. doi:10.1159/000083844. PMID 15692259.
- ↑ Zhang WW, Churchill S, Churchill P (1989). "Developmental regulation of D-beta-hydroxybutyrate dehydrogenase in rat liver and brain". FEBS Lett. 256 (1–2): 71–4. PMID 2806552.
- ↑ Henderson JM, Gilmore GT, Mackay GJ, Galloway JR, Dodson TF, Kutner MH (1992). "Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows". Hepatology. 16 (3): 715–8. PMID 1505914.
- ↑ De Gaetano AM, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K (1995). "Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography". AJR Am J Roentgenol. 165 (5): 1151–5. doi:10.2214/ajr.165.5.7572494. PMID 7572494.
- ↑ Hoekstra J, Janssen HL (2009). "Vascular liver disorders (II): portal vein thrombosis". Neth J Med. 67 (2): 46–53. PMID 19299846.
- ↑ Wang JT, Zhao HY, Liu YL (2005). "Portal vein thrombosis". HBPD INT. 4 (4): 515–8. PMID 16286254.
- ↑ Condat B, Pessione F, Hillaire S, Denninger MH, Guillin MC, Poliquin M, Hadengue A, Erlinger S, Valla D (2001). "Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy". Gastroenterology. 120 (2): 490–7. PMID 11159889.
- ↑ Garcia-Pagán JC, Hernández-Guerra M, Bosch J (2008). "Extrahepatic portal vein thrombosis". Semin. Liver Dis. 28 (3): 282–92. doi:10.1055/s-0028-1085096. PMID 18814081.