COVID-19-associated acute kidney injury: Difference between revisions
Jump to navigation
Jump to search
Gerald Chi- (talk | contribs) |
Gerald Chi- (talk | contribs) m (→Symptoms) |
||
| Line 47: | Line 47: | ||
=== Symptoms === | === Symptoms === | ||
* Patients in the early stages of [[kidney failure]] may be asymptomatic. If left untreated, patients may progress to develop [[Azotemia]] and [[Uremia]], which occur due to the buildup of waste materials in the blood. | |||
* Symptoms of kidney injury include:<ref name="Skorecki">{{cite book |vauthors=Skorecki K, Green J, Brenner BM |veditors=Kasper DL, Braunwald E, Fauci AS |title=Harrison's Principles of Internal Medicine|url=https://archive.org/details/harrisonsprincip00kasp |url-access=limited |edition=16th |year=2005 |publisher=McGraw-Hill |location=New York, NY |isbn=978-0-07-139140-5 |pages=[https://archive.org/details/harrisonsprincip00kasp/page/n1681 1653]–63 |chapter=Chronic renal failure|display-editors=etal}}</ref> | |||
**Nausea and Vomiting | |||
**Weakness | |||
**Fatigue | |||
**[[Confusion]] | |||
**Weight loss | |||
**Loss of appetite | |||
**[[Oliguria]] or [[Anuria]] | |||
**Fluid retention, leading [[edema]] and swelling of face and extremities | |||
**Electrolyte imbalance; High level of [[Potassium]] which leads to [[cardiac arrhythmia]] | |||
===Family History=== | ===Family History=== | ||
Revision as of 17:08, 25 June 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sogand Goudarzi, MD [2], Nasrin Nikravangolsefid, MD-MPH [3]
Synonyms and keywords: COVID-19-associated AKI
Overview
COVID-19 can involve many organs leading to organ failure, one of which is kidneys that manifest with mild proteinuria to advanced acute kidney injury (AKI).
Historical Perspective
- Early reports from China revealed that COVID-19 rarely involves the kidneys, as acute renal failure was not seen among COVID-19 hospitalized patients and mild BUN or creatinine rise [10.8%] and mild proteinuria [7.2%] occurred. [1]
- However, recent study found 75.4% of hospitalized patients with COVID-19 pneumonia developed hematuria, proteinuria, and AKI. But, these findings are not significantly different from other critical diseases.[2]
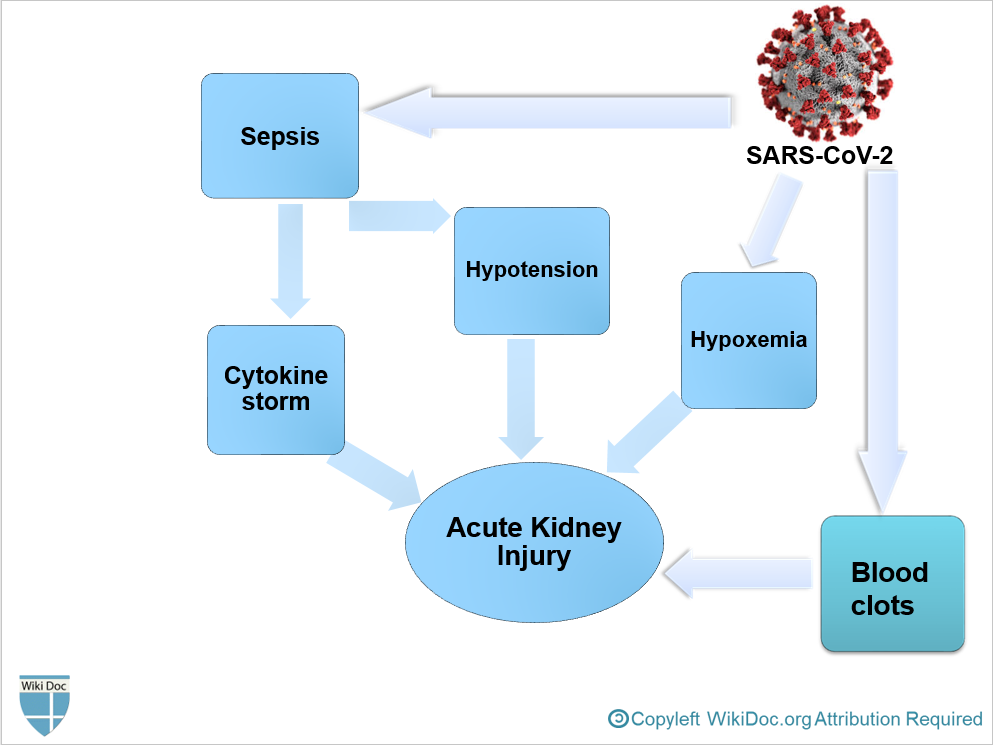
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2), which is a primary receptor for SARS-CoV-2 entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.[3]
- Despite kidney injury following COVID-19 infection is less frequent than severe lung injury, ACE2: ACE ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)[3]
- After SARS-CoV-2 enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
- It is thought that AKI following COVID-19 is the result of: [3]
- Sepsis
- Hypovolemia and Hypotension
- Hypoxemia
- Blood clots formation, leading to impaired blood flow in the renal arterioles.
Epidemiology and Demographics
- AKI is frequently seen among patients with COVID-19 hospitalized in ICU, with prevalence of 0.6-29% in China "Acute Kidney Injury in COVID-19 Patients | COVID-19". and 22.2% in the USA.[4]
- The incidence of AKI in critcally ill patients with COVID-19 is estimated between 27-85%. "Acute Kidney Injury in COVID-19 Patients | COVID-19".
Risk Factors
Screening
Natural History, Complications, and Prognosis
Natural History
- AKI is more likely to develop in the late stages of COVID-19 in critically ill patients.[5]
- Severe COVID-19 pneumonia and severe acute respiratory distress syndrome are associated with developing AKI.[2]
- If no improvement occurs during follow-up, it is contributed to higher mortality.[2]
Diagnosis
Symptoms
- Patients in the early stages of kidney failure may be asymptomatic. If left untreated, patients may progress to develop Azotemia and Uremia, which occur due to the buildup of waste materials in the blood.
- Symptoms of kidney injury include:[6]
Family History
Physical Examination
Appearance of the Patient
Vital Signs
Skin
Head
Eyes
Ear
Nose
Throat
Heart
Lungs
Abdomen
Extremities
Neurologic
Other
Laboratory Findings
Biomarker Studies
CT
MRI
Ultrasound
Treatment
Pharmacotherapy
Acute Pharmacotherapies
Chronic Pharmacotherapies
Surgery and Device Based Therapy
Indications for Surgery
Pre-Operative Assessment
Post-Operative Management
Primary Prevention
Genetic Counseling
References
- ↑ Wang, Luwen; Li, Xun; Chen, Hui; Yan, Shaonan; Li, Dong; Li, Yan; Gong, Zuojiong (2020). "Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China". American Journal of Nephrology. 51 (5): 343–348. doi:10.1159/000507471. ISSN 0250-8095.
- ↑ 2.0 2.1 2.2 Pei, Guangchang; Zhang, Zhiguo; Peng, Jing; Liu, Liu; Zhang, Chunxiu; Yu, Chong; Ma, Zufu; Huang, Yi; Liu, Wei; Yao, Ying; Zeng, Rui; Xu, Gang (2020). "Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia". Journal of the American Society of Nephrology. 31 (6): 1157–1165. doi:10.1681/ASN.2020030276. ISSN 1046-6673.
- ↑ 3.0 3.1 3.2 Malha, Line; Mueller, Franco B.; Pecker, Mark S.; Mann, Samuel J.; August, Phyllis; Feig, Peter U. (2020). "COVID-19 and the Renin-Angiotensin System". Kidney International Reports. 5 (5): 563–565. doi:10.1016/j.ekir.2020.03.024. ISSN 2468-0249.
- ↑ Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW; et al. (2020). "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area". JAMA. doi:10.1001/jama.2020.6775. PMC 7177629 Check
|pmc=value (help). PMID 32320003 Check|pmid=value (help). - ↑ Ronco C, Reis T, Husain-Syed F (2020). "Management of acute kidney injury in patients with COVID-19". Lancet Respir Med. doi:10.1016/S2213-2600(20)30229-0. PMC 7255232 Check
|pmc=value (help). PMID 32416769 Check|pmid=value (help). - ↑ Skorecki K, Green J, Brenner BM (2005). "Chronic renal failure". In Kasper DL, Braunwald E, Fauci AS, et al. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 1653–63. ISBN 978-0-07-139140-5.