Pericarditis CT
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis CT On the Web |
|
American Roentgen Ray Society Images of Pericarditis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Computed Tomography (CT) in Pericarditis [1] [2]
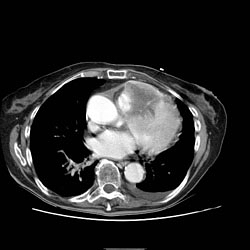
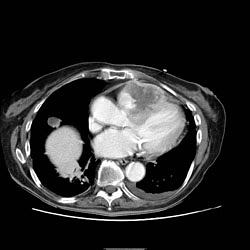
Pericardial Effusion
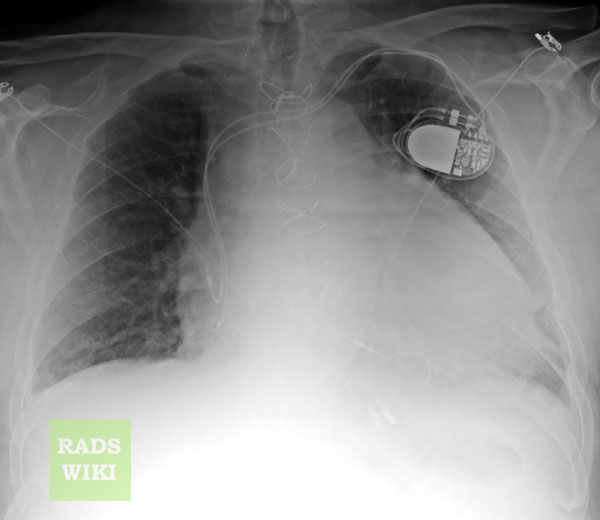
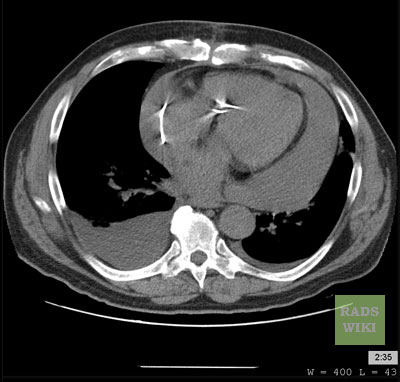
Cross-sectional imaging by CT or MRI is very sensitive in the detection of generalized or loculated pericardial effusions. Some fluid in the pericardial sac contributes to the apparent thickness and should be considered normal. Commonly, free-flowing fluid accumulates first at the posterolateral aspect of the left ventricle, when the patient is imaged in the supine position.
Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Compared to cardiac ultrasound, CT and MRI may be particularly helpful in detecting loculated effusions, owing to the wide field of view provided by these techniques. Hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion. Effusions are often incidentally noted on CT scans obtained for other indications.
Pericardial thickening (thickness >4 mm) is difficult to differentiate from a small generalized effusion. Both entities will reveal a low signal/density line that is thicker than the normal pericardial thickness. In acute pericarditis, the pericardial lining can show intermediate signal intensity and may enhance after gadolinium administration.
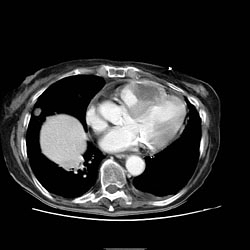
Constrictive Pericarditis
Pericardial thickening may result in constrictive pericarditis. In this entity, pericardial thickening will hamper cardiac function, with hemodynamic consequences. Many disease conditions can lead to constrictive pericarditis (infection, tumor, radiation, heart surgery, etc.).
The diagnostic features include thickened pericardium in conjunction with signs of impaired right ventricular function: dilatation of caval veins and hepatic veins, enlargement of the right atrium, and the right ventricle itself may be normal or even reduced (tubular, sigmoid) in size due to compression. Localized pericardial thickening may also cause functional impairment (localized constrictive pericarditis). Sometimes constriction may occur despite a normal appearance of the pericardium.
Pericardial calcifications are easily visualized by CT but may be difficult or impossible to appreciate on MRI.
Pericardial Tumor
A pericardial cyst is most commonly located at the right cardiophrenic angle. On T1, it appears either as a low signal or an intermediate signal due to high protein content, or with a characteristic light-bulb appearance on T2.
Unusual tumors may arise from the pericardium (mesothelioma, angiosarcoma, etc.). Malignant primary tumors have many overlapping imaging features and generally cannot be differentiated. The role of cross-sectional imaging is to establish a diagnosis and to define the extent of the lesion (invasion of cardiac structures, veins, pericardium, etc.). Sometimes lesions may have helpful signal characteristics to suggest a specific diagnosis, e.g., high-signal fat on T1 or low-density fat on CT in lipoma / liposarcoma.
Secondary tumors are much more common than primary tumors. Lung cancer may invade the mediastinal and cardiac structures directly or indirectly.
The most common secondary tumors affecting the heart are lung cancer, breast cancer, and lymphoma. Metastatic pericardial disease commonly presents as hemorrhagic effusion. Tumor nodules may enhance after intravenous gadolinium administration.
Pericardial Metastases