|
|
| (45 intermediate revisions by 9 users not shown) |
| Line 1: |
Line 1: |
| {{Influenza}} | | {| class="infobox" style="float:right;" |
| | | |- |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]'''
| | | [[File:Siren.gif|30px|link=Influenza resident survival guide]]|| <br> || <br> |
| | | [[Influenza resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = Influenza | | | Name = Influenza | |
| Line 7: |
Line 9: |
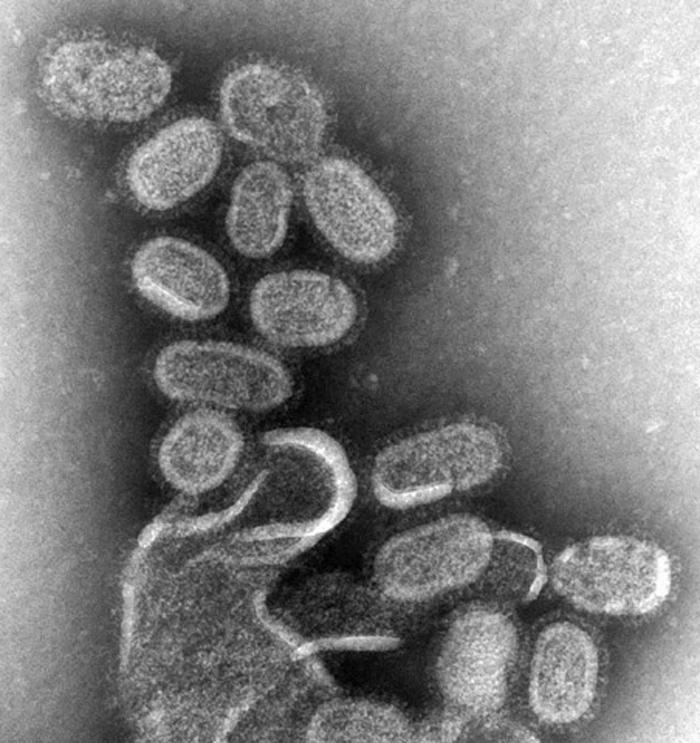
| Caption = [[transmission electron microscopy|TEM]] of negatively stained influenza virons, magnified approximately 70,000 times | | | Caption = [[transmission electron microscopy|TEM]] of negatively stained influenza virons, magnified approximately 70,000 times | |
| Width = 226 | | | Width = 226 | |
| DiseasesDB = 6791 |
| |
| ICD10 = {{ICD10|J|10||j|09}}, {{ICD10|J|11||j|09}} |
| |
| ICD9 = {{ICD9|487}} |
| |
| MedlinePlus = 000080 |
| |
| eMedicineSubj = |
| |
| eMedicineTopic = |
| |
| eMedicine_mult = |
| |
| MeshID = D007251 |
| |
| }} | | }} |
| {{Flu}} | | __NOTOC__ |
| | {{Influenza}} |
| | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
|
| |
|
| {{CMG}}
| | '''For more information about non-human (variant) influenza viruses that may be transmitted to humans, see [[Zoonotic influenza]]''' |
|
| |
|
| ==[[Influenza overview|Overview]]==
| | {{CMG}}; {{AE}} {{AL}}; {{Ammu}} |
|
| |
|
| ==Etymology==
| | {{SK}} Flu; influenza A; influenza B; influenza C; human influenza; human influenza virus |
| The term influenza has its origins in 15th-century Italy, where the cause of the disease was ascribed to unfavourable astrological ''influences''. Evolution in medical thought led to its modification to ''influenza del freddo'', meaning "influence of the cold." The word "influenza" was first attested in English in 1743 when it was borrowed during an outbreak of the disease in Europe.<ref name=Harper>{{cite web | last = Harper | first = D | title=Influenza | url=http://www.etymonline.com/index.php?search=influenza&searchmode=none | publisher= Etymonlin}}</ref> Archaic terms for influenza include epidemic catarrh, grippe (from the French grippe, meaning flu; sometimes spelled "grip" or "gripe"), sweating sickness, and Spanish fever (particularly for the [[Spanish flu|1918 pandemic]] strain).<ref>{{cite web | last = Smith | first = P | title=Archaic Medical Terms | url= http://www.paul_smith.doctors.org.uk/ArchaicMedicalTerms.htm | accessdate = 2006-10-23}}</ref>
| |
| | |
| ==[[Influenza historical perspective|Historical perspective]]==
| |
|
| |
|
| | ==[[Influenza overview|Overview]]== |
| | ==[[Influenza historical perspective|Historical Perspective]]== |
| ==[[Influenza classification|Classification]]== | | ==[[Influenza classification|Classification]]== |
| | ==[[Influenza pathophysiology |Pathophysiology]]== |
| | ==[[Influenza causes|Causes]]== |
| | ==[[Influenza differential diagnosis|Differentiating Influenza from other Diseases]]== |
| | ==[[Influenza epidemiology and demographics|Epidemiology and Demographics]]== |
| | ==[[Influenza risk factors|Risk Factors]]== |
| | ==[[Influenza natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| [[Image:Aerosol from Sneeze.jpg |thumb |right|250px|Influenza spreads by [[aerosol]]s created by coughs or sneezes.]] | | [[Influenza history and symptoms|History and Symptoms]] | [[Influenza physical examination|Physical Examination]] | [[Influenza laboratory findings|Laboratory Findings]] | [[Influenza chest x ray|Chest X Ray]] | [[Influenza other diagnostic studies|Other Diagnostic Studies]] |
| In humans, influenza's effects are much more severe than those of the [[common cold]], and last longer. Recovery takes about one to two weeks. Influenza, however, can be deadly, especially for the weak, old or chronically ill.<ref name=Hilleman/>
| |
| | |
| ===Symptoms===
| |
| Symptoms of influenza can start quite suddenly one to two days after infection. Usually the first symptoms are chills or a chilly sensation but fever is also common early in the infection, with body temperatures as high as 39 °C (approximately 103 °F). Many people are so ill that they are confined to bed for several days, with aches and pains throughout their bodies, which are worst in their backs and legs.<ref name=Merck />
| |
| | |
| Common symptoms of the flu such as fever, headaches, and fatigue come from the huge amounts of proinflammatory [[cytokine]]s and [[chemokine]]s (such as [[interferon]] or [[Tumor necrosis factor-alpha|tumor necrosis factor]]) produced from influenza-infected cells.<ref name=Eccles/><ref>{{cite journal | author = Schmitz N, Kurrer M, Bachmann M, Kopf M | title = Interleukin-1 is responsible for acute lung immunopathology but increases survival of respiratory influenza virus infection. | journal = J Virol | volume = 79 | issue = 10 | pages = 6441–8 | year = 2005 | id = PMID 15858027}}</ref> In contrast to the [[rhinovirus]] that causes the [[common cold]], influenza does cause tissue damage, so symptoms are not entirely due to the inflammatory response.<ref>{{cite journal | author = Winther B, Gwaltney J, Mygind N, Hendley J | title = Viral-induced rhinitis. | journal = Am J Rhinol | volume = 12 | issue = 1 | pages = 17–20 | year = | id = PMID 9513654}}</ref> Symptoms of influenza may include:
| |
| | |
| :* Body aches, especially joints and throat
| |
| :* [[Cough]]ing and [[sneeze|sneezing]]
| |
| :* Extreme coldness and [[fever]]
| |
| :* [[Fatigue (medical)|Fatigue]]
| |
| :* [[Headache]]
| |
| :* Irritated watering eyes
| |
| :* [[Nasal congestion]]
| |
| :* [[Nausea]] and [[vomiting]]
| |
| :* Reddened eyes, skin (especially face), mouth, throat and nose
| |
| | |
| It can be difficult to distinguish between the common cold and influenza in the early stages of these infections,<ref name=Eccles/> but usually the symptoms of the flu are more severe than their common-cold equivalents. Research on signs and symptoms of influenza found that the best findings for excluding the diagnosis of influenza were:<ref name="pmid15728170">{{cite journal | author = Call S, Vollenweider M, Hornung C, Simel D, McKinney W | title = Does this patient have influenza? | journal = JAMA | volume = 293 | issue = 8 | pages = 987-97 | year = 2005 | doi = 10.1001/jama.293.8.987 | id = PMID 15728170}}</ref>
| |
| | |
| {| class="wikitable" style="text-align:center"
| |
| |+ Highest [[sensitivity (tests)|sensitive]] individual findings for diagnosing influenza<ref name="pmid15728170"/>
| |
| ! Finding: !! [[sensitivity (tests)|sensitivity]] !! [[specificity (tests)|specificity]]
| |
| |-
| |
| ! Fever
| |
| | 86% || 25%
| |
| |-
| |
| ! Cough
| |
| | 98% || 23%
| |
| |-
| |
| ! Nasal congestion
| |
| | 70–90% || 20–40%
| |
| |-
| |
| |}
| |
| Notes to table:
| |
| * [[Sensitivity (tests)|Sensitivity]] is the proportion of people that tested positive of all the positive people tested.
| |
| * [[Specificity (tests)|Specificity]] is the proportion of people that tested negative of all the negative people tested.
| |
| * All three findings, especially fever, were less sensitive in patients over 60 years of age.
| |
| | |
| Since anti-viral drugs are effective in treating influenza if given early (see treatment section, below), it can be important to identify cases early. Of the symptoms listed above, the combinations of findings below can improve diagnostic accuracy.<ref name="pmid11088084">{{cite journal | author = Monto A, Gravenstein S, Elliott M, Colopy M, Schweinle J | title = Clinical signs and symptoms predicting influenza infection. | journal = Arch Intern Med | volume = 160 | issue = 21 | pages = 3243–7 | year = 2000 | url http://archinte.ama-assn.org/cgi/content/abstract/160/21/3243 | id = PMID 11088084}}</ref> Unfortunately, even combinations of findings are imperfect. However, [[Bayes Theorem]] can combine pretest probability with clinical findings to adequately diagnose or exclude influenza in some patients. The pretest probability has a strong seasonal variation; the current prevalence of influenza among patients in the United States receiving sentinel testing is available at the [[Centers for Disease Control and Prevention|CDC]].<ref>Centers for Disease Control and Prevention. [http://www.cdc.gov/flu/weekly/ Weekly Report: Influenza Summary Update.] Accessed January 1, 2007.</ref> Using the CDC data, the following table shows how the likelihood of influenza varies with prevalence:
| |
| :
| |
| | |
| <table border="1" cellpadding="5" class="wikitable">
| |
| <caption>Combinations of findings for diagnosing influenza<ref name="pmid15728170"/></caption>
| |
| <tr>
| |
| <th rowspan="2">Combinations of findings </th>
| |
| <th rowspan="2">Sensitivity</th>
| |
| <th rowspan="2">Specificity</th>
| |
| <th colspan="2"><p>As reported in study<ref name="pmid15728170">.</ref><br/>and projected during local outbreaks<br/>
| |
| (prevalence= 66%)</p>
| |
| </th>
| |
| <th colspan="2">Projected during influenza season <br/>
| |
| (prevalence=25%)</th>
| |
| <th colspan="2">Projected in off-season<br/>
| |
| (prevalence=2%) </th>
| |
| </tr>
| |
| <tr>
| |
| <th>PPV</th>
| |
| <th>NPV</th>
| |
| <th>PPV</th>
| |
| <th>NPV</th>
| |
| <th>PPV</th>
| |
| <th>NPV</th>
| |
| </tr>
| |
| <tr>
| |
| <td>Fever and cough</td>
| |
| <td align="center">64%</td>
| |
| <td align="center">67%</td>
| |
| <td align="center">79%</td>
| |
| <td align="center">49%</td>
| |
| <td align="center">39%</td>
| |
| <td align="center">15%</td>
| |
| <td align="center">4%</td>
| |
| <td align="center">1%</td>
| |
| </tr>
| |
| <tr>
| |
| <td>Fever and cough and sore throat</td>
| |
| <td align="center">56</td>
| |
| <td align="center">71</td>
| |
| <td align="center">79</td>
| |
| <td align="center">45</td>
| |
| <td align="center">39</td>
| |
| <td align="center">17</td>
| |
| <td align="center">4</td>
| |
| <td align="center">2</td>
| |
| </tr>
| |
| <tr>
| |
| <td>Fever and cough and nasal congestion</td>
| |
| <td align="center">59</td>
| |
| <td align="center">74</td>
| |
| <td align="center">81</td>
| |
| <td align="center">48</td>
| |
| <td align="center">43</td>
| |
| <td align="center">16</td>
| |
| <td align="center">4</td>
| |
| <td align="center">1</td>
| |
| </tr>
| |
| </table>
| |
| | |
| Two [[decision analysis]] studies<ref name="pmif12361816">{{cite journal | author = Smith K, Roberts M | title = Cost-effectiveness of newer treatment strategies for influenza. | journal = Am J Med | volume = 113 | issue = 4 | pages = 300-7 | year = 2002 | doi = 10.1016/S0002-9343(02)01222-6 | id = PMID 12361816}}</ref><ref name="pimd12965940">{{cite journal | author = Rothberg M, Bellantonio S, Rose D | title = Management of influenza in adults older than 65 years of age: cost-effectiveness of rapid testing and antiviral therapy. | journal = Ann Intern Med | volume = 139 | issue = 5 Pt 1 | pages = 321-9 | year = 2003 | url = http://www.annals.org/cgi/content/abstract/139/5_Part_1/321 | id = PMID 12965940}}</ref> suggest that ''during local outbreaks'' of influenza, the prevalence will be over 70%<ref name="pimd12965940"/> and thus patients with any of the above combinations of symptoms may be treated with neuramidase inhibitors without testing. Even in the absence of a local outbreak, treatment may be justified in the elderly during the influenza season as long as the prevalence is over 15%.<ref name="pimd12965940"/>
| |
| | |
| Most people who get influenza will recover in one to two weeks, but others will develop life-threatening complications (such as [[pneumonia]]). According to the [[World Health Organization]]: "Every winter, tens of millions of people get the flu. Most are home, sick and miserable, for about a week. Some—mostly the elderly—die. We know the world-wide death toll exceeds a few hundred thousand people a year, but even in developed countries the numbers are uncertain, because medical authorities don't usually verify who actually died of influenza and who died of a flu-like illness."<ref>Peter M. Sandman and Jody Lanard [http://www.paho.org/English/DD/PIN/Number22_article1a.htm "Bird Flu: Communicating the Risk"] 2005 ''Perspectives in Health Magazine'' Vol. 10 issue 2.</ref> Even healthy people can be affected, and serious problems from influenza can happen at any age. People over 50 years old, very young children and people of any age with chronic medical conditions, are more likely to get complications from influenza: such as pneumonia, [[bronchitis]], [[sinus]], and [[ear infection]]s.<ref name=CDCkeyfacts> [http://www.cdc.gov/flu/protect/keyfacts.htm Key Facts about Influenza (Flu) Vaccine] CDC publication. Published October 17, 2006. Accessed 18 Oct 2006.</ref>
| |
| | |
| The flu can worsen chronic health problems. People with emphysema, chronic bronchitis or asthma may experience shortness of breath while they have the flu, and influenza may cause worsening of [[coronary heart disease]] or [[congestive heart failure]].<ref>Angelo SJ, Marshall PS, Chrissoheris MP, Chaves AM. "Clinical characteristics associated with poor outcome in patients acutely infected with Influenza A." ''Conn Med.'' 2004 Apr;68(4):199–205. PMID 15095826</ref> [[Tobacco smoking|Smoking]] is another [[risk factor]] associated with more serious disease and increased mortality from influenza.<ref>{{cite journal | author = Murin S, Bilello K | title = Respiratory tract infections: another reason not to smoke. | journal = Cleve Clin J Med | volume = 72 | issue = 10 | pages = 916-20 | year = 2005 | id = PMID 16231688}}</ref>
| |
| | |
| ===Laboratory tests===
| |
| The available laboratory tests for influenza continue to improve. The United States [[Centers for Disease Control and Prevention]] (CDC) maintains an up-to-date summary of available laboratory tests.<ref>Centers for Disease Control and Prevention. [http://www.cdc.gov/flu/professionals/labdiagnosis.htm Lab Diagnosis of Influenza.] Accessed on January 1, 2007</ref> According to the CDC, rapid diagnostic tests have a sensitivity of 70–75% and specificity of 90–95% when compared with viral culture. These tests may be especially useful during the influenza season (prevalence=25%) but in the absence of a local outbreak, or peri-influenza season (prevalence=10%<ref name="pimd12965940"/>).
| |
| | |
| ==Epidemiology==
| |
| | |
| ===Seasonal variations===
| |
| {{further|[[Flu season]]}}
| |
| | |
| [[Image:H5n1 spread with regression.png|thumb|right|300px|Cumulative Confirmed Human Cases of H5N1.<ref name=WHOH5N1data>[http://www.who.int/csr/disease/avian_influenza/country/en/ WHO Confirmed Human Cases of H5N1] Data published by WHO Epidemic and Pandemic Alert and Response (EPR). Accessed 24 Oct. 2006</ref> The regression curve for deaths is shown extended through the end of November 2006.]]
| |
| | |
| Influenza reaches peak prevalence in winter, and because the Northern and Southern Hemisphere have winter at different times of the year, there are actually two different flu seasons each year. This is why the [[World Health Organization]] (assisted by the [[National Influenza Centers]]) makes recommendations for two different vaccine formulations every year; one for the Northern, and one for the Southern Hemisphere.<ref name= WHOrecommendation>[http://www.who.int/csr/disease/influenza/2007northreport.pdf Recommended composition of influenza virus vaccines for use in the 2006–2007 influenza season] WHO report 2006-02-14. Accessed [[19 October]] [[2006]].</ref>
| |
| | |
| It remains unclear why outbreaks of the flu occur seasonally rather than uniformly throughout the year. One possible explanation is that, because people are indoors more often during the winter, they are in close contact more often, and this promotes transmission from person to person. Another is that cold temperatures lead to drier air, which may dehydrate mucus, preventing the body from effectively expelling virus particles. The virus may also survive longer on exposed surfaces (doorknobs, countertops, etc.) in colder temperatures. Increased travel and visitation due to the Northern Hemisphere winter holiday season may also play a role.<ref name = "NPR2003-12-17">[http://www.npr.org/templates/story/story.php?storyId=1551913 Weather and the Flu Season] NPR Day to Day, [[December 17]] [[2003]]. Accessed, [[19 October]] [[2006]]</ref> However, seasonal changes in infection rates are also seen in tropical regions and these peaks of infection are seen mainly during the rainy season.<ref>Shek LP, Lee BW. "Epidemiology and seasonality of respiratory tract virus infections in the tropics." ''Paediatr Respir Rev.'' 2003 Jun;4(2):105–11. PMID 12758047</ref> Seasonal changes in contact rates from school-terms, which are a major factor in other childhood diseases such as [[measles]] and [[pertussis]], may also play a role in flu. A combination of these small seasonal effects may be amplified by "dynamical resonance" with the endogenous disease cycles.<ref>Dushoff J, Plotkin JB, Levin SA, Earn DJ. "Dynamical resonance can account for seasonality of influenza epidemics." ''Proc Natl Acad Sci U S A.'' [[30 November]][[2004]];101(48):16915–6. PMID 15557003</ref> [[H5N1]] exhibits seasonality in both humans and birds.<ref name=WHOH5N1data/>
| |
| | |
| An alternative hypothesis to explain seasonality in influenza infections is an effect of [[vitamin D]] levels on immunity to the virus.<ref>{{cite journal | last = Cannell | first = J | coauthors = Vieth R, Umhau J, Holick M, Grant W, Madronich S, Garland C, Giovannucci E | title = Epidemic influenza and vitamin D | journal = Epidemiol Infect | volume = 134 | issue = 6 | pages = 1129–40 | year = 2006 | id = PMID 16959053}}</ref> This idea was first proposed by Robert Edgar Hope-Simpson in 1965.<ref>{{cite journal | last = HOPE-SIMPSON | first = R | title = The nature of herpes zoster: a long-term study and a new hypothesis | journal = Proc R Soc Med | volume = 58 | issue = | pages = 9–20 | year = | id = PMID 14267505}}</ref> He proposed that the cause of influenza epidemics during winter may be connected to seasonal fluctuations of vitamin D, which is produced in the skin under the influence of solar (or artificial) [[ultraviolet|UV radiation]]. This could explain why influenza occurs mostly in winter and during the tropical rainy season, when people stay indoors, away from the sun, and their vitamin D levels fall. Furthermore, some studies have suggested that administering [[cod liver oil]], which contains large amounts of vitamin D, can reduce the incidence of respiratory tract infections.<ref name = "Linday2004">{{cite journal | last = Linday | first = L | coauthors = Shindledecker R, Tapia-Mendoza J, Dolitsky J | title = Effect of daily cod liver oil and a multivitamin-mineral supplement with selenium on upper respiratory tract pediatric visits by young, inner-city, Latino children: randomized pediatric sites | journal = Ann Otol Rhinol Laryngol | volume = 113 | issue = 11 | pages = 891–901 | year = 2004 | id = PMID 15562899}}</ref>
| |
| | |
| ===Epidemic and pandemic spread===
| |
| {{further|[[Flu pandemic]]}}
| |
| | |
| [[Image:Antigenic drift versus shift.png|thumb|right|400px|[[Antigenic drift]] creates influenza viruses with slightly-modified antigens, while [[antigenic shift]] generates viruses with entirely novel antigens.]]
| |
| | |
| [[Image:Influenza geneticshift.jpg|thumb|right|300px|How antigenic shift, or reassortment, can result in novel and highly pathogenic strains of human influenza]]
| |
| | |
| As influenza is caused by a variety of species and strains of [[virus]]es, in any given year some strains can die out while others create [[epidemic]]s while yet another strain can cause a [[pandemic]]. Typically, in a year's normal two [[flu season]]s (one per hemisphere) there are between three and five million cases of severe illness and up to 500,000 deaths worldwide, which by some definitions is a yearly influenza epidemic.<ref>[http://www.who.int/mediacentre/factsheets/fs211/en/ Influenza] WHO Fact sheet N°211 revised March 2003. Accessed [[22 October]] [[2006]]</ref> Although the incidence of influenza can vary widely between years, approximately 36,000 deaths and more than 200,000 hospitalizations are directly associated with influenza every year in America.<ref>{{cite journal | last = Thompson | first = W | coauthors = Shay D, Weintraub E, Brammer L, Cox N, Anderson L, Fukuda K | title = Mortality associated with influenza and respiratory syncytial virus in the United States | url=http://jama.ama-assn.org/cgi/content/full/289/2/179 | journal = JAMA | volume = 289 | issue = 2 | pages = 179–86 | year = 2003 | id = PMID 12517228}}</ref><ref>{{cite journal | last = Thompson | first = W | coauthors = Shay D, Weintraub E, Brammer L, Bridges C, Cox N, Fukuda K | title = Influenza-associated hospitalizations in the United States | url= http://jama.ama-assn.org/cgi/content/full/292/11/1333 | journal = JAMA | volume = 292 | issue = 11 | pages = 1333–40 | year = 2004 | id = PMID 15367555}}</ref><ref>[http://www.niaid.nih.gov/factsheets/flu.htm Flu factsheet] National Institute of Allergy and Infectious Diseases Accessed 22 Dec 2006</ref> Every ten to twenty years a pandemic occurs, which infects a large proportion of the world's population, and can kill tens of millions of people (see history section).
| |
| | |
| New influenza viruses are constantly being produced by [[mutation]] or by [[reassortment]].<ref name= hay/> Mutations can cause small changes in the hemagglutinin and neuraminidase [[antigen]]s on the surface of the virus. This is called [[antigenic drift]], which creates an increasing variety of strains over time until one of the variants eventually achieves higher [[fitness (biology)|fitness]], becomes dominant, and rapidly sweeps through the human population – often causing an epidemic.<ref>{{cite journal | author = | title = Long intervals of stasis punctuated by bursts of positive selection in the seasonal evolution of influenza A virus | journal = Biol Direct | volume = 1 | issue = 1 | pages = 34 | year = 2006 | id = PMID 17067369}}</ref> In contrast, when influenza viruses re-assort, they may acquire new antigens — for example by reassortment between avian strains and human strains; this is called antigenic shift. If a human influenza virus is produced with entirely novel antigens, everybody will be susceptible and the novel influenza will spread uncontrollably, causing a pandemic.<ref>{{cite journal | last = Parrish | first = C | coauthors = Kawaoka Y | title = The origins of new pandemic viruses: the acquisition of new host ranges by canine parvovirus and influenza A viruses | journal = Annual Rev Microbiol | volume = 59 | issue = | pages = 553–86 | year = | id = PMID 16153179}}</ref> In contrast to this model of pandemics based on antigenic drift and shift, an alternative approach has been proposed where the periodic pandemics are produced by interactions of a fixed set of viral strains with a human population with a constantly-changing set of immunities to different viral strains.<ref>{{cite journal |author=Recker M, Pybus OG, Nee S, Gupta S |title=The generation of influenza outbreaks by a network of host immune responses against a limited set of antigenic types |url=http://www.pnas.org/cgi/content/full/104/18/7711 |journal=Proc Natl Acad Sci U S A. |volume=104 |issue=18 |pages=7711–7716 |year=2007 |pmid=17460037}}</ref>
| |
| | |
| ==Prevention==
| |
| ===Vaccination and infection control===
| |
| {{further|[[Flu vaccine]]}}
| |
| [[Image:Vaccination.jpg|thumb|240px|left|U.S. Navy personnel receiving influenza vaccination]]
| |
| | |
| Vaccination against influenza with a [[flu vaccine]] is strongly recommended for high-risk groups, such as children and the elderly.
| |
| | |
| Flu vaccines can be produced in several ways; the most common method is to grow the virus in fertilised hen eggs. After purification, the virus is inactivated (for example, by treatment with detergent) to produce an inactivated-virus vaccine. Alternatively, the virus can be grown in eggs until it loses [[virulence]] and the avirulent virus given as a live vaccine.<ref name=Hilleman/> The effectiveness of these flu vaccines is variable. Due to the high mutation rate of the virus, a particular flu vaccine usually confers protection for no more than a few years. Every year, the [[World Health Organization]] predicts which strains of the virus are most likely to be circulating in the next year, allowing [[pharmaceutical company|pharmaceutical companies]] to develop vaccines that will provide the best immunity against these strains.<ref name= WHOrecommendation/> Vaccines have also been developed to protect poultry from [[avian influenza]]. These vaccines can be effective against multiple strains and are used either as part of a preventative strategy, or combined with culling in attempts to eradicate outbreaks.<ref>{{cite journal | last = Capua | first = I | coauthors = Alexander D | title = The challenge of avian influenza to the veterinary community. | url= http://taylorandfrancis.metapress.com/media/gmuaahtvwk6vweuhugdh/contributions/t/2/n/2/t2n2431j4u176p7g.pdf | journal = Avian Pathol | volume = 35 | issue = 3 | pages = 189–205 | year = 2006 | id = PMID 16753610}}</ref>
| |
| | |
| It is possible to get vaccinated and still get influenza. The vaccine is reformulated each season for a few specific flu strains, but cannot possibly include all the strains actively infecting people in the world for that season. It takes about six months for the manufacturers to formulate and produce the millions of doses required to deal with the seasonal epidemics; occasionally, a new or overlooked strain becomes prominent during that time and infects people although they have been vaccinated (as by the [[Fujian flu|H3N2 Fujian flu]] in the 2003–2004 flu season).<ref>{{cite journal | last = Holmes | first = E | coauthors = Ghedin E, Miller N, Taylor J, Bao Y, St George K, Grenfell B, Salzberg S, Fraser C, Lipman D, Taubenberger J | title = Whole-genome analysis of human influenza A virus reveals multiple persistent lineages and reassortment among recent H3N2 viruses | journal = PLoS Biol | volume = 3 | issue = 9 | pages = e300 | year = 2005 | id = PMID 16026181}}</ref> It is also possible to get infected just before vaccination and get sick with the very strain that the vaccine is supposed to prevent, as the vaccine takes about two weeks to become effective.<ref name=CDCkeyfacts/>
| |
| | |
| The 2006–2007 season is the first in which the CDC has recommended that children younger than 59 months receive the annual flu vaccine.<ref name=cdcreport> [http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5510a1.htm Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP)] CDC report (MMWR 2006 Jul 28;55(RR10):1–42) accessed 19 Oct 2006.</ref> Vaccines can cause the [[immune system]] to react as if the body were actually being infected, and general infection symptoms (many cold and flu symptoms are just general infection symptoms) can appear, though these symptoms are usually not as severe or long-lasting as influenza. The most dangerous side-effect is a severe [[allergy|allergic reaction]] to either the virus material itself, or residues from the hen eggs used to grow the influenza; however, these reactions are extremely rare.<ref>[http://www.cdc.gov/flu/about/qa/flushot.htm Questions & Answers: Flu Shot] CDC publication updated Jul 24, 2006. Accessed 19 Oct 06.</ref>
| |
| | |
| [[Influenza pandemic#Personal health and hygiene|Good personal health and hygiene habits]] are reasonably effective in avoiding and minimizing influenza. People who contract influenza are most infective between the second and third days after infection and infectivity lasts for around 10 days.<ref name=Carrat>{{cite journal |author=Carrat F, Luong J, Lao H, Sallé A, Lajaunie C, Wackernagel H |title=A 'small-world-like' model for comparing interventions aimed at preventing and controlling influenza pandemics |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=17059593 |journal=BMC Med |volume=4 |issue= |pages=26 |year= |pmid=17059593}}</ref> Children are notably more infectious than adults, and shed virus from just before they develop symptoms until 2 weeks after infection.<ref name=Carrat/><ref>{{cite journal |author=Mitamura K, Sugaya N |title=[Diagnosis and Treatment of influenza—clinical investigation on viral shedding in children with influenza] |journal=Uirusu |volume=56 |issue=1 |pages=109-16 |year=2006 |pmid=17038819}}</ref>
| |
| | |
| Since influenza spreads through [[particulate|aerosols]] and contact with contaminated surfaces, it is important to persuade people to cover their mouths while sneezing and to wash their hands regularly.<ref name=cdcreport/> Surface sanitizing is recommended in areas where influenza may be present on surfaces.<ref>{{cite journal |author=Hota B |title=Contamination, disinfection, and cross-colonization: are hospital surfaces reservoirs for nosocomial infection? |journal=Clin Infect Dis |volume=39 |issue=8 |pages=1182–9 |year=2004 |id=PMID 15486843}}</ref> [[Alcohol]] is an effective sanitizer against influenza viruses, while [[quaternary ammonium]] compounds can be used with alcohol, to increase the duration of the sanitizing action.<ref name=McDonnell>{{cite journal |author=McDonnell G, Russell A |title=Antiseptics and disinfectants: activity, action, and resistance |url=http://cmr.asm.org/cgi/content/full/12/1/147?view=long&pmid=9880479 |journal=Clin Microbiol Rev |volume=12 |issue=1 |pages=147-79 |year=1999 |id=PMID 9880479}}</ref> In hospitals, [[quaternary ammonium]] compounds and halogen-releasing agents such as [[sodium hypochlorite]] are commonly used to sanitize rooms or equipment that have been occupied by patients with influenza symptoms.<ref name=McDonnell/> During past pandemics, closing schools, churches and theaters slowed the spread of the virus but did not have a large effect on the overall death rate.<ref>{{cite journal |author=Hatchett RJ, Mecher CE, Lipsitch M |title=Public health interventions and epidemic intensity during the 1918 influenza pandemic |url=http://www.pnas.org/cgi/content/full/104/18/7582 |journal=Proc Natl Acad Sci U S A. |volume=104 |issue=18 |pages=7582–7587 |year=2007 |pmid=17416679}}</ref><ref>{{cite journal |author=Bootsma MC, Ferguson NM |title=The effect of public health measures on the 1918 influenza pandemic in U.S. cities |url=http://www.pnas.org/cgi/content/full/104/18/7588 |journal=Proc Natl Acad Sci U S A. |volume=104 |issue=18 |pages=7588–7593 |year=2007 |pmid=17416677}}</ref>
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| {{further|[[Influenza treatment]]}}
| | [[Influenza medical therapy|Medical Therapy]] | [[Influenza primary prevention|Primary Prevention]] | [[Influenza cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Influenza future or investigational therapies|Future or Investigational Therapies]] |
| | |
| People with the flu are advised to get plenty of rest, drink a lot of liquids, avoid using [[alcoholic beverage|alcohol]] and [[tobacco smoking|tobacco]] and, if necessary, take medications such as [[paracetamol]] (acetaminophen) to relieve the fever and muscle aches associated with the flu. Children and teenagers with flu symptoms (particularly fever) should avoid taking [[aspirin]] during an influenza infection (especially [[Influenzavirus B|influenza type B]]) because doing so can lead to [[Reye's syndrome]], a rare but potentially fatal disease of the [[liver]].<ref>{{cite journal | last = Glasgow | first = J | coauthors = Middleton B | title = Reye syndrome — insights on causation and prognosis | url=http://adc.bmjjournals.com/cgi/content/full/85/5/351 | journal = Arch Dis Child | volume = 85 | issue = 5 | pages = 351–3 | year = 2001 | id = PMID 11668090}}</ref> Since influenza is caused by a virus, [[antibiotic]]s have no effect on the infection; unless prescribed for [[secondary infection]]s such as [[bacterial pneumonia]], they may lead to resistant bacteria. Antiviral medication is sometimes effective, but viruses can develop resistance to the standard antiviral drugs.
| |
| | |
| The two classes of anti-virals are neuraminidase inhibitors and M2 inhibitors ([[adamantane]] derivatives). Neuraminidase inhibitors are currently preferred for flu virus infections. The CDC recommended against using M2 inhibitors during the 2005–06 influenza season.<ref>Centers for Disease Control and Prevention. [http://www.cdc.gov/flu/han011406.htm CDC Recommends against the Use of Amantadine and Rimantadine for the Treatment or Prophylaxis of Influenza in the United States during the 2005–06 Influenza Season.] [[January 14]], [[2006]]. Retrieved on [[2007-01-01]]</ref>
| |
| | |
| ===Neuraminidase inhibitors===
| |
| Antiviral drugs such as [[oseltamivir]] (trade name Tamiflu) and [[zanamivir]] (trade name Relenza) are [[neuraminidase inhibitor]]s that are designed to halt the spread of the virus in the body.<ref name= Neuraminidase_inhibitors>{{cite journal | last = Moscona | first = A | title = Neuraminidase inhibitors for influenza | url=http://content.nejm.org/cgi/content/full/353/13/1363 | journal = N Engl J Med | volume = 353 | issue = 13 | pages = 1363–73 | year = 2005 | id = PMID 16192481}}</ref> These drugs are often effective against both influenza A and B.<ref name=Stephenson/> The [[Cochrane Collaboration]] reviewed these drugs and concluded that they reduce symptoms and complications.<ref name="pmid16855962">{{cite journal | last = Jefferson | first = T | coauthors = Demicheli V, Di Pietrantonj C, Jones M, Rivetti D | title = Neuraminidase inhibitors for preventing and treating influenza in healthy adults | journal = Cochrane Database Syst Rev | volume = 3 | issue = | pages = CD001265 | year = | doi = 10.1002/14651858.CD001265.pub2 | id = PMID 16855962}}</ref> Different strains of influenza virus have differing degrees of resistance against these antivirals and it is impossible to predict what degree of resistance a future pandemic strain might have.<ref> {{cite journal | last = Webster | first = Robert G. | title = H5N1 Influenza — Continuing Evolution and Spread | url=http://content.nejm.org/cgi/content/full/355/21/2174 | journal = N Engl J Med | volume = 355 | issue = 21 | pages = 2174–77 | year = 2006 | id = PMID 16192481}}</ref>
| |
| | |
| ===M2 inhibitors (adamantanes) ===
| |
| The [[antiviral drug]]s [[amantadine]] and [[rimantadine]] are designed to block a viral [[ion channel]] and prevent the virus from infecting cells. These drugs are sometimes effective against influenza A if given early in the infection, but are always ineffective against influenza B.<ref name= Stephenson>{{cite journal | last = Stephenson | first = I | coauthors = Nicholson K | title = Chemotherapeutic control of influenza | url=http://jac.oxfordjournals.org/cgi/content/full/44/1/6 | journal = J Antimicrob Chemother | volume = 44 | issue = 1 | pages = 6–10 | year = 1999 | id = PMID 10459804}}</ref> Measured resistance to amantadine and rimantadine in American isolates of [[H3N2]] has increased to 91% in 2005.<ref>{{cite journal | author = | title = High levels of adamantane resistance among influenza A (H3N2) viruses and interim guidelines for use of antiviral agents — United States, 2005–06 influenza season | url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5502a7.htm | journal = MMWR Morb Mortal Wkly Rep | volume = 55 | issue = 2 | pages = 44–6 | year = 2006 | id = PMID 16424859}}</ref>
| |
| | |
| ==Research==
| |
| {{further|[[Influenza research]]}}
| |
| [[Image:Influenza research.jpg|thumb|220px|right|CDC scientist working on influenza under high bio-safety conditions]]
| |
|
| |
|
| Research on influenza includes studies on [[molecular virology]], how the virus produces disease ([[pathogenesis]]), host [[immune response]]s, [[genomics|viral genomics]], and how the virus spreads ([[epidemiology]]). These studies help in developing influenza countermeasures; for example, a better understanding of the body's immune response helps [[vaccine]] development, and a detailed picture of how influenza invades cells aids the development of antiviral drugs. One important basic research program is the [[Influenza Genome Sequencing Project]], which is creating a library of influenza sequences; this library should help clarify which factors make one strain more lethal than another, which genes most affect [[immunogenicity]], and how the virus [[evolution|evolves]] over time.<ref> [http://msc.tigr.org/infl_a_virus/index.shtml Influenza A Virus Genome Project] at The Institute of Genomic Research. Accessed 19 Oct 06</ref>
| | ==Case Studies== |
| | :[[Influenza case study one|Case #1]] |
|
| |
|
| Research into new vaccines is particularly important: as current vaccines are slow and expensive to produce and must be reformulated every year. The sequencing of the influenza genome and [[recombinant DNA]] technology may accelerate the generation of new vaccine strains by allowing scientists to substitute new antigens into a previously-developed vaccine strain.<ref>{{cite journal | author = Subbarao K, Katz J | title = Influenza vaccines generated by reverse genetics. | journal = Curr Top Microbiol Immunol | volume = 283 | issue = | pages = 313-42 | year = | id = PMID 15298174}}</ref> New technologies are also being developed to grow virus in [[cell culture]]; which promises higher yields, less cost, better quality and surge capacity.<ref>{{cite journal | author = Bardiya N, Bae J | title = Influenza vaccines: recent advances in production technologies. | url=http://www.springerlink.com/content/jdt26gc39v4bwk9q/ | journal = Appl Microbiol Biotechnol | volume = 67 | issue = 3 | pages = 299–305 | year = 2005 | id = PMID 15660212}}</ref> The U.S. government has purchased from [[Sanofi Pasteur]] and [[Chiron Corporation]] several million doses of vaccine meant to be used in case of an [[influenza pandemic]] of [[H5N1]] avian influenza and is conducting clinical trials with these vaccines.<ref> [http://www.nytimes.com/2006/03/30/health/30vaccine.html?_r=1&oref=slogin New York Times article ""Doubt Cast on Stockpile of a Vaccine for Bird Flu""] by Denise Grady. Published: March 30, 2006. Accessed 19 Oct 06</ref> The UK government is also stockpiling millions of antiviral drugs(tamiflu, oseltamivir, zanimivir) to give to its citizens in the event of an outbreak, the UK [[Health Protection Agency]] has also gathered a limited amount of HPAI H5N1 vaccines for experimental purposes.
| | ==Related Chapters== |
| | |
| ==Infection in other animals==
| |
| {{H5N1}}{{further|[[Influenzavirus A]], [[H5N1]] and [[Transmission and infection of H5N1]]}}
| |
| Influenza infects many animal species and transfer of viral strains between species can occur. Birds are thought to be the main [[host (biology)|animal reservoir]]s of influenza viruses.<ref>{{cite journal | author = Gorman O, Bean W, Kawaoka Y, Webster R | title = Evolution of the nucleoprotein gene of influenza A virus. | url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=2319644 | journal = J Virol | volume = 64 | issue = 4 | pages = 1487–97 | year = 1990 | id = PMID 2319644}}</ref> Sixteen forms of [[hemagglutinin]] and 9 forms of [[neuraminidase]] have been identified. All known subtypes (HxNy) are found in birds but many subtypes are endemic in humans, dogs, horses, and pigs; populations of camels, ferrets, cats, seals, mink, and whales also show evidence of prior infection or exposure to influenza.<ref name=webster/> Variants of flu virus are sometimes named according to the species the strain is endemic in or adapted to. The main variants named using this convention are: Bird flu, [[Human flu|Human Flu]], Swine Flu, Horse Flu and Dog Flu. (Cat flu generally refers to Feline viral rhinotracheitis or Feline calicivirus and not infection from an influenza virus.) In pigs, horses and dogs, influenza symptoms are similar to humans, with cough, fever and loss of appetite.<ref name=webster/> The frequency of animal diseases are not as well-studied as human infection, but an outbreak of influenza in harbour seals caused approximately 500 seal deaths off the New England coast in 1979–1980.<ref>{{cite journal | author = Hinshaw V, Bean W, Webster R, Rehg J, Fiorelli P, Early G, Geraci J, St Aubin D | title = Are seals frequently infected with avian influenza viruses? | url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=6471169 | journal = J Virol | volume = 51 | issue = 3 | pages = 863-5 | year = 1984 | id = PMID 6471169}}</ref> On the other hand, outbreaks in pigs are common and do not cause severe mortality.<ref name=webster/>
| |
| | |
| Flu symptoms in birds are variable and can be unspecific.<ref>{{cite journal | author = Elbers A, Koch G, Bouma A | title = Performance of clinical signs in poultry for the detection of outbreaks during the avian influenza A (H7N7) epidemic in The Netherlands in 2003. | journal = Avian Pathol | volume = 34 | issue = 3 | pages = 181-7 | year = 2005 | id = PMID 16191700}}</ref> The symptoms following infection with low-pathogenicity avian influenza may be as mild as ruffled feathers, a small reduction in egg production, or weight loss combined with minor respiratory disease.<ref>Capua I, Mutinelli F. "Low pathogenicity (LPAI) and highly pathogenic (HPAI) avian influenza in turkeys and chicken." In: Capua I, Mutinelli F. (eds.), A Colour Atlas and Text on Avian Influenza, Papi Editore, Bologna, 2001, pp. 13–20</ref> Since these mild symptoms can make diagnosis in the field difficult, tracking the spread of avian influenza requires laboratory testing of samples from infected birds. Some strains such as Asian [[H9N2]] are highly virulent to poultry, and may cause more extreme symptoms and significant mortality.<ref>{{cite journal | author = Bano S, Naeem K, Malik S | title = Evaluation of pathogenic potential of avian influenza virus serotype H9N2 in chickens. | journal = Avian Dis | volume = 47 | issue = 3 Suppl | pages = 817-22 | year = 2003 | id = PMID 14575070}}</ref> In its most highly pathogenic form, influenza in chickens and turkeys produces a sudden appearance of severe symptoms and almost 100% mortality within two days.<ref>{{cite journal | author = Swayne D, Suarez D | title = Highly pathogenic avian influenza. | journal = Rev Sci Tech | volume = 19 | issue = 2 | pages = 463-82 | year = 2000 | id = PMID 10935274}}</ref> As the virus spreads rapidly in the crowded conditions seen in the intensive farming of chickens and turkeys, these outbreaks can cause large economic losses to poultry farmers.
| |
| | |
| An avian-adapted, highly pathogenic strain of H5N1 (called HPAI A(H5N1), for "highly pathogenic avian influenza virus of type A of subtype H5N1") causes [[transmission and infection of H5N1|H5N1 flu]], commonly known as "avian influenza" or simply "bird flu", and is [[endemic (epidemiology)|endemic]] in many bird populations, especially in Southeast Asia. This Asian lineage strain of HPAI A(H5N1) is [[global spread of H5N1|spreading globally]]. It is [[epizootic]] (an epidemic in non-humans) and panzootic (a disease affecting animals of many species, especially over a wide area) killing tens of millions of birds and spurring the culling of hundreds of millions of other birds in an attempt to control its spread. Most references in the media to "bird flu" and most references to H5N1 are about this specific strain.<ref>{{cite journal | author = Li K, Guan Y, Wang J, Smith G, Xu K, Duan L, Rahardjo A, Puthavathana P, Buranathai C, Nguyen T, Estoepangestie A, Chaisingh A, Auewarakul P, Long H, Hanh N, Webby R, Poon L, Chen H, Shortridge K, Yuen K, Webster R, Peiris J | title = Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. | journal = Nature | volume = 430 | issue = 6996 | pages = 209-13 | year = 2004 | id = PMID 15241415}}</ref><ref>Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. [http://darwin.nap.edu/books/0309095042/html/116.html "The Threat of Pandemic Influenza: Are We Ready?" Workshop Summary] The National Academies Press (2005) "Today's Pandemic Threat: Genesis of a Highly Pathogenic and Potentially Pandemic H5N1 Influenza Virus in Eastern Asia", pages 116–130</ref>
| |
| | |
| At present, HPAI A(H5N1) is an avian disease and there is no evidence suggesting efficient human-to-human transmission of HPAI A(H5N1). In almost all cases, those infected have had extensive physical contact with infected birds.<ref>{{cite journal | author = Liu J | title = Avian influenza—a pandemic waiting to happen? | url=http://jmii.org/content/pdf/v39n1p4.pdf | journal = J Microbiol Immunol Infect | volume = 39 | issue = 1 | pages = 4–10 | year = 2006 | id = PMID 16440117}}</ref> In the future, H5N1 may mutate or reassort into a strain capable of efficient human-to-human transmission. Due to its high lethality and [[virulence]], its [[endemic (epidemiology)|endemic]] presence, and its large and increasing biological host reservoir, the H5N1 virus is the world's pandemic threat in the 2006–7 flu season, and billions of dollars are being raised and spent researching H5N1 and preparing for a potential [[influenza pandemic]].<ref name=Rosenthal> Rosenthal, E. and Bradsher, K. [http://www.nytimes.com/2006/03/16/business/16bird.html?_r=1&oref=slogin Is Business Ready for a Flu Pandemic?] The New York Times 16-03-2006 Accessed 17-04-2006</ref>
| |
| | |
| ==Economic impact==
| |
| {{further|[[Social impact of H5N1]]}}
| |
| Influenza produces [[variable cost|direct cost]]s due to lost [[productivity]] and associated medical treatment, as well as [[indirect costs]] of preventative measures. In the United States, influenza is responsible for a total cost of over $10 billion per year, while it has been estimated that a future pandemic could cause hundreds of billions of dollars in direct and indirect costs.<ref>[http://www.whitehouse.gov/homeland/pandemic-influenza.html Statement from President George W. Bush on Influenza] Accessed 26 Oct 2006</ref> However, the economic impact of past pandemics have not been intensively studied, and some authors have suggested that the [[Spanish flu|Spanish influenza]] actually had a positive long-term effect on per-capita income growth, despite a large reduction in the working population and severe short-term depressive effects.<ref>Brainerd, E. and M. Siegler (2003), “The Economic Effects of the 1918 Influenza Epidemic”, ''CEPR Discussion Paper'', no. 3791.</ref> Other studies have attempted to predict the costs of a pandemic as serious as the 1918 Spanish flu on the U.S. economy, where 30% of all workers became ill, and 2.5% were killed. A 30% sickness rate and a three-week length of illness would decrease [[gross domestic product]] by 5%. Additional costs would come from medical treatment of 18 million to 45 million people, and total economic costs would be approximately $700 billion.<ref>{{cite journal | author = Poland G | title = Vaccines against avian influenza—a race against time. | url=http://content.nejm.org/cgi/content/full/354/13/1411 | journal = N Engl J Med | volume = 354 | issue = 13 | pages = 1411–3 | year = 2006 | id = PMID 16571885}}</ref>
| |
| | |
| Preventative costs are also high. Governments worldwide have spent billions of U.S. dollars preparing and planning for a potential H5N1 avian influenza pandemic, with costs associated with purchasing drugs and vaccines as well as developing disaster drills and strategies for improved border controls.<ref name=Rosenthal/> On November 1 2005, President George W. Bush unveiled the National Strategy to Safeguard Against the Danger of Pandemic Influenza<ref>[http://www.whitehouse.gov/homeland/pandemic-influenza.html National Strategy for Pandemic Influenza] Whitehouse.gov Accessed 26 Oct 2006.</ref> backed by a request to Congress for $7.1 billion to begin implementing the plan.<ref>[http://usinfo.state.gov/gi/Archive/2005/Nov/01-432345.html Bush Outlines $7 Billion Pandemic Flu Preparedness Plan] State.gov. Accessed 26 Oct 2006</ref> Internationally, on January 18 2006 donor nations pledged US$2 billion to combat bird flu at the two-day International Pledging Conference on Avian and Human Influenza held in China.<ref>[http://www.ens-newswire.com/ens/jan2006/2006-01-18-02.asp Donor Nations Pledge $1.85 Billion to Combat Bird Flu] Newswire Accessed 26 Oct 2006.</ref>
| |
| | |
| Up to 2006, over ten billion dollars have been spent and over two hundred million birds have been killed to try to contain H5N1 avian influenza.<ref>[http://www.usaid.gov/about_usaid/acvfa/intro_ai.pdf Avian Influenza and its Global Implications] US AID. Accessed 26 Oct 2006.</ref> However, as these efforts have been largely ineffective at controlling the spread of the virus, other approaches are being tried: for example, the Vietnamese government in 2005 adopted a combination of mass poultry vaccination, disinfecting, culling, information campaigns and bans on live poultry in cities.<ref> [http://today.reuters.co.uk/news/newsArticle.aspx?type=worldNews&storyID=2006-04-28T080147Z_01_HAN5054_RTRUKOC_0_UK-BIRDFLU-VIETNAM.xml Reuters Vietnam to unveil advanced plan to fight bird flu] published on April 28, 2006. Accessed 26 Oct 2006</ref> As a result of such measures, the cost of poultry farming has increased, while the cost to consumers has gone down due to demand for poultry falling below supply. This has resulted in devastating losses for many farmers. Poor poultry farmers cannot afford mandated measures which keep their bird livestock from contact with wild birds (and other measures), thus risking losing their livelihood altogether. Multinational poultry farming is increasingly becoming unprofitable as H5N1 avian influenza becomes endemic in wild birds worldwide.<ref>[http://www.irinnews.org/report.asp?ReportID=52471 Poultry sector suffers despite absence of bird flu] UN Office for the Coordination of Humanitarian Affairs. Accessed 26 Oct 2006</ref> Financial ruin for poor poultry farmers, which can be as severe as threatening starvation, has caused some to commit [[suicide]] and many others to stop cooperating with efforts to deal with this virus – further increasing the human toll, the spread of the disease, and the chances of a pandemic mutation.<ref>[http://www.expressindia.com/fullstory.php?newsid=65957 Nine poultry farmers commit suicide in flu-hit India] Reuters. Published on April 12, 2006. Accessed 26 Oct 2006.</ref><ref>[http://www.nytimes.com/2006/04/14/world/africa/14egypt.html?_r=1&oref=slogin In the Nile Delta, Bird Flu Preys on Ignorance and Poverty] The New York Times. Published on April 13, 2006. Accessed 26 Oct 2006.</ref>
| |
| | |
| ==See also==
| |
|
| |
|
| <!-- Please do not add links already featured in the body of the article above --> | | <!-- Please do not add links already featured in the body of the article above --> |
| Line 231: |
Line 52: |
| *[[Center for Biologics Evaluation and Research]] | | *[[Center for Biologics Evaluation and Research]] |
| *[[H5N1 genetic structure]] | | *[[H5N1 genetic structure]] |
| | *[[ICEID]] |
| | *[[Influenza Genome Sequencing Project]] |
| | *[[Cytokine storm]] |
| | *[[International Partnership on Avian and Pandemic Influenza]] |
| | *[[National Influenza Centers]] |
| | *[[Pandemic Preparedness and Response Act]] |
| | *[[Global Alliance for Vaccines and Immunization]] |
| | *[[IFPMA]] International Federation of Pharmaceutical Manufacturers Associations |
| | *[[Reporting disease cases]] |
| | *[[Original antigenic sin]] |
| | *[[Center for Biologics Evaluation and Research]] |
| *[[ICEID]] | | *[[ICEID]] |
| *[[Influenza Genome Sequencing Project]] | | *[[Influenza Genome Sequencing Project]] |
| Line 239: |
Line 71: |
| </div> | | </div> |
|
| |
|
| ==References and notes== | | ==Further Readings== |
| {{reflist|2}} | | {| style=width:85%" |
|
| |
|
| ==Further reading==
| | | |
| {{Col-begin}} | | {{Col-begin}} |
| {{Col-1-of-2}} | | {{Col-1-of-2}} |
| Line 280: |
Line 112: |
| *[http://www.who.int/csr/resources/publications/influenza/WHO_CDS_EPR_GIP_2006_3C.pdf WHO's assessment of Flu Research] as of November 2006. | | *[http://www.who.int/csr/resources/publications/influenza/WHO_CDS_EPR_GIP_2006_3C.pdf WHO's assessment of Flu Research] as of November 2006. |
| {{Col-end}} | | {{Col-end}} |
| | |} |
|
| |
|
| ==External links== | | ==External Links== |
| *[http://www.cdc.gov/flu/ Info on influenza] at [[Centers for Disease Control and Prevention|CDC]] | | *[http://www.cdc.gov/flu/ Info on influenza] at [[Centers for Disease Control and Prevention|CDC]] |
| *[http://www.who.int/mediacentre/factsheets/fs211/en/index.html Fact Sheet] Overview of influenza at [[World Health Organization]] | | *[http://www.who.int/mediacentre/factsheets/fs211/en/index.html Fact Sheet] Overview of influenza at [[World Health Organization]] |
| *[http://www.nhsdirect.nhs.uk/en.aspx?articleId=163§ionId=1725 Health encyclopedia entry] at [[NHS Direct]]
| |
| *[http://www.biohealthbase.org/ BioHealthBase Bioinformatics Resource Center] Database of influenza sequences and related information.
| |
| *[http://www.medicinenet.com/influenza/article.htm Overview of influenza] at [[MedicineNet]]
| |
| *[http://digital.library.unt.edu/govdocs/crs/search.tkl?q=influenza&search_crit=subject&search=Search&date1=Anytime&date2=Anytime&type=form Congressional Research Service (CRS) Reports regarding Influenza] Law related government reports at [[University of North Texas]]
| |
| *[http://www.fluwikie.com/index.php?n=Geographic.Geographic Influenza Surveillance and Contingency Plans] (by Country/Region)
| |
| *[http://www.ncbi.nlm.nih.gov/ICTVdb/ICTVdB/46000000.htm Orthomyxoviridae] The Universal Virus Database of the [[International Committee on Taxonomy of Viruses]] | | *[http://www.ncbi.nlm.nih.gov/ICTVdb/ICTVdB/46000000.htm Orthomyxoviridae] The Universal Virus Database of the [[International Committee on Taxonomy of Viruses]] |
| *[http://www.ncbi.nlm.nih.gov/genomes/FLU/flubiology.html Influenza Virus Resource] from the [[National Center for Biotechnology Information|NCBI]] | | *[http://www.ncbi.nlm.nih.gov/genomes/FLU/flubiology.html Influenza Virus Resource] from the [[National Center for Biotechnology Information|NCBI]] |
| *[http://www.influenzaworld.com/portal/eipf/pb/t/iwc/home InfluenzaWorld] Resource for all influenza-related information.
| |
|
| |
|
| {{Influenza}}
| |
| {{Respiratory pathology}} | | {{Respiratory pathology}} |
| {{Viral diseases}} | | {{Viral diseases}} |
| {{Link FA|pt}}
| |
|
| |
|
| [[ar:فيروس إنفلونزا]] | | [[ar:فيروس إنفلونزا]] |
| Line 342: |
Line 167: |
| [[pl:Grypa]] | | [[pl:Grypa]] |
| [[tr:Grip]] | | [[tr:Grip]] |
| {{WikiDoc Help Menu}} | | {{WH}} |
| {{WikiDoc Sources}} | | {{WS}} |
|
| |
|
| [[Category:Disease]] | | [[Category:Disease]] |
| Line 349: |
Line 174: |
| [[Category:Pulmonology]] | | [[Category:Pulmonology]] |
| [[Category:Influenza| ]] | | [[Category:Influenza| ]] |
| [[Category:Infectious disease]]
| |