Nephrologic Disorders and COVID-19
To go to the COVID-19 project topics list, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sogand Goudarzi, MD [2] Nasrin Nikravangolsefid, MD-MPH [3]
Complication 1: Acute Kidney Injury in COVID-19
Synonyms and keywords: Acute Kidney Injury, Acute Renal Failure, AKI, ARF
Overview
- COVID-19 can involve many organs leading to organ failure, one of which is kidneys that manifest with mild proteinuria to advanced acute kidney injury (AKI).[1]
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2), which is a primary receptor for SARS-CoV-2 entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.[2]
- Despite kidney injury following COVID-19 infection is less frequent than severe lung injury, ACE2: ACE ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)[2]
- After SARS-CoV-2 enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
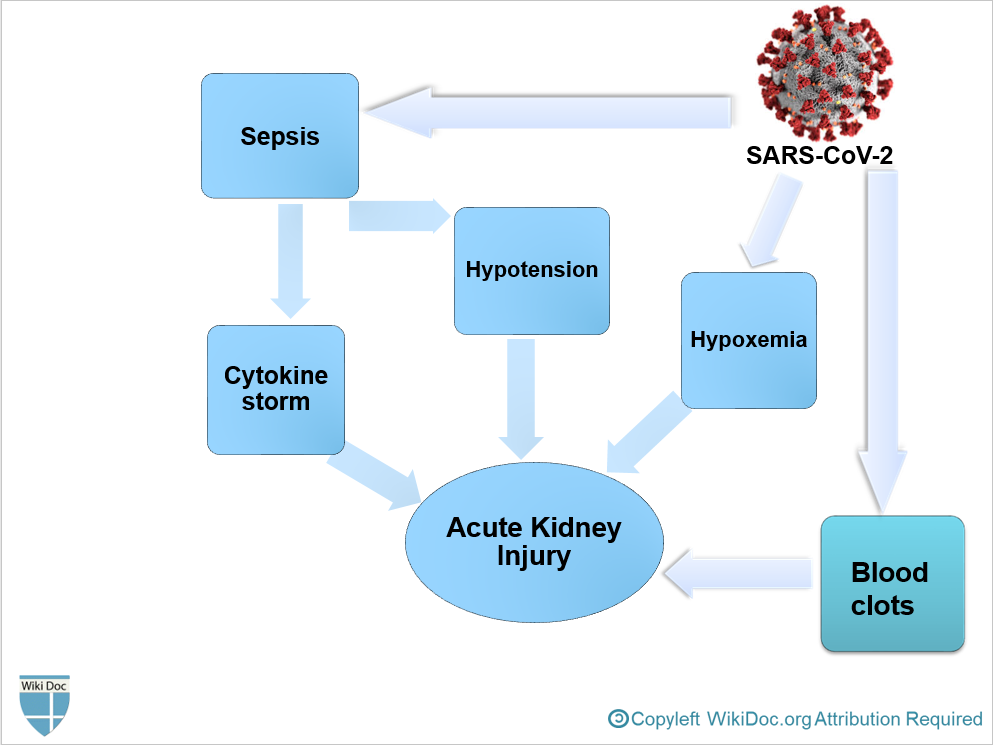
- It is thought that AKI following COVID-19 is the result of[2]
- Sepsis and cytokine storm
- Hypovolemia and Hypotension
- Hypoxemia
- Blood clots formation, leading to impaired blood flow in the renal arterioles.
- AKI is more likely to develop in the late stages of COVID-19 in critically ill patients.[1]
Natural history
- AKI is frequently seen among patients with COVID-19 hospitalized in ICU, with prevalence of 0.6-29% in China "Acute Kidney Injury in COVID-19 Patients | COVID-19". and 22.2% in the USA.[3]
- While, the real incidence of AKI in critcally ill patients with COVID-19 is estimated between 27-85%. "Acute Kidney Injury in COVID-19 Patients | COVID-19".
- Severe COVID-19 pneumonia and severe acute respiratory distress syndrome are associated with developing AKI.[4]
- Approximately half of the new AKI cases following COVID-19 is mild with good short-term prognosis.
- If no improvement occurs during follow-up, it is contributed to higher mortality.[4]
- Early diagnosis and treatment of AKI in patients with COVID-19 can avoid the progression of AKI into ESRD and reduce mortality.[1]
History and Symptoms
- Patients in the early stages of kidney failure may be asymptomatic. If left untreated, patients may progress to develop Azotemia and Uremia, which occur due to the buildup of waste materials in the blood.
History and Symptoms
- Symptoms of kidney injury include[5]:
- Nausea and Vomiting
- Weakness
- Fatigue
- Confusion
- Weight loss
- Loss of appetite
- Decrease in urine output:Oliguria or Anuria
- Fluid retention, leading edema and swelling of face, extremities
- Electrolyte imbalance; High level of Potassium which leads to cardiac arrhythmia
Physical Examination
- Hypotension
- Peripheral edema
- Rales in lungs examination
Diagnosis
Laboratory Findings
- Laboratory findings consistent with the diagnosis of AKI include:
- Elevated BUN level
- Plasma BUN-creatinine ratio> 20 in prerenal AKI
- Plasma BUN-creatinine ratio< 15 in intrinsic AKI or Acute Tubular Necrosis
- Based on KDIGO definition for the diagnosis of AKI[6]:
- Elevated serum Creatinine by ≥0.3 mg/dl (≥26.5 μmol/l) within 48 hours; or
- Elevated serum Creatinine to ≥1.5 times baseline within the previous 7 days; or
- Urine volume < 0.5 ml/kg/h for >6 hours
- Fractional excretion of sodium (FENa)
- (FENa)< 1% in prerenal AKI
- (FENa)> 2% in intrinsic AKI or Acute Tubular Necrosis
- Urinary sediment
- Hyaline casts in prerenal AKI
- Granular or Muddy brown casts in intrinsic AKI or Acute Tubular Necrosis
- Elevated BUN level
Electrocardiogram
- There are no specific ECG findings associated with AKI. However, electrolyte disturbances such as hyperkalemia might lead to various ECG findings.
Ultrasound Finding
Other Diagnostic Studies
Treatment
- Management of AKI following COVID-19 includes treatment of infection, identifying electrolyte disorders, and intravenous fluid administration.
AKI Medical Therapy
- Treatment of AKI following COVID-19 includes[1]:
- Correction of hypovolemia and hypotension by the administration of adequate intravenous fluid
- Correction of electrolyte disturbances
- Renal Replacement Therapy
- If AKI is unresponsive to conservative therapy
- In volume overload conditions
- Modality of choice in unstable hemodynamic status and ESRD
- Anticoagulants in hypercoagulable conditions
- Sequential extracorporeal therapy
References
- ↑ 1.0 1.1 1.2 1.3 Ronco C, Reis T, Husain-Syed F (2020). "Management of acute kidney injury in patients with COVID-19". Lancet Respir Med. doi:10.1016/S2213-2600(20)30229-0. PMC 7255232 Check
|pmc=value (help). PMID 32416769 Check|pmid=value (help). - ↑ 2.0 2.1 2.2 Malha, Line; Mueller, Franco B.; Pecker, Mark S.; Mann, Samuel J.; August, Phyllis; Feig, Peter U. (2020). "COVID-19 and the Renin-Angiotensin System". Kidney International Reports. 5 (5): 563–565. doi:10.1016/j.ekir.2020.03.024. ISSN 2468-0249.
- ↑ Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW; et al. (2020). "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area". JAMA. doi:10.1001/jama.2020.6775. PMC 7177629 Check
|pmc=value (help). PMID 32320003 Check|pmid=value (help). - ↑ 4.0 4.1 Pei, Guangchang; Zhang, Zhiguo; Peng, Jing; Liu, Liu; Zhang, Chunxiu; Yu, Chong; Ma, Zufu; Huang, Yi; Liu, Wei; Yao, Ying; Zeng, Rui; Xu, Gang (2020). "Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia". Journal of the American Society of Nephrology. 31 (6): 1157–1165. doi:10.1681/ASN.2020030276. ISSN 1046-6673.
- ↑ Skorecki K, Green J, Brenner BM (2005). "Chronic renal failure". In Kasper DL, Braunwald E, Fauci AS, et al. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 1653–63. ISBN 978-0-07-139140-5.
- ↑ Khwaja A (2012). "KDIGO clinical practice guidelines for acute kidney injury". Nephron Clin Pract. 120 (4): c179–84. doi:10.1159/000339789. PMID 22890468.