Hyperparathyroidism other imaging findings: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Imaging modalities may be helpful in preoperative localization of hyper-functioning parathyroid glands. This includes both non-invasive and invasive modalities. Non-invasive imaging modalities for preoperative localization of hyper-functioning parathyroid glands include Tc-99m sestamibi scintigraphy (sestamibi or MIBI), single | Imaging modalities may be helpful in preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]]. This includes both non-invasive and [[Invasive (medical)|invasive]] modalities. Non-invasive imaging modalities for preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]] include [[Tc-99m sestamibi scintigraphy]] ([[sestamibi]] or [[Sestamibi|MIBI]]), [[single photon emission computed tomography]] ([[Single photon emission computed tomography|SPECT]]), [[positron emission tomography]] ([[Positron emission tomography|PET]]). Invasive modalities used for preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]] include selective [[Angiogram|arteriography]] and [[Angiogram|angiography]]. [[Dual energy X-ray absorptiometry]] is helpful in detecting low [[bone mineral density]] (BMD) caused by hyperparathyroidism. | ||
==Other Imaging Findings== | ==Other Imaging Findings== | ||
Other imaging modalities are used for preoperative localization of hyper-functioning parathyroid glands. This includes both non-invasive and invasive modalities. Another modality used in hyperparathyroidism is dual energy X-ray | Other imaging modalities are used for preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]]. This includes both non-invasive and [[Invasive (medical)|invasive]] modalities. Another modality used in hyperparathyroidism is [[dual energy X-ray absorptiometry]] ([[DXA]]). [[Dual energy X-ray absorptiometry|DXA]] is helpful in detecting low [[bone mineral density]] (BMD) caused by hyperparathyroidism. | ||
===Non-invasive modalities=== | ===Non-invasive modalities=== | ||
====TC-99m Sestamibi Scintigraphy==== | ====TC-99m Sestamibi Scintigraphy==== | ||
*Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands.<ref name="pmid16150247">{{cite journal| author=Palestro CJ, Tomas MB, Tronco GG| title=Radionuclide imaging of the parathyroid glands. | journal=Semin Nucl Med | year= 2005 | volume= 35 | issue= 4 | pages= 266-76 | pmid=16150247 | doi=10.1053/j.semnuclmed.2005.06.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16150247 }} </ref> | *[[Technetium-99m]]-methoxyisobutylisonitrile ([[Tc-99m sestamibi scintigraphy|99mTc-sestamibi]] or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]].<ref name="pmid16150247">{{cite journal| author=Palestro CJ, Tomas MB, Tronco GG| title=Radionuclide imaging of the parathyroid glands. | journal=Semin Nucl Med | year= 2005 | volume= 35 | issue= 4 | pages= 266-76 | pmid=16150247 | doi=10.1053/j.semnuclmed.2005.06.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16150247 }} </ref> | ||
*Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity.<ref name="pmid11742331">{{cite journal| author=Hetrakul N, Civelek AC, Stagg CA, Udelsman R| title=In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria. | journal=Surgery | year= 2001 | volume= 130 | issue= 6 | pages= 1011-8 | pmid=11742331 | doi=10.1067/msy.2001.118371 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11742331 }} </ref> | *Most of the sestamibi is retained in [[Mitochondrion|mitochondria]] of [[thyroid]] and abnormal [[Parathyroid gland|parathyroid]] tissue and is a function of [[mitochondrial]] activity.<ref name="pmid11742331">{{cite journal| author=Hetrakul N, Civelek AC, Stagg CA, Udelsman R| title=In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria. | journal=Surgery | year= 2001 | volume= 130 | issue= 6 | pages= 1011-8 | pmid=11742331 | doi=10.1067/msy.2001.118371 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11742331 }} </ref> | ||
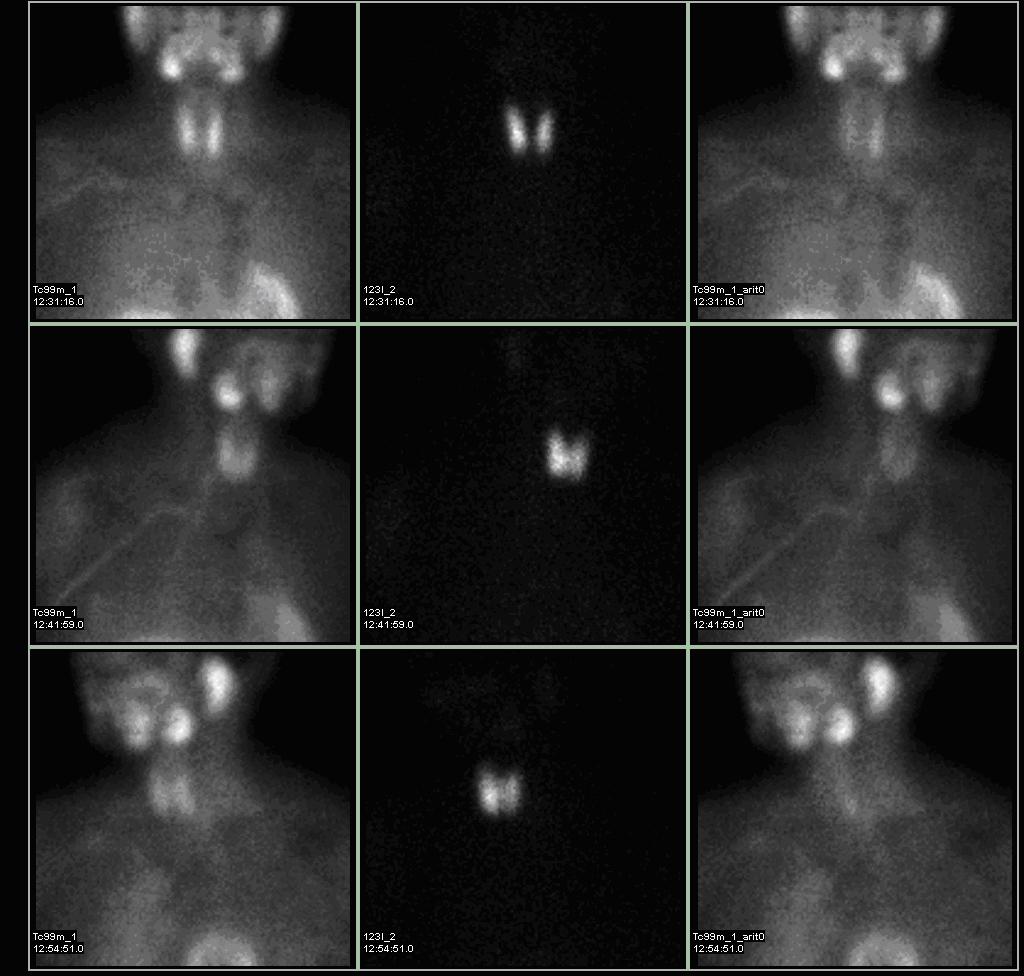
*The basis of | *Single-isotope, double-phase technique is used. The basis of "single-isotope, double-phase technique" is that [[sestamibi]] washes out of the [[thyroid]] more rapidly than from abnormal [[Parathyroid gland|parathyroid]] tissue.<ref name="pmid1328564">{{cite journal| author=Taillefer R, Boucher Y, Potvin C, Lambert R| title=Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study) | journal=J Nucl Med | year= 1992 | volume= 33 | issue= 10 | pages= 1801-7 | pmid=1328564 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1328564 }} </ref> | ||
*Multiple planar images are obtained, typically one shortly after injection of 99mTc-sestamibi and another after two hours to identify the | *Multiple planar images are obtained, typically one shortly after injection of 99mTc-sestamibi and another after two hours to identify the areas of retained [[sestamibi]] showing hyper-functioning [[Parathyroid gland|parathyroid]] tissue. | ||
*As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial.<ref name="pmid8288719">{{cite journal| author=Thulé P, Thakore K, Vansant J, McGarity W, Weber C, Phillips LS| title=Preoperative localization of parathyroid tissue with technetium-99m sestamibi 123I subtraction scanning. | journal=J Clin Endocrinol Metab | year= 1994 | volume= 78 | issue= 1 | pages= 77-82 | pmid=8288719 | doi=10.1210/jcem.78.1.8288719 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8288719 }} </ref> | *As all [[Parathyroid gland|parathyroid]] lesions does not retain [[sestamibi]] nor all [[thyroid]] tissue washes out quickly, subtraction imaging may be beneficial.<ref name="pmid8288719">{{cite journal| author=Thulé P, Thakore K, Vansant J, McGarity W, Weber C, Phillips LS| title=Preoperative localization of parathyroid tissue with technetium-99m sestamibi 123I subtraction scanning. | journal=J Clin Endocrinol Metab | year= 1994 | volume= 78 | issue= 1 | pages= 77-82 | pmid=8288719 | doi=10.1210/jcem.78.1.8288719 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8288719 }} </ref> | ||
*Subtraction technique uses dual contrast Tc-99m sestamibi along with iodine-123 or 99m-technicium pertechnetate which | *Subtraction technique uses dual contrast [[Tc-99m sestamibi scintigraphy|Tc-99m sestamibi]] along with iodine-123 or 99m-technicium pertechnetate, which are taken by [[thyroid tissue]] only. Iodine-123/99m-technicium pertechnetate images of [[thyroid]] are later digitally subtracted from Tc-99m sestamibi images leading to visualization of [[Parathyroid gland|parathyroid]] tissue only.<ref name="pmid25722888">{{cite journal| author=Ryhänen EM, Schildt J, Heiskanen I, Väisänen M, Ahonen A, Löyttyniemi E et al.| title=(99m)Technetium Sestamibi-(123)Iodine Scintigraphy Is More Accurate Than (99m)Technetium Sestamibi Alone before Surgery for Primary Hyperparathyroidism. | journal=Int J Mol Imaging | year= 2015 | volume= 2015 | issue= | pages= 391625 | pmid=25722888 | doi=10.1155/2015/391625 | pmc=4333274 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25722888 }} </ref> | ||
*Presence of solid thyroid nodule is the most common cause of false positive results. Other causes of false positive results may include thyroid carcinoma, lymphoma, and lymphadenopathy. | *Presence of solid [[thyroid nodule]] is the most common cause of [[false positive]] results. Other causes of [[false positive]] results may include [[thyroid carcinoma]], [[lymphoma]], and [[lymphadenopathy]]. | ||
*The sensitivity of sestamibi scintigraphy can be increased by using it concomitantly with neck ultrasound and/or SPECT. <ref name="pmid18794320">{{cite journal| author=Eslamy HK, Ziessman HA| title=Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. | journal=Radiographics | year= 2008 | volume= 28 | issue= 5 | pages= 1461-76 | pmid=18794320 | doi=10.1148/rg.285075055 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18794320 }} </ref><ref name="pmid12153604">{{cite journal| author=Haber RS, Kim CK, Inabnet WB| title=Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. | journal=Clin Endocrinol (Oxf) | year= 2002 | volume= 57 | issue= 2 | pages= 241-9 | pmid=12153604 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12153604 }} </ref> | *The [[sensitivity]] of [[sestamibi]] scintigraphy can be increased by using it concomitantly with neck [[ultrasound]] and/or [[Single photon emission computed tomography|SPECT]]. <ref name="pmid18794320">{{cite journal| author=Eslamy HK, Ziessman HA| title=Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. | journal=Radiographics | year= 2008 | volume= 28 | issue= 5 | pages= 1461-76 | pmid=18794320 | doi=10.1148/rg.285075055 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18794320 }} </ref><ref name="pmid12153604">{{cite journal| author=Haber RS, Kim CK, Inabnet WB| title=Ultrasonography for preoperative localization of enlarged [[parathyroid]] glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. | journal=Clin Endocrinol (Oxf) | year= 2002 | volume= 57 | issue= 2 | pages= 241-9 | pmid=12153604 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12153604 }} </ref> | ||
*The sensitivity of sestamibi scintigraphy is 80% - 90%.<ref name="pmid8678959">{{cite journal |vauthors=Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B |title=Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism |journal=World J Surg |volume=20 |issue=7 |pages=835–9; discussion 839–40 |year=1996 |pmid=8678959 |doi= |url=}}</ref><ref name="pmid17685957">{{cite journal |vauthors=Prasannan S, Davies G, Bochner M, Kollias J, Malycha P |title=Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi |journal=ANZ J Surg |volume=77 |issue=9 |pages=774–7 |year=2007 |pmid=17685957 |doi=10.1111/j.1445-2197.2007.04227.x |url=}}</ref><ref name="pmid20625763">{{cite journal |vauthors=Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A |title=Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism |journal=Langenbecks Arch Surg |volume=395 |issue=7 |pages=929–33 |year=2010 |pmid=20625763 |doi=10.1007/s00423-010-0680-8 |url=}}</ref> | *The sensitivity of [[sestamibi]] scintigraphy is 80% - 90%.<ref name="pmid8678959">{{cite journal |vauthors=Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B |title=Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism |journal=World J Surg |volume=20 |issue=7 |pages=835–9; discussion 839–40 |year=1996 |pmid=8678959 |doi= |url=}}</ref><ref name="pmid17685957">{{cite journal |vauthors=Prasannan S, Davies G, Bochner M, Kollias J, Malycha P |title=Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi |journal=ANZ J Surg |volume=77 |issue=9 |pages=774–7 |year=2007 |pmid=17685957 |doi=10.1111/j.1445-2197.2007.04227.x |url=}}</ref><ref name="pmid20625763">{{cite journal |vauthors=Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A |title=Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism |journal=Langenbecks Arch Surg |volume=395 |issue=7 |pages=929–33 |year=2010 |pmid=20625763 |doi=10.1007/s00423-010-0680-8 |url=}}</ref> | ||
{| | |||
! colspan="3" style="background: #4479BA; text-align: center;" |{{fontcolor|#FFF|Factors influencing sensitivity of Tc-99m sestamibi scintigraphy}} | |||
|- | |||
| colspan="2" style="background: #7d7d7d; text-align: center;" |{{fontcolor|#FFF|'''Factors'''}} | |||
| style="background: #7d7d7d; text-align: center;" |{{fontcolor|#FFF|'''Sensitivity'''}} | |||
|- | |||
| rowspan="4" style="background: #F0FFFF; text-align: center;" |'''Biochemical factors''' | |||
| style="background: #DCDCDC;" |High serum [[calcium]] level<ref name="pmid12769210">{{cite journal| author=Parikshak M, Castillo ED, Conrad MF, Talpos GB| title=Impact of [[hypercalcemia]] and [[parathyroid hormone]] level on the sensitivity of preoperative sestamibi scanning for primary hyperparathyroidism. | journal=Am Surg | year= 2003 | volume= 69 | issue= 5 | pages= 393-8; discussion 399 | pmid=12769210 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12769210 }} </ref> | |||
| style="background: #DCDCDC;" |Increased | |||
|- | |||
| style="background: #DCDCDC;" |High serum parathyroid hormone level<ref name="pmid12769210">{{cite journal| author=Parikshak M, Castillo ED, Conrad MF, Talpos GB| title=Impact of hypercalcemia and parathyroid hormone level on the sensitivity of preoperative sestamibi scanning for primary hyperparathyroidism. | journal=Am Surg | year= 2003 | volume= 69 | issue= 5 | pages= 393-8; discussion 399 | pmid=12769210 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12769210 }} </ref><ref name="pmid17053383">{{cite journal| author=Siegel A, Alvarado M, Barth RJ, Brady M, Lewis J| title=Parameters in the prediction of the sensitivity of parathyroid scanning. | journal=Clin Nucl Med | year= 2006 | volume= 31 | issue= 11 | pages= 679-82 | pmid=17053383 | doi=10.1097/01.rlu.0000242212.23936.a7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17053383 }} </ref> | |||
| style="background: #DCDCDC;" |Increased | |||
|- | |||
| style="background: #DCDCDC;" |Hypovitaminosis D <ref name="pmid18936353">{{cite journal| author=Kandil E, Tufaro AP, Carson KA, Lin F, Somervell H, Farrag T et al.| title=Correlation of plasma 25-hydroxyvitamin D levels with severity of primary hyperparathyroidism and likelihood of parathyroid adenoma localization on sestamibi scan. | journal=Arch Otolaryngol Head Neck Surg | year= 2008 | volume= 134 | issue= 10 | pages= 1071-5 | pmid=18936353 | doi=10.1001/archotol.134.10.1071 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18936353 }} </ref> | |||
(only in primary hyperparathyroidism) | |||
| style="background: #DCDCDC;" |Increased | |||
|- | |||
| style="background: #DCDCDC;" |[[Calcium channel blocker]] use<ref name="pmid15657576">{{cite journal| author=Friedman K, Somervell H, Patel P, Melton GB, Garrett-Mayer E, Dackiw AP et al.| title=Effect of calcium channel blockers on the sensitivity of preoperative 99mTc-MIBI SPECT for hyperparathyroidism. | journal=Surgery | year= 2004 | volume= 136 | issue= 6 | pages= 1199-204 | pmid=15657576 | doi=10.1016/j.surg.2004.06.047 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15657576 }} </ref> | |||
(only in primary hyperparathyroidism) | |||
| style="background: #DCDCDC;" |Decreased | |||
|- | |||
| rowspan="2" style="background: #F0FFFF; text-align: center;" |'''Gross and architectural factors''' | |||
| style="background: #DCDCDC;" |Size (Large)<ref name="pmid15967881">{{cite journal| author=Mehta NY, Ruda JM, Kapadia S, Boyer PJ, Hollenbeak CS, Stack BC| title=Relationship of technetium Tc 99m sestamibi scans to histopathological features of hyperfunctioning parathyroid tissue. | journal=Arch Otolaryngol Head Neck Surg | year= 2005 | volume= 131 | issue= 6 | pages= 493-8 | pmid=15967881 | doi=10.1001/archotol.131.6.493 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15967881 }} </ref><ref name="pmid10565772">{{cite journal| author=Takebayashi S, Hidai H, Chiba T, Takagi Y, Nagatani Y, Matsubara S| title=Hyperfunctional parathyroid glands with 99mTc-MIBI scan: semiquantitative analysis correlated with histologic findings. | journal=J Nucl Med | year= 1999 | volume= 40 | issue= 11 | pages= 1792-7 | pmid=10565772 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10565772 }} </ref> | |||
| style="background: #DCDCDC;" |Increased | |||
|- | |||
| style="background: #DCDCDC;" |Multi-glandular disease<ref name="pmid14585407">{{cite journal| author=Haciyanli M, Lal G, Morita E, Duh QY, Kebebew E, Clark OH| title=Accuracy of preoperative localization studies and intraoperative [[parathyroid hormone]] assay in patients with primary hyperparathyroidism and double [[adenoma]]. | journal=J Am Coll Surg | year= 2003 | volume= 197 | issue= 5 | pages= 739-46 | pmid=14585407 | doi=10.1016/S1072-7515(03)00676-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14585407 }} </ref> | |||
| style="background: #DCDCDC;" |Decreased | |||
|- | |||
| style="background: #F0FFFF; text-align: center;" |'''Cytological factors''' | |||
| style="background: #DCDCDC;" |Increased amount of cellular content<ref name="pmid15967881">{{cite journal| author=Mehta NY, Ruda JM, Kapadia S, Boyer PJ, Hollenbeak CS, Stack BC| title=Relationship of technetium Tc 99m sestamibi scans to histopathological features of hyperfunctioning parathyroid tissue. | journal=Arch Otolaryngol Head Neck Surg | year= 2005 | volume= 131 | issue= 6 | pages= 493-8 | pmid=15967881 | doi=10.1001/archotol.131.6.493 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15967881 }} </ref><ref name="pmid10565772">{{cite journal| author=Takebayashi S, Hidai H, Chiba T, Takagi Y, Nagatani Y, Matsubara S| title=Hyperfunctional parathyroid glands with 99mTc-MIBI scan: semiquantitative analysis correlated with histologic findings. | journal=J Nucl Med | year= 1999 | volume= 40 | issue= 11 | pages= 1792-7 | pmid=10565772 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10565772 }} </ref> | |||
(Chief cells and oxyphil cells) | |||
| style="background: #DCDCDC;" |Increased | |||
|- | |||
| style="background: #F0FFFF; text-align: center;" |'''Immunohistochemical factors''' | |||
| style="background: #DCDCDC;" |Increased P-glycoprotien expression<ref name="pmid17929232">{{cite journal| author=Gupta Y, Ahmed R, Happerfield L, Pinder SE, Balan KK, Wishart GC| title=P-glycoprotein expression is associated with sestamibi washout in primary hyperparathyroidism. | journal=Br J Surg | year= 2007 | volume= 94 | issue= 12 | pages= 1491-5 | pmid=17929232 | doi=10.1002/bjs.5882 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17929232 }} </ref> | |||
| style="background: #DCDCDC;" |Decreased | |||
|- | |||
| colspan="3" style="background: #F0FFFF;" |'''Note:''' P-glycoprotein (Pgp) is a plasma membrane protein encoded by mammalian multidrug resistance gene (MDRI). Many drugs that are lipophilic and cationic at physiological pH interact with P-gp. Sestamibi is a lipophilic cationic on physioligical pH. P-gp acts as ATP-dependent efflux pump and prevents accumulation of sestamibi in parathyroid tissue. So, the uptake of sestamibi into parathyroid adenoma cells depends on the activity of the P-gp<ref name="pmid8094997">{{cite journal| author=Piwnica-Worms D, Chiu ML, Budding M, Kronauge JF, Kramer RA, Croop JM| title=Functional imaging of multidrug-resistant P-glycoprotein with an organotechnetium complex. | journal=Cancer Res | year= 1993 | volume= 53 | issue= 5 | pages= 977-84 | pmid=8094997 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8094997 }} </ref>. | |||
|} | |||
{| | {| | ||
| | | | ||
| Line 28: | Line 69: | ||
|} | |} | ||
====Single | ====Single photon emission computed tomography (SPECT)==== | ||
*Single | *[[Single photon emission computed tomography]] may be used along with [[Tc-99m sestamibi scintigraphy]] for preoperative evaluation of hyper-functioning [[Parathyroid gland|parathyroid]] gland.<ref name="pmid8917173">{{cite journal| author=Billotey C, Sarfati E, Aurengo A, Duet M, Mündler O, Toubert ME et al.| title=Advantages of SPECT in technetium-99m-sestamibi parathyroid scintigraphy. | journal=J Nucl Med | year= 1996 | volume= 37 | issue= 11 | pages= 1773-8 | pmid=8917173 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8917173 }} </ref><ref name="pmid11854692">{{cite journal| author=Civelek AC, Ozalp E, Donovan P, Udelsman R| title=Prospective evaluation of delayed technetium-99m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism. | journal=Surgery | year= 2002 | volume= 131 | issue= 2 | pages= 149-57 | pmid=11854692 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11854692 }} </ref> | ||
*Sestamibi-SPECT is also called pinhone-SPECT (P-SPECT). P-SPECT uses cone beam collimator in contrast to parallel-hole collimator used in SPECT. cone bean collimator possess more suitable geometric properties leading to high spatial resolution.<ref name="pmid8306288">{{cite journal| author=Strand SE, Ivanovic M, Erlandsson K, Franceschi D, Button T, Sjögren K et al.| title=Small animal imaging with pinhole single-photon emission computed tomography. | journal=Cancer | year= 1994 | volume= 73 | issue= 3 Suppl | pages= 981-4 | pmid=8306288 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8306288 }} </ref><ref name="pmid15551591">{{cite journal| author=Jaszczak RJ, Li J, Wang H, Zalutsky MR, Coleman RE| title=Pinhole collimation for ultra-high-resolution, small-field-of-view SPECT. | journal=Phys Med Biol | year= 1994 | volume= 39 | issue= 3 | pages= 425-37 | pmid=15551591 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15551591 }} </ref> | *Sestamibi-SPECT is also called pinhone-SPECT (P-SPECT). P-SPECT uses cone beam collimator in contrast to parallel-hole collimator used in [[Single photon emission computed tomography|SPECT]]. cone bean collimator possess more suitable geometric properties leading to high spatial resolution.<ref name="pmid8306288">{{cite journal| author=Strand SE, Ivanovic M, Erlandsson K, Franceschi D, Button T, Sjögren K et al.| title=Small animal imaging with pinhole single-photon emission computed tomography. | journal=Cancer | year= 1994 | volume= 73 | issue= 3 Suppl | pages= 981-4 | pmid=8306288 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8306288 }} </ref><ref name="pmid15551591">{{cite journal| author=Jaszczak RJ, Li J, Wang H, Zalutsky MR, Coleman RE| title=Pinhole collimation for ultra-high-resolution, small-field-of-view SPECT. | journal=Phys Med Biol | year= 1994 | volume= 39 | issue= 3 | pages= 425-37 | pmid=15551591 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15551591 }} </ref> | ||
*Using SPECT with sestamibi scintigraphy improves detection and localization of hyper-functioning parathyroid gland.<ref name="pmid15078713">{{cite journal| author=Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M| title=Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy. | journal=Arch Surg | year= 2004 | volume= 139 | issue= 4 | pages= 433-7 | pmid=15078713 | doi=10.1001/archsurg.139.4.433 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15078713 }} </ref><ref name="pmid8816526">{{cite journal| author=Perez-Monte JE, Brown ML, Shah AN, Ranger NT, Watson CG, Carty SE et al.| title=Parathyroid adenomas: accurate detection and localization with Tc-99m sestamibi SPECT. | journal=Radiology | year= 1996 | volume= 201 | issue= 1 | pages= 85-91 | pmid=8816526 | doi=10.1148/radiology.201.1.8816526 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8816526 }} </ref> | *Using [[Single photon emission computed tomography|SPECT]] with [[sestamibi]] scintigraphy improves detection and localization of hyper-functioning [[parathyroid gland]].<ref name="pmid15078713">{{cite journal| author=Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M| title=Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy. | journal=Arch Surg | year= 2004 | volume= 139 | issue= 4 | pages= 433-7 | pmid=15078713 | doi=10.1001/archsurg.139.4.433 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15078713 }} </ref><ref name="pmid8816526">{{cite journal| author=Perez-Monte JE, Brown ML, Shah AN, Ranger NT, Watson CG, Carty SE et al.| title=Parathyroid adenomas: accurate detection and localization with Tc-99m sestamibi SPECT. | journal=Radiology | year= 1996 | volume= 201 | issue= 1 | pages= 85-91 | pmid=8816526 | doi=10.1148/radiology.201.1.8816526 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8816526 }} </ref> | ||
*SPECT provides more precise result of sestamibi scitigraphy allowing surgeon to choose best route for surgical intervention. | *P-SPECT provides more precise result of [[sestamibi]] scitigraphy allowing surgeon to choose best route for surgical intervention. | ||
*P-SPECT may detect glands not visible on planer images leading to increased sensitivity. It is very useful in case of uncertain result from conventional sestamibi scitigraphy.<ref name="pmid14734671">{{cite journal| author=Spanu A, Falchi A, Manca A, Marongiu P, Cossu A, Pisu N et al.| title=The usefulness of neck pinhole SPECT as a complementary tool to planar scintigraphy in primary and secondary hyperparathyroidism. | journal=J Nucl Med | year= 2004 | volume= 45 | issue= 1 | pages= 40-8 | pmid=14734671 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14734671 }} </ref><ref name="pmid17960377">{{cite journal |vauthors=Carlier T, Oudoux A, Mirallié E, Seret A, Daumy I, Leux C, Bodet-Milin C, Kraeber-Bodéré F, Ansquer C |title=99mTc-MIBI pinhole SPECT in primary hyperparathyroidism: comparison with conventional SPECT, planar scintigraphy and ultrasonography |journal=Eur. J. Nucl. Med. Mol. Imaging |volume=35 |issue=3 |pages=637–43 |year=2008 |pmid=17960377 |pmc=2964350 |doi=10.1007/s00259-007-0625-9 |url=}}</ref> | *P-SPECT may detect glands not visible on planer images leading to increased [[sensitivity]]. It is very useful in case of uncertain result from conventional [[sestamibi]] scitigraphy.<ref name="pmid14734671">{{cite journal| author=Spanu A, Falchi A, Manca A, Marongiu P, Cossu A, Pisu N et al.| title=The usefulness of neck pinhole SPECT as a complementary tool to planar scintigraphy in primary and secondary hyperparathyroidism. | journal=J Nucl Med | year= 2004 | volume= 45 | issue= 1 | pages= 40-8 | pmid=14734671 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14734671 }} </ref><ref name="pmid17960377">{{cite journal |vauthors=Carlier T, Oudoux A, Mirallié E, Seret A, Daumy I, Leux C, Bodet-Milin C, Kraeber-Bodéré F, Ansquer C |title=99mTc-MIBI pinhole SPECT in primary hyperparathyroidism: comparison with conventional SPECT, planar scintigraphy and ultrasonography |journal=Eur. J. Nucl. Med. Mol. Imaging |volume=35 |issue=3 |pages=637–43 |year=2008 |pmid=17960377 |pmc=2964350 |doi=10.1007/s00259-007-0625-9 |url=}}</ref> | ||
*P-SPECT also enables accurate interpretation sestamibi uptake in upper mediastinum leading to a higher specificity. | *P-SPECT also enables accurate interpretation [[sestamibi]] uptake in upper [[mediastinum]] leading to a higher [[specificity]]. | ||
*In difficult cases, P-SPECT may also be adjuncted with subtraction Tc-99m sestamibi and I-123 scintigraphy or positron emission tomography.<ref name="pmid10336191">{{cite journal| author=Nguyen BD| title=Parathyroid imaging with Tc-99m sestamibi planar and SPECT scintigraphy. | journal=Radiographics | year= 1999 | volume= 19 | issue= 3 | pages= 601-14; discussion 615-6 | pmid=10336191 | doi=10.1148/radiographics.19.3.g99ma10601 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10336191 }} </ref> | *In difficult cases, P-SPECT may also be adjuncted with subtraction [[Sestamibi scan|Tc-99m sestamibi]] and I-123 scintigraphy or [[positron emission tomography]].<ref name="pmid10336191">{{cite journal| author=Nguyen BD| title=Parathyroid imaging with Tc-99m sestamibi planar and SPECT scintigraphy. | journal=Radiographics | year= 1999 | volume= 19 | issue= 3 | pages= 601-14; discussion 615-6 | pmid=10336191 | doi=10.1148/radiographics.19.3.g99ma10601 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10336191 }} </ref> | ||
*P-SPECT is approximately 84% sensitive, 91% specific with positive predictive value of around 91% and negative predictive value of around 84%.<ref name="pmid19578871">{{cite journal |vauthors=Lindqvist V, Jacobsson H, Chandanos E, Bäckdahl M, Kjellman M, Wallin G |title=Preoperative 99Tc(m)-sestamibi scintigraphy with SPECT localizes most pathologic parathyroid glands |journal=Langenbecks Arch Surg |volume=394 |issue=5 |pages=811–5 |year=2009 |pmid=19578871 |doi=10.1007/s00423-009-0536-2 |url=}}</ref> | *P-SPECT is approximately 84% [[Sensitivity|sensitive]], 91% [[Specificity|specific]] with [[positive predictive value]] of around 91% and [[negative predictive value]] of around 84%.<ref name="pmid19578871">{{cite journal |vauthors=Lindqvist V, Jacobsson H, Chandanos E, Bäckdahl M, Kjellman M, Wallin G |title=Preoperative 99Tc(m)-sestamibi scintigraphy with SPECT localizes most pathologic parathyroid glands |journal=Langenbecks Arch Surg |volume=394 |issue=5 |pages=811–5 |year=2009 |pmid=19578871 |doi=10.1007/s00423-009-0536-2 |url=}}</ref> | ||
*Fusion images of CT-MIBI-SPECT is superior to CT or MIBI-SPECT alone in preoperative localization of hyper-functioning parathyroid gland.<ref name="pmid19705144">{{cite journal| author=Wimmer G, Profanter C, Kovacs P, Sieb M, Gabriel M, Putzer D et al.| title=CT-MIBI-SPECT image fusion predicts multiglandular disease in hyperparathyroidism. | journal=Langenbecks Arch Surg | year= 2010 | volume= 395 | issue= 1 | pages= 73-80 | pmid=19705144 | doi=10.1007/s00423-009-0545-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19705144 }} </ref> | *Fusion images of CT-MIBI-SPECT is superior to [[Computed tomography|CT scan]] or MIBI-SPECT alone in preoperative localization of hyper-functioning [[parathyroid gland]].<ref name="pmid19705144">{{cite journal| author=Wimmer G, Profanter C, Kovacs P, Sieb M, Gabriel M, Putzer D et al.| title=CT-MIBI-SPECT image fusion predicts multiglandular disease in hyperparathyroidism. | journal=Langenbecks Arch Surg | year= 2010 | volume= 395 | issue= 1 | pages= 73-80 | pmid=19705144 | doi=10.1007/s00423-009-0545-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19705144 }} </ref> | ||
====Positron Emission Tomography (PET)==== | ====Positron Emission Tomography (PET)==== | ||
*11C-methionine PET along with CT scan (MET-PET/CT) may be used for preoperative localization of hyper-functioning gland.<ref name="pmid18781582">{{cite journal| author=Tang BN, Moreno-Reyes R, Blocklet D, Corvilain B, Cappello M, Delpierre I et al.| title=Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT. | journal=Contrast Media Mol Imaging | year= 2008 | volume= 3 | issue= 4 | pages= 157-63 | pmid=18781582 | doi=10.1002/cmmi.243 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18781582 }} </ref><ref name="pmid23478517">{{cite journal| author=Weber T, Maier-Funk C, Ohlhauser D, Hillenbrand A, Cammerer G, Barth TF et al.| title=Accurate preoperative localization of parathyroid adenomas with C-11 methionine PET/CT. | journal=Ann Surg | year= 2013 | volume= 257 | issue= 6 | pages= 1124-8 | pmid=23478517 | doi=10.1097/SLA.0b013e318289b345 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23478517 }} </ref> | *11C-methionine [[Positron emission tomography|PET]] along with [[Computed tomography|CT scan]] (MET-PET/CT) may be used for preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]].<ref name="pmid18781582">{{cite journal| author=Tang BN, Moreno-Reyes R, Blocklet D, Corvilain B, Cappello M, Delpierre I et al.| title=Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT. | journal=Contrast Media Mol Imaging | year= 2008 | volume= 3 | issue= 4 | pages= 157-63 | pmid=18781582 | doi=10.1002/cmmi.243 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18781582 }} </ref><ref name="pmid23478517">{{cite journal| author=Weber T, Maier-Funk C, Ohlhauser D, Hillenbrand A, Cammerer G, Barth TF et al.| title=Accurate preoperative localization of parathyroid adenomas with C-11 methionine PET/CT. | journal=Ann Surg | year= 2013 | volume= 257 | issue= 6 | pages= 1124-8 | pmid=23478517 | doi=10.1097/SLA.0b013e318289b345 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23478517 }} </ref> | ||
*MET-PET/CT may be used as an complimentary imaging modality for localizing hyper-functioning parathyroid glands in patients with negative Tc-99m sestamibi scintigraphy/SPECT results.<ref name="pmid25029418">{{cite journal| author=Traub-Weidinger T, Mayerhoefer ME, Koperek O, Mitterhauser M, Duan H, Karanikas G et al.| title=11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery. | journal=J Clin Endocrinol Metab | year= 2014 | volume= 99 | issue= 11 | pages= 4199-205 | pmid=25029418 | doi=10.1210/jc.2014-1267 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25029418 }} </ref> | *MET-PET/CT may be used as an complimentary imaging modality for localizing hyper-functioning parathyroid glands in patients with negative [[Tc-99m sestamibi scintigraphy]]/[[Single photon emission computed tomography|SPECT]] results.<ref name="pmid25029418">{{cite journal| author=Traub-Weidinger T, Mayerhoefer ME, Koperek O, Mitterhauser M, Duan H, Karanikas G et al.| title=11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery. | journal=J Clin Endocrinol Metab | year= 2014 | volume= 99 | issue= 11 | pages= 4199-205 | pmid=25029418 | doi=10.1210/jc.2014-1267 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25029418 }} </ref> | ||
===Invasive modalities=== | ===Invasive modalities=== | ||
====Selective arteriography==== | ====Selective arteriography==== | ||
*Selective transarterial hypocalcemic stimulation is combined with nonselective venous sampling to perform selective arteriography.<ref name="pmid19958942">{{cite journal| author=Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, Pingpank JF et al.| title=Reoperation for parathyroid adenoma: a contemporary experience. | journal=Surgery | year= 2009 | volume= 146 | issue= 6 | pages= 1144-55 | pmid=19958942 | doi=10.1016/j.surg.2009.09.015 | pmc=3467310 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19958942 }} </ref> | *Selective transarterial [[Hypocalcemia|hypocalcemic]] stimulation is combined with nonselective [[venous]] sampling to perform selective [[arteriography]].<ref name="pmid19958942">{{cite journal| author=Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, Pingpank JF et al.| title=Reoperation for parathyroid adenoma: a contemporary experience. | journal=Surgery | year= 2009 | volume= 146 | issue= 6 | pages= 1144-55 | pmid=19958942 | doi=10.1016/j.surg.2009.09.015 | pmc=3467310 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19958942 }} </ref> | ||
*Sodium citrate is injected to induce hypocalcemia. Simultaneous arteriography is performed. | *[[Sodium citrate]] is injected to induce [[hypocalcemia]]. Simultaneous [[arteriography]] is performed. | ||
*Samples are taken for superior vena cava at basaeline and timed intervals (20 sec, 40 sec, and 60 sec). | *Samples are taken for [[superior vena cava]] at basaeline and timed intervals (20 sec, 40 sec, and 60 sec). | ||
*An increase in the parathyroid hormone level to 1.4 times above the baseline or a clear blush observed on arteriography is considered as positive localization. | *An increase in the [[parathyroid hormone]] level to 1.4 times above the baseline or a clear blush observed on [[Angiogram|arteriography]] is considered as positive localization. | ||
* Arterial stimulation venous sampling is performed simultaneously with arteriogram due to similarly high PPV. | * Arterial stimulation venous sampling is performed simultaneously with arteriogram due to similarly high PPV. | ||
====Angiography==== | ====Angiography==== | ||
*Superselective arterial digital subtraction angiography (DSA) and superselective conventional angiography (CA) may be used for preoperative localization of hyper-functioning parathyroid glands in which noninvasive imaging modalities are negative or inconclusive.<ref name="pmid2644666">{{cite journal| author=Miller DL, Chang R, Doppman JL, Norton JA| title=Localization of parathyroid adenomas: superselective arterial DSA versus superselective conventional angiography. | journal=Radiology | year= 1989 | volume= 170 | issue= 3 Pt 2 | pages= 1003-6 | pmid=2644666 | doi=10.1148/radiology.170.3.2644666 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2644666 }} </ref> | *Superselective arterial [[digital subtraction angiography]] (DSA) and superselective conventional [[Angiogram|angiography]] (CA) may be used for preoperative localization of hyper-functioning [[Parathyroid gland|parathyroid glands]] in which noninvasive imaging modalities are negative or inconclusive.<ref name="pmid2644666">{{cite journal| author=Miller DL, Chang R, Doppman JL, Norton JA| title=Localization of parathyroid adenomas: superselective arterial DSA versus superselective conventional angiography. | journal=Radiology | year= 1989 | volume= 170 | issue= 3 Pt 2 | pages= 1003-6 | pmid=2644666 | doi=10.1148/radiology.170.3.2644666 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2644666 }} </ref> | ||
*Sensitivity of superselective digital subtraction angiography appears to be similar to conventional angiography. | *Sensitivity of superselective [[digital subtraction angiography]] appears to be similar to conventional [[Angiogram|angiography]]. | ||
*Superselective arterial digital subtraction angiography may be more sensitive than conventional angiography for preoperative localization of mediastinal hyper-functioning parathyroid glands. | *Superselective arterial [[digital subtraction angiography]] may be more sensitive than conventional [[Angiogram|angiography]] for preoperative localization of [[mediastinal]] hyper-functioning [[Parathyroid gland|parathyroid glands]]. | ||
===Dual Energy X-ray Absorptiometry=== | ===Dual Energy X-ray Absorptiometry (DXA)=== | ||
*Low bone mineral density (BMD) is caused by primary hyperparathyroidism. Distal forearm is affected most commonly. | *Low [[bone mineral density]] (BMD) is caused by primary hyperparathyroidism. Distal forearm is affected most commonly. | ||
*DXA of distal forearm should be done in all patients of primary hyperparathyroidism. | *[[Dual energy X-ray absorptiometry|DXA]] of distal forearm should be done in all patients of primary hyperparathyroidism. Very low T-score of distal forearm is observed in patients with primary hyperparathyroidism.<ref name="pmid22258698">{{cite journal| author=Wood K, Dhital S, Chen H, Sippel RS| title=What is the utility of distal forearm DXA in primary hyperparathyroidism? | journal=Oncologist | year= 2012 | volume= 17 | issue= 3 | pages= 322-5 | pmid=22258698 | doi=10.1634/theoncologist.2011-0285 | pmc=3316917 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22258698 }} </ref> | ||
==References== | ==References== | ||
| Line 66: | Line 107: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
| |||
[[Category:Disease]] | |||
[[Category:Medicine]] | |||
[[Category:Endocrinology]] | |||
[[Category:Parathyroid disorders]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Radiology]] | |||
Latest revision as of 22:16, 29 July 2020
|
Hyperparathyroidism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hyperparathyroidism other imaging findings On the Web |
|
American Roentgen Ray Society Images of Hyperparathyroidism other imaging findings |
|
Risk calculators and risk factors for Hyperparathyroidism other imaging findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2]
Overview
Imaging modalities may be helpful in preoperative localization of hyper-functioning parathyroid glands. This includes both non-invasive and invasive modalities. Non-invasive imaging modalities for preoperative localization of hyper-functioning parathyroid glands include Tc-99m sestamibi scintigraphy (sestamibi or MIBI), single photon emission computed tomography (SPECT), positron emission tomography (PET). Invasive modalities used for preoperative localization of hyper-functioning parathyroid glands include selective arteriography and angiography. Dual energy X-ray absorptiometry is helpful in detecting low bone mineral density (BMD) caused by hyperparathyroidism.
Other Imaging Findings
Other imaging modalities are used for preoperative localization of hyper-functioning parathyroid glands. This includes both non-invasive and invasive modalities. Another modality used in hyperparathyroidism is dual energy X-ray absorptiometry (DXA). DXA is helpful in detecting low bone mineral density (BMD) caused by hyperparathyroidism.
Non-invasive modalities
TC-99m Sestamibi Scintigraphy
- Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands.[1]
- Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity.[2]
- Single-isotope, double-phase technique is used. The basis of "single-isotope, double-phase technique" is that sestamibi washes out of the thyroid more rapidly than from abnormal parathyroid tissue.[3]
- Multiple planar images are obtained, typically one shortly after injection of 99mTc-sestamibi and another after two hours to identify the areas of retained sestamibi showing hyper-functioning parathyroid tissue.
- As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial.[4]
- Subtraction technique uses dual contrast Tc-99m sestamibi along with iodine-123 or 99m-technicium pertechnetate, which are taken by thyroid tissue only. Iodine-123/99m-technicium pertechnetate images of thyroid are later digitally subtracted from Tc-99m sestamibi images leading to visualization of parathyroid tissue only.[5]
- Presence of solid thyroid nodule is the most common cause of false positive results. Other causes of false positive results may include thyroid carcinoma, lymphoma, and lymphadenopathy.
- The sensitivity of sestamibi scintigraphy can be increased by using it concomitantly with neck ultrasound and/or SPECT. [6][7]
- The sensitivity of sestamibi scintigraphy is 80% - 90%.[8][9][10]
| Factors influencing sensitivity of Tc-99m sestamibi scintigraphy | ||
|---|---|---|
| Factors | Sensitivity | |
| Biochemical factors | High serum calcium level[11] | Increased |
| High serum parathyroid hormone level[11][12] | Increased | |
| Hypovitaminosis D [13]
(only in primary hyperparathyroidism) |
Increased | |
| Calcium channel blocker use[14]
(only in primary hyperparathyroidism) |
Decreased | |
| Gross and architectural factors | Size (Large)[15][16] | Increased |
| Multi-glandular disease[17] | Decreased | |
| Cytological factors | Increased amount of cellular content[15][16]
(Chief cells and oxyphil cells) |
Increased |
| Immunohistochemical factors | Increased P-glycoprotien expression[18] | Decreased |
| Note: P-glycoprotein (Pgp) is a plasma membrane protein encoded by mammalian multidrug resistance gene (MDRI). Many drugs that are lipophilic and cationic at physiological pH interact with P-gp. Sestamibi is a lipophilic cationic on physioligical pH. P-gp acts as ATP-dependent efflux pump and prevents accumulation of sestamibi in parathyroid tissue. So, the uptake of sestamibi into parathyroid adenoma cells depends on the activity of the P-gp[19]. | ||
 |
 |
Single photon emission computed tomography (SPECT)
- Single photon emission computed tomography may be used along with Tc-99m sestamibi scintigraphy for preoperative evaluation of hyper-functioning parathyroid gland.[20][21]
- Sestamibi-SPECT is also called pinhone-SPECT (P-SPECT). P-SPECT uses cone beam collimator in contrast to parallel-hole collimator used in SPECT. cone bean collimator possess more suitable geometric properties leading to high spatial resolution.[22][23]
- Using SPECT with sestamibi scintigraphy improves detection and localization of hyper-functioning parathyroid gland.[24][25]
- P-SPECT provides more precise result of sestamibi scitigraphy allowing surgeon to choose best route for surgical intervention.
- P-SPECT may detect glands not visible on planer images leading to increased sensitivity. It is very useful in case of uncertain result from conventional sestamibi scitigraphy.[26][27]
- P-SPECT also enables accurate interpretation sestamibi uptake in upper mediastinum leading to a higher specificity.
- In difficult cases, P-SPECT may also be adjuncted with subtraction Tc-99m sestamibi and I-123 scintigraphy or positron emission tomography.[28]
- P-SPECT is approximately 84% sensitive, 91% specific with positive predictive value of around 91% and negative predictive value of around 84%.[29]
- Fusion images of CT-MIBI-SPECT is superior to CT scan or MIBI-SPECT alone in preoperative localization of hyper-functioning parathyroid gland.[30]
Positron Emission Tomography (PET)
- 11C-methionine PET along with CT scan (MET-PET/CT) may be used for preoperative localization of hyper-functioning parathyroid glands.[31][32]
- MET-PET/CT may be used as an complimentary imaging modality for localizing hyper-functioning parathyroid glands in patients with negative Tc-99m sestamibi scintigraphy/SPECT results.[33]
Invasive modalities
Selective arteriography
- Selective transarterial hypocalcemic stimulation is combined with nonselective venous sampling to perform selective arteriography.[34]
- Sodium citrate is injected to induce hypocalcemia. Simultaneous arteriography is performed.
- Samples are taken for superior vena cava at basaeline and timed intervals (20 sec, 40 sec, and 60 sec).
- An increase in the parathyroid hormone level to 1.4 times above the baseline or a clear blush observed on arteriography is considered as positive localization.
- Arterial stimulation venous sampling is performed simultaneously with arteriogram due to similarly high PPV.
Angiography
- Superselective arterial digital subtraction angiography (DSA) and superselective conventional angiography (CA) may be used for preoperative localization of hyper-functioning parathyroid glands in which noninvasive imaging modalities are negative or inconclusive.[35]
- Sensitivity of superselective digital subtraction angiography appears to be similar to conventional angiography.
- Superselective arterial digital subtraction angiography may be more sensitive than conventional angiography for preoperative localization of mediastinal hyper-functioning parathyroid glands.
Dual Energy X-ray Absorptiometry (DXA)
- Low bone mineral density (BMD) is caused by primary hyperparathyroidism. Distal forearm is affected most commonly.
- DXA of distal forearm should be done in all patients of primary hyperparathyroidism. Very low T-score of distal forearm is observed in patients with primary hyperparathyroidism.[36]
References
- ↑ Palestro CJ, Tomas MB, Tronco GG (2005). "Radionuclide imaging of the parathyroid glands". Semin Nucl Med. 35 (4): 266–76. doi:10.1053/j.semnuclmed.2005.06.001. PMID 16150247.
- ↑ Hetrakul N, Civelek AC, Stagg CA, Udelsman R (2001). "In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria". Surgery. 130 (6): 1011–8. doi:10.1067/msy.2001.118371. PMID 11742331.
- ↑ Taillefer R, Boucher Y, Potvin C, Lambert R (1992). "Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study)". J Nucl Med. 33 (10): 1801–7. PMID 1328564.
- ↑ Thulé P, Thakore K, Vansant J, McGarity W, Weber C, Phillips LS (1994). "Preoperative localization of parathyroid tissue with technetium-99m sestamibi 123I subtraction scanning". J Clin Endocrinol Metab. 78 (1): 77–82. doi:10.1210/jcem.78.1.8288719. PMID 8288719.
- ↑ Ryhänen EM, Schildt J, Heiskanen I, Väisänen M, Ahonen A, Löyttyniemi E; et al. (2015). "(99m)Technetium Sestamibi-(123)Iodine Scintigraphy Is More Accurate Than (99m)Technetium Sestamibi Alone before Surgery for Primary Hyperparathyroidism". Int J Mol Imaging. 2015: 391625. doi:10.1155/2015/391625. PMC 4333274. PMID 25722888.
- ↑ Eslamy HK, Ziessman HA (2008). "Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT". Radiographics. 28 (5): 1461–76. doi:10.1148/rg.285075055. PMID 18794320.
- ↑ Haber RS, Kim CK, Inabnet WB (2002). "Ultrasonography for preoperative localization of enlarged [[parathyroid]] glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy". Clin Endocrinol (Oxf). 57 (2): 241–9. PMID 12153604. URL–wikilink conflict (help)
- ↑ Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B (1996). "Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism". World J Surg. 20 (7): 835–9, discussion 839–40. PMID 8678959.
- ↑ Prasannan S, Davies G, Bochner M, Kollias J, Malycha P (2007). "Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi". ANZ J Surg. 77 (9): 774–7. doi:10.1111/j.1445-2197.2007.04227.x. PMID 17685957.
- ↑ Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A (2010). "Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism". Langenbecks Arch Surg. 395 (7): 929–33. doi:10.1007/s00423-010-0680-8. PMID 20625763.
- ↑ 11.0 11.1 Parikshak M, Castillo ED, Conrad MF, Talpos GB (2003). "Impact of [[hypercalcemia]] and [[parathyroid hormone]] level on the sensitivity of preoperative sestamibi scanning for primary hyperparathyroidism". Am Surg. 69 (5): 393–8, discussion 399. PMID 12769210. URL–wikilink conflict (help)
- ↑ Siegel A, Alvarado M, Barth RJ, Brady M, Lewis J (2006). "Parameters in the prediction of the sensitivity of parathyroid scanning". Clin Nucl Med. 31 (11): 679–82. doi:10.1097/01.rlu.0000242212.23936.a7. PMID 17053383.
- ↑ Kandil E, Tufaro AP, Carson KA, Lin F, Somervell H, Farrag T; et al. (2008). "Correlation of plasma 25-hydroxyvitamin D levels with severity of primary hyperparathyroidism and likelihood of parathyroid adenoma localization on sestamibi scan". Arch Otolaryngol Head Neck Surg. 134 (10): 1071–5. doi:10.1001/archotol.134.10.1071. PMID 18936353.
- ↑ Friedman K, Somervell H, Patel P, Melton GB, Garrett-Mayer E, Dackiw AP; et al. (2004). "Effect of calcium channel blockers on the sensitivity of preoperative 99mTc-MIBI SPECT for hyperparathyroidism". Surgery. 136 (6): 1199–204. doi:10.1016/j.surg.2004.06.047. PMID 15657576.
- ↑ 15.0 15.1 Mehta NY, Ruda JM, Kapadia S, Boyer PJ, Hollenbeak CS, Stack BC (2005). "Relationship of technetium Tc 99m sestamibi scans to histopathological features of hyperfunctioning parathyroid tissue". Arch Otolaryngol Head Neck Surg. 131 (6): 493–8. doi:10.1001/archotol.131.6.493. PMID 15967881.
- ↑ 16.0 16.1 Takebayashi S, Hidai H, Chiba T, Takagi Y, Nagatani Y, Matsubara S (1999). "Hyperfunctional parathyroid glands with 99mTc-MIBI scan: semiquantitative analysis correlated with histologic findings". J Nucl Med. 40 (11): 1792–7. PMID 10565772.
- ↑ Haciyanli M, Lal G, Morita E, Duh QY, Kebebew E, Clark OH (2003). "Accuracy of preoperative localization studies and intraoperative [[parathyroid hormone]] assay in patients with primary hyperparathyroidism and double [[adenoma]]". J Am Coll Surg. 197 (5): 739–46. doi:10.1016/S1072-7515(03)00676-8. PMID 14585407. URL–wikilink conflict (help)
- ↑ Gupta Y, Ahmed R, Happerfield L, Pinder SE, Balan KK, Wishart GC (2007). "P-glycoprotein expression is associated with sestamibi washout in primary hyperparathyroidism". Br J Surg. 94 (12): 1491–5. doi:10.1002/bjs.5882. PMID 17929232.
- ↑ Piwnica-Worms D, Chiu ML, Budding M, Kronauge JF, Kramer RA, Croop JM (1993). "Functional imaging of multidrug-resistant P-glycoprotein with an organotechnetium complex". Cancer Res. 53 (5): 977–84. PMID 8094997.
- ↑ Billotey C, Sarfati E, Aurengo A, Duet M, Mündler O, Toubert ME; et al. (1996). "Advantages of SPECT in technetium-99m-sestamibi parathyroid scintigraphy". J Nucl Med. 37 (11): 1773–8. PMID 8917173.
- ↑ Civelek AC, Ozalp E, Donovan P, Udelsman R (2002). "Prospective evaluation of delayed technetium-99m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism". Surgery. 131 (2): 149–57. PMID 11854692.
- ↑ Strand SE, Ivanovic M, Erlandsson K, Franceschi D, Button T, Sjögren K; et al. (1994). "Small animal imaging with pinhole single-photon emission computed tomography". Cancer. 73 (3 Suppl): 981–4. PMID 8306288.
- ↑ Jaszczak RJ, Li J, Wang H, Zalutsky MR, Coleman RE (1994). "Pinhole collimation for ultra-high-resolution, small-field-of-view SPECT". Phys Med Biol. 39 (3): 425–37. PMID 15551591.
- ↑ Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M (2004). "Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy". Arch Surg. 139 (4): 433–7. doi:10.1001/archsurg.139.4.433. PMID 15078713.
- ↑ Perez-Monte JE, Brown ML, Shah AN, Ranger NT, Watson CG, Carty SE; et al. (1996). "Parathyroid adenomas: accurate detection and localization with Tc-99m sestamibi SPECT". Radiology. 201 (1): 85–91. doi:10.1148/radiology.201.1.8816526. PMID 8816526.
- ↑ Spanu A, Falchi A, Manca A, Marongiu P, Cossu A, Pisu N; et al. (2004). "The usefulness of neck pinhole SPECT as a complementary tool to planar scintigraphy in primary and secondary hyperparathyroidism". J Nucl Med. 45 (1): 40–8. PMID 14734671.
- ↑ Carlier T, Oudoux A, Mirallié E, Seret A, Daumy I, Leux C, Bodet-Milin C, Kraeber-Bodéré F, Ansquer C (2008). "99mTc-MIBI pinhole SPECT in primary hyperparathyroidism: comparison with conventional SPECT, planar scintigraphy and ultrasonography". Eur. J. Nucl. Med. Mol. Imaging. 35 (3): 637–43. doi:10.1007/s00259-007-0625-9. PMC 2964350. PMID 17960377.
- ↑ Nguyen BD (1999). "Parathyroid imaging with Tc-99m sestamibi planar and SPECT scintigraphy". Radiographics. 19 (3): 601–14, discussion 615-6. doi:10.1148/radiographics.19.3.g99ma10601. PMID 10336191.
- ↑ Lindqvist V, Jacobsson H, Chandanos E, Bäckdahl M, Kjellman M, Wallin G (2009). "Preoperative 99Tc(m)-sestamibi scintigraphy with SPECT localizes most pathologic parathyroid glands". Langenbecks Arch Surg. 394 (5): 811–5. doi:10.1007/s00423-009-0536-2. PMID 19578871.
- ↑ Wimmer G, Profanter C, Kovacs P, Sieb M, Gabriel M, Putzer D; et al. (2010). "CT-MIBI-SPECT image fusion predicts multiglandular disease in hyperparathyroidism". Langenbecks Arch Surg. 395 (1): 73–80. doi:10.1007/s00423-009-0545-1. PMID 19705144.
- ↑ Tang BN, Moreno-Reyes R, Blocklet D, Corvilain B, Cappello M, Delpierre I; et al. (2008). "Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT". Contrast Media Mol Imaging. 3 (4): 157–63. doi:10.1002/cmmi.243. PMID 18781582.
- ↑ Weber T, Maier-Funk C, Ohlhauser D, Hillenbrand A, Cammerer G, Barth TF; et al. (2013). "Accurate preoperative localization of parathyroid adenomas with C-11 methionine PET/CT". Ann Surg. 257 (6): 1124–8. doi:10.1097/SLA.0b013e318289b345. PMID 23478517.
- ↑ Traub-Weidinger T, Mayerhoefer ME, Koperek O, Mitterhauser M, Duan H, Karanikas G; et al. (2014). "11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery". J Clin Endocrinol Metab. 99 (11): 4199–205. doi:10.1210/jc.2014-1267. PMID 25029418.
- ↑ Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, Pingpank JF; et al. (2009). "Reoperation for parathyroid adenoma: a contemporary experience". Surgery. 146 (6): 1144–55. doi:10.1016/j.surg.2009.09.015. PMC 3467310. PMID 19958942.
- ↑ Miller DL, Chang R, Doppman JL, Norton JA (1989). "Localization of parathyroid adenomas: superselective arterial DSA versus superselective conventional angiography". Radiology. 170 (3 Pt 2): 1003–6. doi:10.1148/radiology.170.3.2644666. PMID 2644666.
- ↑ Wood K, Dhital S, Chen H, Sippel RS (2012). "What is the utility of distal forearm DXA in primary hyperparathyroidism?". Oncologist. 17 (3): 322–5. doi:10.1634/theoncologist.2011-0285. PMC 3316917. PMID 22258698.