Glomerulonephritis
| Glomerulonephritis | |
 | |
|---|---|
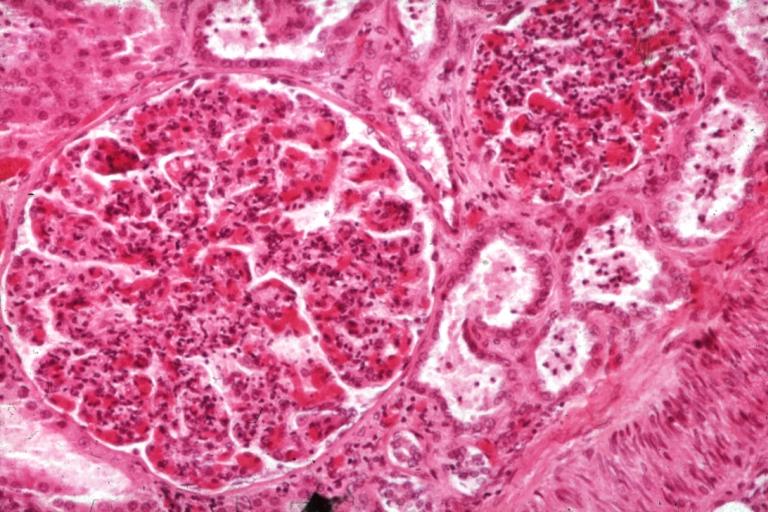
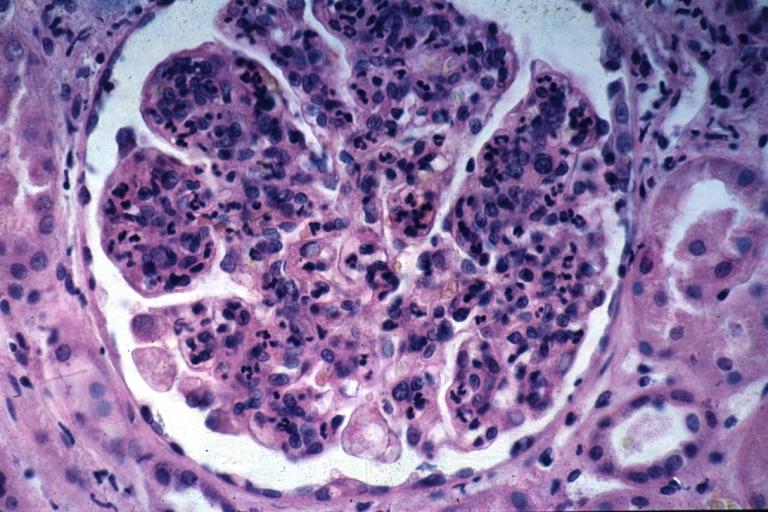
| Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | N00, N01, N03, N18 |
| ICD-9 | 580-582 |
| DiseasesDB | 5245 |
| MeSH | D005921 |
|
Glomerulonephritis Main page |
|
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: GN; glomerular nephritis
Overview
Glomerulonephritis, also known as glomerular nephritis and abbreviated GN', is a primary or secondary immune-mediated renal disease characterized by inflammation of the glomeruli, or small blood vessels in the kidneys. It may present with isolated hematuria and/or proteinuria (blood resp. protein in the urine); or as a nephrotic syndrome, a nephritic syndrome, acute renal failure, or chronic renal failure.
They are categorized into several different pathological patterns, which are broadly grouped into non-proliferative or proliferative types. Diagnosing the pattern of GN is important because the outcome and treatment differs in different types. Primary causes are one which are intrinsic to the kidney, whilst secondary causes are associated with certain infections (bacterial, viral or parasitic pathogens), drugs, systemic disorders (SLE, vasculitis) or cancers.
Histopathology
The majority of glomeruli present "crescents". Formation of crescents is initiated by passage of fibrin into the Bowman space as a result of increased permeability of glomerular basement membrane. Fibrin stimulates the proliferation of parietal cells of Bowman capsule, and an influx of monocytes. Rapid growing and fibrosis of crescents compresses the capillary loops and decreases the Bowman space which leads to renal failure within weeks or months.
-
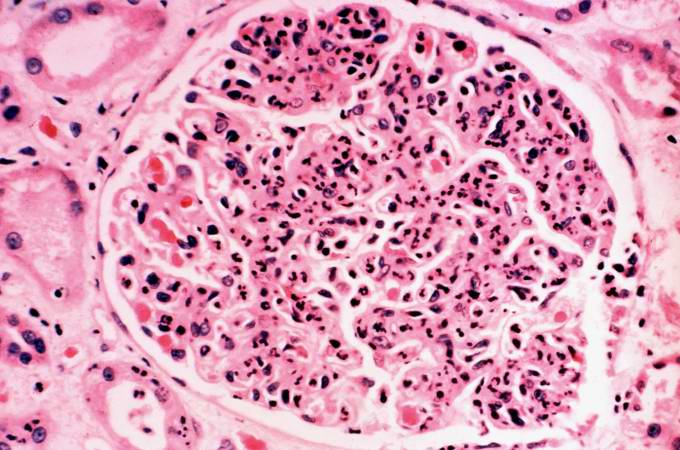
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Pathological Findings: A Case Example
Clinical Summary
A 17-year-old white male had end-stage renal disease requiring hemodialysis for 10 years. For the previous four years he had hypertension which slowly increased to about 180/120 mm Hg. Laboratory findings included a greatly elevated BUN and creatinine. He was admitted for bilateral nephrectomy and discharged in satisfactory condition on the 10th postoperative day. He was to be contacted in the future for transplantation.
Autopsy Findings
The left (97 grams) and right (88 grams) kidneys were of similar appearance. Cortices were pale, diffusely granular with a few 1-2 mm cysts. On being sectioned, the cortex of each kidney was thin (4-5 mm) and pale. Renal medullae were pale yellow-tan in color and there was abundant peripelvic fat. The ureters, pelvis, calyces and hilar vessels showed no abnormalities.
-
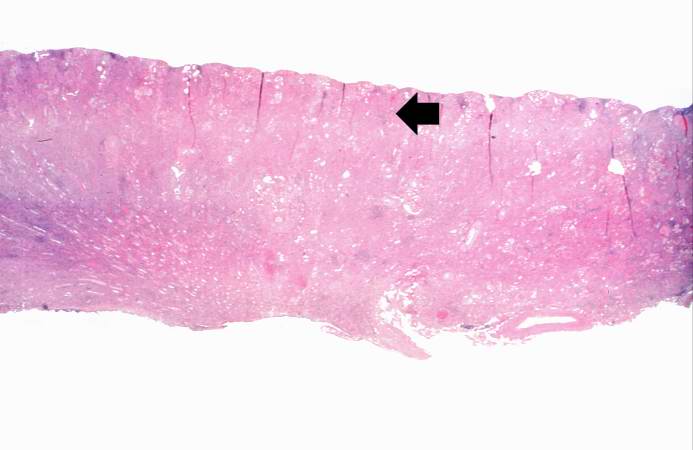
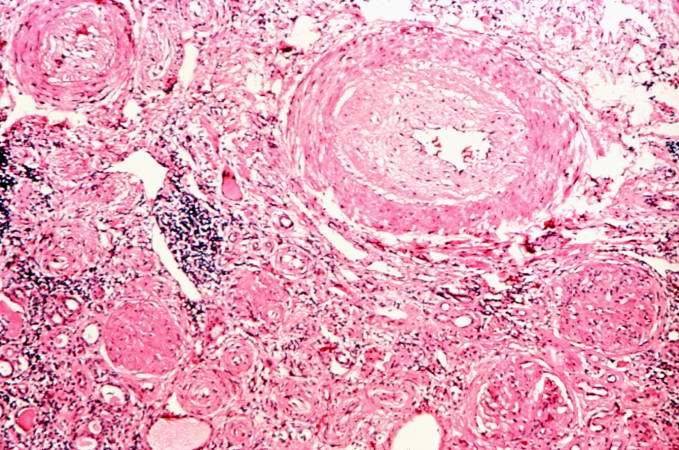
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
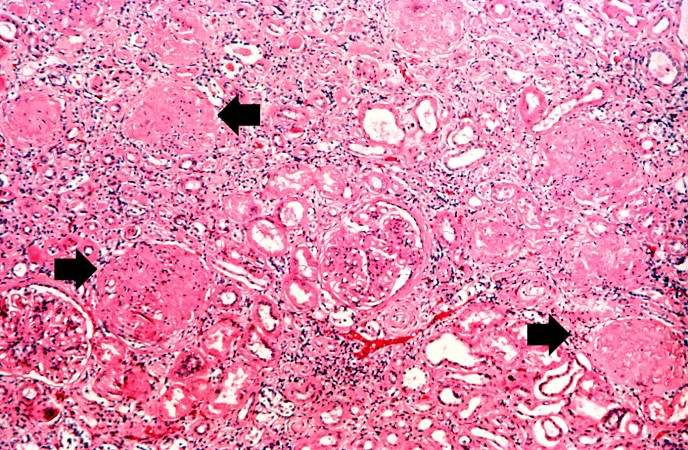
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
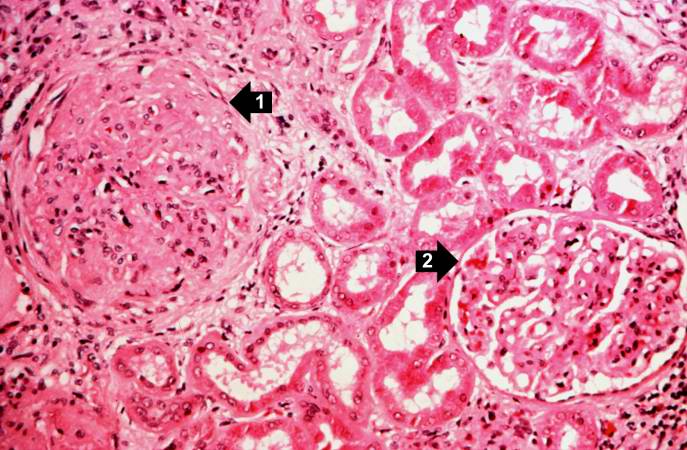
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
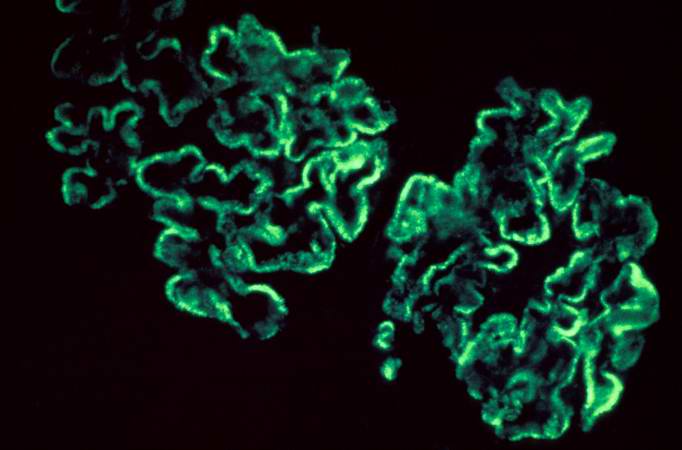
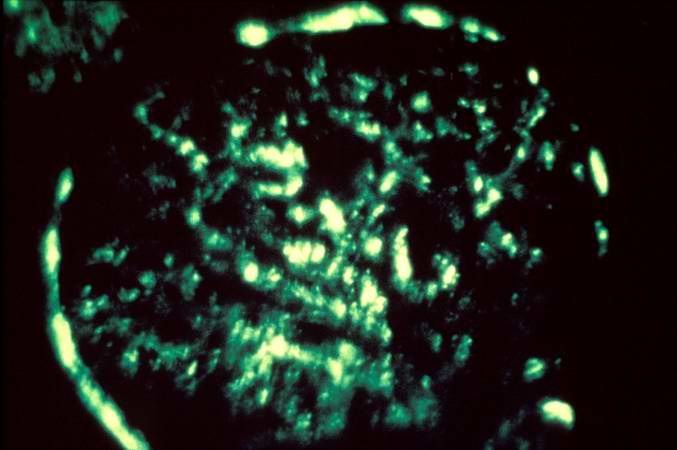
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
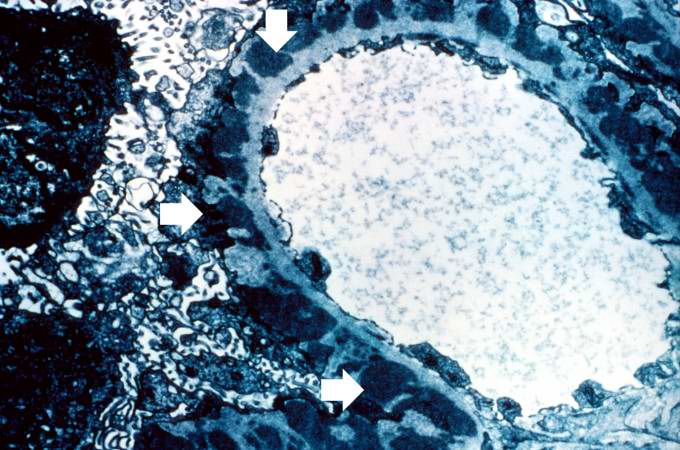
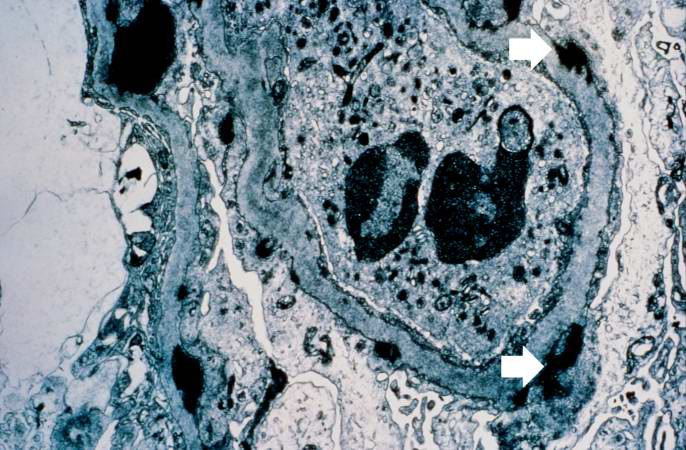
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
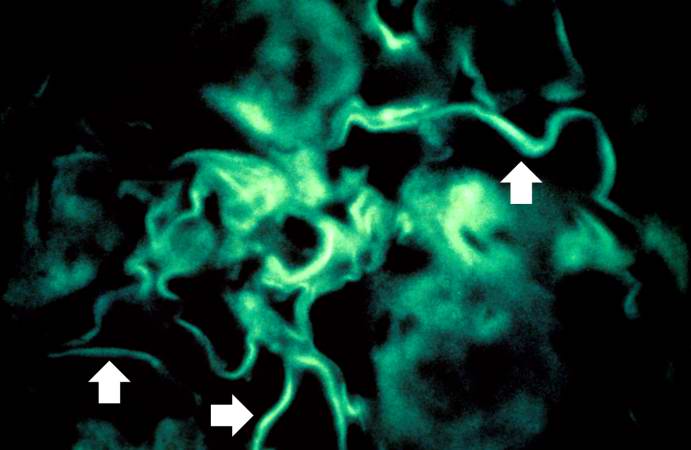
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.
Related chapters
Resources
Images:
HDCN
- HDCN Nephritis Channel - Collection of lectures and links pertaining to glomerulonephritis on the HDCN (Hypertension, Dialysis, and Clinical Nephrology) on-line journal.
- Post-infectious glomerulonephritis - mayoclinic.com.
- Group A Streptococcal Infections - National Institute of Allergy and Infectious Diseases.
References
de:Glomerulonephritis nl:Glomerulonefritis sv:Glomerulonefrit