Pancreatic cancer pathophysiology: Difference between revisions
No edit summary |
|||
| (43 intermediate revisions by 3 users not shown) | |||
| Line 6: | Line 6: | ||
|} | |} | ||
__NOTOC__ | __NOTOC__ | ||
{{Pancreatic cancer}} | {{Pancreatic cancer}} | ||
{{CMG}}; {{AE}} {{Cherry}} | |||
==Overview== | ==Overview== | ||
The | The development of [[pancreatic cancer]] is influenced by complex interactions between several cellular [[Cell signaling|signaling]] pathways that include inactivation of [[Tumor suppressor gene|tumor suppressor genes]], activation of [[Oncogene|oncogenes]] and deregulation of molecules in various [[Signal transduction|signaling pathways]]. Some of the important [[Tumor suppressor gene|tumor suppressor genes]] involved are [[P53 (protein)|p53]], [[P16 (gene)|p16]], ''p27CIP1'', ''DPC4'' and [[BRCA2]]. These [[Tumor suppressor gene|tumor suppressor genes]] are commonly inactivated by [[Deletion (genetics)|deletion]], [[Methylation|hypermethylation]] or [[mutation]]. The [[Oncogene|oncogenes]] involved in the [[pathogenesis]] of [[pancreatic cancer]] include [[Ras]], [[Cyclooxygenase|Cox-2]], [[AKT|Akt]]-2, [[Notch]], [[Cyclin D1|Cyclin- D1]] [[Gene|genes]]. [[Signal transduction|Signal transduction pathways]] such as [[EGFR]], [[AKT|Akt]], [[NF-kB]] and [[Hedgehog signaling pathway|Hedgehog]] pathways undergo [[Genomics|genomic]] alterations and crosstalk between these pathways plays an important role in [[Pancreas|pancreatic]] [[tumorigenesis]]. | ||
[ | |||
[ | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis and Genetics=== | ===Pathogenesis and Genetics=== | ||
*The pathogenesis of [[pancreatic cancer]] involves the activation or inactivation of multiple [[gene]] subsets.<ref name="pmid12946833">{{cite journal |vauthors=Cowgill SM, Muscarella P |title=The genetics of pancreatic cancer |journal=Am. J. Surg. |volume=186 |issue=3 |pages=279–86 |year=2003 |pmid=12946833 |doi= |url=}}</ref><ref name="pmid10436789">{{cite journal |vauthors=Hruban RH, Petersen GM, Goggins M, Tersmette AC, Offerhaus GJ, Falatko F, Yeo CJ, Kern SE |title=Familial pancreatic cancer |journal=Ann. Oncol. |volume=10 Suppl 4 |issue= |pages=69–73 |year=1999 |pmid=10436789 |doi= |url=}}</ref><ref name="pmid17958761">{{cite journal |vauthors=Greer JB, Whitcomb DC, Brand RE |title=Genetic predisposition to pancreatic cancer: a brief review |journal=Am. J. Gastroenterol. |volume=102 |issue=11 |pages=2564–9 |year=2007 |pmid=17958761 |doi=10.1111/j.1572-0241.2007.01475.x |url=}}</ref><ref name="pmid16760004">{{cite journal |vauthors=Soto JL, Barbera VM, Saceda M, Carrato A |title=Molecular biology of exocrine pancreatic cancer |journal=Clin Transl Oncol |volume=8 |issue=5 |pages=306–12 |year=2006 |pmid=16760004 |doi= |url=}}</ref><ref name="pmid18580095">{{cite journal |vauthors=Shi C, Daniels JA, Hruban RH |title=Molecular characterization of pancreatic neoplasms |journal=Adv Anat Pathol |volume=15 |issue=4 |pages=185–95 |year=2008 |pmid=18580095 |doi=10.1097/PAP.0b013e31817bf57d |url=}}</ref><ref name="pmid18063061">{{cite journal |vauthors=Blansfield JA, Choyke L, Morita SY, Choyke PL, Pingpank JF, Alexander HR, Seidel G, Shutack Y, Yuldasheva N, Eugeni M, Bartlett DL, Glenn GM, Middelton L, Linehan WM, Libutti SK |title=Clinical, genetic and radiographic analysis of 108 patients with von Hippel-Lindau disease (VHL) manifested by pancreatic neuroendocrine neoplasms (PNETs) |journal=Surgery |volume=142 |issue=6 |pages=814–8; discussion 818.e1–2 |year=2007 |pmid=18063061 |doi=10.1016/j.surg.2007.09.012 |url=}}</ref><ref name="pmid16680581">{{cite journal |vauthors=Kouvaraki MA, Shapiro SE, Cote GJ, Lee JE, Yao JC, Waguespack SG, Gagel RF, Evans DB, Perrier ND |title=Management of pancreatic endocrine tumors in multiple endocrine neoplasia type 1 |journal=World J Surg |volume=30 |issue=5 |pages=643–53 |year=2006 |pmid=16680581 |doi=10.1007/s00268-006-0360-y |url=}}</ref> | |||
*The pathogenesis of pancreatic cancer involves the activation or inactivation of multiple gene subsets.<ref name="pmid12946833">{{cite journal |vauthors=Cowgill SM, Muscarella P |title=The genetics of pancreatic cancer |journal=Am. J. Surg. |volume=186 |issue=3 |pages=279–86 |year=2003 |pmid=12946833 |doi= |url=}}</ref> | *The progression and development of [[pancreatic cancer]] is influenced by complex interactions and crosstalk between several cellular signaling pathways: <ref name="pmid16549325">{{cite journal |vauthors=Maitra A, Kern SE, Hruban RH |title=Molecular pathogenesis of pancreatic cancer |journal=Best Pract Res Clin Gastroenterol |volume=20 |issue=2 |pages=211–26 |year=2006 |pmid=16549325 |doi=10.1016/j.bpg.2005.10.002 |url=}}</ref><ref name="pmid16258363">{{cite journal |vauthors=Mimeault M, Brand RE, Sasson AA, Batra SK |title=Recent advances on the molecular mechanisms involved in pancreatic cancer progression and therapies |journal=Pancreas |volume=31 |issue=4 |pages=301–16 |year=2005 |pmid=16258363 |doi= |url=}}</ref><ref name="pmid16940943">{{cite journal |vauthors=Talar-Wojnarowska R, Malecka-Panas E |title=Molecular pathogenesis of pancreatic adenocarcinoma: potential clinical implications |journal=Med. Sci. Monit. |volume=12 |issue=9 |pages=RA186–93 |year=2006 |pmid=16940943 |doi= |url=}}</ref><ref name="pmid1663781">{{cite journal |vauthors=Neuman WL, Wasylyshyn ML, Jacoby R, Erroi F, Angriman I, Montag A, Brasitus T, Michelassi F, Westbrook CA |title=Evidence for a common molecular pathogenesis in colorectal, gastric, and pancreatic cancer |journal=Genes Chromosomes Cancer |volume=3 |issue=6 |pages=468–73 |year=1991 |pmid=1663781 |doi= |url=}}</ref><ref name="pmid22116519">{{cite journal |vauthors=Matthaios D, Zarogoulidis P, Balgouranidou I, Chatzaki E, Kakolyris S |title=Molecular pathogenesis of pancreatic cancer and clinical perspectives |journal=Oncology |volume=81 |issue=3-4 |pages=259–72 |year=2011 |pmid=22116519 |doi=10.1159/000334449 |url=}}</ref><ref name="pmid12520639">{{cite journal |vauthors=Konner J, O'Reilly E |title=Pancreatic cancer: epidemiology, genetics, and approaches to screening |journal=Oncology (Williston Park, N.Y.) |volume=16 |issue=12 |pages=1615–22, 1631–2; discussion 1632–3, 1637–8 |year=2002 |pmid=12520639 |doi= |url=}}</ref><ref name="pmid12063826">{{cite journal |vauthors=Hilgers W, Rosty C, Hahn SA |title=Molecular pathogenesis of pancreatic cancer |journal=Hematol. Oncol. Clin. North Am. |volume=16 |issue=1 |pages=17–35, v |year=2002 |pmid=12063826 |doi= |url=}}</ref><ref name="pmid11561601">{{cite journal |vauthors=Hruban RH, Iacobuzio-Donahue C, Wilentz RE, Goggins M, Kern SE |title=Molecular pathology of pancreatic cancer |journal=Cancer J |volume=7 |issue=4 |pages=251–8 |year=2001 |pmid=11561601 |doi= |url=}}</ref><ref name="pmid16549325">{{cite journal |vauthors=Maitra A, Kern SE, Hruban RH |title=Molecular pathogenesis of pancreatic cancer |journal=Best Pract Res Clin Gastroenterol |volume=20 |issue=2 |pages=211–26 |year=2006 |pmid=16549325 |doi=10.1016/j.bpg.2005.10.002 |url=}}</ref><ref name="pmid23073476">{{cite journal |vauthors=Singh S, Chitkara D, Kumar V, Behrman SW, Mahato RI |title=miRNA profiling in pancreatic cancer and restoration of chemosensitivity |journal=Cancer Lett. |volume=334 |issue=2 |pages=211–20 |year=2013 |pmid=23073476 |doi=10.1016/j.canlet.2012.10.008 |url=}}</ref><ref name="pmid15940643">{{cite journal |vauthors=Yan L, McFaul C, Howes N, Leslie J, Lancaster G, Wong T, Threadgold J, Evans J, Gilmore I, Smart H, Lombard M, Neoptolemos J, Greenhalf W |title=Molecular analysis to detect pancreatic ductal adenocarcinoma in high-risk groups |journal=Gastroenterology |volume=128 |issue=7 |pages=2124–30 |year=2005 |pmid=15940643 |doi= |url=}}</ref><ref name="pmid18772397">{{cite journal |vauthors=Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Kamiyama H, Jimeno A, Hong SM, Fu B, Lin MT, Calhoun ES, Kamiyama M, Walter K, Nikolskaya T, Nikolsky Y, Hartigan J, Smith DR, Hidalgo M, Leach SD, Klein AP, Jaffee EM, Goggins M, Maitra A, Iacobuzio-Donahue C, Eshleman JR, Kern SE, Hruban RH, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW |title=Core signaling pathways in human pancreatic cancers revealed by global genomic analyses |journal=Science |volume=321 |issue=5897 |pages=1801–6 |year=2008 |pmid=18772397 |pmc=2848990 |doi=10.1126/science.1164368 |url=}}</ref> | ||
*The progression and development of pancreatic cancer is influenced by complex interactions and crosstalk between several cellular signaling pathways: <ref name="pmid16549325">{{cite journal |vauthors=Maitra A, Kern SE, Hruban RH |title=Molecular pathogenesis of pancreatic cancer |journal=Best Pract Res Clin Gastroenterol |volume=20 |issue=2 |pages=211–26 |year=2006 |pmid=16549325 |doi=10.1016/j.bpg.2005.10.002 |url=}}</ref><ref name="pmid16258363">{{cite journal |vauthors=Mimeault M, Brand RE, Sasson AA, Batra SK |title=Recent advances on the molecular mechanisms involved in pancreatic cancer progression and therapies |journal=Pancreas |volume=31 |issue=4 |pages=301–16 |year=2005 |pmid=16258363 |doi= |url=}}</ref><ref name="pmid16940943">{{cite journal |vauthors=Talar-Wojnarowska R, Malecka-Panas E |title=Molecular pathogenesis of pancreatic adenocarcinoma: potential clinical implications |journal=Med. Sci. Monit. |volume=12 |issue=9 |pages=RA186–93 |year=2006 |pmid=16940943 |doi= |url=}}</ref> | **Inactivation of [[Tumor suppressor gene|tumor suppressor genes]] | ||
**Inactivation of tumor suppressor genes | **Activation of [[Oncogene|oncogenes]] | ||
**Activation of oncogenes | **Deregulation of molecules in various [[Signal transduction|signaling pathways]] | ||
**Deregulation of molecules in various signaling pathways | ***[[EGFR]] | ||
***EGFR | ***[[AKT|Akt]] | ||
***Akt | ***[[NF-kB]] | ||
***NF-kB | ***[[Hedgehog signaling pathway|Hedgehog pathways]] | ||
***Hedgehog pathways | |||
'''Inactivation of tumor suppressor genes:''' | '''Inactivation of tumor suppressor genes:''' | ||
* Tumor suppressor genes may be inactivated by: | * [[Tumor suppressor gene|Tumor suppressor genes]] may be inactivated by: | ||
** | **[[Mutation]] | ||
** Hypermethylation | **[[Methylation|Hypermethylation]] | ||
** | **[[Deletion (genetics)|Deletion]] | ||
* '''p53''' | <br /> | ||
** Deletion or mutation of p53 causes its inactivation in at least half of the pancreatic cancers. p53 is a tumor suppressor gene that is involved in cell cycle control and induction of apoptosis. | *'''p53'''<ref name="pmid9646028">{{cite journal |vauthors=Li Y, Bhuiyan M, Vaitkevicius VK, Sarkar FH |title=Molecular analysis of the p53 gene in pancreatic adenocarcinoma |journal=Diagn. Mol. Pathol. |volume=7 |issue=1 |pages=4–9 |year=1998 |pmid=9646028 |doi= |url=}}</ref> | ||
** p53 stimulates the production of p21WAF1, which inhibits the complex of cyclin D1 and CDK2, causing cell cycle arrest at the G1 phase and inhibition of cell growth. | ** Deletion or [[mutation]] of [[P53 (protein)|p53]] causes its inactivation in at least half of the [[Pancreatic cancer|pancreatic cancers]]. [[P53 (protein)|p53]] is a [[tumor suppressor gene]] that is involved in [[cell cycle]] control and induction of [[apoptosis]]. | ||
** p53 inactivation causes uncontrolled cell growth and proliferation. | ** [[P53 (protein)|p53]] stimulates the production of p21WAF1, which inhibits the complex of [[cyclin D1]] and [[Cyclin-dependent kinase 2|CDK2]], causing cell cycle arrest at the [[G1 phase]] and inhibition of [[cell growth]]. | ||
** The established association of Kras mutations with p53 inactivation is suggestive of crosstalk between different | ** [[P53 (protein)|p53]] inactivation causes uncontrolled [[cell growth]] and proliferation. | ||
** Loss of p53 can also determine a patient’s response to chemotherapy as its inactivation can increase resistance to certain agents of chemotherapy. | ** The established association of [[KRAS|Kras mutations]] with [[P53 (protein)|p53]] inactivation is suggestive of crosstalk between different [[Cell signaling|signaling pathways]] involved in [[Pancreas|pancreatic]] [[carcinogenesis]]. | ||
** Loss of [[P53 (protein)|p53]] can also determine a patient’s response to [[chemotherapy]] as its inactivation can increase resistance to certain agents of [[chemotherapy]]. | |||
<br /> | |||
* '''p16''' <ref name="pmid12946833">{{cite journal |vauthors=Cowgill SM, Muscarella P |title=The genetics of pancreatic cancer |journal=Am. J. Surg. |volume=186 |issue=3 |pages=279–86 |year=2003 |pmid=12946833 |doi= |url=}}</ref><ref name="pmid16146690">{{cite journal |vauthors=Garcea G, Neal CP, Pattenden CJ, Steward WP, Berry DP |title=Molecular prognostic markers in pancreatic cancer: a systematic review |journal=Eur. J. Cancer |volume=41 |issue=15 |pages=2213–36 |year=2005 |pmid=16146690 |doi=10.1016/j.ejca.2005.04.044 |url=}}</ref><ref name="pmid9242437">{{cite journal |vauthors=Schutte M, Hruban RH, Geradts J, Maynard R, Hilgers W, Rabindran SK, Moskaluk CA, Hahn SA, Schwarte-Waldhoff I, Schmiegel W, Baylin SB, Kern SE, Herman JG |title=Abrogation of the Rb/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas |journal=Cancer Res. |volume=57 |issue=15 |pages=3126–30 |year=1997 |pmid=9242437 |doi= |url=}}</ref><ref name="pmid10436774">{{cite journal |vauthors=Goggins M, Kern SE, Offerhaus JA, Hruban RH |title=Progress in cancer genetics: lessons from pancreatic cancer |journal=Ann. Oncol. |volume=10 Suppl 4 |issue= |pages=4–8 |year=1999 |pmid=10436774 |doi= |url=}}</ref><ref name="pmid11561603">{{cite journal |vauthors=Klein AP, Hruban RH, Brune KA, Petersen GM, Goggins M |title=Familial pancreatic cancer |journal=Cancer J |volume=7 |issue=4 |pages=266–73 |year=2001 |pmid=11561603 |doi= |url=}}</ref><ref name="pmid9820739">{{cite journal |vauthors=Mangray S, King TC |title=Molecular pathobiology of pancreatic adenocarcinoma |journal=Front. Biosci. |volume=3 |issue= |pages=D1148–60 |year=1998 |pmid=9820739 |doi= |url=}}</ref><ref name="pmid12903437">{{cite journal |vauthors=Wang C, Lu X |title=[Alterations of the p16 gene for the carcinogenesis in pancreas] |language=Chinese |journal=Zhongguo Yi Xue Ke Xue Yuan Xue Bao |volume=22 |issue=5 |pages=491–3 |year=2000 |pmid=12903437 |doi= |url=}}</ref><ref name="pmid11075991">{{cite journal |vauthors=Gerdes B, Bartsch DK, Ramaswamy A, Kersting M, Wild A, Schuermann M, Frey M, Rothmund M |title=Multiple primary tumors as an indicator for p16INK4a germline mutations in pancreatic cancer patients? |journal=Pancreas |volume=21 |issue=4 |pages=369–75 |year=2000 |pmid=11075991 |doi= |url=}}</ref> | |||
** '''p16''' participates in the aggressiveness of [[pancreatic cancer]] by inhibiting [[cyclin D]] and [[Cyclin-dependent kinase 4|CDK4/6]] mediated [[phosphorylation]] of [[Rb]] in the [[G1/S transition]] of the [[cell cycle]]. | |||
** [[Phosphorylation]] of [[Rb]] activates [[Gene|genes]] in the [[cell cycle]] required for [[DNA synthesis]] and lack of [[phosphorylation]] inhibits [[cell growth]]. | |||
** 95% of the patients with [[pancreatic cancer]] have inactivated [[P16 (gene)|p16]] with: | |||
*** 40% [[Deletion (genetics)|deletion]] | |||
*** 15% [[Methylation|hypermethylation]] | |||
* '''p27CIP1 | *** 40% [[mutation]] | ||
** '''p27CIP1''' mutations have been implicated in pancreatic cancer by altering cellular progression in the G1 to S phase. | ** [[P16 (gene)|P16]] [[mutation]] causes increased [[Rb]] [[phosphorylation]], leading to uncontrolled cellular [[Cell growth|proliferation]] and increased [[carcinogenesis]]. Survival time is lesser and [[tumor]] is larger in size in patients with [[P16 (gene)|p16]] mutation. | ||
* '''DPC4 | <br /> | ||
** DPC4 has been found to be deleted in approximately half of all pancreatic cancers. | * '''p27CIP1''' | ||
** The inactivation of DPC4 causes impaired function of a gene that plays an important role in the inhibition of cell growth and angiogenesis. | ** '''p27CIP1''' [[Mutation|mutations]] have been implicated in [[pancreatic cancer]] by altering cellular progression in the [[G1]] to [[S phase]]. | ||
** DPC4 inactivation causes increased angiogenesis and proliferation of cancer cells, with increase in the incidence of poorly differentiated tumors, thereby worsening prognosis in patients. | <br /> | ||
* '''BRCA2 | * '''DPC4''' | ||
** | ** DPC4 has been found to be deleted in approximately half of all [[Pancreatic cancer|pancreatic cancers]]. | ||
** The inactivation of DPC4 causes impaired function of a [[gene]] that plays an important role in the inhibition of [[cell growth]] and [[angiogenesis]]. | |||
** DPC4 inactivation causes increased [[angiogenesis]] and proliferation of [[Cancer|cancer cells]], with increase in the [[incidence]] of poorly differentiated [[Tumor|tumors]], thereby worsening [[prognosis]] in patients. | |||
<br /> | |||
* '''BRCA2'''<ref name="pmid11561603" /><ref name="pmid8968085">{{cite journal |vauthors=Goggins M, Schutte M, Lu J, Moskaluk CA, Weinstein CL, Petersen GM, Yeo CJ, Jackson CE, Lynch HT, Hruban RH, Kern SE |title=Germline BRCA2 gene mutations in patients with apparently sporadic pancreatic carcinomas |journal=Cancer Res. |volume=56 |issue=23 |pages=5360–4 |year=1996 |pmid=8968085 |doi= |url=}}</ref><ref name="pmid12569143">{{cite journal |vauthors=Hahn SA, Greenhalf B, Ellis I, Sina-Frey M, Rieder H, Korte B, Gerdes B, Kress R, Ziegler A, Raeburn JA, Campra D, Grützmann R, Rehder H, Rothmund M, Schmiegel W, Neoptolemos JP, Bartsch DK |title=BRCA2 germline mutations in familial pancreatic carcinoma |journal=J. Natl. Cancer Inst. |volume=95 |issue=3 |pages=214–21 |year=2003 |pmid=12569143 |doi= |url=}}</ref><ref name="pmid12097290">{{cite journal |vauthors=Murphy KM, Brune KA, Griffin C, Sollenberger JE, Petersen GM, Bansal R, Hruban RH, Kern SE |title=Evaluation of candidate genes MAP2K4, MADH4, ACVR1B, and BRCA2 in familial pancreatic cancer: deleterious BRCA2 mutations in 17% |journal=Cancer Res. |volume=62 |issue=13 |pages=3789–93 |year=2002 |pmid=12097290 |doi= |url=}}</ref><ref name="pmid9443984">{{cite journal |vauthors=Hruban RH, Petersen GM, Ha PK, Kern SE |title=Genetics of pancreatic cancer. From genes to families |journal=Surg. Oncol. Clin. N. Am. |volume=7 |issue=1 |pages=1–23 |year=1998 |pmid=9443984 |doi= |url=}}</ref> | |||
** [[BRCA2]], a [[gene]] that participates in [[DNA repair|DNA damage repair]] has also been implicated in the [[pathogenesis]] of [[pancreatic cancer]] by altering the [[G1/S transition|G1 to S cell cycle transition.]] | |||
'''Activation of oncogenes:''' | '''Activation of oncogenes:''' | ||
* Oncogenes may be activated by: | * [[Oncogenes]] may be activated by: | ||
** Amplification | ** [[Amplification]] | ||
** Point mutation | ** [[Point mutation]] | ||
* '''Ras oncogene''' | * '''Ras oncogene'''<ref name="pmid17804724">{{cite journal |vauthors=Kojima K, Vickers SM, Adsay NV, Jhala NC, Kim HG, Schoeb TR, Grizzle WE, Klug CA |title=Inactivation of Smad4 accelerates Kras(G12D)-mediated pancreatic neoplasia |journal=Cancer Res. |volume=67 |issue=17 |pages=8121–30 |year=2007 |pmid=17804724 |doi=10.1158/0008-5472.CAN-06-4167 |url=}}</ref><ref name="pmid2453289">{{cite journal |vauthors=Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M |title=Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes |journal=Cell |volume=53 |issue=4 |pages=549–54 |year=1988 |pmid=2453289 |doi= |url=}}</ref><ref name="pmid12082617">{{cite journal |vauthors=Laghi L, Orbetegli O, Bianchi P, Zerbi A, Di Carlo V, Boland CR, Malesci A |title=Common occurrence of multiple K-RAS mutations in pancreatic cancers with associated precursor lesions and in biliary cancers |journal=Oncogene |volume=21 |issue=27 |pages=4301–6 |year=2002 |pmid=12082617 |doi=10.1038/sj.onc.1205533 |url=}}</ref><ref name="pmid27371108">{{cite journal |vauthors=Cheng RF, Wang J, Zhang JY, Sun L, Zhao YR, Qiu ZQ, Sun BC, Sun Y |title=MicroRNA-506 is up-regulated in the development of pancreatic ductal adenocarcinoma and is associated with attenuated disease progression |journal=Chin J Cancer |volume=35 |issue=1 |pages=64 |year=2016 |pmid=27371108 |pmc=4930606 |doi=10.1186/s40880-016-0128-9 |url=}}</ref><ref name="pmid12094699">{{cite journal |vauthors=Hayashi N, Egami H, Ogawa M |title=[Genetics of pancreatic cancer: recent advances in molecular diagnosis] |language=Japanese |journal=Nihon Geka Gakkai Zasshi |volume=103 |issue=6 |pages=476–81 |year=2002 |pmid=12094699 |doi= |url=}}</ref><ref name="pmid9364657">{{cite journal |vauthors=Howe JR, Conlon KC |title=The molecular genetics of pancreatic cancer |journal=Surg Oncol |volume=6 |issue=1 |pages=1–18 |year=1997 |pmid=9364657 |doi= |url=}}</ref> | ||
** [[Ras|Ras oncogene]] activation is found in over ninety percent of [[Pancreatic cancer|pancreatic cancers]]. This [[oncogene]] is involved in mediating [[Cell growth|cell proliferation]], migration and [[signal transduction]]. | |||
** [[Point mutation]] or [[amplification]] of K-[[ras]] in the early phase of [[carcinogenesis]] leads to the formation of a constitutively activated [[Ras]] that binds to [[G protein|GTP]] and propagates uncontrolled [[DNA replication|cellular replication]] via downstream signaling pathways. | |||
* '''Cox-2 activation''' | <br /> | ||
*'''Cox-2 activation'''<ref name="pmid15542781">{{cite journal |vauthors=El-Rayes BF, Ali S, Sarkar FH, Philip PA |title=Cyclooxygenase-2-dependent and -independent effects of celecoxib in pancreatic cancer cell lines |journal=Mol. Cancer Ther. |volume=3 |issue=11 |pages=1421–6 |year=2004 |pmid=15542781 |doi= |url=}}</ref><ref name="pmid15455372">{{cite journal |vauthors=Hussain T, Gupta S, Adhami VM, Mukhtar H |title=Green tea constituent epigallocatechin-3-gallate selectively inhibits COX-2 without affecting COX-1 expression in human prostate carcinoma cells |journal=Int. J. Cancer |volume=113 |issue=4 |pages=660–9 |year=2005 |pmid=15455372 |doi=10.1002/ijc.20629 |url=}}</ref><ref name="pmid15026340">{{cite journal |vauthors=Wei D, Wang L, He Y, Xiong HQ, Abbruzzese JL, Xie K |title=Celecoxib inhibits vascular endothelial growth factor expression in and reduces angiogenesis and metastasis of human pancreatic cancer via suppression of Sp1 transcription factor activity |journal=Cancer Res. |volume=64 |issue=6 |pages=2030–8 |year=2004 |pmid=15026340 |doi= |url=}}</ref><ref name="pmid10473081">{{cite journal |vauthors=Okami J, Yamamoto H, Fujiwara Y, Tsujie M, Kondo M, Noura S, Oshima S, Nagano H, Dono K, Umeshita K, Ishikawa O, Sakon M, Matsuura N, Nakamori S, Monden M |title=Overexpression of cyclooxygenase-2 in carcinoma of the pancreas |journal=Clin. Cancer Res. |volume=5 |issue=8 |pages=2018–24 |year=1999 |pmid=10473081 |doi= |url=}}</ref><ref name="pmid11490843">{{cite journal |vauthors=Inoue S, Tezel E, Nakao A |title=Molecular diagnosis of pancreatic cancer |journal=Hepatogastroenterology |volume=48 |issue=40 |pages=933–8 |year=2001 |pmid=11490843 |doi= |url=}}</ref> | |||
** [[Cyclooxygenase|COX]]-2 is an inducible [[Protein isoform|isoform]] of the [[Cyclooxygenase|COX]] [[enzyme]] and its synthesis is stimulated in [[Pancreas|pancreatic]] [[Carcinogen|carcinogenic]] and [[Inflammation|inflammatory]] processes. | |||
** Activated [[Ras]] present in ninety percent of [[Pancreatic cancer|pancreatic cancers]] increases [[Cyclooxygenase|COX]]-2 [[Messenger RNA|mRNA]] stability, hence contributing to [[Pancreas|pancreatic]] [[carcinogenesis]]. | |||
<br /> | |||
* '''Akt-2 gene amplification''' | * '''Akt-2 gene amplification''' | ||
** Akt-2 gene amplification occurs in 10–15% of pancreatic cancers leading to its activation. | ** [[AKT|Akt]]-2 [[gene]] [[amplification]] occurs in 10–15% of [[Pancreatic cancer|pancreatic cancers]] leading to its activation. | ||
** Activation of Akt-2 gene stimulates cell growth, thereby accelerating progression to pancreatic cancer. | ** Activation of [[AKT|Akt]]-2 gene stimulates [[cell growth]], thereby accelerating progression to [[pancreatic cancer]]. | ||
* '''Notch gene | <br /> | ||
* '''Notch gene<ref name="pmid16510599">{{cite journal |vauthors=Wang Z, Banerjee S, Li Y, Rahman KM, Zhang Y, Sarkar FH |title=Down-regulation of notch-1 inhibits invasion by inactivation of nuclear factor-kappaB, vascular endothelial growth factor, and matrix metalloproteinase-9 in pancreatic cancer cells |journal=Cancer Res. |volume=66 |issue=5 |pages=2778–84 |year=2006 |pmid=16510599 |doi=10.1158/0008-5472.CAN-05-4281 |url=}}</ref><ref name="pmid16327489">{{cite journal |vauthors=Büchler P, Gazdhar A, Schubert M, Giese N, Reber HA, Hines OJ, Giese T, Ceyhan GO, Müller M, Büchler MW, Friess H |title=The Notch signaling pathway is related to neurovascular progression of pancreatic cancer |journal=Ann. Surg. |volume=242 |issue=6 |pages=791–800, discussion 800–1 |year=2005 |pmid=16327489 |pmc=1409885 |doi= |url=}}</ref><ref name="pmid12842085">{{cite journal |vauthors=Miyamoto Y, Maitra A, Ghosh B, Zechner U, Argani P, Iacobuzio-Donahue CA, Sriuranpong V, Iso T, Meszoely IM, Wolfe MS, Hruban RH, Ball DW, Schmid RM, Leach SD |title=Notch mediates TGF alpha-induced changes in epithelial differentiation during pancreatic tumorigenesis |journal=Cancer Cell |volume=3 |issue=6 |pages=565–76 |year=2003 |pmid=12842085 |doi= |url=}}</ref><ref name="pmid16284950">{{cite journal |vauthors=Wang Z, Zhang Y, Banerjee S, Li Y, Sarkar FH |title=Inhibition of nuclear factor kappab activity by genistein is mediated via Notch-1 signaling pathway in pancreatic cancer cells |journal=Int. J. Cancer |volume=118 |issue=8 |pages=1930–6 |year=2006 |pmid=16284950 |doi=10.1002/ijc.21589 |url=}}</ref><ref name="pmid16628653">{{cite journal |vauthors=Wang Z, Zhang Y, Banerjee S, Li Y, Sarkar FH |title=Notch-1 down-regulation by curcumin is associated with the inhibition of cell growth and the induction of apoptosis in pancreatic cancer cells |journal=Cancer |volume=106 |issue=11 |pages=2503–13 |year=2006 |pmid=16628653 |doi=10.1002/cncr.21904 |url=}}</ref><ref name="pmid16546962">{{cite journal |vauthors=Wang Z, Zhang Y, Li Y, Banerjee S, Liao J, Sarkar FH |title=Down-regulation of Notch-1 contributes to cell growth inhibition and apoptosis in pancreatic cancer cells |journal=Mol. Cancer Ther. |volume=5 |issue=3 |pages=483–93 |year=2006 |pmid=16546962 |doi=10.1158/1535-7163.MCT-05-0299 |url=}}</ref>''' | |||
** [[Notch]] protein activation causes translocation of [[Notch]] into the [[Cell nucleus|nucleus]]. The [[Notch|Notch protein]] is bound to transcriptional factors and plays a vital role in the development of organs and [[Pancreas|pancreatic]] [[carcinogenesis]] by regulating the expression of [[Target cell|target genes]]. | |||
** Notch also contributes to [[pancreatic cancer]] by inhibition of [[apoptosis]] of cells. | |||
<br /> | |||
* '''Up-regulation of cyclin D1''' | * '''Up-regulation of cyclin D1''' | ||
** Cyclin D1 overexpression promotes tumor cell growth and confers resistance to cisplatin, proving the effect of cyclin D1 on the pathogenesis of pancreatic cancer.<ref name="pmid16115953">{{cite journal |vauthors=Biliran H, Wang Y, Banerjee S, Xu H, Heng H, Thakur A, Bollig A, Sarkar FH, Liao JD |title=Overexpression of cyclin D1 promotes tumor cell growth and confers resistance to cisplatin-mediated apoptosis in an elastase-myc transgene-expressing pancreatic tumor cell line |journal=Clin. Cancer Res. |volume=11 |issue=16 |pages=6075–86 |year=2005 |pmid=16115953 |doi=10.1158/1078-0432.CCR-04-2419 |url=}}</ref><ref name="pmid9435306">{{cite journal |vauthors=Kornmann M, Arber N, Korc M |title=Inhibition of basal and mitogen-stimulated pancreatic cancer cell growth by cyclin D1 antisense is associated with loss of tumorigenicity and potentiation of cytotoxicity to cisplatinum |journal=J. Clin. Invest. |volume=101 |issue=2 |pages=344–52 |year=1998 |pmid=9435306 |pmc=508573 |doi=10.1172/JCI1323 |url=}}</ref> | ** [[Cyclin D1]] overexpression promotes [[tumor]] [[cell growth]] and confers resistance to [[cisplatin]], proving the effect of [[cyclin D1]] on the [[pathogenesis]] of [[pancreatic cancer]].<ref name="pmid16115953">{{cite journal |vauthors=Biliran H, Wang Y, Banerjee S, Xu H, Heng H, Thakur A, Bollig A, Sarkar FH, Liao JD |title=Overexpression of cyclin D1 promotes tumor cell growth and confers resistance to cisplatin-mediated apoptosis in an elastase-myc transgene-expressing pancreatic tumor cell line |journal=Clin. Cancer Res. |volume=11 |issue=16 |pages=6075–86 |year=2005 |pmid=16115953 |doi=10.1158/1078-0432.CCR-04-2419 |url=}}</ref><ref name="pmid9435306">{{cite journal |vauthors=Kornmann M, Arber N, Korc M |title=Inhibition of basal and mitogen-stimulated pancreatic cancer cell growth by cyclin D1 antisense is associated with loss of tumorigenicity and potentiation of cytotoxicity to cisplatinum |journal=J. Clin. Invest. |volume=101 |issue=2 |pages=344–52 |year=1998 |pmid=9435306 |pmc=508573 |doi=10.1172/JCI1323 |url=}}</ref> | ||
'''Deregulation of EGFR signalling''': | <br /> | ||
* Genomic alterations of EGFR include the following: | '''Deregulation of EGFR signalling''':<ref name="pmid10815919">{{cite journal |vauthors=Bruns CJ, Harbison MT, Davis DW, Portera CA, Tsan R, McConkey DJ, Evans DB, Abbruzzese JL, Hicklin DJ, Radinsky R |title=Epidermal growth factor receptor blockade with C225 plus gemcitabine results in regression of human pancreatic carcinoma growing orthotopically in nude mice by antiangiogenic mechanisms |journal=Clin. Cancer Res. |volume=6 |issue=5 |pages=1936–48 |year=2000 |pmid=10815919 |doi= |url=}}</ref> | ||
** Deletion | * Genomic alterations of [[EGFR]] include the following: | ||
** [[Deletion (genetics)|Deletion]] | |||
** Over-expression | ** Over-expression | ||
** Rearrangement | ** Rearrangement | ||
** Mutation | ** [[Mutation]] | ||
* EGFR consists of an intracellular tyrosine kinase domain and its activation causes mobilization of molecules in different cell signaling pathways by transphosphorylation of tyrosine residues. | * [[EGFR]] consists of an [[intracellular]] [[tyrosine kinase]] domain and its activation causes mobilization of molecules in different [[Cell signaling|cell signaling pathways]] by transphosphorylation of [[tyrosine]] residues. | ||
* Alterations of EGFR stimulate receptor tyrosine kinases and promote the development and progression of pancreatic cancer by influencing:<ref name="pmid16909423">{{cite journal |vauthors=Marshall J |title=Clinical implications of the mechanism of epidermal growth factor receptor inhibitors |journal=Cancer |volume=107 |issue=6 |pages=1207–18 |year=2006 |pmid=16909423 |doi=10.1002/cncr.22133 |url=}}</ref><ref name="pmid16885366">{{cite journal |vauthors=Wang Z, Sengupta R, Banerjee S, Li Y, Zhang Y, Rahman KM, Aboukameel A, Mohammad R, Majumdar AP, Abbruzzese JL, Sarkar FH |title=Epidermal growth factor receptor-related protein inhibits cell growth and invasion in pancreatic cancer |journal=Cancer Res. |volume=66 |issue=15 |pages=7653–60 |year=2006 |pmid=16885366 |doi=10.1158/0008-5472.CAN-06-1019 |url=}}</ref><ref name="pmid16424038">{{cite journal |vauthors=Zhang Y, Banerjee S, Wang Z, Xu H, Zhang L, Mohammad R, Aboukameel A, Adsay NV, Che M, Abbruzzese JL, Majumdar AP, Sarkar FH |title=Antitumor activity of epidermal growth factor receptor-related protein is mediated by inactivation of ErbB receptors and nuclear factor-kappaB in pancreatic cancer |journal=Cancer Res. |volume=66 |issue=2 |pages=1025–32 |year=2006 |pmid=16424038 |doi=10.1158/0008-5472.CAN-05-2968 |url=}}</ref><ref name="pmid15867387">{{cite journal |vauthors=Zhang Y, Banerjee S, Wang ZW, Marciniak DJ, Majumdar AP, Sarkar FH |title=Epidermal growth factor receptor-related protein inhibits cell growth and induces apoptosis of BxPC3 pancreatic cancer cells |journal=Cancer Res. |volume=65 |issue=9 |pages=3877–82 |year=2005 |pmid=15867387 |doi=10.1158/0008-5472.CAN-04-3654 |url=}}</ref> | * Alterations of [[EGFR]] stimulate receptor [[Tyrosine kinase|tyrosine kinases]] and promote the development and progression of [[pancreatic cancer]] by influencing:<ref name="pmid16909423">{{cite journal |vauthors=Marshall J |title=Clinical implications of the mechanism of epidermal growth factor receptor inhibitors |journal=Cancer |volume=107 |issue=6 |pages=1207–18 |year=2006 |pmid=16909423 |doi=10.1002/cncr.22133 |url=}}</ref><ref name="pmid16885366">{{cite journal |vauthors=Wang Z, Sengupta R, Banerjee S, Li Y, Zhang Y, Rahman KM, Aboukameel A, Mohammad R, Majumdar AP, Abbruzzese JL, Sarkar FH |title=Epidermal growth factor receptor-related protein inhibits cell growth and invasion in pancreatic cancer |journal=Cancer Res. |volume=66 |issue=15 |pages=7653–60 |year=2006 |pmid=16885366 |doi=10.1158/0008-5472.CAN-06-1019 |url=}}</ref><ref name="pmid16424038">{{cite journal |vauthors=Zhang Y, Banerjee S, Wang Z, Xu H, Zhang L, Mohammad R, Aboukameel A, Adsay NV, Che M, Abbruzzese JL, Majumdar AP, Sarkar FH |title=Antitumor activity of epidermal growth factor receptor-related protein is mediated by inactivation of ErbB receptors and nuclear factor-kappaB in pancreatic cancer |journal=Cancer Res. |volume=66 |issue=2 |pages=1025–32 |year=2006 |pmid=16424038 |doi=10.1158/0008-5472.CAN-05-2968 |url=}}</ref><ref name="pmid15867387">{{cite journal |vauthors=Zhang Y, Banerjee S, Wang ZW, Marciniak DJ, Majumdar AP, Sarkar FH |title=Epidermal growth factor receptor-related protein inhibits cell growth and induces apoptosis of BxPC3 pancreatic cancer cells |journal=Cancer Res. |volume=65 |issue=9 |pages=3877–82 |year=2005 |pmid=15867387 |doi=10.1158/0008-5472.CAN-04-3654 |url=}}</ref> | ||
** Cell cycle progression and division | ** [[Cell cycle]] progression and [[Division (biology)|division]] | ||
** Apoptosis | ** [[Apoptosis]] | ||
** Angiogenesis | ** [[Angiogenesis]] | ||
** Motility | ** [[Motility]] | ||
** Invasion | ** [[Invasive (medical)|Invasion]] | ||
** Resistance to chemotherapy | ** Resistance to [[chemotherapy]] | ||
** Metastasis<ref name=" | ** [[Metastasis]] | ||
<br /> | |||
* Under normal conditions, NF-κB is sequestered in the cytoplasm under tight association with its inhibitors: p100 proteins and IκB. | '''Deregulation of NF-κB signalling:''' <ref name="pmid10467400">{{cite journal |vauthors=Wang W, Abbruzzese JL, Evans DB, Chiao PJ |title=Overexpression of urokinase-type plasminogen activator in pancreatic adenocarcinoma is regulated by constitutively activated RelA |journal=Oncogene |volume=18 |issue=32 |pages=4554–63 |year=1999 |pmid=10467400 |doi=10.1038/sj.onc.1202833 |url=}}</ref><ref name="pmid15590651">{{cite journal |vauthors=Bava SV, Puliappadamba VT, Deepti A, Nair A, Karunagaran D, Anto RJ |title=Sensitization of taxol-induced apoptosis by curcumin involves down-regulation of nuclear factor-kappaB and the serine/threonine kinase Akt and is independent of tubulin polymerization |journal=J. Biol. Chem. |volume=280 |issue=8 |pages=6301–8 |year=2005 |pmid=15590651 |doi=10.1074/jbc.M410647200 |url=}}</ref><ref name="pmid15051014">{{cite journal |vauthors=Fahy BN, Schlieman MG, Virudachalam S, Bold RJ |title=Inhibition of AKT abrogates chemotherapy-induced NF-kappaB survival mechanisms: implications for therapy in pancreatic cancer |journal=J. Am. Coll. Surg. |volume=198 |issue=4 |pages=591–9 |year=2004 |pmid=15051014 |doi=10.1016/j.jamcollsurg.2003.12.005 |url=}}</ref><ref name="pmid12538487">{{cite journal |vauthors=Fujioka S, Sclabas GM, Schmidt C, Frederick WA, Dong QG, Abbruzzese JL, Evans DB, Baker C, Chiao PJ |title=Function of nuclear factor kappaB in pancreatic cancer metastasis |journal=Clin. Cancer Res. |volume=9 |issue=1 |pages=346–54 |year=2003 |pmid=12538487 |doi= |url=}}</ref><ref name="pmid16724054">{{cite journal |vauthors=Karin M |title=Nuclear factor-kappaB in cancer development and progression |journal=Nature |volume=441 |issue=7092 |pages=431–6 |year=2006 |pmid=16724054 |doi=10.1038/nature04870 |url=}}</ref><ref name="pmid15476283">{{cite journal |vauthors=Li L, Aggarwal BB, Shishodia S, Abbruzzese J, Kurzrock R |title=Nuclear factor-kappaB and IkappaB kinase are constitutively active in human pancreatic cells, and their down-regulation by curcumin (diferuloylmethane) is associated with the suppression of proliferation and the induction of apoptosis |journal=Cancer |volume=101 |issue=10 |pages=2351–62 |year=2004 |pmid=15476283 |doi=10.1002/cncr.20605 |url=}}</ref><ref name="pmid16061678">{{cite journal |vauthors=Li Y, Ahmed F, Ali S, Philip PA, Kucuk O, Sarkar FH |title=Inactivation of nuclear factor kappaB by soy isoflavone genistein contributes to increased apoptosis induced by chemotherapeutic agents in human cancer cells |journal=Cancer Res. |volume=65 |issue=15 |pages=6934–42 |year=2005 |pmid=16061678 |doi=10.1158/0008-5472.CAN-04-4604 |url=}}</ref><ref name="pmid15574364">{{cite journal |vauthors=Li Y, Chinni SR, Sarkar FH |title=Selective growth regulatory and pro-apoptotic effects of DIM is mediated by AKT and NF-kappaB pathways in prostate cancer cells |journal=Front. Biosci. |volume=10 |issue= |pages=236–43 |year=2005 |pmid=15574364 |doi= |url=}}</ref> | ||
* NF-κB is activated by phosphorylation of IκB and p100, resulting in the translocation of active NF-κB into the nucleus, thereby up-regulating gene transcription. | * Under normal conditions, [[NF-κB]] is sequestered in the cytoplasm under tight association with its inhibitors: p100 proteins and IκB. | ||
* The constitutive activation of NF-κB in pancreatic cancer causes increased expression of many genes eg. uPA , survivin, VEGF, MMP-9, involved in: <ref name="pmid12767057">{{cite journal |vauthors=Liptay S, Weber CK, Ludwig L, Wagner M, Adler G, Schmid RM |title=Mitogenic and antiapoptotic role of constitutive NF-kappaB/Rel activity in pancreatic cancer |journal=Int. J. Cancer |volume=105 |issue=6 |pages=735–46 |year=2003 |pmid=12767057 |doi=10.1002/ijc.11081 |url=}}</ref><ref name="pmid15665315">{{cite journal |vauthors=Rahman KW, Sarkar FH |title=Inhibition of nuclear translocation of nuclear factor-{kappa}B contributes to 3,3'-diindolylmethane-induced apoptosis in breast cancer cells |journal=Cancer Res. |volume=65 |issue=1 |pages=364–71 |year=2005 |pmid=15665315 |doi= |url=}}</ref><ref name="pmid12687011">{{cite journal |vauthors=Zhang H, Morisaki T, Nakahara C, Matsunaga H, Sato N, Nagumo F, Tadano J, Katano M |title=PSK-mediated NF-kappaB inhibition augments docetaxel-induced apoptosis in human pancreatic cancer cells NOR-P1 |journal=Oncogene |volume=22 |issue=14 |pages=2088–96 |year=2003 |pmid=12687011 |doi=10.1038/sj.onc.1206310 |url=}}</ref> | * [[NF-κB]] is activated by [[phosphorylation]] of IκB and p100, resulting in the translocation of active [[NF-κB]] into the [[Cell nucleus|nucleus]], thereby up-regulating [[Transcription (genetics)|gene transcription]]. | ||
** Apoptosis | * The constitutive activation of [[NF-κB]] in [[pancreatic cancer]] causes increased expression of many [[Gene|genes]] eg. uPA , survivin, [[Vascular endothelial growth factor|VEGF]], [[Matrix metalloproteinase|MMP]]-9, involved in: <ref name="pmid12767057">{{cite journal |vauthors=Liptay S, Weber CK, Ludwig L, Wagner M, Adler G, Schmid RM |title=Mitogenic and antiapoptotic role of constitutive NF-kappaB/Rel activity in pancreatic cancer |journal=Int. J. Cancer |volume=105 |issue=6 |pages=735–46 |year=2003 |pmid=12767057 |doi=10.1002/ijc.11081 |url=}}</ref><ref name="pmid15665315"><nowiki>{{cite journal |vauthors=Rahman KW, Sarkar FH |title=Inhibition of nuclear translocation of nuclear factor-{kappa}B contributes to 3,3'-diindolylmethane-induced apoptosis in breast cancer cells |journal=Cancer Res. |volume=65 |issue=1 |pages=364–71 |year=2005 |pmid=15665315 |doi= |url=}}</nowiki></ref><ref name="pmid12687011">{{cite journal |vauthors=Zhang H, Morisaki T, Nakahara C, Matsunaga H, Sato N, Nagumo F, Tadano J, Katano M |title=PSK-mediated NF-kappaB inhibition augments docetaxel-induced apoptosis in human pancreatic cancer cells NOR-P1 |journal=Oncogene |volume=22 |issue=14 |pages=2088–96 |year=2003 |pmid=12687011 |doi=10.1038/sj.onc.1206310 |url=}}</ref> | ||
** Cell growth | ** [[Apoptosis]] | ||
** Inflammation | ** [[Cell growth]] | ||
** [[Inflammation]] | |||
** Stress response | ** Stress response | ||
** Cell differentiation | ** [[Cellular differentiation|Cell differentiation]] | ||
** Angiogenesis | ** [[Angiogenesis]] | ||
** Invasion | ** [[Invasive (medical)|Invasion]] | ||
** Cell survival | ** [[Cell (biology)|Cell]] survival | ||
** Metastasis | ** [[Metastasis]] | ||
** | ** [[Pancreatic cancer|Pancreatic cance]]<nowiki/>r cells display over expression of [[urokinase]]-type [[plasminogen]] activator (uPA), directly involved in the regulation of [[angiogenesis]], [[tumor]] invasion and [[metastasis]]. | ||
<br /> | |||
'''Deregulation of Akt signaling''': | '''Deregulation of Akt signaling''': | ||
* Deregulation of Akt signaling is found in about seventy percent of the cases of pancreatic cancer and is associated with high tumor grade and prognosis. | * Deregulation of [[AKT|Akt]] signaling is found in about seventy percent of the cases of [[pancreatic cancer]] and is associated with high [[tumor]] grade and [[prognosis]]. | ||
* EGF binding leads to PI3K pathway activation. | * EGF binding leads to [[Phosphoinositide 3-kinase|PI3K]] pathway activation. | ||
* Activated PI3K phosphorylates phosphatidylinositides (PIP3) and this, in turn causes phosphorylation and activation of Akt. | * Activated [[Phosphoinositide 3-kinase|PI3K]] phosphorylates phosphatidylinositides ([[Phosphatidylinositol (3,4,5)-trisphosphate|PIP3]]) and this, in turn causes [[phosphorylation]] and activation of [[AKT|Akt]]. | ||
* | * [[Phosphorylation]] of [[AKT|Akt]] (p-Akt) activates [[NF-κB]] and inhibits [[apoptosis]], thereby promoting cell survival. | ||
* Akt also regulates the NF-κB pathway via phosphorylation and activation, causing upregulation of gene transcription. | * [[AKT|Akt]] also regulates the [[NF-κB]] pathway via [[phosphorylation]] and activation, causing [[upregulation]] of [[Transcription (genetics)|gene transcription]]. | ||
'''Deregulation of Hedgehog | '''Deregulation of Hedgehog signaling''':<ref name="pmid22116519" /><ref name="pmid16849549">{{cite journal |vauthors=Nakashima H, Nakamura M, Yamaguchi H, Yamanaka N, Akiyoshi T, Koga K, Yamaguchi K, Tsuneyoshi M, Tanaka M, Katano M |title=Nuclear factor-kappaB contributes to hedgehog signaling pathway activation through sonic hedgehog induction in pancreatic cancer |journal=Cancer Res. |volume=66 |issue=14 |pages=7041–9 |year=2006 |pmid=16849549 |doi=10.1158/0008-5472.CAN-05-4588 |url=}}</ref><ref name="pmid14520413">{{cite journal |vauthors=Thayer SP, di Magliano MP, Heiser PW, Nielsen CM, Roberts DJ, Lauwers GY, Qi YP, Gysin S, Fernández-del Castillo C, Yajnik V, Antoniu B, McMahon M, Warshaw AL, Hebrok M |title=Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis |journal=Nature |volume=425 |issue=6960 |pages=851–6 |year=2003 |pmid=14520413 |pmc=3688051 |doi=10.1038/nature02009 |url=}}</ref><ref name="pmid14520411">{{cite journal |vauthors=Berman DM, Karhadkar SS, Maitra A, Montes De Oca R, Gerstenblith MR, Briggs K, Parker AR, Shimada Y, Eshleman JR, Watkins DN, Beachy PA |title=Widespread requirement for Hedgehog ligand stimulation in growth of digestive tract tumours |journal=Nature |volume=425 |issue=6960 |pages=846–51 |year=2003 |pmid=14520411 |doi=10.1038/nature01972 |url=}}</ref><ref name="pmid25310976">{{cite journal |vauthors=Mathew E, Zhang Y, Holtz AM, Kane KT, Song JY, Allen BL, Pasca di Magliano M |title=Dosage-dependent regulation of pancreatic cancer growth and angiogenesis by hedgehog signaling |journal=Cell Rep |volume=9 |issue=2 |pages=484–94 |year=2014 |pmid=25310976 |pmc=4362534 |doi=10.1016/j.celrep.2014.09.010 |url=}}</ref> | ||
* In case of [[Pancreas|pancreatic]] development in the [[embryo]], [[Hedgehog signaling pathway|Hedgehog (Hh) signaling]] is an essential pathway. | |||
* [[Hedgehog signaling pathway|Hedgehog signaling]] plays an essential role in: | |||
** [[Tissue (biology)|Tissue]] [[morphogenesis]] | |||
** Organ formation of developing [[gastrointestinal tract]] | |||
* Deregulation of the [[Hedgehog signaling pathway|Hh pathway]] leading to overexpression of Shh is known to contribute to [[Pancreas|pancreatic]] [[tumorigenesis]]. | |||
* Sonic [[Hedgehog signaling pathway|hedgehog signaling]] is aberrantly expressed in seventy percent of [[pancreas]] specimens from [[carcinoma]] patients, implicating its role in [[Pancreas|pancreatic]] [[tumorigenesis]]. | |||
==Gross Pathology== | ==Gross Pathology== | ||
The [[gross pathology]] of [[Pancreatic cancer|pancreatic adenocarcinoma]], which accounts for three-fourths of all [[Pancreas|pancreatic]] [[Cancer|malignancies]] is as follows:<ref name="pmid25320520">{{cite journal |vauthors=Esposito I, Konukiewitz B, Schlitter AM, Klöppel G |title=Pathology of pancreatic ductal adenocarcinoma: facts, challenges, and future developments |journal=World J. Gastroenterol. |volume=20 |issue=38 |pages=13833–41 |year=2014 |pmid=25320520 |pmc=4194566 |doi=10.3748/wjg.v20.i38.13833 |url=}}</ref> | |||
* Grossly, ductal [[Adenocarcinoma|adenocarcinomas]] of the [[pancreas]] tend to be gritty, hard, gray-white poorly defined masses that cause obstruction of the main [[pancreatic duct]] and the distal [[common bile duct]]. | |||
* [[Chronic pancreatitis]] of the obstructed [[Pancreas|pancreatic]] segment arises due to obstruction of the main [[Pancreas|pancreatic]] [[Duct (anatomy)|duct]]. | |||
* Patients do not present with [[malabsorption]] or [[steatorrhea]] as the accessory [[duct of Santorini]] can still allow bypass of the main [[pancreatic duct]]. | |||
* The [[Head of pancreas|head of the pancreas]] is most commonly involved. | |||
* [[Head of pancreas|Head lesions]] make up 75% of all lesions, while the rest are body/tail [[Lesion|lesions]]. | |||
* [[Ductal carcinoma|Ductal]] adenocarcinomas do not always originate in the main [[Pancreas|pancreatic]] or major branch ducts and may arise in small ducts within the peripheral [[Acinus|acinar]] tissue. Hence, the term "ductal" is based on [[histology]] and not the origin. | |||
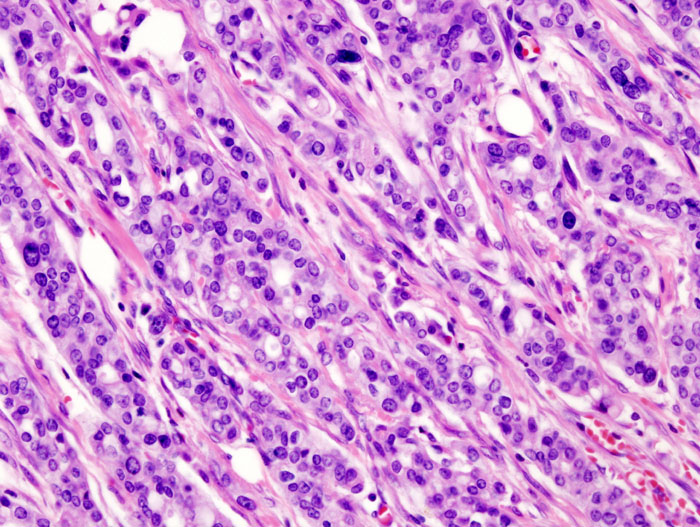
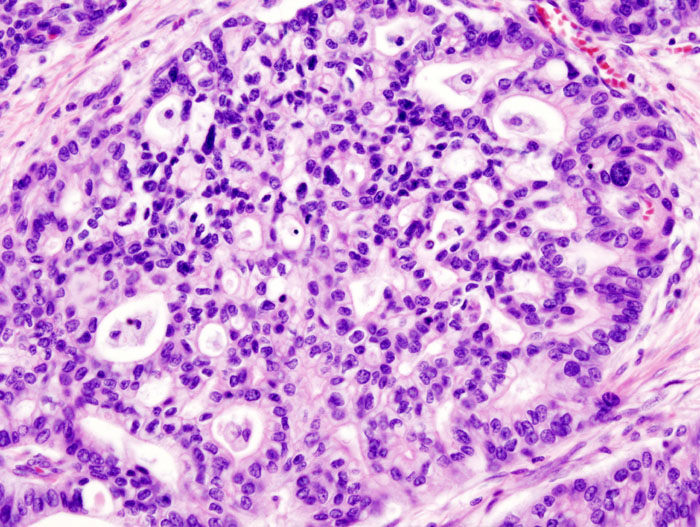
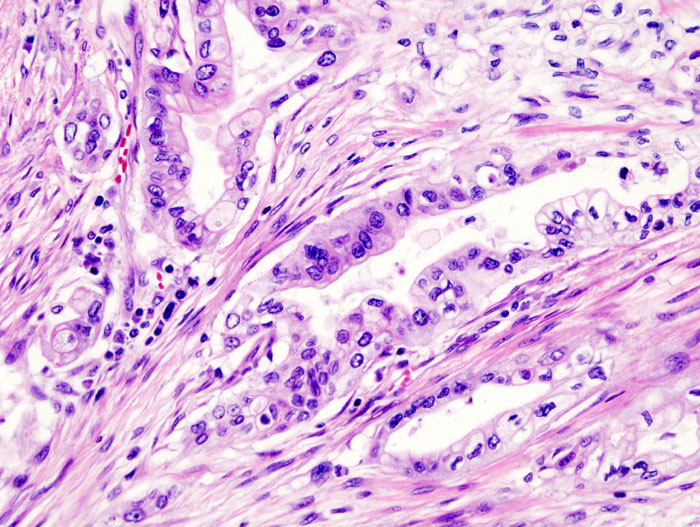
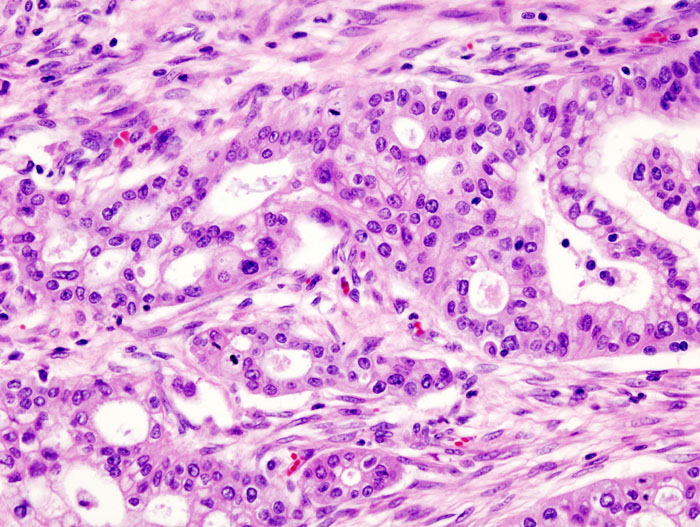
==Microscopic Pathology== | ==Microscopic Pathology== | ||
On microscopic histopathological analysis, the following features are noted:<ref name="pmid25170201">{{cite journal |vauthors=Rossi ML, Rehman AA, Gondi CS |title=Therapeutic options for the management of pancreatic cancer |journal=World J. Gastroenterol. |volume=20 |issue=32 |pages=11142–59 |year=2014 |pmid=25170201 |pmc=4145755 |doi=10.3748/wjg.v20.i32.11142 |url=}}</ref> | |||
*Majority of [[Ductal carcinoma|ductal]] [[Adenocarcinoma|adenocarcinomas]] have varying degrees of [[mucin]] production and [[Duct (anatomy)|duct]]-like structures and present as moderate-poorly differentiated masses. | |||
* The ductal [[Adenocarcinoma|adenocarcinomas]] are referred to as “[[Desmoplasia|desmoplastic]]” or "scirrhous" carcinomas due to their characteristic dense [[stromal]] fibrosis occurring due to alterations in [[TGF beta|transforming growth factor-beta]] ([[TGF beta|TGF-beta]]) signaling. | |||
*There is typically considerable [[desmoplasia]] or formation of a dense fibrous [[Stroma (animal tissue)|stroma]] or structural tissue consisting of a range of [[cell type]]s (including [[myofibroblast]]s, [[macrophage]]s, [[lymphocyte]]s and [[mast cell]]s) and deposited material (such as [[type I collagen]] and [[hyaluronic acid]]). | |||
*Local extension of [[tumor]] cells may occur into adjacent structures such as:<ref name="pmid24931343">{{cite journal |vauthors=Oda Y, Aishima S, Morimatsu K, Shindo K, Fujino M, Mizuuchi Y, Hattori M, Miyazaki T, Tanaka M, Oda Y |title=Pancreatic intraepithelial neoplasia in the background of invasive ductal carcinoma of the pancreas as a prognostic factor |journal=Histopathology |volume=65 |issue=3 |pages=389–97 |year=2014 |pmid=24931343 |doi=10.1111/his.12397 |url=}}</ref> | |||
**[[Superior mesenteric vein|Superior mesenteric vessels]] | |||
**Perineural invasion: both inside and outside the [[pancreas]] (eg, the [[retroperitoneum]]) | |||
**[[Duodenum]] | |||
**[[Portal vein]] | |||
**[[Stomach]] | |||
**[[Vertebral column]] | |||
**[[Adrenal gland|Adrenal glands]] | |||
**[[Spleen]] | |||
**[[Transverse colon]] | |||
*[[Lymph node]] spread can occur to the following sites:<ref name="pmid20981102">{{cite journal |vauthors=Yachida S, Jones S, Bozic I, Antal T, Leary R, Fu B, Kamiyama M, Hruban RH, Eshleman JR, Nowak MA, Velculescu VE, Kinzler KW, Vogelstein B, Iacobuzio-Donahue CA |title=Distant metastasis occurs late during the genetic evolution of pancreatic cancer |journal=Nature |volume=467 |issue=7319 |pages=1114–7 |year=2010 |pmid=20981102 |pmc=3148940 |doi=10.1038/nature09515 |url=}}</ref><ref name="pmid20981101">{{cite journal |vauthors=Campbell PJ, Yachida S, Mudie LJ, Stephens PJ, Pleasance ED, Stebbings LA, Morsberger LA, Latimer C, McLaren S, Lin ML, McBride DJ, Varela I, Nik-Zainal SA, Leroy C, Jia M, Menzies A, Butler AP, Teague JW, Griffin CA, Burton J, Swerdlow H, Quail MA, Stratton MR, Iacobuzio-Donahue C, Futreal PA |title=The patterns and dynamics of genomic instability in metastatic pancreatic cancer |journal=Nature |volume=467 |issue=7319 |pages=1109–13 |year=2010 |pmid=20981101 |pmc=3137369 |doi=10.1038/nature09460 |url=}}</ref> | |||
**Regional peripancreatic [[Lymph node|lymph nodes]] | |||
**[[Mesentery|Mesenteric]] | |||
**Perigastric | |||
** Portahepatic | |||
**[[Omental]] | |||
*'''Microscopic study reveals the following:''' | |||
**Mostly [[Gland|glandular]] appearance, may present as a [[solid]] occasionally. | |||
**[[Cell nucleus|Nuclei]] shows the following features: | |||
***[[Pleomorphism]] may be observed minimally. | |||
***[[Cell nucleus|Nuclei]] is often small | |||
***Coffee-bean appearance may be observed sometimes | |||
**[[Cytoplasm]] shows the following features: | |||
***[[Granule cell|Granular]] and abundant. | |||
**Quasi [[Endocrine system|endocrine]] look is observed, which may stain positive for [[Endocrine system|endocrine]] markers | |||
*Other features: | |||
**May or may not present with [[Necrosis]]. | |||
**May or may not show myxoid [[degeneration]]. | |||
**May or may not present with [[Cell (biology)|cells]] around [[Blood vessel|vessels]]. | |||
<gallery> | |||
Image:Pancreas_adenocarcinoma_-_1.jpg|thumb|350px|left|CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552900 | |||
Image:Pancreas_adenocarcinoma_-_2.jpg|thumb|350px|center|CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552901 | |||
Image:Pancreas_adenocarcinoma_-_3.jpg|thumb|350px|right|CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552904 | |||
Image:Pancreas_adenocarcinoma_-_4.jpg|thumb|350px|center|CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552903 | |||
</gallery> | |||
==References== | ==References== | ||
| Line 151: | Line 184: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category: | [[Category:Gastroenterology]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Surgery]] | |||
[[Category:Gastroenterology]] | |||
Latest revision as of 13:53, 14 March 2019
| https://https://www.youtube.com/watch?v=XFxMOiJRZQg%7C350}} |
|
Pancreatic cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pancreatic cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Pancreatic cancer pathophysiology |
|
Risk calculators and risk factors for Pancreatic cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sudarshana Datta, MD [2]
Overview
The development of pancreatic cancer is influenced by complex interactions between several cellular signaling pathways that include inactivation of tumor suppressor genes, activation of oncogenes and deregulation of molecules in various signaling pathways. Some of the important tumor suppressor genes involved are p53, p16, p27CIP1, DPC4 and BRCA2. These tumor suppressor genes are commonly inactivated by deletion, hypermethylation or mutation. The oncogenes involved in the pathogenesis of pancreatic cancer include Ras, Cox-2, Akt-2, Notch, Cyclin- D1 genes. Signal transduction pathways such as EGFR, Akt, NF-kB and Hedgehog pathways undergo genomic alterations and crosstalk between these pathways plays an important role in pancreatic tumorigenesis.
Pathophysiology
Pathogenesis and Genetics
- The pathogenesis of pancreatic cancer involves the activation or inactivation of multiple gene subsets.[1][2][3][4][5][6][7]
- The progression and development of pancreatic cancer is influenced by complex interactions and crosstalk between several cellular signaling pathways: [8][9][10][11][12][13][14][15][8][16][17][18]
- Inactivation of tumor suppressor genes
- Activation of oncogenes
- Deregulation of molecules in various signaling pathways
Inactivation of tumor suppressor genes:
- Tumor suppressor genes may be inactivated by:
- p53[19]
- Deletion or mutation of p53 causes its inactivation in at least half of the pancreatic cancers. p53 is a tumor suppressor gene that is involved in cell cycle control and induction of apoptosis.
- p53 stimulates the production of p21WAF1, which inhibits the complex of cyclin D1 and CDK2, causing cell cycle arrest at the G1 phase and inhibition of cell growth.
- p53 inactivation causes uncontrolled cell growth and proliferation.
- The established association of Kras mutations with p53 inactivation is suggestive of crosstalk between different signaling pathways involved in pancreatic carcinogenesis.
- Loss of p53 can also determine a patient’s response to chemotherapy as its inactivation can increase resistance to certain agents of chemotherapy.
- p16 [1][20][21][22][23][24][25][26]
- p16 participates in the aggressiveness of pancreatic cancer by inhibiting cyclin D and CDK4/6 mediated phosphorylation of Rb in the G1/S transition of the cell cycle.
- Phosphorylation of Rb activates genes in the cell cycle required for DNA synthesis and lack of phosphorylation inhibits cell growth.
- 95% of the patients with pancreatic cancer have inactivated p16 with:
- 40% deletion
- 15% hypermethylation
- 40% mutation
- P16 mutation causes increased Rb phosphorylation, leading to uncontrolled cellular proliferation and increased carcinogenesis. Survival time is lesser and tumor is larger in size in patients with p16 mutation.
- p27CIP1
- p27CIP1 mutations have been implicated in pancreatic cancer by altering cellular progression in the G1 to S phase.
- DPC4
- DPC4 has been found to be deleted in approximately half of all pancreatic cancers.
- The inactivation of DPC4 causes impaired function of a gene that plays an important role in the inhibition of cell growth and angiogenesis.
- DPC4 inactivation causes increased angiogenesis and proliferation of cancer cells, with increase in the incidence of poorly differentiated tumors, thereby worsening prognosis in patients.
- BRCA2[23][27][28][29][30]
- BRCA2, a gene that participates in DNA damage repair has also been implicated in the pathogenesis of pancreatic cancer by altering the G1 to S cell cycle transition.
Activation of oncogenes:
- Oncogenes may be activated by:
- Ras oncogene[31][32][33][34][35][36]
- Ras oncogene activation is found in over ninety percent of pancreatic cancers. This oncogene is involved in mediating cell proliferation, migration and signal transduction.
- Point mutation or amplification of K-ras in the early phase of carcinogenesis leads to the formation of a constitutively activated Ras that binds to GTP and propagates uncontrolled cellular replication via downstream signaling pathways.
- Cox-2 activation[37][38][39][40][41]
- COX-2 is an inducible isoform of the COX enzyme and its synthesis is stimulated in pancreatic carcinogenic and inflammatory processes.
- Activated Ras present in ninety percent of pancreatic cancers increases COX-2 mRNA stability, hence contributing to pancreatic carcinogenesis.
- Akt-2 gene amplification
- Akt-2 gene amplification occurs in 10–15% of pancreatic cancers leading to its activation.
- Activation of Akt-2 gene stimulates cell growth, thereby accelerating progression to pancreatic cancer.
- Notch gene[42][43][44][45][46][47]
- Notch protein activation causes translocation of Notch into the nucleus. The Notch protein is bound to transcriptional factors and plays a vital role in the development of organs and pancreatic carcinogenesis by regulating the expression of target genes.
- Notch also contributes to pancreatic cancer by inhibition of apoptosis of cells.
- Up-regulation of cyclin D1
- Cyclin D1 overexpression promotes tumor cell growth and confers resistance to cisplatin, proving the effect of cyclin D1 on the pathogenesis of pancreatic cancer.[48][49]
Deregulation of EGFR signalling:[50]
- Genomic alterations of EGFR include the following:
- EGFR consists of an intracellular tyrosine kinase domain and its activation causes mobilization of molecules in different cell signaling pathways by transphosphorylation of tyrosine residues.
- Alterations of EGFR stimulate receptor tyrosine kinases and promote the development and progression of pancreatic cancer by influencing:[51][52][53][54]
- Cell cycle progression and division
- Apoptosis
- Angiogenesis
- Motility
- Invasion
- Resistance to chemotherapy
- Metastasis
Deregulation of NF-κB signalling: [55][56][57][58][59][60][61][62]
- Under normal conditions, NF-κB is sequestered in the cytoplasm under tight association with its inhibitors: p100 proteins and IκB.
- NF-κB is activated by phosphorylation of IκB and p100, resulting in the translocation of active NF-κB into the nucleus, thereby up-regulating gene transcription.
- The constitutive activation of NF-κB in pancreatic cancer causes increased expression of many genes eg. uPA , survivin, VEGF, MMP-9, involved in: [63][64][65]
- Apoptosis
- Cell growth
- Inflammation
- Stress response
- Cell differentiation
- Angiogenesis
- Invasion
- Cell survival
- Metastasis
- Pancreatic cancer cells display over expression of urokinase-type plasminogen activator (uPA), directly involved in the regulation of angiogenesis, tumor invasion and metastasis.
Deregulation of Akt signaling:
- Deregulation of Akt signaling is found in about seventy percent of the cases of pancreatic cancer and is associated with high tumor grade and prognosis.
- EGF binding leads to PI3K pathway activation.
- Activated PI3K phosphorylates phosphatidylinositides (PIP3) and this, in turn causes phosphorylation and activation of Akt.
- Phosphorylation of Akt (p-Akt) activates NF-κB and inhibits apoptosis, thereby promoting cell survival.
- Akt also regulates the NF-κB pathway via phosphorylation and activation, causing upregulation of gene transcription.
Deregulation of Hedgehog signaling:[12][66][67][68][69]
- In case of pancreatic development in the embryo, Hedgehog (Hh) signaling is an essential pathway.
- Hedgehog signaling plays an essential role in:
- Tissue morphogenesis
- Organ formation of developing gastrointestinal tract
- Deregulation of the Hh pathway leading to overexpression of Shh is known to contribute to pancreatic tumorigenesis.
- Sonic hedgehog signaling is aberrantly expressed in seventy percent of pancreas specimens from carcinoma patients, implicating its role in pancreatic tumorigenesis.
Gross Pathology
The gross pathology of pancreatic adenocarcinoma, which accounts for three-fourths of all pancreatic malignancies is as follows:[70]
- Grossly, ductal adenocarcinomas of the pancreas tend to be gritty, hard, gray-white poorly defined masses that cause obstruction of the main pancreatic duct and the distal common bile duct.
- Chronic pancreatitis of the obstructed pancreatic segment arises due to obstruction of the main pancreatic duct.
- Patients do not present with malabsorption or steatorrhea as the accessory duct of Santorini can still allow bypass of the main pancreatic duct.
- The head of the pancreas is most commonly involved.
- Head lesions make up 75% of all lesions, while the rest are body/tail lesions.
- Ductal adenocarcinomas do not always originate in the main pancreatic or major branch ducts and may arise in small ducts within the peripheral acinar tissue. Hence, the term "ductal" is based on histology and not the origin.
Microscopic Pathology
On microscopic histopathological analysis, the following features are noted:[71]
- Majority of ductal adenocarcinomas have varying degrees of mucin production and duct-like structures and present as moderate-poorly differentiated masses.
- The ductal adenocarcinomas are referred to as “desmoplastic” or "scirrhous" carcinomas due to their characteristic dense stromal fibrosis occurring due to alterations in transforming growth factor-beta (TGF-beta) signaling.
- There is typically considerable desmoplasia or formation of a dense fibrous stroma or structural tissue consisting of a range of cell types (including myofibroblasts, macrophages, lymphocytes and mast cells) and deposited material (such as type I collagen and hyaluronic acid).
- Local extension of tumor cells may occur into adjacent structures such as:[72]
- Superior mesenteric vessels
- Perineural invasion: both inside and outside the pancreas (eg, the retroperitoneum)
- Duodenum
- Portal vein
- Stomach
- Vertebral column
- Adrenal glands
- Spleen
- Transverse colon
- Lymph node spread can occur to the following sites:[73][74]
- Regional peripancreatic lymph nodes
- Mesenteric
- Perigastric
- Portahepatic
- Omental
- Microscopic study reveals the following:
- Mostly glandular appearance, may present as a solid occasionally.
- Nuclei shows the following features:
- Pleomorphism may be observed minimally.
- Nuclei is often small
- Coffee-bean appearance may be observed sometimes
- Cytoplasm shows the following features:
- Granular and abundant.
- Quasi endocrine look is observed, which may stain positive for endocrine markers
- Other features:
- May or may not present with Necrosis.
- May or may not show myxoid degeneration.
- May or may not present with cells around vessels.
-
CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552900
-
CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552901
-
CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552904
-
CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=552903
References
- ↑ 1.0 1.1 Cowgill SM, Muscarella P (2003). "The genetics of pancreatic cancer". Am. J. Surg. 186 (3): 279–86. PMID 12946833.
- ↑ Hruban RH, Petersen GM, Goggins M, Tersmette AC, Offerhaus GJ, Falatko F, Yeo CJ, Kern SE (1999). "Familial pancreatic cancer". Ann. Oncol. 10 Suppl 4: 69–73. PMID 10436789.
- ↑ Greer JB, Whitcomb DC, Brand RE (2007). "Genetic predisposition to pancreatic cancer: a brief review". Am. J. Gastroenterol. 102 (11): 2564–9. doi:10.1111/j.1572-0241.2007.01475.x. PMID 17958761.
- ↑ Soto JL, Barbera VM, Saceda M, Carrato A (2006). "Molecular biology of exocrine pancreatic cancer". Clin Transl Oncol. 8 (5): 306–12. PMID 16760004.
- ↑ Shi C, Daniels JA, Hruban RH (2008). "Molecular characterization of pancreatic neoplasms". Adv Anat Pathol. 15 (4): 185–95. doi:10.1097/PAP.0b013e31817bf57d. PMID 18580095.
- ↑ Blansfield JA, Choyke L, Morita SY, Choyke PL, Pingpank JF, Alexander HR, Seidel G, Shutack Y, Yuldasheva N, Eugeni M, Bartlett DL, Glenn GM, Middelton L, Linehan WM, Libutti SK (2007). "Clinical, genetic and radiographic analysis of 108 patients with von Hippel-Lindau disease (VHL) manifested by pancreatic neuroendocrine neoplasms (PNETs)". Surgery. 142 (6): 814–8, discussion 818.e1–2. doi:10.1016/j.surg.2007.09.012. PMID 18063061.
- ↑ Kouvaraki MA, Shapiro SE, Cote GJ, Lee JE, Yao JC, Waguespack SG, Gagel RF, Evans DB, Perrier ND (2006). "Management of pancreatic endocrine tumors in multiple endocrine neoplasia type 1". World J Surg. 30 (5): 643–53. doi:10.1007/s00268-006-0360-y. PMID 16680581.
- ↑ 8.0 8.1 Maitra A, Kern SE, Hruban RH (2006). "Molecular pathogenesis of pancreatic cancer". Best Pract Res Clin Gastroenterol. 20 (2): 211–26. doi:10.1016/j.bpg.2005.10.002. PMID 16549325.
- ↑ Mimeault M, Brand RE, Sasson AA, Batra SK (2005). "Recent advances on the molecular mechanisms involved in pancreatic cancer progression and therapies". Pancreas. 31 (4): 301–16. PMID 16258363.
- ↑ Talar-Wojnarowska R, Malecka-Panas E (2006). "Molecular pathogenesis of pancreatic adenocarcinoma: potential clinical implications". Med. Sci. Monit. 12 (9): RA186–93. PMID 16940943.
- ↑ Neuman WL, Wasylyshyn ML, Jacoby R, Erroi F, Angriman I, Montag A, Brasitus T, Michelassi F, Westbrook CA (1991). "Evidence for a common molecular pathogenesis in colorectal, gastric, and pancreatic cancer". Genes Chromosomes Cancer. 3 (6): 468–73. PMID 1663781.
- ↑ 12.0 12.1 Matthaios D, Zarogoulidis P, Balgouranidou I, Chatzaki E, Kakolyris S (2011). "Molecular pathogenesis of pancreatic cancer and clinical perspectives". Oncology. 81 (3–4): 259–72. doi:10.1159/000334449. PMID 22116519.
- ↑ Konner J, O'Reilly E (2002). "Pancreatic cancer: epidemiology, genetics, and approaches to screening". Oncology (Williston Park, N.Y.). 16 (12): 1615–22, 1631–2, discussion 1632–3, 1637–8. PMID 12520639.
- ↑ Hilgers W, Rosty C, Hahn SA (2002). "Molecular pathogenesis of pancreatic cancer". Hematol. Oncol. Clin. North Am. 16 (1): 17–35, v. PMID 12063826.
- ↑ Hruban RH, Iacobuzio-Donahue C, Wilentz RE, Goggins M, Kern SE (2001). "Molecular pathology of pancreatic cancer". Cancer J. 7 (4): 251–8. PMID 11561601.
- ↑ Singh S, Chitkara D, Kumar V, Behrman SW, Mahato RI (2013). "miRNA profiling in pancreatic cancer and restoration of chemosensitivity". Cancer Lett. 334 (2): 211–20. doi:10.1016/j.canlet.2012.10.008. PMID 23073476.
- ↑ Yan L, McFaul C, Howes N, Leslie J, Lancaster G, Wong T, Threadgold J, Evans J, Gilmore I, Smart H, Lombard M, Neoptolemos J, Greenhalf W (2005). "Molecular analysis to detect pancreatic ductal adenocarcinoma in high-risk groups". Gastroenterology. 128 (7): 2124–30. PMID 15940643.
- ↑ Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Kamiyama H, Jimeno A, Hong SM, Fu B, Lin MT, Calhoun ES, Kamiyama M, Walter K, Nikolskaya T, Nikolsky Y, Hartigan J, Smith DR, Hidalgo M, Leach SD, Klein AP, Jaffee EM, Goggins M, Maitra A, Iacobuzio-Donahue C, Eshleman JR, Kern SE, Hruban RH, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW (2008). "Core signaling pathways in human pancreatic cancers revealed by global genomic analyses". Science. 321 (5897): 1801–6. doi:10.1126/science.1164368. PMC 2848990. PMID 18772397.
- ↑ Li Y, Bhuiyan M, Vaitkevicius VK, Sarkar FH (1998). "Molecular analysis of the p53 gene in pancreatic adenocarcinoma". Diagn. Mol. Pathol. 7 (1): 4–9. PMID 9646028.
- ↑ Garcea G, Neal CP, Pattenden CJ, Steward WP, Berry DP (2005). "Molecular prognostic markers in pancreatic cancer: a systematic review". Eur. J. Cancer. 41 (15): 2213–36. doi:10.1016/j.ejca.2005.04.044. PMID 16146690.
- ↑ Schutte M, Hruban RH, Geradts J, Maynard R, Hilgers W, Rabindran SK, Moskaluk CA, Hahn SA, Schwarte-Waldhoff I, Schmiegel W, Baylin SB, Kern SE, Herman JG (1997). "Abrogation of the Rb/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas". Cancer Res. 57 (15): 3126–30. PMID 9242437.
- ↑ Goggins M, Kern SE, Offerhaus JA, Hruban RH (1999). "Progress in cancer genetics: lessons from pancreatic cancer". Ann. Oncol. 10 Suppl 4: 4–8. PMID 10436774.
- ↑ 23.0 23.1 Klein AP, Hruban RH, Brune KA, Petersen GM, Goggins M (2001). "Familial pancreatic cancer". Cancer J. 7 (4): 266–73. PMID 11561603.
- ↑ Mangray S, King TC (1998). "Molecular pathobiology of pancreatic adenocarcinoma". Front. Biosci. 3: D1148–60. PMID 9820739.
- ↑ Wang C, Lu X (2000). "[Alterations of the p16 gene for the carcinogenesis in pancreas]". Zhongguo Yi Xue Ke Xue Yuan Xue Bao (in Chinese). 22 (5): 491–3. PMID 12903437.
- ↑ Gerdes B, Bartsch DK, Ramaswamy A, Kersting M, Wild A, Schuermann M, Frey M, Rothmund M (2000). "Multiple primary tumors as an indicator for p16INK4a germline mutations in pancreatic cancer patients?". Pancreas. 21 (4): 369–75. PMID 11075991.
- ↑ Goggins M, Schutte M, Lu J, Moskaluk CA, Weinstein CL, Petersen GM, Yeo CJ, Jackson CE, Lynch HT, Hruban RH, Kern SE (1996). "Germline BRCA2 gene mutations in patients with apparently sporadic pancreatic carcinomas". Cancer Res. 56 (23): 5360–4. PMID 8968085.
- ↑ Hahn SA, Greenhalf B, Ellis I, Sina-Frey M, Rieder H, Korte B, Gerdes B, Kress R, Ziegler A, Raeburn JA, Campra D, Grützmann R, Rehder H, Rothmund M, Schmiegel W, Neoptolemos JP, Bartsch DK (2003). "BRCA2 germline mutations in familial pancreatic carcinoma". J. Natl. Cancer Inst. 95 (3): 214–21. PMID 12569143.
- ↑ Murphy KM, Brune KA, Griffin C, Sollenberger JE, Petersen GM, Bansal R, Hruban RH, Kern SE (2002). "Evaluation of candidate genes MAP2K4, MADH4, ACVR1B, and BRCA2 in familial pancreatic cancer: deleterious BRCA2 mutations in 17%". Cancer Res. 62 (13): 3789–93. PMID 12097290.
- ↑ Hruban RH, Petersen GM, Ha PK, Kern SE (1998). "Genetics of pancreatic cancer. From genes to families". Surg. Oncol. Clin. N. Am. 7 (1): 1–23. PMID 9443984.
- ↑ Kojima K, Vickers SM, Adsay NV, Jhala NC, Kim HG, Schoeb TR, Grizzle WE, Klug CA (2007). "Inactivation of Smad4 accelerates Kras(G12D)-mediated pancreatic neoplasia". Cancer Res. 67 (17): 8121–30. doi:10.1158/0008-5472.CAN-06-4167. PMID 17804724.
- ↑ Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M (1988). "Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes". Cell. 53 (4): 549–54. PMID 2453289.
- ↑ Laghi L, Orbetegli O, Bianchi P, Zerbi A, Di Carlo V, Boland CR, Malesci A (2002). "Common occurrence of multiple K-RAS mutations in pancreatic cancers with associated precursor lesions and in biliary cancers". Oncogene. 21 (27): 4301–6. doi:10.1038/sj.onc.1205533. PMID 12082617.
- ↑ Cheng RF, Wang J, Zhang JY, Sun L, Zhao YR, Qiu ZQ, Sun BC, Sun Y (2016). "MicroRNA-506 is up-regulated in the development of pancreatic ductal adenocarcinoma and is associated with attenuated disease progression". Chin J Cancer. 35 (1): 64. doi:10.1186/s40880-016-0128-9. PMC 4930606. PMID 27371108.
- ↑ Hayashi N, Egami H, Ogawa M (2002). "[Genetics of pancreatic cancer: recent advances in molecular diagnosis]". Nihon Geka Gakkai Zasshi (in Japanese). 103 (6): 476–81. PMID 12094699.
- ↑ Howe JR, Conlon KC (1997). "The molecular genetics of pancreatic cancer". Surg Oncol. 6 (1): 1–18. PMID 9364657.
- ↑ El-Rayes BF, Ali S, Sarkar FH, Philip PA (2004). "Cyclooxygenase-2-dependent and -independent effects of celecoxib in pancreatic cancer cell lines". Mol. Cancer Ther. 3 (11): 1421–6. PMID 15542781.
- ↑ Hussain T, Gupta S, Adhami VM, Mukhtar H (2005). "Green tea constituent epigallocatechin-3-gallate selectively inhibits COX-2 without affecting COX-1 expression in human prostate carcinoma cells". Int. J. Cancer. 113 (4): 660–9. doi:10.1002/ijc.20629. PMID 15455372.
- ↑ Wei D, Wang L, He Y, Xiong HQ, Abbruzzese JL, Xie K (2004). "Celecoxib inhibits vascular endothelial growth factor expression in and reduces angiogenesis and metastasis of human pancreatic cancer via suppression of Sp1 transcription factor activity". Cancer Res. 64 (6): 2030–8. PMID 15026340.
- ↑ Okami J, Yamamoto H, Fujiwara Y, Tsujie M, Kondo M, Noura S, Oshima S, Nagano H, Dono K, Umeshita K, Ishikawa O, Sakon M, Matsuura N, Nakamori S, Monden M (1999). "Overexpression of cyclooxygenase-2 in carcinoma of the pancreas". Clin. Cancer Res. 5 (8): 2018–24. PMID 10473081.
- ↑ Inoue S, Tezel E, Nakao A (2001). "Molecular diagnosis of pancreatic cancer". Hepatogastroenterology. 48 (40): 933–8. PMID 11490843.
- ↑ Wang Z, Banerjee S, Li Y, Rahman KM, Zhang Y, Sarkar FH (2006). "Down-regulation of notch-1 inhibits invasion by inactivation of nuclear factor-kappaB, vascular endothelial growth factor, and matrix metalloproteinase-9 in pancreatic cancer cells". Cancer Res. 66 (5): 2778–84. doi:10.1158/0008-5472.CAN-05-4281. PMID 16510599.
- ↑ Büchler P, Gazdhar A, Schubert M, Giese N, Reber HA, Hines OJ, Giese T, Ceyhan GO, Müller M, Büchler MW, Friess H (2005). "The Notch signaling pathway is related to neurovascular progression of pancreatic cancer". Ann. Surg. 242 (6): 791–800, discussion 800–1. PMC 1409885. PMID 16327489.
- ↑ Miyamoto Y, Maitra A, Ghosh B, Zechner U, Argani P, Iacobuzio-Donahue CA, Sriuranpong V, Iso T, Meszoely IM, Wolfe MS, Hruban RH, Ball DW, Schmid RM, Leach SD (2003). "Notch mediates TGF alpha-induced changes in epithelial differentiation during pancreatic tumorigenesis". Cancer Cell. 3 (6): 565–76. PMID 12842085.
- ↑ Wang Z, Zhang Y, Banerjee S, Li Y, Sarkar FH (2006). "Inhibition of nuclear factor kappab activity by genistein is mediated via Notch-1 signaling pathway in pancreatic cancer cells". Int. J. Cancer. 118 (8): 1930–6. doi:10.1002/ijc.21589. PMID 16284950.
- ↑ Wang Z, Zhang Y, Banerjee S, Li Y, Sarkar FH (2006). "Notch-1 down-regulation by curcumin is associated with the inhibition of cell growth and the induction of apoptosis in pancreatic cancer cells". Cancer. 106 (11): 2503–13. doi:10.1002/cncr.21904. PMID 16628653.
- ↑ Wang Z, Zhang Y, Li Y, Banerjee S, Liao J, Sarkar FH (2006). "Down-regulation of Notch-1 contributes to cell growth inhibition and apoptosis in pancreatic cancer cells". Mol. Cancer Ther. 5 (3): 483–93. doi:10.1158/1535-7163.MCT-05-0299. PMID 16546962.
- ↑ Biliran H, Wang Y, Banerjee S, Xu H, Heng H, Thakur A, Bollig A, Sarkar FH, Liao JD (2005). "Overexpression of cyclin D1 promotes tumor cell growth and confers resistance to cisplatin-mediated apoptosis in an elastase-myc transgene-expressing pancreatic tumor cell line". Clin. Cancer Res. 11 (16): 6075–86. doi:10.1158/1078-0432.CCR-04-2419. PMID 16115953.
- ↑ Kornmann M, Arber N, Korc M (1998). "Inhibition of basal and mitogen-stimulated pancreatic cancer cell growth by cyclin D1 antisense is associated with loss of tumorigenicity and potentiation of cytotoxicity to cisplatinum". J. Clin. Invest. 101 (2): 344–52. doi:10.1172/JCI1323. PMC 508573. PMID 9435306.
- ↑ Bruns CJ, Harbison MT, Davis DW, Portera CA, Tsan R, McConkey DJ, Evans DB, Abbruzzese JL, Hicklin DJ, Radinsky R (2000). "Epidermal growth factor receptor blockade with C225 plus gemcitabine results in regression of human pancreatic carcinoma growing orthotopically in nude mice by antiangiogenic mechanisms". Clin. Cancer Res. 6 (5): 1936–48. PMID 10815919.
- ↑ Marshall J (2006). "Clinical implications of the mechanism of epidermal growth factor receptor inhibitors". Cancer. 107 (6): 1207–18. doi:10.1002/cncr.22133. PMID 16909423.
- ↑ Wang Z, Sengupta R, Banerjee S, Li Y, Zhang Y, Rahman KM, Aboukameel A, Mohammad R, Majumdar AP, Abbruzzese JL, Sarkar FH (2006). "Epidermal growth factor receptor-related protein inhibits cell growth and invasion in pancreatic cancer". Cancer Res. 66 (15): 7653–60. doi:10.1158/0008-5472.CAN-06-1019. PMID 16885366.
- ↑ Zhang Y, Banerjee S, Wang Z, Xu H, Zhang L, Mohammad R, Aboukameel A, Adsay NV, Che M, Abbruzzese JL, Majumdar AP, Sarkar FH (2006). "Antitumor activity of epidermal growth factor receptor-related protein is mediated by inactivation of ErbB receptors and nuclear factor-kappaB in pancreatic cancer". Cancer Res. 66 (2): 1025–32. doi:10.1158/0008-5472.CAN-05-2968. PMID 16424038.
- ↑ Zhang Y, Banerjee S, Wang ZW, Marciniak DJ, Majumdar AP, Sarkar FH (2005). "Epidermal growth factor receptor-related protein inhibits cell growth and induces apoptosis of BxPC3 pancreatic cancer cells". Cancer Res. 65 (9): 3877–82. doi:10.1158/0008-5472.CAN-04-3654. PMID 15867387.
- ↑ Wang W, Abbruzzese JL, Evans DB, Chiao PJ (1999). "Overexpression of urokinase-type plasminogen activator in pancreatic adenocarcinoma is regulated by constitutively activated RelA". Oncogene. 18 (32): 4554–63. doi:10.1038/sj.onc.1202833. PMID 10467400.
- ↑ Bava SV, Puliappadamba VT, Deepti A, Nair A, Karunagaran D, Anto RJ (2005). "Sensitization of taxol-induced apoptosis by curcumin involves down-regulation of nuclear factor-kappaB and the serine/threonine kinase Akt and is independent of tubulin polymerization". J. Biol. Chem. 280 (8): 6301–8. doi:10.1074/jbc.M410647200. PMID 15590651.
- ↑ Fahy BN, Schlieman MG, Virudachalam S, Bold RJ (2004). "Inhibition of AKT abrogates chemotherapy-induced NF-kappaB survival mechanisms: implications for therapy in pancreatic cancer". J. Am. Coll. Surg. 198 (4): 591–9. doi:10.1016/j.jamcollsurg.2003.12.005. PMID 15051014.
- ↑ Fujioka S, Sclabas GM, Schmidt C, Frederick WA, Dong QG, Abbruzzese JL, Evans DB, Baker C, Chiao PJ (2003). "Function of nuclear factor kappaB in pancreatic cancer metastasis". Clin. Cancer Res. 9 (1): 346–54. PMID 12538487.
- ↑ Karin M (2006). "Nuclear factor-kappaB in cancer development and progression". Nature. 441 (7092): 431–6. doi:10.1038/nature04870. PMID 16724054.
- ↑ Li L, Aggarwal BB, Shishodia S, Abbruzzese J, Kurzrock R (2004). "Nuclear factor-kappaB and IkappaB kinase are constitutively active in human pancreatic cells, and their down-regulation by curcumin (diferuloylmethane) is associated with the suppression of proliferation and the induction of apoptosis". Cancer. 101 (10): 2351–62. doi:10.1002/cncr.20605. PMID 15476283.
- ↑ Li Y, Ahmed F, Ali S, Philip PA, Kucuk O, Sarkar FH (2005). "Inactivation of nuclear factor kappaB by soy isoflavone genistein contributes to increased apoptosis induced by chemotherapeutic agents in human cancer cells". Cancer Res. 65 (15): 6934–42. doi:10.1158/0008-5472.CAN-04-4604. PMID 16061678.
- ↑ Li Y, Chinni SR, Sarkar FH (2005). "Selective growth regulatory and pro-apoptotic effects of DIM is mediated by AKT and NF-kappaB pathways in prostate cancer cells". Front. Biosci. 10: 236–43. PMID 15574364.
- ↑ Liptay S, Weber CK, Ludwig L, Wagner M, Adler G, Schmid RM (2003). "Mitogenic and antiapoptotic role of constitutive NF-kappaB/Rel activity in pancreatic cancer". Int. J. Cancer. 105 (6): 735–46. doi:10.1002/ijc.11081. PMID 12767057.
- ↑ {{cite journal |vauthors=Rahman KW, Sarkar FH |title=Inhibition of nuclear translocation of nuclear factor-{kappa}B contributes to 3,3'-diindolylmethane-induced apoptosis in breast cancer cells |journal=Cancer Res. |volume=65 |issue=1 |pages=364–71 |year=2005 |pmid=15665315 |doi= |url=}}
- ↑ Zhang H, Morisaki T, Nakahara C, Matsunaga H, Sato N, Nagumo F, Tadano J, Katano M (2003). "PSK-mediated NF-kappaB inhibition augments docetaxel-induced apoptosis in human pancreatic cancer cells NOR-P1". Oncogene. 22 (14): 2088–96. doi:10.1038/sj.onc.1206310. PMID 12687011.
- ↑ Nakashima H, Nakamura M, Yamaguchi H, Yamanaka N, Akiyoshi T, Koga K, Yamaguchi K, Tsuneyoshi M, Tanaka M, Katano M (2006). "Nuclear factor-kappaB contributes to hedgehog signaling pathway activation through sonic hedgehog induction in pancreatic cancer". Cancer Res. 66 (14): 7041–9. doi:10.1158/0008-5472.CAN-05-4588. PMID 16849549.
- ↑ Thayer SP, di Magliano MP, Heiser PW, Nielsen CM, Roberts DJ, Lauwers GY, Qi YP, Gysin S, Fernández-del Castillo C, Yajnik V, Antoniu B, McMahon M, Warshaw AL, Hebrok M (2003). "Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis". Nature. 425 (6960): 851–6. doi:10.1038/nature02009. PMC 3688051. PMID 14520413.
- ↑ Berman DM, Karhadkar SS, Maitra A, Montes De Oca R, Gerstenblith MR, Briggs K, Parker AR, Shimada Y, Eshleman JR, Watkins DN, Beachy PA (2003). "Widespread requirement for Hedgehog ligand stimulation in growth of digestive tract tumours". Nature. 425 (6960): 846–51. doi:10.1038/nature01972. PMID 14520411.
- ↑ Mathew E, Zhang Y, Holtz AM, Kane KT, Song JY, Allen BL, Pasca di Magliano M (2014). "Dosage-dependent regulation of pancreatic cancer growth and angiogenesis by hedgehog signaling". Cell Rep. 9 (2): 484–94. doi:10.1016/j.celrep.2014.09.010. PMC 4362534. PMID 25310976.
- ↑ Esposito I, Konukiewitz B, Schlitter AM, Klöppel G (2014). "Pathology of pancreatic ductal adenocarcinoma: facts, challenges, and future developments". World J. Gastroenterol. 20 (38): 13833–41. doi:10.3748/wjg.v20.i38.13833. PMC 4194566. PMID 25320520.
- ↑ Rossi ML, Rehman AA, Gondi CS (2014). "Therapeutic options for the management of pancreatic cancer". World J. Gastroenterol. 20 (32): 11142–59. doi:10.3748/wjg.v20.i32.11142. PMC 4145755. PMID 25170201.
- ↑ Oda Y, Aishima S, Morimatsu K, Shindo K, Fujino M, Mizuuchi Y, Hattori M, Miyazaki T, Tanaka M, Oda Y (2014). "Pancreatic intraepithelial neoplasia in the background of invasive ductal carcinoma of the pancreas as a prognostic factor". Histopathology. 65 (3): 389–97. doi:10.1111/his.12397. PMID 24931343.
- ↑ Yachida S, Jones S, Bozic I, Antal T, Leary R, Fu B, Kamiyama M, Hruban RH, Eshleman JR, Nowak MA, Velculescu VE, Kinzler KW, Vogelstein B, Iacobuzio-Donahue CA (2010). "Distant metastasis occurs late during the genetic evolution of pancreatic cancer". Nature. 467 (7319): 1114–7. doi:10.1038/nature09515. PMC 3148940. PMID 20981102.
- ↑ Campbell PJ, Yachida S, Mudie LJ, Stephens PJ, Pleasance ED, Stebbings LA, Morsberger LA, Latimer C, McLaren S, Lin ML, McBride DJ, Varela I, Nik-Zainal SA, Leroy C, Jia M, Menzies A, Butler AP, Teague JW, Griffin CA, Burton J, Swerdlow H, Quail MA, Stratton MR, Iacobuzio-Donahue C, Futreal PA (2010). "The patterns and dynamics of genomic instability in metastatic pancreatic cancer". Nature. 467 (7319): 1109–13. doi:10.1038/nature09460. PMC 3137369. PMID 20981101.