Jefferson fracture
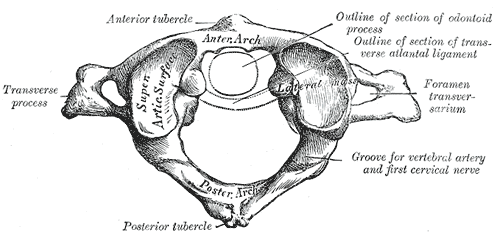
A Jefferson fracture is a bone fracture occurring at the first vertebrae. It is classically described as a four-part break that fractures the anterior and posterior arches of the vertebra,[1] though it may also appear as a three or two part fracture. The fracture may result from compression of the second vertebra or hyperextension of the neck, causing a posterior break, and may be accompanied by a break in other parts of the cervical spine.[1]
It is named after the British neurologist and neurosurgeon Sir Geoffrey Jefferson, who reported four cases of the fracture in 1920 in addition to reviewing previous cases that had been reported previously.[2]
The differential diagnoses include: occipital condyle fractures; fractures through the superior facets of C2; odontoid fractures; ligamentous injuries; blunt vertebral artery injuries; vertebral artery dissection; and fractures through the remaining subaxial cervical spine, including vertebral body fractures, transverse process fractures, spinous process fractures, and compression fractures.[3]
Etiology
The most common mechanism of injury is axial compression to C1. This is seen in injuries involving direct head impact, such as head-first tackling in football or diving into shallow water. Jefferson fractures are also commonly seen in high impact motor vehicle collisions and traumatic falls.[4] In children, Jefferson fractures may occur due to falls from playground equipment.[5] Less frequently, strong rotation of the head may also result in Jefferson fractures.[6]
Jefferson fractures are extremely rare in children, but recovery is usually complete without surgery.[5] Atlas fractures account for 1-2% of spinal column fractures and 2-13% of overall injuries to the cervical spine. [7] [4][8] There is a bimodal distribution of atlas fractures, with most injuries seen in those in their mid-twenties and between 80-84 years of age.[8] Approximately 57-69% of atlas fractures occur in males.[8] The risk of cervical injury is doubled in trauma patients greater than 65 years old.[3]
Symptoms
Individuals with Jefferson fractures usually experience pain in the cervical spine following a traumatic axial force or hyperextension injury to the neck.[8][4] Patients may describe this as a muscle spasm or pain at the base of the occiput. On exam, they may have focal midline tenderness to palpation of the cervical spine, with limited and/or painful range of motion.[4][9] As the spinal canal is relatively wide at C1 and fracture segments tend to spread outward, neurological signs/deficits are not common, but if the transverse atlantal ligament is compromised, the dens may impact the spinal cord and result in neurological deficits..[3][8][7] The fracture may also cause damage to the arteries in the neck, resulting in Lateral medullary syndrome, Horner's syndrome, ataxia, and the inability to sense pain or temperature.[1]
In rare cases, congenital abnormality may cause the same symptoms as a Jefferson fracture.[10][11]
Treatment
Immediately place patients with a suspected or confirmed Jefferson fracture in spinal immobilization using a rigid cervical collar. Often times, a cervical collar is already placed by EMS in the prehospital setting. The use of surgery to treat a Jefferson fracture is somewhat controversial.[12] A primary factor in deciding between surgical and non-surgical intervention is the degree of stability[12][13] as well as the presence of damage to other cervical vertebrae.[13] Stable, isolated Jefferson fractures, defined as having an intact transverse atlantal ligament, are treated successfully with external immobilization devices such as rigid cervical collars, a halo-thoracic braces, or a sterno-occipitomandibular braces for 8-12 weeks.[14][8] The use of rigid halos can lead to intracranial infections and are often uncomfortable for individuals wearing them, and may be replaced with a more flexible alternative depending on the stability of the injured bones, but treatment of a stable injury with a halo collar can result in a full recovery.[13] If there is a disruption of the transverse atlantal ligament, a C1-C2 fusion can be performed. Discuss treatment and disposition in conjunction with Neurosurgery or Orthopedics, depending on institutional practice. [Mead, Ryken]
Non-surgical treatment varies depending on if the fracture is stable or unstable, defined by an intact or broken transverse ligament and degree of fracture of the anterior arch.[15][1] An intact ligament requires the use of a soft or hard collar, while a ruptured ligament may require traction, a halo or surgery. Surgical treatment of a Jefferson fracture involves fusion or fixation of the first three cervical vertebrae;[12][1] fusion may occur immediately, or later during treatment in cases where non-surgical interventions are unsuccessful.[12]
Though a serious injury, the long-term consequences of a Jefferson's fracture are uncertain and may not impact longevity or abilities, even if untreated.[16] Conservative treatment with an immobilization device can produce excellent long-term recovery.[17][18]
Pain, however, is a frequent complaint for patients, even beyond the first year after injury. Nearly 14-80% of patients report mild neck pain, 20% report scalp dysesthesias, and 8-20% report neck stiffness. Nearly 34% of patients with a Jefferson fracture report at least some impairment of daily living activities.[19]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Wheeless, Clifford. "Atlas Frx / Jefferson Fracture". Duke University Division of Orthopaedic Surgery. Retrieved 2007-11-29.
- ↑ Jefferson G (1920). "Fracture of the atlas vertebra: report of four cases, and a review of those previously recorded". Br J Surg. 7: 407–22. doi:10.1002/bjs.1800072713.
- ↑ 3.0 3.1 3.2 Pimentel, L (2010). "Evaluation and Management of Acute Cervical Spine Trauma". Emergency Medicine Clinics of North America. 28: 719–38.
- ↑ 4.0 4.1 4.2 4.3 Ivancic, P (2012). "Atlas injury mechanisms during head-first impact". Spine. 37: 1022–29.
- ↑ 5.0 5.1 Korinth MC, Kapser A, Weinzierl MR (2007). "Jefferson fracture in a child--illustrative case report". Pediatr Neurosurg. 43 (6): 526–30. doi:10.1159/000108801. PMID 17992046.
- ↑ Foster, Mark (2006-12-01). "C1 Fractures". WebMD. Retrieved 2007-11-29.
- ↑ 7.0 7.1 Gardner, A (2005). "Cervical spine trauma". Trauma. 7: 109–21.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Mead, L (2016). "C1 fractures: a review of diagnoses, management options, and outcomes". Current Reviews in Musculoskeletal Medicine. 9: 255–62.
- ↑ Ly, J (2002). "Jefferson Fracture". Journal of emergency medicine. 23: 415–16.
- ↑ de Zoete A, Langeveld UA (2007). "A congenital anomaly of the atlas as a diagnostic dilemma: a case report". J Manipulative Physiol Ther. 30 (1): 62–4. doi:10.1016/j.jmpt.2006.11.011. PMID 17224357.
- ↑ Gehweiler JA, Daffner RH, Roberts L (1983). "Malformations of the atlas vertebra simulating the Jefferson fracture". AJR Am J Roentgenol. 140 (6): 1083–6. PMID 6602470.
- ↑ 12.0 12.1 12.2 12.3 Hein C, Richter HP, Rath SA (2002). "Atlantoaxial screw fixation for the treatment of isolated and combined unstable jefferson fractures - experiences with 8 patients". Acta Neurochir (Wien). 144 (11): 1187–92. doi:10.1007/s00701-002-0998-2. PMID 12434175.
- ↑ 13.0 13.1 13.2 Lee TT, Green BA, Petrin DR (1998). "Treatment of stable burst fracture of the atlas (Jefferson fracture) with rigid cervical collar". Spine. 23 (18): 1963–7. PMID 9779528.
- ↑ Ryken, T (2013). "Management of isolated fractures of the Axis in Adults". Neurosurgery. 72: 132–150.
- ↑ Lee C, Woodring JH (1991). "Unstable Jefferson variant atlas fractures: an unrecognized cervical injury". AJNR Am J Neuroradiol. 12 (6): 1105–10. PMID 1763734.
- ↑ Mindell ER (2005). "James Platt White, MD (1811-1881): his interesting and remarkable accident". Clin. Orthop. Relat. Res. (430): 227–31. PMID 15662328.
- ↑ Kesterson L, Benzel E, Orrison W, Coleman J (1991). "Evaluation and treatment of atlas burst fractures (Jefferson fractures)". J. Neurosurg. 75 (2): 213–20. PMID 2072157.
- ↑ Claux E, Everaert P (1989). "[Result 5 years after orthopedic treatment of a Jefferson fracture]". Acta Orthop Belg (in French). 55 (2): 233–7. PMID 2801087.
- ↑ Lewkonia, P (2012). "An Evidence-Based Medicine Process to Determine Outcomes After Cervical Spine Trauma". Spine. 37: E1140–E1147.