Assessment of cardiovascular risk
|
Atherosclerosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
ACC/AHA Guideline Recommendations |
|
Case Studies |
|
Assessment of cardiovascular risk On the Web |
|
American Roentgen Ray Society Images of Assessment of cardiovascular risk |
|
Risk calculators and risk factors for Assessment of cardiovascular risk |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk[1]
Summary of Recommendations for Risk Assessment of Cardiovascular Risk
Implementation of Risk Assessment Work Group Recommendations
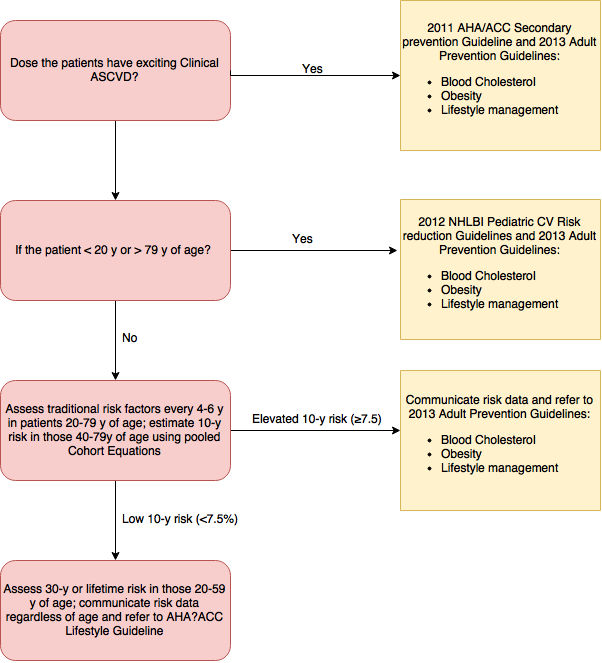
Assessment of 10-Year Risk of a First Hard ASCVD Event
| Class I |
| "1. The race- and sex-specific Pooled Cohort Equations* to predict 10-year risk of a first hard ASCVD event should be used in non-Hispanic African
Americans and non-Hispanic whites, 40–79 years of age.(Level of Evidence: B)" |
| Class IIb |
"1. Assessment of 10-Year Risk of a First Hard ASCVD Event
|
Use of Newer Risk Markers After Quantitative Risk Assessment
| Class IIb† |
| "1.If, after quantitative risk assessment, a risk-based treatment decision is uncertain, assessment of ≥1 of the followingdfamily history, hs-CRP, CAC score, or ABIdmay be considered to inform treatment decision making. (Level of Evidence: B)" |
| Class III† |
| "1.Routine measurement of CIMT is not recommended in clinical practice for risk assessment for a first ASCVD event. (Level of Evidence: B) " |
Long-Term Risk Assessment
| Class IIa |
| "1. It is reasonable to assess traditional ASCVD risk factors‡ every 4–6 years in adults 20–79 years of age who are free from ASCVD and to estimate 10-year ASCVD risk every 4–6 years in adults 40–79 years of age who are free from ASCVD.(Level of Evidence: B)" |
| Class IIb |
| "3. Assessment of 30-year or lifetime ASCVD risk on the basis of traditional risk factorsz may be considered in adults 20–59 years of age who are free from ASCVD and are not at high short-term risk. (Level of Evidence: C)" |
*Derived from the ARIC (Atherosclerosis Risk in Communities) study, Cardiovascular Health Study , CARDIA (Coronary Artery Risk Development in Young Adults) study , and Framingham original and offspring cohorts
†Based on new evidence reviewed during ACC/AHA update of evidence
‡Age, sex, total cholesterol, high-density lipoprotein cholesterol, systolic BP, use of antihypertensive therapy, diabetes, and current smoking.
ABI indicates ankle-brachial index; ACC, American College of Cardiology; AHA, American Heart Association; ApoB, apolipoprotein B; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CAC, coronary artery calcium; CIMT, carotid intima-media thickness; CKD, chronic kidney disease; COR, Class of Recommendation; CQ, critical question, ES, evidence statement; hs-CRP, high-sensitivity C-reactive protein; LOE, Level of Evidence; NHLBI, National Heart, Lung, and Blood Institute; and d, not applicable.
References
- ↑ 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk. http://ac.els-cdn.com/S0735109713060312/1-s2.0-S0735109713060312-main.pdf?_tid=b1900316-9d1f-11e6-92c8-00000aacb360&acdnat=1477667193_f8c7920ce856f2c1fa93cb7968f1cb92 Accessed on October 28, 2016