Angiosarcoma: Difference between revisions
(→Causes) |
No edit summary |
||
| (82 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | {{SI}} | ||
{{CMG}}; {{AE}} {{ | {{CMG}} {{shyam}}; {{AE}} {{M.B}}<br> | ||
{{SK}} Hemangiosarcoma; Pulmonary angiosarcoma; Vascular sarcoma | {{SK}} Hemangiosarcoma; Pulmonary angiosarcoma; Vascular sarcoma | ||
==Overview== | ==Overview== | ||
'''Angiosarcoma''' is a rare [[malignant]] [[vascular]] [[neoplasm]] of [[endothelial]]-type [[cells]] that line [[Vessel wall|vessel walls]]. The peak age of [[incidence]] appears to be the 7th decade, and men are affected more commonly than women. Angiosarcoma was first described by Dr. Juan Rosai, in 1976. The [[pathogenesis]] of angiosarcoma is characterized by a rapid and extensively infiltrating overgrowth of [[vascular]] [[endothelial]] [[cells]]. Angiosarcoma may arise in any part of the body, but is more common in [[soft tissues]] than in [[bones]]. Common angiosarcoma locations include the [[head and neck]] area, [[kidney]], [[liver]], [[lung]], and and the most common site of [[radiation]]-induced angiosarcoma development is the [[breast]]. The [[PTPRB]]/[[Phospholipase C|PLCG1]] [[genes]] are associated with the development of angiosarcoma; [[mutation]] of these [[genes]] result in aberrant [[angiogenesis]]. The imaging modality of choice for [[Diagnose|diagnosing]] angiosarcoma will depend on the location. For [[pulmonary]] angiosarcoma, the imaging modality of choice is [[CT scan]] with [[intravenous]] contrast. For other types angiosarcoma, the imaging modality of choice is [[MRI]]. On [[CT scan]], findings suggestive of angiosarcoma may include [[vascular]] [[invasion]], nodular enhancement (common), and a hypoattenuating [[mass]]. The mainstay [[adjuvant therapy]] for angiosarcoma is a [[doxorubicin]]-based regimen. The response rate for [[chemotherapy]] in patients with angiosarcoma is poor. | |||
'''Angiosarcoma''' is a rare [[malignant]] vascular [[neoplasm]] of [[endothelial]]-type cells that line vessel walls. The peak age of incidence appears to be the 7th decade, and men are affected more than women. Angiosarcoma was first described by Dr. Juan Rosai, in 1976. The pathogenesis of angiosarcoma is characterized by a rapid and extensively infiltrating overgrowth of vascular [[ | |||
==Historical Perspective== | ==Historical Perspective== | ||
[[Angiosarcoma]] was first discovered by Dr. Juan Rosai, M.D. and colleagues in 1976.<ref name="pmid24946325">{{cite journal |vauthors=Barber W, Scriven P, Turner D, Hughes D, Wyld D |title=Epithelioid angiosarcoma: Use of angiographic embolisation and radiotherapy to control recurrent haemorrhage |journal=J Surg Case Rep |volume=2010 |issue=5 |pages=7 |year=2010 |pmid=24946325 |pmc=3649120 |doi=10.1093/jscr/2010.5.7 |url=}}</ref> | *[[Angiosarcoma]] was first discovered by Dr. Juan Rosai, M.D. and colleagues in 1976.<ref name="pmid24946325">{{cite journal |vauthors=Barber W, Scriven P, Turner D, Hughes D, Wyld D |title=Epithelioid angiosarcoma: Use of angiographic embolisation and radiotherapy to control recurrent haemorrhage |journal=J Surg Case Rep |volume=2010 |issue=5 |pages=7 |year=2010 |pmid=24946325 |pmc=3649120 |doi=10.1093/jscr/2010.5.7 |url=}}</ref> | ||
==Classification== | ==Classification== | ||
Angiosarcoma may be classified according to the clinical heterogeneity into two main groups, and every group can be subdivided into subtypes according to the anatomical location and etiology:<ref>{{ | *Angiosarcoma may be [[classification|classified]] according to the clinical heterogeneity into two main groups, and every group can be subdivided into subtypes according to the [[anatomical]] location and etiology:<ref name="pmid16053668">{{cite journal |vauthors=Fury MG, Antonescu CR, Van Zee KJ, Brennan MF, Maki RG |title=A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy |journal=Cancer J |volume=11 |issue=3 |pages=241–7 |date=2005 |pmid=16053668 |doi= |url=}}</ref><ref name="pmid18771914">{{cite journal |vauthors=Schlemmer M, Reichardt P, Verweij J, Hartmann JT, Judson I, Thyss A, Hogendoorn PC, Marreaud S, Van Glabbeke M, Blay JY |title=Paclitaxel in patients with advanced angiosarcomas of soft tissue: a retrospective study of the EORTC soft tissue and bone sarcoma group |journal=Eur. J. Cancer |volume=44 |issue=16 |pages=2433–6 |date=November 2008 |pmid=18771914 |doi=10.1016/j.ejca.2008.07.037 |url=}}</ref><ref name="pmid25532684">{{cite journal |vauthors=Karanian M, Coindre JM |title=[Fourth edition of WHO classification tumours of soft tissue] |language=French |journal=Ann Pathol |volume=35 |issue=1 |pages=71–85 |date=January 2015 |pmid=25532684 |doi=10.1016/j.annpat.2014.11.003 |url=}}</ref> | ||
}}</ref> | |||
<ref>{{ | |||
}}</ref><ref>{{ | |||
}}</ref> | |||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
| colspan="2" align="center" style="background-color: #0080FF; font-weight: bold;" | Angiosarcoma | | colspan="2" align="center" style="background-color: #0080FF; font-weight: bold;" | Angiosarcoma | ||
| Line 63: | Line 24: | ||
| style="background: #F5F5F5; text-align: center;" |Angiosarcoma due to exposure to mutatgens | | style="background: #F5F5F5; text-align: center;" |Angiosarcoma due to exposure to mutatgens | ||
|- | |- | ||
| style="background: #F5F5F5; text-align: center;" |Visceral|| | | style="background: #F5F5F5; text-align: center;" |Visceral | ||
| style="background: #F5F5F5; text-align: center;" |- | |||
|- | |- | ||
|} | |} | ||
== Pathophysiology == | |||
==Pathophysiology== | *The [[pathogenesis]] of angiosarcoma is characterized by a rapid and extensive infiltrating overgrowth of [[vascular]] [[endothelial cells]].<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |date=October 2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | ||
*Angiosarcoma is a locally aggressive [[tumor]] with a high rate of [[lymph node]] infiltration and [[metastases]]. | |||
The pathogenesis of angiosarcoma is characterized by a rapid and extensive infiltrating overgrowth of vascular [[ | *Angiosarcomas demonstrate obvious unregulated vascular-specific [[receptor tyrosine kinases]] containing [[TIE1]], [[KDR]], [[TEK]] and [[FLT]]. | ||
*The up-regulation of these [[genes]] and [[over-expression]] of [[vascular]] [[endothelial]] [[growth factor receptors]] can cause [[endothelial cell]] expansion, [[angiogenesis]], and also vascular leaks in the structure of [[vessels]].<ref name="pmid14746640">{{cite journal |vauthors=Amo Y, Masuzawa M, Hamada Y, Katsuoka K |title=Serum concentrations of vascular endothelial growth factor-D in angiosarcoma patients |journal=Br. J. Dermatol. |volume=150 |issue=1 |pages=160–1 |date=January 2004 |pmid=14746640 |doi=10.1111/j.1365-2133.2004.05751.x |url=}}</ref><ref name="pmid20008140">{{cite journal |vauthors=Manner J, Radlwimmer B, Hohenberger P, Mössinger K, Küffer S, Sauer C, Belharazem D, Zettl A, Coindre JM, Hallermann C, Hartmann JT, Katenkamp D, Katenkamp K, Schöffski P, Sciot R, Wozniak A, Lichter P, Marx A, Ströbel P |title=MYC high level gene amplification is a distinctive feature of angiosarcomas after irradiation or chronic lymphedema |journal=Am. J. Pathol. |volume=176 |issue=1 |pages=34–9 |date=January 2010 |pmid=20008140 |pmc=2797867 |doi=10.2353/ajpath.2010.090637 |url=}}</ref><ref name="pmid20949568">{{cite journal |vauthors=Guo T, Zhang L, Chang NE, Singer S, Maki RG, Antonescu CR |title=Consistent MYC and FLT4 gene amplification in radiation-induced angiosarcoma but not in other radiation-associated atypical vascular lesions |journal=Genes Chromosomes Cancer |volume=50 |issue=1 |pages=25–33 |date=January 2011 |pmid=20949568 |pmc=3150534 |doi=10.1002/gcc.20827 |url=}}</ref><ref name="pmid22121953">{{cite journal |vauthors=Fernandez AP, Sun Y, Tubbs RR, Goldblum JR, Billings SD |title=FISH for MYC amplification and anti-MYC immunohistochemistry: useful diagnostic tools in the assessment of secondary angiosarcoma and atypical vascular proliferations |journal=J. Cutan. Pathol. |volume=39 |issue=2 |pages=234–42 |date=February 2012 |pmid=22121953 |doi=10.1111/j.1600-0560.2011.01843.x |url=}}</ref> | |||
The [[ | **[[KDR]] [[mutations]] are seen in primary [[breast]] angiosarcoma regardless of exposure to [[radiation]]. | ||
=== | ** High level [[MYC]] amplification is seen is seen in [[radiation]]-induced and lymphedema-associated angiosarcoma. | ||
On gross pathology, characteristic findings of angiosarcoma may include | **[[FLT4]] amplification has been detected in 25% of secondary angiosarcomas. | ||
* | {| align="right" | ||
|[[File:Angiosarcoma (5617087462) (1).jpg|thumb|right|200px|Image courtesy of Yale Rosen, contributed by Wikimedia commons]] | |||
|} | |||
On microscopic histopathological analysis, characteristic findings of angiosarcoma may include | * On [[gross pathology]], characteristic findings of angiosarcoma may include red/dark tan [[papules]] or [[noduls]], which are ytpically poorly circumscribed with central earas of [[necrosis]] and [[hemoorrhage]].<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | ||
*[[ | * On microscopic [[histopathological]] analysis, characteristic findings of angiosarcoma may include irregular anastomosing [[vascular]] spaces lined by [[endothelial] [[cells]].<ref name="pmid17998731">{{cite journal |vauthors=Mittal S, Goswami C, Kanoria N, Bhattacharya A |title=Post-irradiation angiosarcoma of bone |journal=J Cancer Res Ther |volume=3 |issue=2 |pages=96–9 |date=2007 |pmid=17998731 |doi= |url=}}</ref> | ||
*[[Endothelial cells]] have hyperchromatic or vesicular nuclei with fast [[mitotic]] activity and [[necrotic]] spots.<ref name="pmid7569134">{{cite journal |vauthors=Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS |title=From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation |journal=Radiographics |volume=15 |issue=4 |pages=893–917 |date=July 1995 |pmid=7569134 |doi=10.1148/radiographics.15.4.7569134 |url=}}</ref> | |||
*The [[tumor]] [[cells]] in solid area are characterized by a spindled appearance and contain Weibel-Palade bodies.<ref name="pmid28477885">{{cite journal |vauthors=Marušić Z, Billings SD |title=Histopathology of Spindle Cell Vascular Tumors |journal=Surg Pathol Clin |volume=10 |issue=2 |pages=345–366 |date=June 2017 |pmid=28477885 |doi=10.1016/j.path.2017.01.006 |url=}}</ref> | |||
* | *[[Immunohistochemical]] staining of spindle cells highlights [[CD31]], [[CD34]] and [[von-Willebrand factor]] related [[antigens]] which define the [[vascular]] origin of the [[tumor]] [[cells]].<ref name="pmid12150140">{{cite journal |vauthors=Kiyohara T, Kumakiri M, Kobayashl H, Itoh K, Lao LM, Ohkawara A, Nakmura H |title=Spindle cell angiosarcoma following irradiation therapy for cervical carcinoma |journal=J. Cutan. Pathol. |volume=29 |issue=2 |pages=96–100 |date=February 2002 |pmid=12150140 |doi=10.1034/j.1600-0560.2002.290206.x |url=}}</ref> | ||
*[[ | |||
==Causes== | ==Causes== | ||
*Common [[causes]] of angiosarcoma include exposure to [[vinyl chloride]] monomer (VCM) for prolonged periods, [[polyvinyl chloride]] ([[PVC]]) polymerisation plants, [[arsenic]]-containing [[insecticides]], and [[thorium dioxide]] [[irradiation]].<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | |||
==Differentiating Angiosarcoma from Other Diseases== | ==Differentiating Angiosarcoma from Other Diseases== | ||
Angiosarcoma must be differentiated from other diseases that cause a highly vascular mass or non-healing cutaneous ulcerations | *Angiosarcoma must be differentiated from other [[diseases]] that cause a highly [[vascular]] mass or non-healing [[cutaneous]] ulcerations. | ||
*Cutaneous angiosarcoma must be differentiated from other diseases with non-healing cutaneous ulcerations such as [[basal cell carcinoma]], [[keratoacanthoma]], [[nodular melanoma]], [[mycosis fungoides]], [[kaposi sarcoma]], kaposi-like hemangioendothelioma, and angiolymphoid hyperplasia.<ref name="pmid9640382">{{cite journal |vauthors=Sinclair SA, Sviland L, Natarajan S |title=Angiosarcoma arising in a chronically lymphoedematous leg |journal=Br. J. Dermatol. |volume=138 |issue=4 |pages=692–4 |date=April 1998 |pmid=9640382 |doi=10.1046/j.1365-2133.1998.02188.x |url=}}</ref><ref name="pmid18307140">{{cite journal |vauthors=de Keizer RJ, de Wolff-Rouendaal D, Nooy MA |title=Angiosarcoma of the eyelid and periorbital region. Experience in Leiden with iridium192 brachytherapy and low-dose doxorubicin chemotherapy |journal=Orbit |volume=27 |issue=1 |pages=5–12 |date=2008 |pmid=18307140 |doi=10.1080/01676830601168926 |url=}}</ref><ref name="pmid25484419">{{cite journal |vauthors=Vora R, Anjaneyan G, Gupta R |title=Cutaneous angiosarcoma of head and neck |journal=Indian J Dermatol |volume=59 |issue=6 |pages=632 |date=November 2014 |pmid=25484419 |pmc=4248527 |doi=10.4103/0019-5154.143575 |url=}}</ref> | |||
*Angiosarcoma must be differentiated from other diseases that cause a highly vascular mass such as atypical vascular lesions, [[hemangioma]], glomangiosarcoma, [[carotid body tumor]], and [[malignant fibrous histiocytoma]] of soft tissue.<ref name="pmid1718176">{{cite journal |vauthors=Fletcher CD, Beham A, Bekir S, Clarke AM, Marley NJ |title=Epithelioid angiosarcoma of deep soft tissue: a distinctive tumor readily mistaken for an epithelial neoplasm |journal=Am. J. Surg. Pathol. |volume=15 |issue=10 |pages=915–24 |date=October 1991 |pmid=1718176 |doi=10.1097/00000478-199110000-00001 |url=}}</ref> | |||
Cutaneous angiosarcoma must be differentiated from other diseases with non-healing cutaneous ulcerations such as | |||
=== | |||
Angiosarcoma must be differentiated from other diseases that cause a highly vascular mass such as | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*The [[incidence]] of angiosarcomas can be calculated approximately 1.2 per 1,000.000 person.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |date=October 2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref><ref name="pmid21793180">{{cite journal |vauthors=Ferrari A, Sultan I, Huang TT, Rodriguez-Galindo C, Shehadeh A, Meazza C, Ness KK, Casanova M, Spunt SL |title=Soft tissue sarcoma across the age spectrum: a population-based study from the Surveillance Epidemiology and End Results database |journal=Pediatr Blood Cancer |volume=57 |issue=6 |pages=943–9 |date=December 2011 |pmid=21793180 |pmc=4261144 |doi=10.1002/pbc.23252 |url=}}</ref> | |||
* | *Angiosarcoma is more commonly observed among patients aged between 40 to 75 years old.The peak age of [[incidence]] appears is the 7th decade,<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | ||
=== | |||
*Angiosarcoma is more commonly observed among patients aged between 40 to 75 years old.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | |||
*Males are more commonly affected with angiosarcoma than females.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | *Males are more commonly affected with angiosarcoma than females.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | ||
*The male to female ratio is 2:1.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | *The male to female ratio is 2:1.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | ||
*There is no racial predilection for angiosarcoma. however, African-Americans in the U.S are rarely affected.<ref name="pmid12778019">{{cite journal |vauthors=Sturgis EM, Potter BO |title=Sarcomas of the head and neck region |journal=Curr Opin Oncol |volume=15 |issue=3 |pages=239–52 |date=May 2003 |pmid=12778019 |doi=10.1097/00001622-200305000-00011 |url=}}</ref> | |||
*There is no racial predilection for angiosarcoma. | |||
==Risk Factors== | ==Risk Factors== | ||
Common risk factors in the development of angiosarcoma include | Common [[risk factors]] in the development of angiosarcoma include chronic [[lymphedema]], chronic exposure to [[polyvinyl chloride]] ([[PVC]]), [[radiation exposure]], and exposure to [[Thorotrast]].<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | ||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
* The majority of [[patients]] with angiosarcoma remain [[asymptomatic]] for years.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | |||
* The majority of patients with angiosarcoma remain asymptomatic for years.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | * Early [[clinical]] features may include nonspecific [[symptoms]], such as [[pain]], [[fatigue]], [[malaise]], and [[nausea]]. | ||
* Early clinical features may include nonspecific symptoms, such as [[pain]], [[fatigue]], [[malaise]], and [[nausea]]. | * If left untreated, the majority of [[patients]] with angiosarcoma may rapidly progress to develop [[metastases]].<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | ||
* If left untreated, the majority of patients with angiosarcoma may rapidly progress to develop [[metastases]].<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | * Common [[complications]] of angiosarcoma include [[fractures|Pathologic fractures]], [[anemia]], and [[hepatic dysfunction]].<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | ||
*[[Prognosis]] is generally poor; the 5-year survival rate of [[patients]] with angiosarcoma is approximately 12-33%. | |||
* Poor [[prognostic]] factors include [[patient]] age (> 65 years), [[retroperitoneal]] location, and large [[tumor]] size.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | |||
Common complications of angiosarcoma include | |||
*[[ | |||
* Poor prognostic factors include patient age (> 65 years), [[retroperitoneal]] location, and large [[tumor]] size.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | |||
== Diagnosis == | == Diagnosis == | ||
=== | === Diagnostic Study of Choice === | ||
* Angiosarcoma is | * There is no single [[Diagnosis|diagnostic]] study of choice for the [[diagnosis]] of angiosarcomas. | ||
* | *The [[imaging]] modality of choice for angiosarcoma or use of [[punch biopsy]] of [[skin]] will depend on the [[anatomic]] location of [[lesions]]. | ||
**[[Magnetic resonance imaging]] ([[MRI]]) is the [[imaging]] modality of choice for evaluating of suspicious [[lesions]] of the extremities, [[retroperitoneum]], or [[abdominal]] wall.<ref name="pmid28471264">{{cite journal |vauthors=Gaballah AH, Jensen CT, Palmquist S, Pickhardt PJ, Duran A, Broering G, Elsayes KM |title=Angiosarcoma: clinical and imaging features from head to toe |journal=Br J Radiol |volume=90 |issue=1075 |pages=20170039 |date=July 2017 |pmid=28471264 |pmc=5594986 |doi=10.1259/bjr.20170039 |url=}}</ref> | |||
**[[CT scan]] is useful for evaluating [[lung]], [[pleural]], and [[mediastinal]] involvement. | |||
**[[Punch biopsy]] of [[cutaneous]] [[lesions]] accompanied with [[immunohistochemical staining]] provide accurate findings for [[diagnosis]] of [[cutaneous]] angiosarcoma.<ref name="pmid17998731">{{cite journal |vauthors=Mittal S, Goswami C, Kanoria N, Bhattacharya A |title=Post-irradiation angiosarcoma of bone |journal=J Cancer Res Ther |volume=3 |issue=2 |pages=96–9 |date=2007 |pmid=17998731 |doi= |url=}}</ref><ref name="pmid12150140">{{cite journal |vauthors=Kiyohara T, Kumakiri M, Kobayashl H, Itoh K, Lao LM, Ohkawara A, Nakmura H |title=Spindle cell angiosarcoma following irradiation therapy for cervical carcinoma |journal=J. Cutan. Pathol. |volume=29 |issue=2 |pages=96–100 |date=February 2002 |pmid=12150140 |doi=10.1034/j.1600-0560.2002.290206.x |url=}}</ref> | |||
=== Staging === | |||
* According to the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) and by Enneking classification, [[soft tissue]] [[sarcomas]] are [[Classification|classified]] to different stages based on the primary [[tumor]] characteristics, [[histological]] grading and the local or [[Metastasis|distant tumor involvement]]. | |||
* Table below provides summarized information regarding staging of angiosarcoma:<ref name="pmid28128848">{{cite journal |vauthors=Lydiatt WM, Patel SG, O'Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, Loomis AM, Shah JP |title=Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual |journal=CA Cancer J Clin |volume=67 |issue=2 |pages=122–137 |date=March 2017 |pmid=28128848 |doi=10.3322/caac.21389 |url=}}</ref><ref name="pmid20333492">{{cite journal |vauthors=Jawad MU, Scully SP |title=In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system |journal=Clin. Orthop. Relat. Res. |volume=468 |issue=7 |pages=2000–2 |date=July 2010 |pmid=20333492 |pmc=2882012 |doi=10.1007/s11999-010-1315-7 |url=}}</ref> | |||
{| | |||
|+ | |||
! style="background: #4479BA; text-align: center;" |{{fontcolor|#FFF|Stage}} | |||
! style="background: #4479BA; text-align: center;" |{{fontcolor|#FFF|Grade}} | |||
! style="background: #4479BA; text-align: center;" |{{fontcolor|#FFF|Site}} | |||
! style="background: #4479BA; text-align: center;" |{{fontcolor|#FFF|Metastasis}} | |||
|- | |||
| style="background: #DCDCDC; text-align: center;" |Ia | |||
| style="background: #F5F5F5;" |Low grade (G1) | |||
| style="background: #F5F5F5; " |Intracompartmental (T1) | |||
| style="background: #F5F5F5; " |No metastasis (M0) | |||
|- | |||
| style="background: #DCDCDC; text-align: center;" |Ib | |||
| style="background: #F5F5F5;" |Low grade (G1) | |||
| style="background: #F5F5F5; " |Extracompartmental (T2) | |||
| style="background: #F5F5F5; " |No metastasis (M0) | |||
|- | |||
| style="background: #DCDCDC; text-align: center;" |IIa | |||
| style="background: #F5F5F5;" |High grade (G2) | |||
| style="background: #F5F5F5; " |Intracompartmental (T1) | |||
| style="background: #F5F5F5; " |No metastasis (M0) | |||
|- | |||
| style="background: #DCDCDC; text-align: center;" |IIb | |||
| style="background: #F5F5F5;" |High grade (G2) | |||
| style="background: #F5F5F5; " |Extracompartmental (T2) | |||
| style="background: #F5F5F5; " |No metastasis (M0) | |||
|- | |||
| style="background: #DCDCDC; text-align: center;" |IIIa | |||
| style="background: #F5F5F5;" |Low or High grade (G1-G2) | |||
| style="background: #F5F5F5; " |Intracompartmental (T1) | |||
| style="background: #F5F5F5; " |Metastasis (M1) | |||
|- | |||
| style="background: #DCDCDC; text-align: center;" |IIIb | |||
| style="background: #F5F5F5;" |Low or High grade (G1-G2) | |||
| style="background: #F5F5F5; " |Extracompartmental (T2) | |||
| style="background: #F5F5F5; " |Metastasis (M1) | |||
|} | |||
=== History and Symptoms === | |||
*Angiosarcomas occur at different [[anatomic]] sites and grow insidiously, then they can present with various misleading [[symptoms]].<ref name="YoungBrown2010">{{cite journal|last1=Young|first1=Robin J|last2=Brown|first2=Nicola J|last3=Reed|first3=Malcolm W|last4=Hughes|first4=David|last5=Woll|first5=Penella J|title=Angiosarcoma|journal=The Lancet Oncology|volume=11|issue=10|year=2010|pages=983–991|issn=14702045|doi=10.1016/S1470-2045(10)70023-1}}</ref> | |||
*The most common [[clinical]] manifestation is a gradually enlarging, painless [[mass]].<ref name="pmid28471264">{{cite journal |vauthors=Gaballah AH, Jensen CT, Palmquist S, Pickhardt PJ, Duran A, Broering G, Elsayes KM |title=Angiosarcoma: clinical and imaging features from head to toe |journal=Br J Radiol |volume=90 |issue=1075 |pages=20170039 |date=July 2017 |pmid=28471264 |pmc=5594986 |doi=10.1259/bjr.20170039 |url=}}</ref> | |||
*Some [[patients]] complain of [[pain]] or [[symptoms]] due to compression of adjacent neurovascular structures that causes [[pain]] or [[edema]] in an extremity. | |||
*Secondary angiosarcomas include [[radiation]]-Induced and lymphedema-associated angiosarcoma have a distinct feature, presenting as single or several [[Ecchymosis|ecchymotic]] [[maculopapular]] cutaneous [[lesions]] in the radiation field or in areas exposed to chronic [[lymphedema]].<ref name="pmid26617830">{{cite journal |vauthors=Cui L, Zhang J, Zhang X, Chang H, Qu C, Zhang J, Zhong D |title=Angiosarcoma (Stewart-Treves syndrome) in postmastectomy patients: report of 10 cases and review of literature |journal=Int J Clin Exp Pathol |volume=8 |issue=9 |pages=11108–15 |date=2015 |pmid=26617830 |pmc=4637645 |doi= |url=}}</ref> | |||
=== Physical Examination === | === Physical Examination === | ||
Patients with angiosarcoma may appear [[Cachexia| | * [[Patients]] with angiosarcoma may appear [[Cachexia|cachexic]] or normal. In cutaneous angiosarcoma, physical examination findings may include: | ||
* | * Primary cutaneous, [[Head and neck cancer|head and neck]] and breast angiosarcoma may present with skin thickening, [[erythema]], or [[bruise]] or [[skin ulceration]], and blushed purple-red [[papule]].<ref name="pmid7199829">{{cite journal |vauthors=Donnell RM, Rosen PP, Lieberman PH, Kaufman RJ, Kay S, Braun DW, Kinne DW |title=Angiosarcoma and other vascular tumors of the breast |journal=Am. J. Surg. Pathol. |volume=5 |issue=7 |pages=629–42 |date=October 1981 |pmid=7199829 |doi=10.1097/00000478-198110000-00005 |url=}}</ref><ref name="pmid28471264" /> | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
There are no specific laboratory findings associated with angiosarcoma. | *There are no specific laboratory findings [[Association (statistics)|associated]] with angiosarcoma. | ||
===Electrocardiogram=== | |||
*There are no [[ECG]] findings [[Association (statistics)|associated]] with angiosarcoma. | |||
===Echocardiography or Ultrasound=== | |||
*On [[ultrasound imaging]], angiosarcoma may have variable features according to the location of the [[tumor]]. It may appear as an [[echogenic]], [[nodular]], or lobulated [[mass]].<ref name="BendelMaleszewski2011">{{cite journal|last1=Bendel|first1=Emily C.|last2=Maleszewski|first2=Joseph J.|last3=Araoz|first3=Philip A.|title=Imaging Sarcomas of the Great Vessels and Heart|journal=Seminars in Ultrasound, CT and MRI|volume=32|issue=5|year=2011|pages=377–404|issn=08872171|doi=10.1053/j.sult.2011.06.001}}</ref> | |||
===X-ray=== | |||
*An [[x-ray]] may be helpful in the [[diagnosis]] of bone angiosarcoma. | |||
*Findings on an [[x-ray]] suggestive of [[diagnostic]] include solitary [[lytic]] [[lesion]], with irregular borders or a mixed [[lytic]]-sclerotic pattern.<ref name="pmid11201031">{{cite journal |vauthors=Wenger DE, Wold LE |title=Malignant vascular lesions of bone: radiologic and pathologic features |journal=Skeletal Radiol. |volume=29 |issue=11 |pages=619–31 |date=November 2000 |pmid=11201031 |doi=10.1007/s002560000261 |url=}}</ref> | |||
===Imaging Findings=== | ===Imaging Findings=== | ||
*The imaging modality of choice for angiosarcoma will depend on the location. | *The imaging modality of choice for angiosarcoma will depend on the location. | ||
*For pulmonary angiosarcoma, the imaging modality of choice is | *For pulmonary angiosarcoma, the imaging modality of choice is [[CT scan]] with [[intravenous]] contrast.<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | ||
*For other types angiosarcoma, the imaging modality of choice is [[MRI]]. | |||
On CT, findings of angiosarcoma may include | ===CT Scan=== | ||
On [[CT]], findings of angiosarcoma may include [[vascular]] [[invasion]], nodular enhancement (common), and multicentric [[lesions]].<ref name="angio">Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52</ref> | |||
===MRI=== | |||
*On [[MRI]], findings of angiosarcoma may include:<ref name="pmid28471264">{{cite journal |vauthors=Gaballah AH, Jensen CT, Palmquist S, Pickhardt PJ, Duran A, Broering G, Elsayes KM |title=Angiosarcoma: clinical and imaging features from head to toe |journal=Br J Radiol |volume=90 |issue=1075 |pages=20170039 |date=July 2017 |pmid=28471264 |pmc=5594986 |doi=10.1259/bjr.20170039 |url=}}</ref> | |||
**T1/T2: [[heterogeneous]] areas of hyperintensity suggestive of a mixed [[tumor]] and [[hemorrhage]] | |||
**T1 C+ (Gd): [[heterogeneous]] enhancement | |||
===Other Imaging Findings=== | |||
*There are no other [[imaging]] findings associated with angiosarcoma. | |||
===Other Diagnostic Studies=== | |||
*There are no other [[diagnostic]] studies associated with angiosarcoma. | |||
On MRI, findings of angiosarcoma may include: | |||
*T1/T2: heterogeneous areas of hyperintensity suggestive of a mixed | |||
*T1 C+ (Gd): heterogeneous enhancement | |||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*The | * The role of [[adjuvant chemotherapy]], is unclear. [[Adjuvant chemotherapy]] and/or [[radiotheray]] provide less mutilating surgery, and for [[patients]] with unresectable [[tumors]] or those who refuse [[surgery]] is an option.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |date=October 2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref><ref name="pmid20485141">{{cite journal |vauthors=Lahat G, Dhuka AR, Hallevi H, Xiao L, Zou C, Smith KD, Phung TL, Pollock RE, Benjamin R, Hunt KK, Lazar AJ, Lev D |title=Angiosarcoma: clinical and molecular insights |journal=Ann. Surg. |volume=251 |issue=6 |pages=1098–106 |date=June 2010 |pmid=20485141 |doi=10.1097/SLA.0b013e3181dbb75a |url=}}</ref> | ||
* | *Since angiosarcomas are [[histologically]] [[anthracycline]]-sensitive, then initial systemic [[chemotherapy]] for unresectable and/or [[metastatic]] angiosarcomas include [[doxorubicin]]-based therapy with or without [[ifosfamide]].<ref name="pmid21566149">{{cite journal |vauthors=Penel N, Italiano A, Ray-Coquard I, Chaigneau L, Delcambre C, Robin YM, Bui B, Bertucci F, Isambert N, Cupissol D, Bompas E, Bay JO, Duffaud F, Guillemet C, Blay JY |title=Metastatic angiosarcomas: doxorubicin-based regimens, weekly paclitaxel and metastasectomy significantly improve the outcome |journal=Ann. Oncol. |volume=23 |issue=2 |pages=517–23 |date=February 2012 |pmid=21566149 |doi=10.1093/annonc/mdr138 |url=}}</ref> | ||
*However, [[taxane]]-based regimen may be preferred for initial therapy. | |||
*[[Paclitaxel]] is effective for advanced angiosarcoma.<ref name="pmid15948172">{{cite journal |vauthors=Skubitz KM, Haddad PA |title=Paclitaxel and pegylated-liposomal doxorubicin are both active in angiosarcoma |journal=Cancer |volume=104 |issue=2 |pages=361–6 |date=July 2005 |pmid=15948172 |doi=10.1002/cncr.21140 |url=}}</ref> | |||
*[[Gemcitabine]]-based regimen is preferable to [[doxorubicin]] with or without [[ifosfamide]] for [[patients]] with significant clinical [[heart failure]], due to heart-[[toxicity]] of [[doxorubicin]].<ref name="pmid28794805">{{cite journal |vauthors=In GK, Hu JS, Tseng WW |title=Treatment of advanced, metastatic soft tissue sarcoma: latest evidence and clinical considerations |journal=Ther Adv Med Oncol |volume=9 |issue=8 |pages=533–550 |date=August 2017 |pmid=28794805 |pmc=5524246 |doi=10.1177/1758834017712963 |url=}}</ref> | |||
*In addition, some vascular biologic molecules, with antiangiogenic characteristics including [[bevacizumab]], [[sunitinib]], and [[sorafenib]], and with or without [[cytotoxic]] [[chemotherapy]] have shown dramatic responses in a small number of angiosarcoma [[patients]].<ref name="pmid27274393">{{cite journal |vauthors=Vo KT, Matthay KK, DuBois SG |title=Targeted antiangiogenic agents in combination with cytotoxic chemotherapy in preclinical and clinical studies in sarcoma |journal=Clin Sarcoma Res |volume=6 |issue= |pages=9 |date=2016 |pmid=27274393 |pmc=4896001 |doi=10.1186/s13569-016-0049-z |url=}}</ref> | |||
=== Surgery === | === Surgery === | ||
Surgical resection in combination with [[radiation therapy]] is the treatment of choice for small angiosarcomas.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | *The mainstay of treatment for angiosarcoma is complete [[surgical]] resection with wide margins for local and locoregional [[disease]] in combination with preoperative or postoperative [[radiotherapy]].<ref name="pmid7977971">{{cite journal |vauthors=Lydiatt WM, Shaha AR, Shah JP |title=Angiosarcoma of the head and neck |journal=Am. J. Surg. |volume=168 |issue=5 |pages=451–4 |date=November 1994 |pmid=7977971 |doi=10.1016/s0002-9610(05)80097-2 |url=}}</ref><ref name="pmid27182479">{{cite journal |vauthors=Arifi S, Belbaraka R, Rahhali R, Ismaili N |title=Treatment of Adult Soft Tissue Sarcomas: An Overview |journal=Rare Cancers Ther |volume=3 |issue= |pages=69–87 |date=2015 |pmid=27182479 |pmc=4837937 |doi=10.1007/s40487-015-0011-x |url=}}</ref> | ||
* | *[[Surgical]] resection in combination with [[radiation therapy]] is the treatment of choice for small angiosarcomas.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | ||
*Complete [[surgical]] resection with wide margins is preferred for local and locoregional angiosarcoma.<ref name="pmid20537949">{{cite journal |vauthors=Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ |title=Angiosarcoma |journal=Lancet Oncol. |volume=11 |issue=10 |pages=983–91 |year=2010 |pmid=20537949 |doi=10.1016/S1470-2045(10)70023-1 |url=}}</ref> | |||
=== | *Owing to the tendency for local infiltration, [[surgical]] resection should be associated with preoperative or postoperative [[radiotherapy]].<ref name="pmid20960566">{{cite journal |vauthors=Guadagnolo BA, Zagars GK, Araujo D, Ravi V, Shellenberger TD, Sturgis EM |title=Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp |journal=Head Neck |volume=33 |issue=5 |pages=661–7 |date=May 2011 |pmid=20960566 |pmc=4090937 |doi=10.1002/hed.21513 |url=}}</ref> | ||
*[[Surgery]] is not recommended on [[patients]] with large sized angiosarcomas. | |||
*It usually occurs after a median of six months locally or distantly and the three-year disease-free and overall [[survival rates]] both are low.<ref name="pmid23428947">{{cite journal |vauthors=Buehler D, Rice SR, Moody JS, Rush P, Hafez GR, Attia S, Longley BJ, Kozak KR |title=Angiosarcoma outcomes and prognostic factors: a 25-year single institution experience |journal=Am. J. Clin. Oncol. |volume=37 |issue=5 |pages=473–9 |date=October 2014 |pmid=23428947 |pmc=3664266 |doi=10.1097/COC.0b013e31827e4e7b |url=}}</ref><ref name="pmid22466664">{{cite journal |vauthors=Seinen JM, Styring E, Verstappen V, Vult von Steyern F, Rydholm A, Suurmeijer AJ, Hoekstra HJ |title=Radiation-associated angiosarcoma after breast cancer: high recurrence rate and poor survival despite surgical treatment with R0 resection |journal=Ann. Surg. Oncol. |volume=19 |issue=8 |pages=2700–6 |date=August 2012 |pmid=22466664 |pmc=3404270 |doi=10.1245/s10434-012-2310-x |url=}}</ref> | |||
====Primary Prevention==== | ====Primary Prevention==== | ||
There are no primary preventive measures available for angiosarcoma. | * There are no [[Primary prevention|primary preventive]] measures available for angiosarcoma. | ||
====Secondary Prevention==== | ====Secondary Prevention==== | ||
*There are no [[Secondary prevention|secondary preventive]] measures available for angiosarcoma. | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
Latest revision as of 15:27, 25 October 2019
|
WikiDoc Resources for Angiosarcoma |
|
Articles |
|---|
|
Most recent articles on Angiosarcoma Most cited articles on Angiosarcoma |
|
Media |
|
Powerpoint slides on Angiosarcoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Angiosarcoma at Clinical Trials.gov Clinical Trials on Angiosarcoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Angiosarcoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Angiosarcoma Discussion groups on Angiosarcoma Patient Handouts on Angiosarcoma Directions to Hospitals Treating Angiosarcoma Risk calculators and risk factors for Angiosarcoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Angiosarcoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Shyam Patel [2]; Associate Editor(s)-in-Chief: Mohsen Basiri M.D.
Synonyms and keywords: Hemangiosarcoma; Pulmonary angiosarcoma; Vascular sarcoma
Overview
Angiosarcoma is a rare malignant vascular neoplasm of endothelial-type cells that line vessel walls. The peak age of incidence appears to be the 7th decade, and men are affected more commonly than women. Angiosarcoma was first described by Dr. Juan Rosai, in 1976. The pathogenesis of angiosarcoma is characterized by a rapid and extensively infiltrating overgrowth of vascular endothelial cells. Angiosarcoma may arise in any part of the body, but is more common in soft tissues than in bones. Common angiosarcoma locations include the head and neck area, kidney, liver, lung, and and the most common site of radiation-induced angiosarcoma development is the breast. The PTPRB/PLCG1 genes are associated with the development of angiosarcoma; mutation of these genes result in aberrant angiogenesis. The imaging modality of choice for diagnosing angiosarcoma will depend on the location. For pulmonary angiosarcoma, the imaging modality of choice is CT scan with intravenous contrast. For other types angiosarcoma, the imaging modality of choice is MRI. On CT scan, findings suggestive of angiosarcoma may include vascular invasion, nodular enhancement (common), and a hypoattenuating mass. The mainstay adjuvant therapy for angiosarcoma is a doxorubicin-based regimen. The response rate for chemotherapy in patients with angiosarcoma is poor.
Historical Perspective
- Angiosarcoma was first discovered by Dr. Juan Rosai, M.D. and colleagues in 1976.[1]
Classification
- Angiosarcoma may be classified according to the clinical heterogeneity into two main groups, and every group can be subdivided into subtypes according to the anatomical location and etiology:[2][3][4]
| Angiosarcoma | |
| Primary | Secondary |
| Cutaneous | Post Radiation Angiosarcoma |
| Breast | Lymphedema-associated Angiosarcoma |
| Soft tissue and Bone | Angiosarcoma due to exposure to mutatgens |
| Visceral | - |
Pathophysiology
- The pathogenesis of angiosarcoma is characterized by a rapid and extensive infiltrating overgrowth of vascular endothelial cells.[5]
- Angiosarcoma is a locally aggressive tumor with a high rate of lymph node infiltration and metastases.
- Angiosarcomas demonstrate obvious unregulated vascular-specific receptor tyrosine kinases containing TIE1, KDR, TEK and FLT.
- The up-regulation of these genes and over-expression of vascular endothelial growth factor receptors can cause endothelial cell expansion, angiogenesis, and also vascular leaks in the structure of vessels.[6][7][8][9]
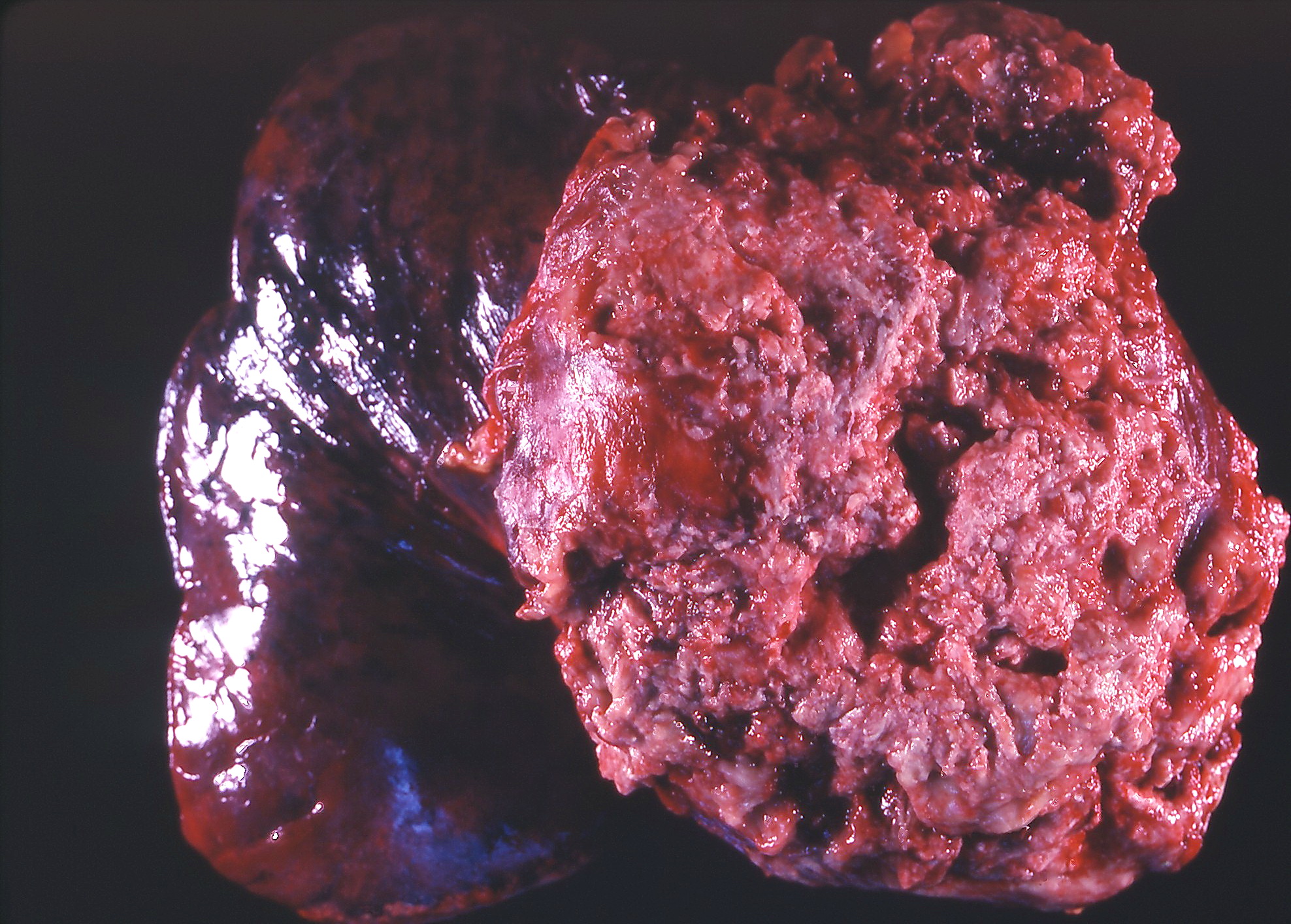 |
- On gross pathology, characteristic findings of angiosarcoma may include red/dark tan papules or noduls, which are ytpically poorly circumscribed with central earas of necrosis and hemoorrhage.[5]
- On microscopic histopathological analysis, characteristic findings of angiosarcoma may include irregular anastomosing vascular spaces lined by [[endothelial] cells.[10]
- Endothelial cells have hyperchromatic or vesicular nuclei with fast mitotic activity and necrotic spots.[11]
- The tumor cells in solid area are characterized by a spindled appearance and contain Weibel-Palade bodies.[12]
- Immunohistochemical staining of spindle cells highlights CD31, CD34 and von-Willebrand factor related antigens which define the vascular origin of the tumor cells.[13]
Causes
- Common causes of angiosarcoma include exposure to vinyl chloride monomer (VCM) for prolonged periods, polyvinyl chloride (PVC) polymerisation plants, arsenic-containing insecticides, and thorium dioxide irradiation.[5]
Differentiating Angiosarcoma from Other Diseases
- Angiosarcoma must be differentiated from other diseases that cause a highly vascular mass or non-healing cutaneous ulcerations.
- Cutaneous angiosarcoma must be differentiated from other diseases with non-healing cutaneous ulcerations such as basal cell carcinoma, keratoacanthoma, nodular melanoma, mycosis fungoides, kaposi sarcoma, kaposi-like hemangioendothelioma, and angiolymphoid hyperplasia.[14][15][16]
- Angiosarcoma must be differentiated from other diseases that cause a highly vascular mass such as atypical vascular lesions, hemangioma, glomangiosarcoma, carotid body tumor, and malignant fibrous histiocytoma of soft tissue.[17]
Epidemiology and Demographics
- The incidence of angiosarcomas can be calculated approximately 1.2 per 1,000.000 person.[5][18]
- Angiosarcoma is more commonly observed among patients aged between 40 to 75 years old.The peak age of incidence appears is the 7th decade,[19]
- Males are more commonly affected with angiosarcoma than females.[19]
- The male to female ratio is 2:1.[19]
- There is no racial predilection for angiosarcoma. however, African-Americans in the U.S are rarely affected.[20]
Risk Factors
Common risk factors in the development of angiosarcoma include chronic lymphedema, chronic exposure to polyvinyl chloride (PVC), radiation exposure, and exposure to Thorotrast.[5]
Natural History, Complications and Prognosis
- The majority of patients with angiosarcoma remain asymptomatic for years.[5]
- Early clinical features may include nonspecific symptoms, such as pain, fatigue, malaise, and nausea.
- If left untreated, the majority of patients with angiosarcoma may rapidly progress to develop metastases.[19]
- Common complications of angiosarcoma include Pathologic fractures, anemia, and hepatic dysfunction.[5]
- Prognosis is generally poor; the 5-year survival rate of patients with angiosarcoma is approximately 12-33%.
- Poor prognostic factors include patient age (> 65 years), retroperitoneal location, and large tumor size.[19]
Diagnosis
Diagnostic Study of Choice
- There is no single diagnostic study of choice for the diagnosis of angiosarcomas.
- The imaging modality of choice for angiosarcoma or use of punch biopsy of skin will depend on the anatomic location of lesions.
- Magnetic resonance imaging (MRI) is the imaging modality of choice for evaluating of suspicious lesions of the extremities, retroperitoneum, or abdominal wall.[21]
- CT scan is useful for evaluating lung, pleural, and mediastinal involvement.
- Punch biopsy of cutaneous lesions accompanied with immunohistochemical staining provide accurate findings for diagnosis of cutaneous angiosarcoma.[10][13]
Staging
- According to the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) and by Enneking classification, soft tissue sarcomas are classified to different stages based on the primary tumor characteristics, histological grading and the local or distant tumor involvement.
- Table below provides summarized information regarding staging of angiosarcoma:[22][23]
| Stage | Grade | Site | Metastasis |
|---|---|---|---|
| Ia | Low grade (G1) | Intracompartmental (T1) | No metastasis (M0) |
| Ib | Low grade (G1) | Extracompartmental (T2) | No metastasis (M0) |
| IIa | High grade (G2) | Intracompartmental (T1) | No metastasis (M0) |
| IIb | High grade (G2) | Extracompartmental (T2) | No metastasis (M0) |
| IIIa | Low or High grade (G1-G2) | Intracompartmental (T1) | Metastasis (M1) |
| IIIb | Low or High grade (G1-G2) | Extracompartmental (T2) | Metastasis (M1) |
History and Symptoms
- Angiosarcomas occur at different anatomic sites and grow insidiously, then they can present with various misleading symptoms.[24]
- The most common clinical manifestation is a gradually enlarging, painless mass.[21]
- Some patients complain of pain or symptoms due to compression of adjacent neurovascular structures that causes pain or edema in an extremity.
- Secondary angiosarcomas include radiation-Induced and lymphedema-associated angiosarcoma have a distinct feature, presenting as single or several ecchymotic maculopapular cutaneous lesions in the radiation field or in areas exposed to chronic lymphedema.[25]
Physical Examination
- Patients with angiosarcoma may appear cachexic or normal. In cutaneous angiosarcoma, physical examination findings may include:
- Primary cutaneous, head and neck and breast angiosarcoma may present with skin thickening, erythema, or bruise or skin ulceration, and blushed purple-red papule.[26][21]
Laboratory Findings
- There are no specific laboratory findings associated with angiosarcoma.
Electrocardiogram
- There are no ECG findings associated with angiosarcoma.
Echocardiography or Ultrasound
- On ultrasound imaging, angiosarcoma may have variable features according to the location of the tumor. It may appear as an echogenic, nodular, or lobulated mass.[27]
X-ray
- An x-ray may be helpful in the diagnosis of bone angiosarcoma.
- Findings on an x-ray suggestive of diagnostic include solitary lytic lesion, with irregular borders or a mixed lytic-sclerotic pattern.[28]
Imaging Findings
- The imaging modality of choice for angiosarcoma will depend on the location.
- For pulmonary angiosarcoma, the imaging modality of choice is CT scan with intravenous contrast.[19]
- For other types angiosarcoma, the imaging modality of choice is MRI.
CT Scan
On CT, findings of angiosarcoma may include vascular invasion, nodular enhancement (common), and multicentric lesions.[19]
MRI
- On MRI, findings of angiosarcoma may include:[21]
- T1/T2: heterogeneous areas of hyperintensity suggestive of a mixed tumor and hemorrhage
- T1 C+ (Gd): heterogeneous enhancement
Other Imaging Findings
- There are no other imaging findings associated with angiosarcoma.
Other Diagnostic Studies
- There are no other diagnostic studies associated with angiosarcoma.
Treatment
Medical Therapy
- The role of adjuvant chemotherapy, is unclear. Adjuvant chemotherapy and/or radiotheray provide less mutilating surgery, and for patients with unresectable tumors or those who refuse surgery is an option.[5][29]
- Since angiosarcomas are histologically anthracycline-sensitive, then initial systemic chemotherapy for unresectable and/or metastatic angiosarcomas include doxorubicin-based therapy with or without ifosfamide.[30]
- However, taxane-based regimen may be preferred for initial therapy.
- Paclitaxel is effective for advanced angiosarcoma.[31]
- Gemcitabine-based regimen is preferable to doxorubicin with or without ifosfamide for patients with significant clinical heart failure, due to heart-toxicity of doxorubicin.[32]
- In addition, some vascular biologic molecules, with antiangiogenic characteristics including bevacizumab, sunitinib, and sorafenib, and with or without cytotoxic chemotherapy have shown dramatic responses in a small number of angiosarcoma patients.[33]
Surgery
- The mainstay of treatment for angiosarcoma is complete surgical resection with wide margins for local and locoregional disease in combination with preoperative or postoperative radiotherapy.[34][35]
- Surgical resection in combination with radiation therapy is the treatment of choice for small angiosarcomas.[5]
- Complete surgical resection with wide margins is preferred for local and locoregional angiosarcoma.[5]
- Owing to the tendency for local infiltration, surgical resection should be associated with preoperative or postoperative radiotherapy.[36]
- Surgery is not recommended on patients with large sized angiosarcomas.
- It usually occurs after a median of six months locally or distantly and the three-year disease-free and overall survival rates both are low.[37][38]
Primary Prevention
- There are no primary preventive measures available for angiosarcoma.
Secondary Prevention
- There are no secondary preventive measures available for angiosarcoma.
References
- ↑ Barber W, Scriven P, Turner D, Hughes D, Wyld D (2010). "Epithelioid angiosarcoma: Use of angiographic embolisation and radiotherapy to control recurrent haemorrhage". J Surg Case Rep. 2010 (5): 7. doi:10.1093/jscr/2010.5.7. PMC 3649120. PMID 24946325.
- ↑ Fury MG, Antonescu CR, Van Zee KJ, Brennan MF, Maki RG (2005). "A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy". Cancer J. 11 (3): 241–7. PMID 16053668.
- ↑ Schlemmer M, Reichardt P, Verweij J, Hartmann JT, Judson I, Thyss A, Hogendoorn PC, Marreaud S, Van Glabbeke M, Blay JY (November 2008). "Paclitaxel in patients with advanced angiosarcomas of soft tissue: a retrospective study of the EORTC soft tissue and bone sarcoma group". Eur. J. Cancer. 44 (16): 2433–6. doi:10.1016/j.ejca.2008.07.037. PMID 18771914.
- ↑ Karanian M, Coindre JM (January 2015). "[Fourth edition of WHO classification tumours of soft tissue]". Ann Pathol (in French). 35 (1): 71–85. doi:10.1016/j.annpat.2014.11.003. PMID 25532684.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ (October 2010). "Angiosarcoma". Lancet Oncol. 11 (10): 983–91. doi:10.1016/S1470-2045(10)70023-1. PMID 20537949.
- ↑ Amo Y, Masuzawa M, Hamada Y, Katsuoka K (January 2004). "Serum concentrations of vascular endothelial growth factor-D in angiosarcoma patients". Br. J. Dermatol. 150 (1): 160–1. doi:10.1111/j.1365-2133.2004.05751.x. PMID 14746640.
- ↑ Manner J, Radlwimmer B, Hohenberger P, Mössinger K, Küffer S, Sauer C, Belharazem D, Zettl A, Coindre JM, Hallermann C, Hartmann JT, Katenkamp D, Katenkamp K, Schöffski P, Sciot R, Wozniak A, Lichter P, Marx A, Ströbel P (January 2010). "MYC high level gene amplification is a distinctive feature of angiosarcomas after irradiation or chronic lymphedema". Am. J. Pathol. 176 (1): 34–9. doi:10.2353/ajpath.2010.090637. PMC 2797867. PMID 20008140.
- ↑ Guo T, Zhang L, Chang NE, Singer S, Maki RG, Antonescu CR (January 2011). "Consistent MYC and FLT4 gene amplification in radiation-induced angiosarcoma but not in other radiation-associated atypical vascular lesions". Genes Chromosomes Cancer. 50 (1): 25–33. doi:10.1002/gcc.20827. PMC 3150534. PMID 20949568.
- ↑ Fernandez AP, Sun Y, Tubbs RR, Goldblum JR, Billings SD (February 2012). "FISH for MYC amplification and anti-MYC immunohistochemistry: useful diagnostic tools in the assessment of secondary angiosarcoma and atypical vascular proliferations". J. Cutan. Pathol. 39 (2): 234–42. doi:10.1111/j.1600-0560.2011.01843.x. PMID 22121953.
- ↑ 10.0 10.1 Mittal S, Goswami C, Kanoria N, Bhattacharya A (2007). "Post-irradiation angiosarcoma of bone". J Cancer Res Ther. 3 (2): 96–9. PMID 17998731.
- ↑ Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS (July 1995). "From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation". Radiographics. 15 (4): 893–917. doi:10.1148/radiographics.15.4.7569134. PMID 7569134.
- ↑ Marušić Z, Billings SD (June 2017). "Histopathology of Spindle Cell Vascular Tumors". Surg Pathol Clin. 10 (2): 345–366. doi:10.1016/j.path.2017.01.006. PMID 28477885.
- ↑ 13.0 13.1 Kiyohara T, Kumakiri M, Kobayashl H, Itoh K, Lao LM, Ohkawara A, Nakmura H (February 2002). "Spindle cell angiosarcoma following irradiation therapy for cervical carcinoma". J. Cutan. Pathol. 29 (2): 96–100. doi:10.1034/j.1600-0560.2002.290206.x. PMID 12150140.
- ↑ Sinclair SA, Sviland L, Natarajan S (April 1998). "Angiosarcoma arising in a chronically lymphoedematous leg". Br. J. Dermatol. 138 (4): 692–4. doi:10.1046/j.1365-2133.1998.02188.x. PMID 9640382.
- ↑ de Keizer RJ, de Wolff-Rouendaal D, Nooy MA (2008). "Angiosarcoma of the eyelid and periorbital region. Experience in Leiden with iridium192 brachytherapy and low-dose doxorubicin chemotherapy". Orbit. 27 (1): 5–12. doi:10.1080/01676830601168926. PMID 18307140.
- ↑ Vora R, Anjaneyan G, Gupta R (November 2014). "Cutaneous angiosarcoma of head and neck". Indian J Dermatol. 59 (6): 632. doi:10.4103/0019-5154.143575. PMC 4248527. PMID 25484419.
- ↑ Fletcher CD, Beham A, Bekir S, Clarke AM, Marley NJ (October 1991). "Epithelioid angiosarcoma of deep soft tissue: a distinctive tumor readily mistaken for an epithelial neoplasm". Am. J. Surg. Pathol. 15 (10): 915–24. doi:10.1097/00000478-199110000-00001. PMID 1718176.
- ↑ Ferrari A, Sultan I, Huang TT, Rodriguez-Galindo C, Shehadeh A, Meazza C, Ness KK, Casanova M, Spunt SL (December 2011). "Soft tissue sarcoma across the age spectrum: a population-based study from the Surveillance Epidemiology and End Results database". Pediatr Blood Cancer. 57 (6): 943–9. doi:10.1002/pbc.23252. PMC 4261144. PMID 21793180.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003 May. 15(3):239-52
- ↑ Sturgis EM, Potter BO (May 2003). "Sarcomas of the head and neck region". Curr Opin Oncol. 15 (3): 239–52. doi:10.1097/00001622-200305000-00011. PMID 12778019.
- ↑ 21.0 21.1 21.2 21.3 Gaballah AH, Jensen CT, Palmquist S, Pickhardt PJ, Duran A, Broering G, Elsayes KM (July 2017). "Angiosarcoma: clinical and imaging features from head to toe". Br J Radiol. 90 (1075): 20170039. doi:10.1259/bjr.20170039. PMC 5594986. PMID 28471264.
- ↑ Lydiatt WM, Patel SG, O'Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, Loomis AM, Shah JP (March 2017). "Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual". CA Cancer J Clin. 67 (2): 122–137. doi:10.3322/caac.21389. PMID 28128848.
- ↑ Jawad MU, Scully SP (July 2010). "In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system". Clin. Orthop. Relat. Res. 468 (7): 2000–2. doi:10.1007/s11999-010-1315-7. PMC 2882012. PMID 20333492.
- ↑ Young, Robin J; Brown, Nicola J; Reed, Malcolm W; Hughes, David; Woll, Penella J (2010). "Angiosarcoma". The Lancet Oncology. 11 (10): 983–991. doi:10.1016/S1470-2045(10)70023-1. ISSN 1470-2045.
- ↑ Cui L, Zhang J, Zhang X, Chang H, Qu C, Zhang J, Zhong D (2015). "Angiosarcoma (Stewart-Treves syndrome) in postmastectomy patients: report of 10 cases and review of literature". Int J Clin Exp Pathol. 8 (9): 11108–15. PMC 4637645. PMID 26617830.
- ↑ Donnell RM, Rosen PP, Lieberman PH, Kaufman RJ, Kay S, Braun DW, Kinne DW (October 1981). "Angiosarcoma and other vascular tumors of the breast". Am. J. Surg. Pathol. 5 (7): 629–42. doi:10.1097/00000478-198110000-00005. PMID 7199829.
- ↑ Bendel, Emily C.; Maleszewski, Joseph J.; Araoz, Philip A. (2011). "Imaging Sarcomas of the Great Vessels and Heart". Seminars in Ultrasound, CT and MRI. 32 (5): 377–404. doi:10.1053/j.sult.2011.06.001. ISSN 0887-2171.
- ↑ Wenger DE, Wold LE (November 2000). "Malignant vascular lesions of bone: radiologic and pathologic features". Skeletal Radiol. 29 (11): 619–31. doi:10.1007/s002560000261. PMID 11201031.
- ↑ Lahat G, Dhuka AR, Hallevi H, Xiao L, Zou C, Smith KD, Phung TL, Pollock RE, Benjamin R, Hunt KK, Lazar AJ, Lev D (June 2010). "Angiosarcoma: clinical and molecular insights". Ann. Surg. 251 (6): 1098–106. doi:10.1097/SLA.0b013e3181dbb75a. PMID 20485141.
- ↑ Penel N, Italiano A, Ray-Coquard I, Chaigneau L, Delcambre C, Robin YM, Bui B, Bertucci F, Isambert N, Cupissol D, Bompas E, Bay JO, Duffaud F, Guillemet C, Blay JY (February 2012). "Metastatic angiosarcomas: doxorubicin-based regimens, weekly paclitaxel and metastasectomy significantly improve the outcome". Ann. Oncol. 23 (2): 517–23. doi:10.1093/annonc/mdr138. PMID 21566149.
- ↑ Skubitz KM, Haddad PA (July 2005). "Paclitaxel and pegylated-liposomal doxorubicin are both active in angiosarcoma". Cancer. 104 (2): 361–6. doi:10.1002/cncr.21140. PMID 15948172.
- ↑ In GK, Hu JS, Tseng WW (August 2017). "Treatment of advanced, metastatic soft tissue sarcoma: latest evidence and clinical considerations". Ther Adv Med Oncol. 9 (8): 533–550. doi:10.1177/1758834017712963. PMC 5524246. PMID 28794805.
- ↑ Vo KT, Matthay KK, DuBois SG (2016). "Targeted antiangiogenic agents in combination with cytotoxic chemotherapy in preclinical and clinical studies in sarcoma". Clin Sarcoma Res. 6: 9. doi:10.1186/s13569-016-0049-z. PMC 4896001. PMID 27274393.
- ↑ Lydiatt WM, Shaha AR, Shah JP (November 1994). "Angiosarcoma of the head and neck". Am. J. Surg. 168 (5): 451–4. doi:10.1016/s0002-9610(05)80097-2. PMID 7977971.
- ↑ Arifi S, Belbaraka R, Rahhali R, Ismaili N (2015). "Treatment of Adult Soft Tissue Sarcomas: An Overview". Rare Cancers Ther. 3: 69–87. doi:10.1007/s40487-015-0011-x. PMC 4837937. PMID 27182479.
- ↑ Guadagnolo BA, Zagars GK, Araujo D, Ravi V, Shellenberger TD, Sturgis EM (May 2011). "Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp". Head Neck. 33 (5): 661–7. doi:10.1002/hed.21513. PMC 4090937. PMID 20960566.
- ↑ Buehler D, Rice SR, Moody JS, Rush P, Hafez GR, Attia S, Longley BJ, Kozak KR (October 2014). "Angiosarcoma outcomes and prognostic factors: a 25-year single institution experience". Am. J. Clin. Oncol. 37 (5): 473–9. doi:10.1097/COC.0b013e31827e4e7b. PMC 3664266. PMID 23428947.
- ↑ Seinen JM, Styring E, Verstappen V, Vult von Steyern F, Rydholm A, Suurmeijer AJ, Hoekstra HJ (August 2012). "Radiation-associated angiosarcoma after breast cancer: high recurrence rate and poor survival despite surgical treatment with R0 resection". Ann. Surg. Oncol. 19 (8): 2700–6. doi:10.1245/s10434-012-2310-x. PMC 3404270. PMID 22466664.