Goodpasture syndrome pathophysiology
|
Goodpasture syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Goodpasture syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Goodpasture syndrome pathophysiology |
|
Risk calculators and risk factors for Goodpasture syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathogenesis
The pathogenesis of Goodpasture syndrome is the presence of autoantibodies against the glomerular or alveolar basement membranes. The target antigen that has the strongest pathogenic effect on anti-GBM disease is the non-collagenous 1 domain of alpha-3 type IV collagen. There are 2 dominant epitopes, they are epitope A and epitope B. These epitopes are seen in the alpha-3 non-collagenous 1 domain of type IV collagen and antibodies do not normally bind unless a change has occurred in the non-cross linked hexamers or trimers. In Goodpasture syndrome these epitopes undergo a transitional change in the non-cross linked hexamers or trimers. This allows antibodies to be bound to the epitopes. The cause of this is said to be due to many factors such as oxidation, nitrosylation, glycation, increases in body temperature, or proteolytic cleavage.
Antibodies are unable In Goodpasture syndrome, when a transitional change occurs in non-cross linked hexamers or trimers
(Zhao, J., Cui, Z., Yang, R., Jia, X., Zhang, Y., Zhao, M.).
GS undergoes a transitional change in non-cross linked hexamers or trimers that form neoepitopes, causing antibodies to be produced and bound. The cause of this change can be due to many factors or a combination of factors such as oxidation, nitrosylation, and glycation, increases in body temperature, or proteolytic cleavage. It has been shown that cleavage of a disulfide bond in alpha-3 NC1 in a non-cross linked hexamer allows greater binding of Goodpasture antibodies. Other factors that may play a role in GS are environmental factor such as smoking which has a pathogenic factor that causes an inhibition sulfilimine bond substances forming higher extents of non-cross linked hexamers (Pedchenko, V., Bondar, O., Fogo, A., Vanacore, R., Voziyan, P., Kitching, R., Wieslander, J., Kashtan, C., Borza, D., Neilson, G., Wilson, C., Hudson, B.). The pathogenic role of epitopes such as EA, have been shown to affect the function of the renals, especially of the alpha-3 type IV collagen of non-collagenous 1 domain. Epitope B however was is not able to induce GS by itself (Chen, J., Hu, S., Jia, X., Zhao, J., Yang, R., Cui, Z., Zhao, M). The cause of renal injury is due to anti-GBM antibodies that binding and activate complements and proteases, which results in interruption of the filtration barrier as well as the Bowman’s capsule. The interruption of both the filtration barrier and the Bowman’s capsule causes the outcome of proteinuria and induces crescent formation of the renals. The renal injury causes the induction of T cells (CD4+, CD8+) and intrinsic renal epithelium to signal both macrophages and neutrophils to the injured renals. Crescent formation of the renals is induced by Il-12 and interferon gamma (Hudson, B., Tryggvason, K., Sundaramoorthy, M., Neilson, E.).
Pathophysiology
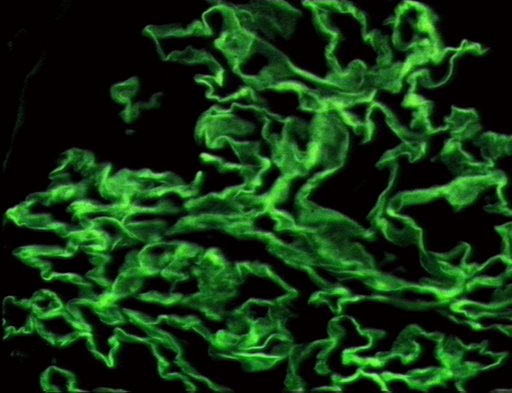
As with many autoimmune conditions, the precise cause of Goodpasture’s Syndrome is not yet known. It is believed to be a type II hypersensitivity reaction to Goodpasture’s antigens on the cells of the glomeruli of the kidneys and the pulmonary alveoli, specifically the basement membrane's (including a-3 chain of type IV collagen), whereby the immune system wrongly recognizes these cells as foreign and attacks and destroys them, as it would an invading pathogen.
Pathology