Haemophilus influenzae: Difference between revisions
No edit summary |
|||
| Line 43: | Line 43: | ||
It is unclear why ''H. influenzae'' is not affected by the immune response.<ref name=Lysenko_2005>{{cite journal |author=Lysenko E, Ratner A, Nelson A, Weiser J |title=The role of innate immune responses in the outcome of interspecies competition for colonization of mucosal surfaces |journal=PLoS Pathog |volume=1 |issue=1 |pages=e1 |year=2005 |id=PMID 16201010}}</ref> | It is unclear why ''H. influenzae'' is not affected by the immune response.<ref name=Lysenko_2005>{{cite journal |author=Lysenko E, Ratner A, Nelson A, Weiser J |title=The role of innate immune responses in the outcome of interspecies competition for colonization of mucosal surfaces |journal=PLoS Pathog |volume=1 |issue=1 |pages=e1 |year=2005 |id=PMID 16201010}}</ref> | ||
==Related Chapters== | ==Related Chapters== | ||
Revision as of 20:04, 10 August 2015
| Haemophilus influenzae | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
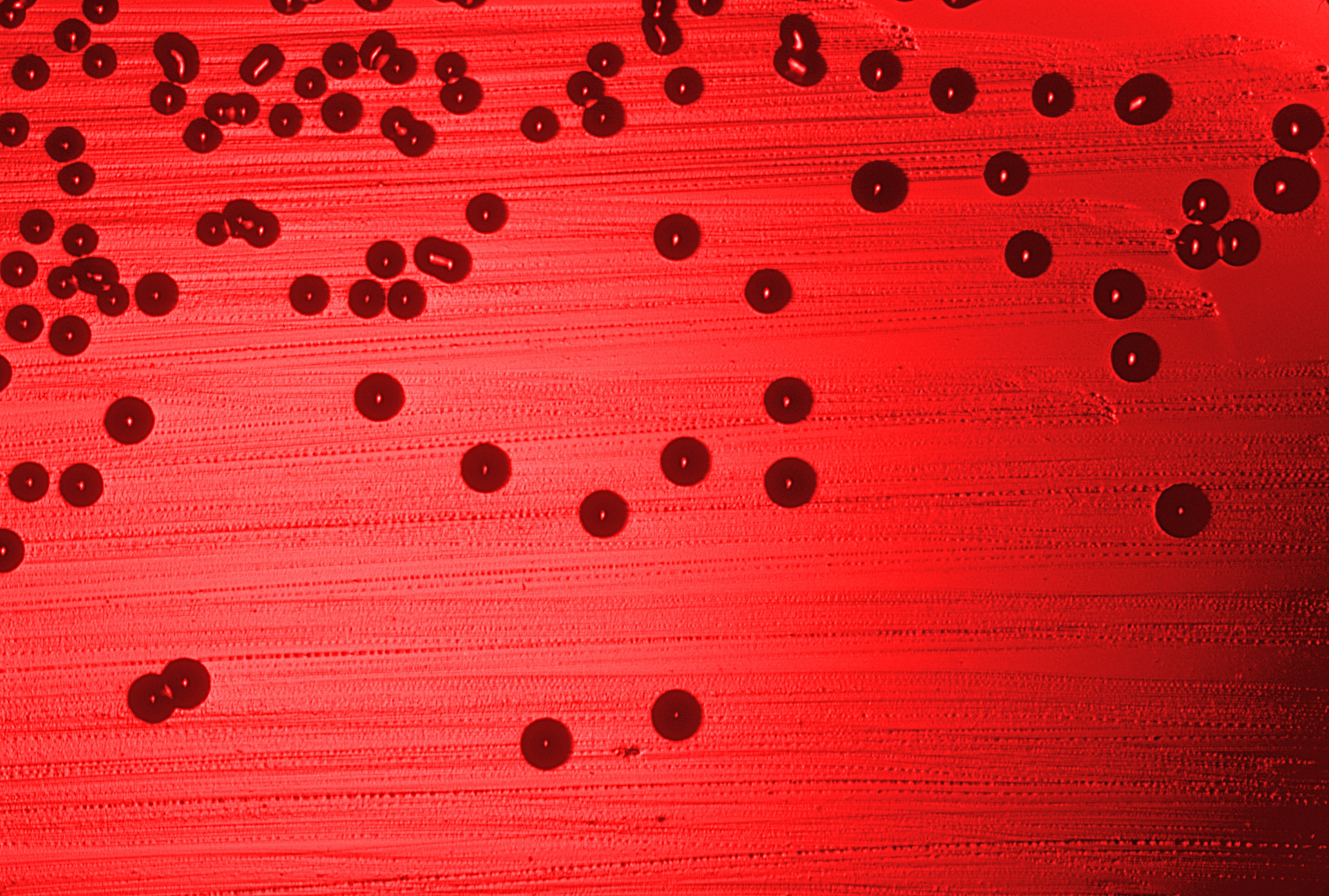 H. influenzae on a blood agar plate.
| ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Haemophilus influenzae (Lehmann & Neumann 1896) Winslow et al. 1917 |
Overview
Haemophilus influenzae, formerly called Pfeiffer's bacillus or Bacillus influenzae, is a non-motile Gram-negative coccobacillus first described in 1892 by Richard Pfeiffer during an influenza pandemic. It is generally aerobic, but can grow as a facultative anaerobe. H. influenzae was mistakenly considered to be the cause of the common flu until 1933, when the viral etiology of the flu became apparent. Still, H. influenzae is responsible for a wide range of clinical diseases.
Because of its small genome, H. influenzae became the first free-living organism with its entire genome sequenced. Its genome consists of 1,830,140 base pairs of DNA and contains 1740 genes. The method used was Whole genome shotgun. The sequencing project, completed and published in Science in 1995, was conducted at The Institute for Genomic Research.[1]
Serotypes
In 1930, 2 major categories of H. influenzae were defined: the unencapsulated strains and the encapsulated strains. The pathogenesis of H. influenzae infections is not completely understood, although the presence of the encapsulated type b (Hib) is known to be the major factor in virulence. Their capsule allows them to resist phagocytosis and complement-mediated lysis in the non-immune host. Unencapsulated strains are less invasive, but they are able to induce an inflammatory response that causes disease, such as epiglottitis. Vaccination with Hib conjugate vaccines is effective in preventing infection, and several vaccines are now available for routine use.
Diseases
Most strains of H. influenzae are opportunistic pathogens - that is, they usually live in their host without causing disease, but cause problems only when other factors (such as a viral infection or reduced immune function) create an opportunity. There are six generally recognized types of H. influenzae: a, b, c, d, e, and f.[2]
Naturally-acquired disease caused by H. influenzae seems to occur in humans only. In infants and young children, H. influenzae type b (Hib) causes bacteremia, and acute bacterial meningitis. Occasionally, it causes cellulitis, osteomyelitis, epiglottitis, and joint infections. Due to routine use of the Hib conjugate vaccine in the U.S. since 1990, the incidence of invasive Hib disease has decreased to 1.3/100,000 children. However, Hib remains a major cause of lower respiratory tract infections in infants and children in developing countries where vaccine is not widely used. Unencapsulated H. influenzae (non-B type) causes ear (otitis media) and eye (conjunctivitis) infections and sinusitis in children, and is associated with pneumonia.
Interaction with Streptococcus pneumoniae
Both H. influenzae and S. pneumoniae can be found in the upper respiratory system of humans. A study of competition in a laboratory revealed that, in a petri dish, S. pneumoniae always overpowered H. influenzae by attacking it with a hydrogen peroxide and stripping off the surface molecules H. influenzae needs for survival.
When both bacteria are placed together into a nasal cavity, within 2 weeks, only H. influenzae survives. When both are placed separately into a nasal cavity, each one survives. Upon examining the upper respiratory tissue from mice exposed to both bacteria species, an extraordinarily large number of neutrophils immune cells were found. In mice exposed to only one bacteria, the cells were not present.
Lab tests showed that neutrophils exposed to dead H. influenzae were more aggressive in attacking S. pneumoniae than unexposed neutrophils. Exposure to dead H. influenzae had no effect on live H. influenzae.
Two scenarios may be responsible for this response:
- When H. influenzae is attacked by S. pneumoniae, it signals the immune system to attack the S. pneumoniae
- The combination of the two species together triggers an immune system response that is not set off by either species individually.
It is unclear why H. influenzae is not affected by the immune response.[3]
Related Chapters
Gallery
-
Gross pathology of subacute bacterial endocarditis involving mitral valve. From Public Health Image Library (PHIL). [4]
-
Haemophilus influenzae satelliting around Staphylococcus aureus. From Public Health Image Library (PHIL). [4]
-
Blood agar plate culture of Haemophilus influenzae. From Public Health Image Library (PHIL). [4]
-
Photomicrograph of Haemophilus influenzae using immunofluorescence. From Public Health Image Library (PHIL). [4]
-
Brain infected with Gram-negative Haemophilus influenzae bacteria From Public Health Image Library (PHIL). [4]
-
Photomicrograph reveals Gram-negative rods, and Gram-negative cocci, which were determined to be Haemophilus influenzae, and non-meningococcal Neisseria sp. organisms respectively (1000X mag). From Public Health Image Library (PHIL). [4]
-
Photograph of Gram-negative Haemophilus influenzae bacteria, which were cultured on chocolate agar medium (10X mag). From Public Health Image Library (PHIL). [4]
-
Photomicrograph reveals Gram-negative rods, and Gram-negative cocci, which were determined to be Haemophilus influenzae, and non-meningococcal Neisseria sp. organisms in sample of a transtracheal aspirate (1000x mag). From Public Health Image Library (PHIL). [4]
References
- ↑ Fleischmann R, Adams M, White O, Clayton R, Kirkness E, Kerlavage A, Bult C, Tomb J, Dougherty B, Merrick J (1995). "Whole-genome random sequencing and assembly of Haemophilus influenzae Rd". Science. 269 (5223): 496–512. PMID 7542800.
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. pp. 396&ndash, 401. ISBN 0838585299.
- ↑ Lysenko E, Ratner A, Nelson A, Weiser J (2005). "The role of innate immune responses in the outcome of interspecies competition for colonization of mucosal surfaces". PLoS Pathog. 1 (1): e1. PMID 16201010.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 "Public Health Image Library (PHIL)".
External Links
- Hib information on the World Health Organization (WHO) site.
- Fact sheet on the Centers for Disease Control and Prevention (CDC) site.
- Hib Initiative - from Johns Hopkins University, London School of Hygiene & Tropical Medicine, CDC & WHO
![Gross pathology of subacute bacterial endocarditis involving mitral valve. From Public Health Image Library (PHIL). [4]](/images/f/f2/Haemophilus_influenzae08.jpeg)
![Haemophilus influenzae satelliting around Staphylococcus aureus. From Public Health Image Library (PHIL). [4]](/images/b/b7/Haemophilus_influenzae07.jpeg)
![Blood agar plate culture of Haemophilus influenzae. From Public Health Image Library (PHIL). [4]](/images/8/8a/Haemophilus_influenzae06.jpeg)
![Photomicrograph of Haemophilus influenzae using immunofluorescence. From Public Health Image Library (PHIL). [4]](/images/9/96/Haemophilus_influenzae05.jpeg)
![Brain infected with Gram-negative Haemophilus influenzae bacteria From Public Health Image Library (PHIL). [4]](/images/e/e1/Haemophilus_influenzae04.jpeg)
![Photomicrograph reveals Gram-negative rods, and Gram-negative cocci, which were determined to be Haemophilus influenzae, and non-meningococcal Neisseria sp. organisms respectively (1000X mag). From Public Health Image Library (PHIL). [4]](/images/7/77/Haemophilus_influenzae03.jpeg)
![Photograph of Gram-negative Haemophilus influenzae bacteria, which were cultured on chocolate agar medium (10X mag). From Public Health Image Library (PHIL). [4]](/images/a/a1/Haemophilus_influenzae02.jpeg)
![Photomicrograph reveals Gram-negative rods, and Gram-negative cocci, which were determined to be Haemophilus influenzae, and non-meningococcal Neisseria sp. organisms in sample of a transtracheal aspirate (1000x mag). From Public Health Image Library (PHIL). [4]](/images/3/35/Haemophilus_influenzae01.jpeg)