Ambrisentan: Difference between revisions
No edit summary |
No edit summary |
||
| (27 intermediate revisions by the same user not shown) | |||
| Line 12: | Line 12: | ||
|aOrAn= | |aOrAn= | ||
an | |||
|drugClass= | |drugClass= | ||
| Line 28: | Line 28: | ||
|adverseReactions= | |adverseReactions= | ||
[[edema]], decreased [[hemoglobin]], and [[headache]] | |||
<!--Black Box Warning--> | <!--Black Box Warning--> | ||
|blackBoxWarningTitle= | |blackBoxWarningTitle= | ||
WARNING: EMBRYO-FETAL TOXICITY | |||
|blackBoxWarningBody= | |blackBoxWarningBody= | ||
* Do not administer Letairis to a pregnant female because it may cause fetal harm. Letairis is very likely to produce serious birth defects if used by pregnant females, as this effect has been seen consistently when it is administered to animals. | |||
* Exclude pregnancy before the initiation of treatment with Letairis. Females of reproductive potential must use acceptable methods of contraception during treatment with Letairis and for one month after treatment. Obtain monthly pregnancy tests during treatment and 1 month after discontinuation of treatment. | |||
* | * Because of the risk of embryo-fetal toxicity, females can only receive Letairis through a restricted program called the Letairis REMS program. | ||
<!--Adult Indications and Dosage--> | <!--Adult Indications and Dosage--> | ||
| Line 46: | Line 46: | ||
|fdaLIADAdult= | |fdaLIADAdult= | ||
===== | =====Pulmonary Arterial Hypertension===== | ||
* Letairis is indicated for the treatment of [[pulmonary arterial hypertension]] (PAH) (WHO Group 1) to improve exercise ability and delay clinical worsening. Studies establishing effectiveness included predominantly patients with WHO Functional Class II–III symptoms and etiologies of idiopathic or heritable PAH (64%) or PAH associated with connective tissue diseases (32%). | |||
* Dosing Information | * Dosing Information | ||
:* Initiate treatment at 5 mg once daily, and consider increasing the dose to 10 mg once daily if 5 mg is tolerated. | |||
:* Tablets may be administered with or without food. Tablets should not be split, crushed, or chewed. Doses higher than 10 mg once daily have not been studied in patients with [[pulmonary arterial hypertension]] (PAH). | |||
======Pregnancy Testing in Females of Reproductive Potential====== | |||
===== | |||
* Initiate treatment with Letairis in females of reproductive potential only after a negative pregnancy test. Obtain monthly pregnancy tests during treatment. | |||
<!--Off-Label Use and Dosage (Adult)--> | <!--Off-Label Use and Dosage (Adult)--> | ||
| Line 75: | Line 63: | ||
|offLabelAdultGuideSupport= | |offLabelAdultGuideSupport= | ||
There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | ||
| Line 95: | Line 69: | ||
|offLabelAdultNoGuideSupport= | |offLabelAdultNoGuideSupport= | ||
There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | ||
| Line 112: | Line 78: | ||
|fdaLIADPed= | |fdaLIADPed= | ||
* Safety and effectiveness of Letairis in pediatric patients have not been established. | |||
* | |||
<!--Off-Label Use and Dosage (Pediatric)--> | <!--Off-Label Use and Dosage (Pediatric)--> | ||
| Line 127: | Line 85: | ||
|offLabelPedGuideSupport= | |offLabelPedGuideSupport= | ||
There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | ||
| Line 147: | Line 91: | ||
|offLabelPedNoGuideSupport= | |offLabelPedNoGuideSupport= | ||
There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | ||
| Line 162: | Line 98: | ||
|contraindications= | |contraindications= | ||
* | * Pregnancy | ||
:* Letairis may cause fetal harm when administered to a pregnant female. Letairis is contraindicated in females who are pregnant. Letairis was consistently shown to have teratogenic effects when administered to animals. If this drug is used during [[pregnancy]], or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus. | |||
* Idiopathic Pulmonary Fibrosis | |||
:* Letairis is contraindicated in patients with [[idiopathic pulmonary fibrosis]] (IPF), including IPF patients with [[pulmonary hypertension]] (WHO Group 3) | |||
<!--Warnings--> | <!--Warnings--> | ||
| Line 168: | Line 107: | ||
|warnings= | |warnings= | ||
* | ======Embryo-fetal Toxicity====== | ||
* Letairis may cause fetal harm when administered during [[pregnancy]] and is contraindicated for use in females who are pregnant. In females of reproductive potential, exclude pregnancy prior to initiation of therapy, ensure use of acceptable contraceptive methods, and obtain monthly [[pregnancy]] tests. | |||
* Letairis is only available for females through a restricted program under a REMS. | |||
======Letairis REMS Program====== | |||
* For all females, Letairis is available only through a restricted program called the Letairis REMS, because of the risk of embryo-fetal toxicity. | |||
* Notable requirements of the Letairis REMS program include the following: | |||
:* Prescribers must be certified with the program by enrolling and completing training. | |||
:* All females, regardless of reproductive potential, must enroll in the Letairis REMS program prior to initiating Letairis. Male patients are not enrolled in the REMS. | |||
::* Females of reproductive potential must comply with the [[pregnancy]] testing and contraception requirements. | |||
:* Pharmacies that dispense Letairis must be certified with the program and must dispense to female patients who are authorized to receive Letairis. | |||
* Further information is available at www.letairisrems.com or 1-866-664-5327. | |||
======Fluid Retention====== | |||
* Peripheral edema is a known class effect of [[endothelin]] receptor antagonists, and is also a clinical consequence of PAH and worsening PAH. In the placebo-controlled studies, there was an increased incidence of peripheral edema in patients treated with doses of 5 or 10 mg Letairis compared to placebo. Most edema was mild to moderate in severity, and it occurred with greater frequency and severity in elderly patients. | |||
* In addition, there have been postmarketing reports of fluid retention in patients with [[pulmonary hypertension]], occurring within weeks after starting Letairis. Patients required intervention with a diuretic, fluid management, or, in some cases, hospitalization for decompensating heart failure. | |||
* If clinically significant fluid retention develops, with or without associated weight gain, further evaluation should be undertaken to determine the cause, such as Letairis or underlying heart failure, and the possible need for specific treatment or discontinuation of Letairis therapy. | |||
======Pulmonary Edema with Pulmonary Veno-occlusive Disease (PVOD)====== | |||
* If patients develop acute [[pulmonary edema]] during initiation of therapy with vasodilating agents such as Letairis, the possibility of PVOD should be considered, and if confirmed Letairis should be discontinued. | |||
==== | ======Decreased Sperm Counts====== | ||
* Decreased sperm counts have been observed in human and animal studies with another [[endothelin receptor antagonist]] and in animal fertility studies with ambrisentan. Letairis may have an adverse effect on [[spermatogenesis]]. Counsel patients about potential effects on fertility. | |||
* | ======Hematological Changes====== | ||
* Decreases in hemoglobin concentration and hematocrit have followed administration of other endothelin receptor antagonists and were observed in clinical studies with Letairis. These decreases were observed within the first few weeks of treatment with Letairis, and stabilized thereafter. The mean decrease in [[hemoglobin]] from baseline to end of treatment for those patients receiving Letairis in the 12-week placebo-controlled studies was 0.8 g/dL. | |||
* Marked decreases in hemoglobin (>15% decrease from baseline resulting in a value below the lower limit of normal) were observed in 7% of all patients receiving Letairis (and 10% of patients receiving 10 mg) compared to 4% of patients receiving placebo. The cause of the decrease in [[hemoglobin]] is unknown, but it does not appear to result from [[hemorrhage]] or [[hemolysis]]. | |||
* In the long-term open-label extension of the two pivotal clinical studies, mean decreases from baseline (ranging from 0.9 to 1.2 g/dL) in [[hemoglobin]] concentrations persisted for up to 4 years of treatment. | |||
* There have been postmarketing reports of decreases in [[hemoglobin]] concentration and hematocrit that have resulted in [[anemia]] requiring [[transfusion]]. | |||
* Measure hemoglobin prior to initiation of Letairis, at one month, and periodically thereafter. Initiation of Letairis therapy is not recommended for patients with clinically significant [[anemia]]. If a clinically significant decrease in [[hemoglobin]] is observed and other causes have been excluded, consider discontinuing Letairis. | |||
<!--Adverse Reactions--> | <!--Adverse Reactions--> | ||
| Line 180: | Line 144: | ||
|clinicalTrials= | |clinicalTrials= | ||
* Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |||
* Safety data for Letairis were obtained from two 12-week, placebo-controlled studies in patients with [[pulmonary arterial hypertension]] ([[pulmonary arterial hypertension|PAH]]) (ARIES-1 and ARIES-2) and four nonplacebo-controlled studies in 483 patients with [[pulmonary arterial hypertension|PAH]] who were treated with doses of 1, 2.5, 5, or 10 mg once daily. The exposure to Letairis in these studies ranged from 1 day to 4 years (N = 418 for at least 6 months and N = 343 for at least 1 year). | |||
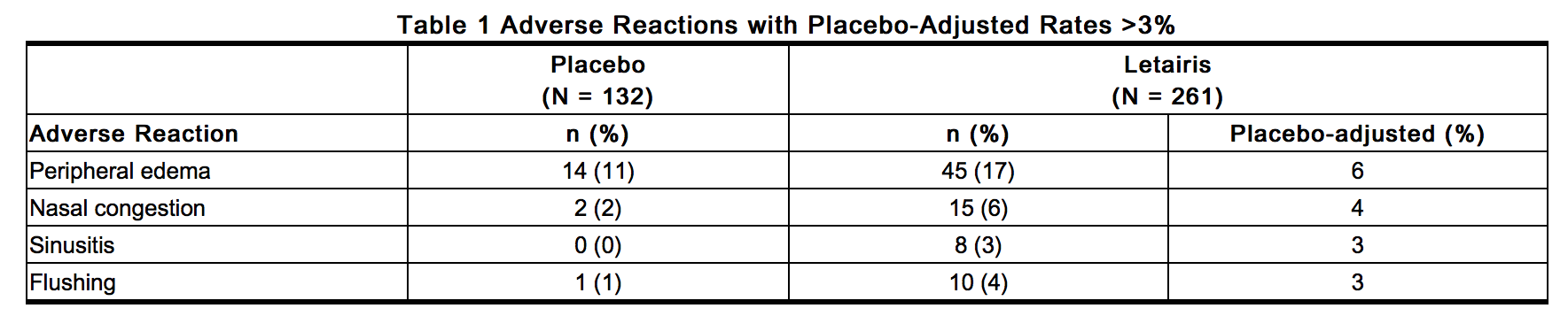
* In ARIES-1 and ARIES-2, a total of 261 patients received Letairis at doses of 2.5, 5, or 10 mg once daily and 132 patients received placebo. The adverse reactions that occurred in >3% more patients receiving Letairis than receiving placebo are shown in Table 1. | |||
: [[File:{{PAGENAME}}02.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
* Most adverse drug reactions were mild to moderate and only nasal congestion was dose-dependent. | |||
* Few notable differences in the incidence of adverse reactions were observed for patients by age or sex. Peripheral edema was similar in younger patients (<65 years) receiving Letairis (14%; 29/205) or placebo (13%; 13/104), and was greater in elderly patients (≥65 years) receiving Letairis (29%; 16/56) compared to placebo (4%; 1/28). The results of such subgroup analyses must be interpreted cautiously. | |||
* The incidence of treatment discontinuations due to adverse events other than those related to [[pulmonary arterial hypertension|PAH]] during the clinical trials in patients with [[pulmonary arterial hypertension|PAH]] was similar for Letairis (2%; 5/261 patients) and placebo (2%; 3/132 patients). The incidence of patients with serious adverse events other than those related to [[pulmonary arterial hypertension|PAH]] during the clinical trials in patients with [[pulmonary arterial hypertension|PAH]] was similar for placebo (7%; 9/132 patients) and for Letairis (5%; 13/261 patients). | |||
* During 12-week controlled clinical trials, the incidence of [[aminotransferase]] elevations >3 × upper limit of normal (ULN) were 0% on Letairis and 2.3% on placebo. In practice, cases of hepatic injury should be carefully evaluated for cause. | |||
=====Use in Patients with Prior Endothelin Receptor Antagonist (ERA) Related Serum Liver Enzyme Abnormalities===== | |||
* In an uncontrolled, open-label study, 36 patients who had previously discontinued endothelin receptor antagonists (ERAs: bosentan, an investigational drug, or both) due to [[aminotransferase]] elevations >3 × ULN were treated with Letairis. Prior elevations were predominantly moderate, with 64% of the ALT elevations <5 × ULN, but 9 patients had elevations >8 × ULN. Eight patients had been re-challenged with bosentan and/or the investigational ERA and all eight had a recurrence of [[aminotransferase]] abnormalities that required discontinuation of ERA therapy. All patients had to have normal aminotransferase levels on entry to this study. Twenty-five of the 36 patients were also receiving prostanoid and/or [[phosphodiesterase]] type 5 (PDE5) inhibitor therapy. Two patients discontinued early (including one of the patients with a prior 8 × ULN elevation). Of the remaining 34 patients, one patient experienced a mild [[aminotransferase]] elevation at 12 weeks on Letairis 5 mg that resolved with decreasing the dosage to 2.5 mg, and that did not recur with later escalations to 10 mg. With a median follow-up of 13 months and with 50% of patients increasing the dose of Letairis to 10 mg, no patients were discontinued for [[aminotransferase]] elevations. While the uncontrolled study design does not provide information about what would have occurred with re-administration of previously used ERAs or show that Letairis led to fewer [[aminotransferase]] elevations than would have been seen with those drugs, the study indicates that Letairis may be tried in patients who have experienced asymptomatic [[aminotransferase]] elevations on other ERAs after [[aminotransferase]] levels have returned to normal. | |||
<!--Postmarketing Experience--> | <!--Postmarketing Experience--> | ||
|postmarketing= | |postmarketing= | ||
* The following adverse reactions were identified during postapproval use of Letairis. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to estimate reliably the frequency or to establish a causal relationship to drug exposure: [[anemia]], [[heart failure]] (associated with fluid retention), [[hypersensitivity]] (eg, [[angioedema]], [[rash]]), [[nausea]], and [[vomiting]]. | |||
* Elevations of liver [[aminotransferase]]s (ALT, AST) have been reported with Letairis use; in most cases alternative causes of the liver injury could be identified (heart failure, hepatic congestion, hepatitis, alcohol use, hepatotoxic medications). Other endothelin receptor antagonists have been associated with elevations of [[aminotransferase]]s, [[hepatotoxicity]], and cases of [[liver failure]]. | |||
<!--Drug Interactions--> | |||
|drugInteractions= | |||
* Multiple dose coadministration of ambrisentan and cyclosporine resulted in an approximately 2-fold increase in ambrisentan exposure in healthy volunteers; therefore, limit the dose of ambrisentan to 5 mg once daily when coadministered with cyclosporine. | |||
======In Vitro Studies====== | |||
* Studies with human liver tissue indicate that ambrisentan is metabolized by CYP3A, CYP2C19, and uridine 5'-diphosphate glucuronosyltransferases (UGTs) 1A9S, 2B7S, and 1A3S. In vitro studies suggest that ambrisentan is a substrate of the Organic Anion Transporting Polypeptides OATP1B1 and OATP1B3, and [[P-glycoprotein]] (P-gp). Drug interactions might be expected because of these factors; however, a clinically relevant interaction has been demonstrated only with cyclosporine. In vitro studies found ambrisentan to have little to no inhibition of human hepatic transporters. Ambrisentan demonstrated weak dose-dependent inhibition of OATP1B1, OATP1B3, and NTCP (IC50 of 47 µM, 45 µM, and approximately 100 µM, respectively) and no transporter-specific inhibition of BSEP, BRCP, P-gp, or MRP2. Ambrisentan does not inhibit or induce drug metabolizing enzymes at clinically relevant concentrations. | |||
======In Vivo Studies====== | |||
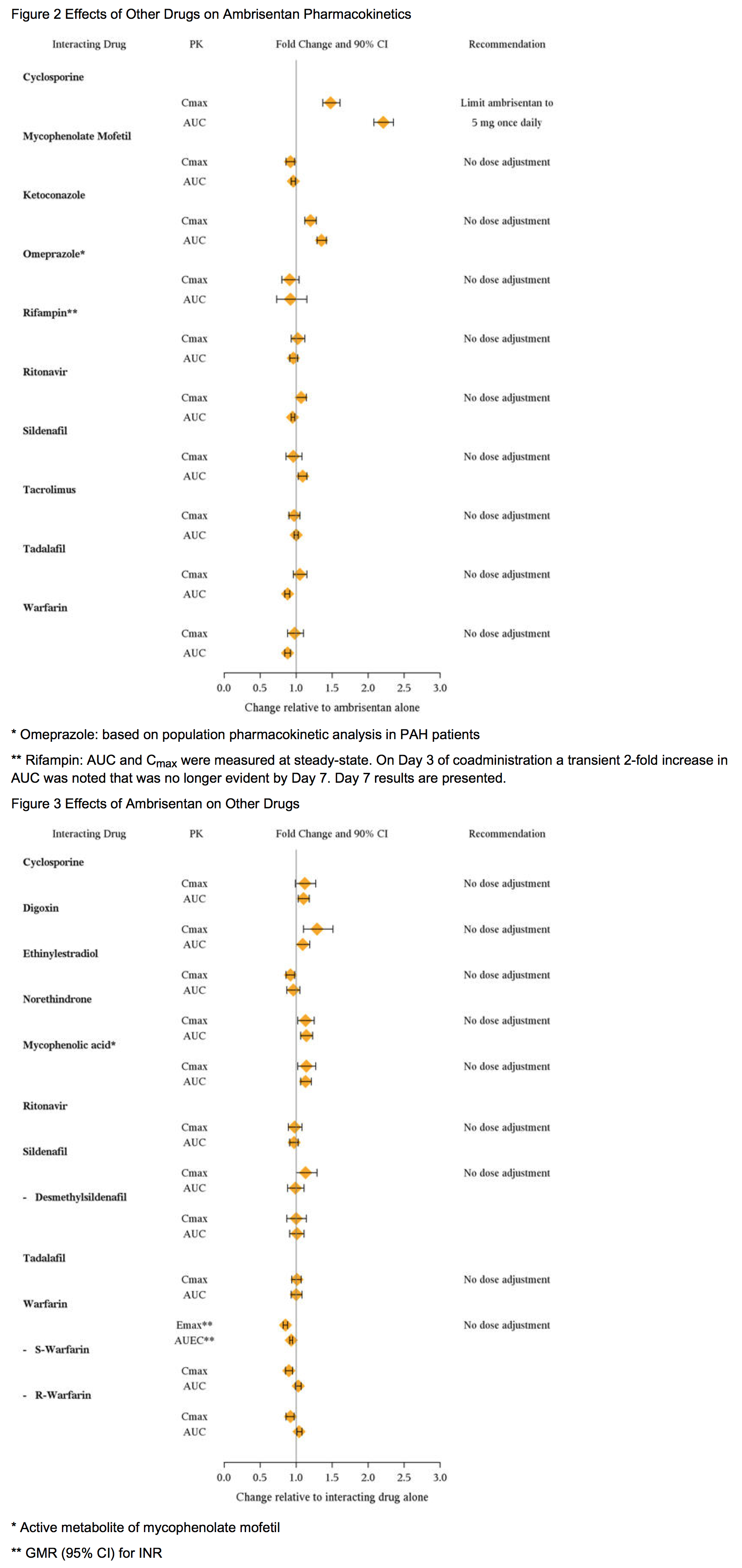
* The effects of other drugs on ambrisentan pharmacokinetics and the effects of ambrisentan on the exposure to other drugs are shown in Figure 2 and Figure 3, respectively. | |||
: [[File:{{PAGENAME}}03.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
| | |||
<!--Use in Specific Populations--> | <!--Use in Specific Populations--> | ||
|useInPregnancyFDA= | |useInPregnancyFDA= | ||
* '''Pregnancy Category''' | * '''Pregnancy Category X''' | ||
:* Risk Summary | |||
::* Letairis may cause fetal harm when administered to a pregnant woman and is contraindicated during pregnancy. Letairis was teratogenic in rats and rabbits at doses which resulted in exposures of 3.5 and 1.7 times, respectively, the human dose of 10 mg per day. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, advise the patient of the potential hazard to a fetus. | |||
:* Animal Data | |||
::* Letairis was teratogenic at oral doses of ≥ 15 mg/kg/day (AUC 51.7 h•µg/mL) in rats and ≥ 7 mg/kg/day (24.7 h•µg/mL) in rabbits; it was not studied at lower doses. These doses are of 3.5 and 1.7 times, respectively, the human dose of 10 mg per day (14.8 h•µg/mL) based on AUC. In both species, there were abnormalities of the lower jaw and hard and soft palate, malformation of the heart and great vessels, and failure of formation of the thymus and thyroid. | |||
::* A preclinical study in rats has shown decreased survival of newborn pups (mid and high doses) and effects on testicle size and fertility of pups (high dose) following maternal treatment with ambrisentan from late gestation through weaning. Doses tested were 17 ×, 51 ×, and 170 × (on a mg/kg:mg/m2 basis) the maximum oral human dose of 10 mg and an average adult body weight of 70 kg. | |||
|useInPregnancyAUS= | |useInPregnancyAUS= | ||
* '''Australian Drug Evaluation Committee (ADEC) Pregnancy Category''' | * '''Australian Drug Evaluation Committee (ADEC) Pregnancy Category''' | ||
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | ||
|useInLaborDelivery= | |useInLaborDelivery= | ||
There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | ||
|useInNursing= | |useInNursing= | ||
* It is not known whether ambrisentan is present in human milk. Because many drugs are present in human milk and because of the potential for serious adverse reactions in nursing infants from Letairis, a decision should be made whether to discontinue nursing or discontinue Letairis, taking into account the importance of the drug to the mother. | |||
|useInPed= | |useInPed= | ||
* Safety and effectiveness of Letairis in pediatric patients have not been established. | |||
|useInGeri= | |useInGeri= | ||
* In the two placebo-controlled clinical studies of Letairis, 21% of patients were ≥65 years old and 5% were ≥75 years old. The elderly (age ≥65 years) showed less improvement in walk distances with Letairis than younger patients did, but the results of such subgroup analyses must be interpreted cautiously. Peripheral edema was more common in the elderly than in younger patients. | |||
|useInGender= | |useInGender= | ||
There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | ||
|useInRace= | |useInRace= | ||
There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | ||
|useInRenalImpair= | |useInRenalImpair= | ||
There is no | * The impact of renal impairment on the pharmacokinetics of ambrisentan has been examined using a population pharmacokinetic approach in [[pulmonary arterial hypertension|PAH]] patients with creatinine clearances ranging between 20 and 150 mL/min. There was no significant impact of mild or moderate renal impairment on exposure to ambrisentan. Dose adjustment of Letairis in patients with mild or moderate renal impairment is therefore not required. There is no information on the exposure to ambrisentan in patients with severe renal impairment. | ||
* The impact of hemodialysis on the disposition of ambrisentan has not been investigated. | |||
|useInHepaticImpair= | |useInHepaticImpair= | ||
There is no | * Pre-existing Hepatic Impairment | ||
:* The influence of pre-existing hepatic impairment on the pharmacokinetics of ambrisentan has not been evaluated. Because there is in vitro and in vivo evidence of significant metabolic and biliary contribution to the elimination of ambrisentan, hepatic impairment might be expected to have significant effects on the pharmacokinetics of ambrisentan. Letairis is not recommended in patients with moderate or severe hepatic impairment. There is no information on the use of Letairis in patients with mild pre-existing impaired liver function; however, exposure to ambrisentan may be increased in these patients. | |||
* Elevation of Liver Transaminases | |||
:* Other endothelin receptor antagonists (ERAs) have been associated with aminotransferase (AST, ALT) elevations, hepatotoxicity, and cases of liver failure. In patients who develop hepatic impairment after Letairis initiation, the cause of liver injury should be fully investigated. Discontinue Letairis if elevations of liver aminotransferases are >5 × ULN or if elevations are accompanied by bilirubin >2 × ULN, or by signs or symptoms of liver dysfunction and other causes are excluded. | |||
|useInReproPotential= | |||
* Pregnancy Testing | |||
:* Female patients of reproductive potential must have a negative pregnancy test prior to initiation of treatment, monthly pregnancy test during treatment, and 1 month after stopping treatment with Letairis. Advise patients to contact their healthcare provider if they become pregnant or suspect they may be pregnant. Perform a pregnancy test if pregnancy is suspected for any reason. For positive pregnancy tests, counsel patient on the potential risk to the fetus and patient options. | |||
* Contraception | |||
:* Female patients of reproductive potential must use acceptable methods of contraception during treatment with Letairis and for 1 month after stopping treatment with Letairis. Patients may choose one highly effective form of contraception (intrauterine device (IUD), contraceptive implant, or tubal sterilization) or a combination of methods (hormone method with a barrier method or two barrier methods). If a partner's vasectomy is the chosen method of contraception, a hormone or barrier method must be used along with this method. Counsel patients on pregnancy planning and prevention, including emergency contraception, or designate counseling by another healthcare provider trained in contraceptive counseling. | |||
* Infertility in Males | |||
:* In a 6-month study of another endothelin receptor antagonist, bosentan, 25 male patients with WHO functional class III and IV [[pulmonary arterial hypertension|PAH]] and normal baseline sperm count were evaluated for effects on testicular function. There was a decline in sperm count of at least 50% in 25% of the patients after 3 or 6 months of treatment with bosentan. One patient developed marked oligospermia at 3 months, and the sperm count remained low with 2 follow-up measurements over the subsequent 6 weeks. Bosentan was discontinued and after 2 months the sperm count had returned to baseline levels. In 22 patients who completed 6 months of treatment, sperm count remained within the normal range and no changes in sperm morphology, sperm motility, or hormone levels were observed. Based on these findings and preclinical data from endothelin receptor antagonists, it cannot be excluded that endothelin receptor antagonists such as Letairis have an adverse effect on spermatogenesis. Counsel patients about the potential effects on fertility. | |||
|useInImmunocomp= | |useInImmunocomp= | ||
There is no FDA guidance one the use of {{PAGENAME}} in patients who are immunocompromised. | There is no FDA guidance one the use of {{PAGENAME}} in patients who are immunocompromised. | ||
<!--Administration and Monitoring--> | <!--Administration and Monitoring--> | ||
|administration= | |administration= | ||
* Oral | * Oral | ||
|monitoring= | |monitoring= | ||
There is limited information regarding <i>Monitoring</i> of {{PAGENAME}} in the drug label. | There is limited information regarding <i>Monitoring</i> of {{PAGENAME}} in the drug label. | ||
<!--IV Compatibility--> | <!--IV Compatibility--> | ||
|IVCompat= | |IVCompat= | ||
| Line 372: | Line 235: | ||
<!--Overdosage--> | <!--Overdosage--> | ||
|overdose= | |overdose= | ||
===Acute Overdose=== | ===Acute Overdose=== | ||
* There is no experience with overdosage of Letairis. The highest single dose of Letairis administered to healthy volunteers was 100 mg, and the highest daily dose administered to patients with [[pulmonary arterial hypertension|PAH]] was 10 mg once daily. In healthy volunteers, single doses of 50 mg and 100 mg (5 to 10 times the maximum recommended dose) were associated with headache, flushing, dizziness, nausea, and nasal congestion. Massive overdosage could potentially result in hypotension that may require intervention. | |||
===Chronic Overdose=== | ===Chronic Overdose=== | ||
| Line 392: | Line 248: | ||
<!--Drug box 2--> | <!--Drug box 2--> | ||
|drugBox= | |||
{{Drugbox2 | |||
| verifiedrevid = 437179007 | |||
| IUPAC_name = (2''S'')-2-[(4,6-dimethylpyrimidin-2-yl)oxy]-3-methoxy- 3,3-diphenylpropanoic acid | |||
| image = Ambrisentan.png | |||
<!--Clinical data--> | |||
| tradename = | |||
| Drugs.com = {{drugs.com|monograph|ambrisentan}} | |||
| licence_EU = Volibris | |||
| licence_US = Ambrisentan | |||
| pregnancy_AU = X | |||
| pregnancy_US = X | |||
| pregnancy_category = | |||
| legal_AU = S4 | |||
| legal_CA = Rx-only | |||
| legal_UK = POM | |||
| legal_US = Rx-only | |||
| legal_status = | |||
| routes_of_administration = Oral | |||
| | <!--Pharmacokinetic data--> | ||
| bioavailability = Undetermined | |||
| protein_bound = 99% | |||
| metabolism = | |||
| elimination_half-life = 15 hours (terminal) | |||
| excretion = | |||
<!--Identifiers--> | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 177036-94-1 | |||
| ATC_prefix = C02 | |||
| ATC_suffix = KX02 | |||
| PubChem = 6918493 | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = 5293690 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = HW6NV07QEC | |||
| ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| ChEMBL = 1111 | |||
<!--Chemical data--> | |||
| C=22 | H=22 | N=2 | O=4 | |||
| molecular_weight = 378.421 g/mol | |||
| smiles = O=C(O)[C@@H](Oc1nc(cc(n1)C)C)C(OC)(c2ccccc2)c3ccccc3 | |||
| InChI = 1/C22H22N2O4/c1-15-14-16(2)24-21(23-15)28-19(20(25)26)22(27-3,17-10-6-4-7-11-17)18-12-8-5-9-13-18/h4-14,19H,1-3H3,(H,25,26)/t19-/m1/s1 | |||
| InChIKey = OUJTZYPIHDYQMC-LJQANCHMBI | |||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChI = 1S/C22H22N2O4/c1-15-14-16(2)24-21(23-15)28-19(20(25)26)22(27-3,17-10-6-4-7-11-17)18-12-8-5-9-13-18/h4-14,19H,1-3H3,(H,25,26)/t19-/m1/s1 | |||
| StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChIKey = OUJTZYPIHDYQMC-LJQANCHMSA-N | |||
}} | |||
<!--Mechanism of Action--> | <!--Mechanism of Action--> | ||
|mechAction= | |mechAction= | ||
* | * Endothelin-1 (ET-1) is a potent autocrine and paracrine peptide. Two receptor subtypes, ETA and ETB, mediate the effects of ET-1 in the vascular smooth muscle and endothelium. The primary actions of ETA are vasoconstriction and cell proliferation, while the predominant actions of ETB are vasodilation, antiproliferation, and ET-1 clearance. | ||
* In patients with [[pulmonary arterial hypertension|PAH]], plasma ET-1 concentrations are increased as much as 10-fold and correlate with increased mean right atrial pressure and disease severity. ET-1 and ET-1 mRNA concentrations are increased as much as 9-fold in the lung tissue of patients with [[pulmonary arterial hypertension|PAH]], primarily in the endothelium of pulmonary arteries. These findings suggest that ET-1 may play a critical role in the pathogenesis and progression of [[pulmonary arterial hypertension|PAH]]. | |||
* Ambrisentan is a high-affinity (Ki=0.011 nM) ETA receptor antagonist with a high selectivity for the ETA versus ETB receptor (>4000-fold). The clinical impact of high selectivity for ETA is not known. | |||
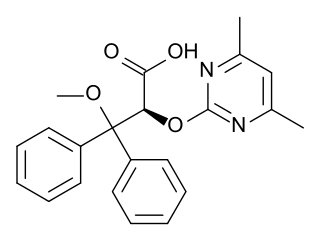
<!--Structure--> | <!--Structure--> | ||
|structure= | |structure= | ||
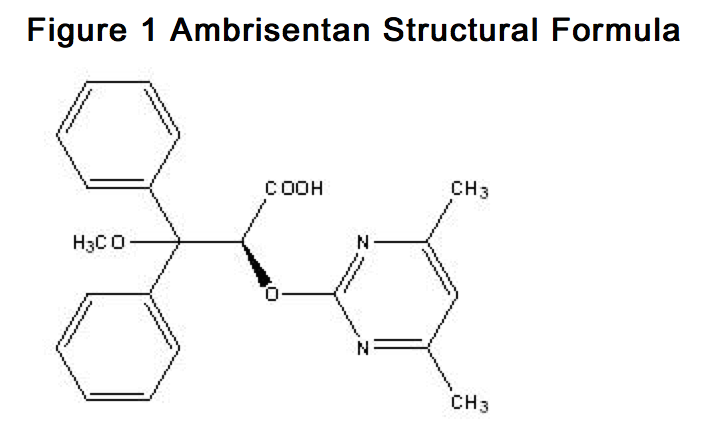
* | * Letairis is the brand name for ambrisentan, an endothelin receptor antagonist that is selective for the endothelin type-A (ETA) receptor. The chemical name of ambrisentan is (+)-(2S)-2-[(4,6-dimethylpyrimidin-2-yl)oxy]-3-methoxy-3,3-diphenylpropanoic acid. It has a molecular formula of C22H22N2O4 and a molecular weight of 378.42. It contains a single chiral center determined to be the (S) configuration and has the following structural formula: | ||
: [[File:{{PAGENAME}}01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:{{PAGENAME}}01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
* Ambrisentan is a white to off-white, crystalline solid. It is a carboxylic acid with a pKa of 4.0. Ambrisentan is practically insoluble in water and in aqueous solutions at low pH. Solubility increases in aqueous solutions at higher pH. In the solid state ambrisentan is very stable, is not hygroscopic, and is not light sensitive. | |||
* Letairis is available as 5 mg and 10 mg film-coated tablets for once daily oral administration. The tablets include the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate and microcrystalline cellulose. The tablets are film-coated with a coating material containing FD&C Red #40 aluminum lake, lecithin, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide. Each square, pale pink Letairis tablet contains 5 mg of ambrisentan. Each oval, deep pink Letairis tablet contains 10 mg of ambrisentan. Letairis tablets are unscored. | |||
<!--Pharmacodynamics--> | <!--Pharmacodynamics--> | ||
|PD= | |PD= | ||
* Cardiac Electrophysiology | |||
:* In a randomized, positive- and placebo-controlled, parallel-group study, healthy subjects received either Letairis 10 mg daily followed by a single dose of 40 mg, placebo followed by a single dose of moxifloxacin 400 mg, or placebo alone. Letairis 10 mg daily had no significant effect on the QTc interval. The 40 mg dose of Letairis increased mean QTc at tmax by 5 ms with an upper 95% confidence limit of 9 ms. For patients receiving Letairis 5–10 mg daily and not taking metabolic inhibitors, no significant QT prolongation is expected. | |||
<!--Pharmacokinetics--> | <!--Pharmacokinetics--> | ||
|PK= | |PK= | ||
* The pharmacokinetics of ambrisentan (S-ambrisentan) in healthy subjects is dose proportional. The absolute bioavailability of ambrisentan is not known. Ambrisentan is absorbed with peak concentrations occurring approximately 2 hours after oral administration in healthy subjects and [[pulmonary arterial hypertension|PAH]] patients. Food does not affect its bioavailability. In vitro studies indicate that ambrisentan is a substrate of P-gp. Ambrisentan is highly bound to plasma proteins (99%). The elimination of ambrisentan is predominantly by non-renal pathways, but the relative contributions of metabolism and biliary elimination have not been well characterized. In plasma, the AUC of 4-hydroxymethyl ambrisentan accounts for approximately 4% relative to parent ambrisentan AUC. The in vivo inversion of S-ambrisentan to R-ambrisentan is negligible. The mean oral clearance of ambrisentan is 38 mL/min and 19 mL/min in healthy subjects and in [[pulmonary arterial hypertension|PAH]] patients, respectively. Although ambrisentan has a 15-hour terminal half-life, the mean trough concentration of ambrisentan at steady-state is about 15% of the mean peak concentration and the accumulation factor is about 1.2 after long-term daily dosing, indicating that the effective half-life of ambrisentan is about 9 hours. | |||
<!--Nonclinical Toxicology--> | <!--Nonclinical Toxicology--> | ||
|nonClinToxic= | |nonClinToxic= | ||
There | * Carcinogenesis, Mutagenesis, Impairment of Fertility | ||
:* Oral carcinogenicity studies of up to two years duration were conducted at starting doses of 10, 30, and 60 mg/kg/day in rats (8 to 48 times the maximum recommended human dose [MRHD] on a mg/m2 basis) and at 50, 150, and 250 mg/kg/day in mice (28 to 140 times the MRHD). In the rat study, the high- and mid-dose male and female groups had their doses lowered to 40 and 20 mg/kg/day, respectively, in week 51 because of effects on survival. The high-dose males and females were taken off drug completely in weeks 69 and 93, respectively. The only evidence of ambrisentan-related carcinogenicity was a positive trend in male rats, for the combined incidence of benign basal cell tumor and basal cell carcinoma of skin/subcutis in the mid-dose group (high-dose group excluded from analysis), and the occurrence of mammary fibroadenomas in males in the high-dose group. In the mouse study, high-dose male and female groups had their doses lowered to 150 mg/kg/day in week 39 and were taken off drug completely in week 96 (males) or week 76 (females). In mice, ambrisentan was not associated with excess tumors in any dosed group. | |||
:* Positive findings of clastogenicity were detected, at drug concentrations producing moderate to high toxicity, in the chromosome aberration assay in cultured human [[lymphocyte]]s. There was no evidence for genetic toxicity of ambrisentan when tested in vitro in bacteria (Ames test) or in vivo in rats (micronucleus assay, unscheduled DNA synthesis assay). | |||
:* The development of testicular tubular atrophy and impaired fertility has been linked to the chronic administration of endothelin receptor antagonists in rodents. Testicular tubular degeneration was observed in rats treated with ambrisentan for two years at doses ≥10 mg/kg/day (8-fold MRHD). Increased incidences of testicular findings were also observed in mice treated for two years at doses ≥50 mg/kg/day (28-fold MRHD). Effects on sperm count, sperm morphology, mating performance, and fertility were observed in fertility studies in which male rats were treated with ambrisentan at oral doses of 300 mg/kg/day (236-fold MRHD). At doses of ≥10 mg/kg/day, observations of testicular histopathology in the absence of fertility and sperm effects were also present. | |||
<!--Clinical Studies--> | <!--Clinical Studies--> | ||
|clinicalStudies= | |||
=====Pulmonary Arterial Hypertension ([[pulmonary arterial hypertension|PAH]])===== | |||
* Two 12-week, randomized, double-blind, placebo-controlled, multicenter studies were conducted in 393 patients with [[pulmonary arterial hypertension|PAH]] (WHO Group 1). The two studies were identical in design except for the doses of Letairis and the geographic region of the investigational sites. ARIES-1 compared once-daily doses of 5 mg and 10 mg Letairis to placebo, while ARIES-2 compared once-daily doses of 2.5 mg and 5 mg Letairis to placebo. In both studies, Letairis or placebo was added to current therapy, which could have included a combination of anticoagulants, diuretics, calcium channel blockers, or digoxin, but not epoprostenol, treprostinil, iloprost, bosentan, or sildenafil. The primary study endpoint was 6-minute walk distance. In addition, clinical worsening, WHO functional class, dyspnea, and SF-36® Health Survey were assessed. | |||
* Patients had idiopathic or heritable [[pulmonary arterial hypertension|PAH]] (64%) or [[pulmonary arterial hypertension|PAH]] associated with connective tissue diseases (32%), HIV infection (3%), or anorexigen use (1%). There were no patients with [[pulmonary arterial hypertension|PAH]] associated with congenital heart disease. | |||
* Patients had WHO functional class I (2%), II (38%), III (55%), or IV (5%) symptoms at baseline. The mean age of patients was 50 years, 79% of patients were female, and 77% were Caucasian. | |||
======Submaximal Exercise Ability====== | |||
* Results of the 6-minute walk distance at 12 weeks for the ARIES-1 and ARIES-2 studies are shown in Table 2 and Figure 4. | |||
: [[File:{{PAGENAME}}04.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
: [[File:{{PAGENAME}}05.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
* In both studies, treatment with Letairis resulted in a significant improvement in 6-minute walk distance for each dose of Letairis and the improvements increased with dose. An increase in 6-minute walk distance was observed after 4 weeks of treatment with Letairis, with a dose-response observed after 12 weeks of treatment. Improvements in walk distance with Letairis were smaller for elderly patients (age ≥65) than younger patients and for patients with secondary [[pulmonary arterial hypertension|PAH]] than for patients with idiopathic or heritable [[pulmonary arterial hypertension|PAH]]. The results of such subgroup analyses must be interpreted cautiously. | |||
* The effects of Letairis on walk distances at trough drug levels are not known. Because only once-daily dosing was studied in the clinical trials, the efficacy and safety of more frequent dosing regimens for Letairis are not known. If exercise ability is not sustained throughout the day in a patient, consider other [[pulmonary arterial hypertension|PAH]] treatments that have been studied with more-frequent dosing regimens. | |||
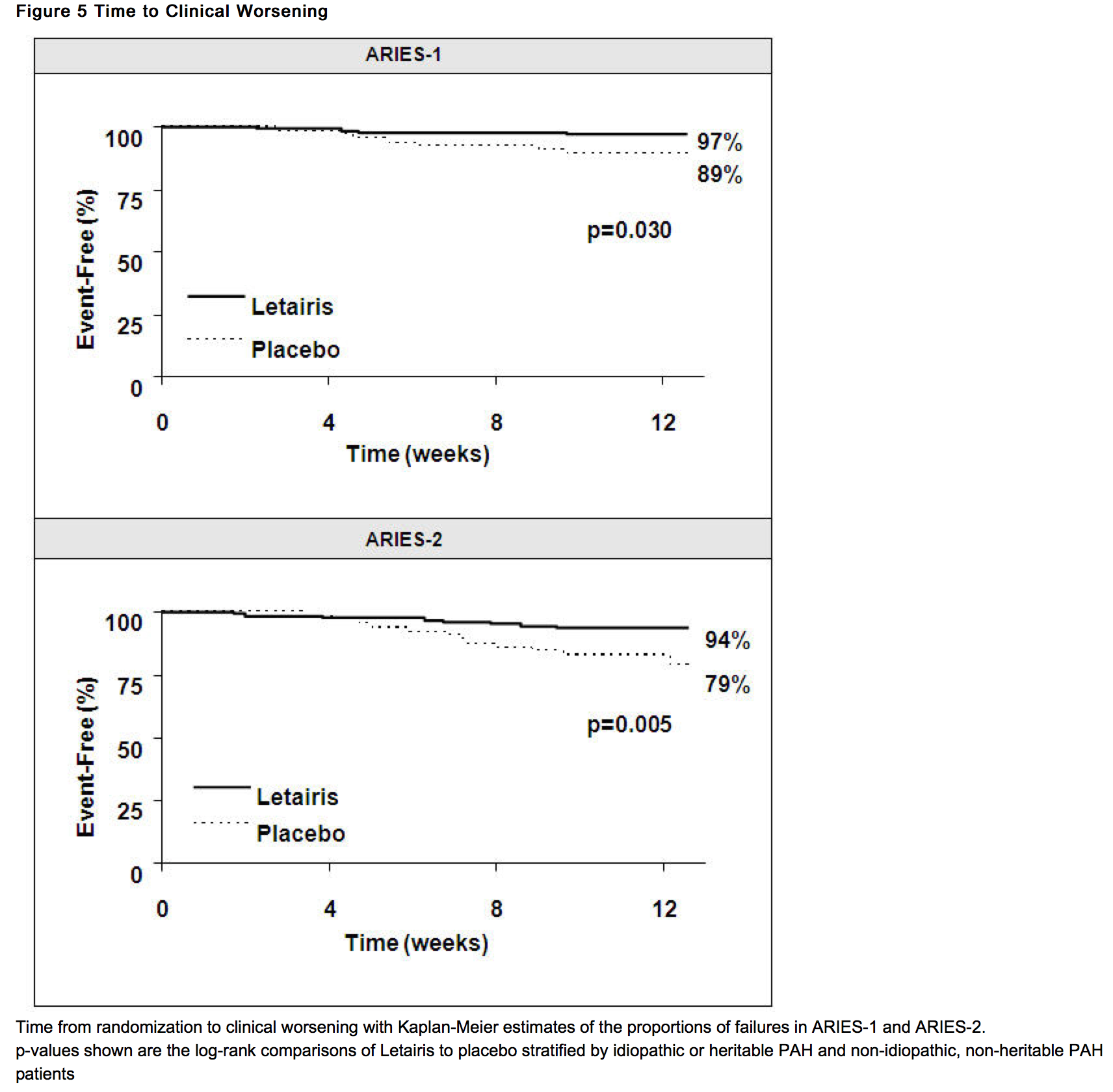
======Clinical Worsening====== | |||
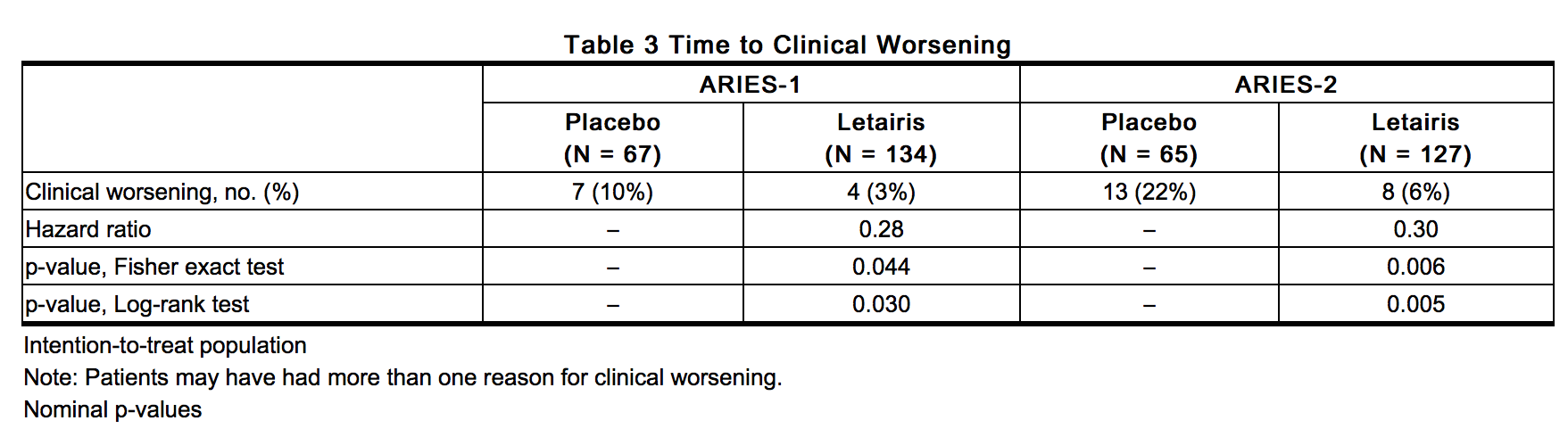
* Time to clinical worsening of [[pulmonary arterial hypertension|PAH]] was defined as the first occurrence of death, lung transplantation, hospitalization for [[pulmonary arterial hypertension|PAH]], atrial septostomy, study withdrawal due to the addition of other [[pulmonary arterial hypertension|PAH]] therapeutic agents, or study withdrawal due to early escape. Early escape was defined as meeting two or more of the following criteria: a 20% decrease in the 6-minute walk distance; an increase in WHO functional class; worsening right ventricular failure; rapidly progressing cardiogenic, hepatic, or [[renal failure]]; or refractory systolic [[hypotension]]. The clinical worsening events during the 12-week treatment period of the Letairis clinical trials are shown in Table 3 and Figure 5. | |||
: [[File:{{PAGENAME}}06.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
* There was a significant delay in the time to clinical worsening for patients receiving Letairis compared to placebo. Results in subgroups such as the elderly were also favorable. | |||
| | : [[File:{{PAGENAME}}07.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
=====Long-term Treatment of [[pulmonary arterial hypertension|PAH]]===== | |||
* In long-term follow-up of patients who were treated with Letairis (2.5 mg, 5 mg, or 10 mg once daily) in the two pivotal studies and their open-label extension (N = 383), Kaplan-Meier estimates of survival at 1, 2, and 3 years were 93%, 85%, and 79%, respectively. Of the patients who remained on Letairis for up to 3 years, the majority received no other treatment for [[pulmonary arterial hypertension|PAH]]. These uncontrolled observations do not allow comparison with a group not given Letairis and cannot be used to determine the long-term effect of Letairis on mortality. | |||
=====Adverse Effects in Idiopathic Pulmonary Fibrosis (IPF)===== | |||
* A randomized controlled study in patients with IPF, with or without pulmonary hypertension (WHO Group 3), compared Letairis (N = 329) to placebo (N = 163). The study was terminated after 34 weeks for lack of efficacy, and was found to demonstrate a greater risk of disease progression or death on Letairis. More patients taking Letairis died (8% vs. 4%), had a respiratory hospitalization (13% vs. 6%), and had a decrease in FVC/DLCO (17% vs. 12%). | |||
<!--How Supplied--> | <!--How Supplied--> | ||
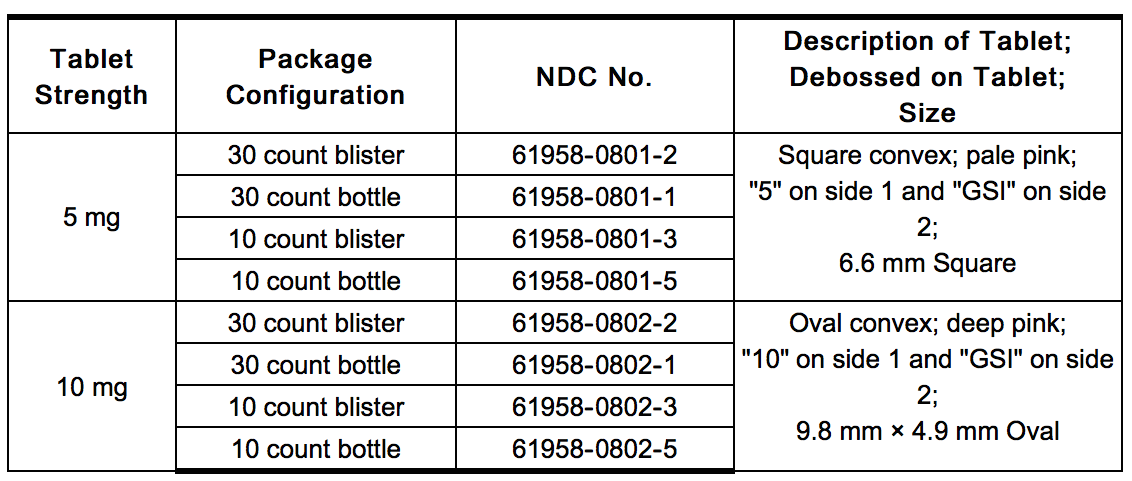
|howSupplied= | |||
| | * Letairis film-coated tablets are supplied as follows: | ||
: [[File:{{PAGENAME}}08.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
* | * Store at 25° C (77° F); excursions permitted to 15–30° C (59–86° F). | ||
* Store Letairis in its original packaging. | |||
<!--Patient Counseling Information--> | <!--Patient Counseling Information--> | ||
|fdaPatientInfo= | |fdaPatientInfo= | ||
[[File:{{PAGENAME}}09.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
<!--Precautions with Alcohol--> | <!--Precautions with Alcohol--> | ||
|alcohol= | |alcohol= | ||
| Line 454: | Line 393: | ||
<!--Brand Names--> | <!--Brand Names--> | ||
|brandNames= | |brandNames= | ||
* | * Letairis®<ref>{{Cite web | title = LETAIRIS (ambrisentan) tablet, film coated | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=725d4e73-6c83-477a-adc6-0ae4a133a844 }}</ref> | ||
<!--Look-Alike Drug Names--> | <!--Look-Alike Drug Names--> | ||
|lookAlike= | |lookAlike= | ||
* | * Letairis® — Letaris®<ref name="www.ismp.org">{{Cite web | last = | first = | title = http://www.ismp.org | url = http://www.ismp.org | publisher = | date = }}</ref> | ||
<!--Drug Shortage Status--> | <!--Drug Shortage Status--> | ||
|drugShortage= | |drugShortage= | ||
}} | }} | ||
| Line 490: | Line 426: | ||
{{LabelImage | {{LabelImage | ||
|fileName={{PAGENAME}} | |fileName={{PAGENAME}}10.png|This image is provided by the National Library of Medicine. | ||
}} | }} | ||
| Line 497: | Line 433: | ||
}} | }} | ||
{{LabelImage | |||
|fileName={{PAGENAME}}12.png|This image is provided by the National Library of Medicine. | |||
}} | |||
<!--Category--> | <!--Category--> | ||
Latest revision as of 15:40, 27 July 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gerald Chi
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: EMBRYO-FETAL TOXICITY
See full prescribing information for complete Boxed Warning.
* Do not administer Letairis to a pregnant female because it may cause fetal harm. Letairis is very likely to produce serious birth defects if used by pregnant females, as this effect has been seen consistently when it is administered to animals.
|
Overview
Ambrisentan is an endothelin receptor antagonist that is FDA approved for the {{{indicationType}}} of pulmonary arterial hypertension. There is a Black Box Warning for this drug as shown here. Common adverse reactions include edema, decreased hemoglobin, and headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Pulmonary Arterial Hypertension
- Letairis is indicated for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1) to improve exercise ability and delay clinical worsening. Studies establishing effectiveness included predominantly patients with WHO Functional Class II–III symptoms and etiologies of idiopathic or heritable PAH (64%) or PAH associated with connective tissue diseases (32%).
- Dosing Information
- Initiate treatment at 5 mg once daily, and consider increasing the dose to 10 mg once daily if 5 mg is tolerated.
- Tablets may be administered with or without food. Tablets should not be split, crushed, or chewed. Doses higher than 10 mg once daily have not been studied in patients with pulmonary arterial hypertension (PAH).
Pregnancy Testing in Females of Reproductive Potential
- Initiate treatment with Letairis in females of reproductive potential only after a negative pregnancy test. Obtain monthly pregnancy tests during treatment.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ambrisentan in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ambrisentan in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- Safety and effectiveness of Letairis in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ambrisentan in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ambrisentan in pediatric patients.
Contraindications
- Pregnancy
- Letairis may cause fetal harm when administered to a pregnant female. Letairis is contraindicated in females who are pregnant. Letairis was consistently shown to have teratogenic effects when administered to animals. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
- Idiopathic Pulmonary Fibrosis
- Letairis is contraindicated in patients with idiopathic pulmonary fibrosis (IPF), including IPF patients with pulmonary hypertension (WHO Group 3)
Warnings
|
WARNING: EMBRYO-FETAL TOXICITY
See full prescribing information for complete Boxed Warning.
* Do not administer Letairis to a pregnant female because it may cause fetal harm. Letairis is very likely to produce serious birth defects if used by pregnant females, as this effect has been seen consistently when it is administered to animals.
|
Embryo-fetal Toxicity
- Letairis may cause fetal harm when administered during pregnancy and is contraindicated for use in females who are pregnant. In females of reproductive potential, exclude pregnancy prior to initiation of therapy, ensure use of acceptable contraceptive methods, and obtain monthly pregnancy tests.
- Letairis is only available for females through a restricted program under a REMS.
Letairis REMS Program
- For all females, Letairis is available only through a restricted program called the Letairis REMS, because of the risk of embryo-fetal toxicity.
- Notable requirements of the Letairis REMS program include the following:
- Prescribers must be certified with the program by enrolling and completing training.
- All females, regardless of reproductive potential, must enroll in the Letairis REMS program prior to initiating Letairis. Male patients are not enrolled in the REMS.
- Females of reproductive potential must comply with the pregnancy testing and contraception requirements.
- Pharmacies that dispense Letairis must be certified with the program and must dispense to female patients who are authorized to receive Letairis.
- Further information is available at www.letairisrems.com or 1-866-664-5327.
Fluid Retention
- Peripheral edema is a known class effect of endothelin receptor antagonists, and is also a clinical consequence of PAH and worsening PAH. In the placebo-controlled studies, there was an increased incidence of peripheral edema in patients treated with doses of 5 or 10 mg Letairis compared to placebo. Most edema was mild to moderate in severity, and it occurred with greater frequency and severity in elderly patients.
- In addition, there have been postmarketing reports of fluid retention in patients with pulmonary hypertension, occurring within weeks after starting Letairis. Patients required intervention with a diuretic, fluid management, or, in some cases, hospitalization for decompensating heart failure.
- If clinically significant fluid retention develops, with or without associated weight gain, further evaluation should be undertaken to determine the cause, such as Letairis or underlying heart failure, and the possible need for specific treatment or discontinuation of Letairis therapy.
Pulmonary Edema with Pulmonary Veno-occlusive Disease (PVOD)
- If patients develop acute pulmonary edema during initiation of therapy with vasodilating agents such as Letairis, the possibility of PVOD should be considered, and if confirmed Letairis should be discontinued.
Decreased Sperm Counts
- Decreased sperm counts have been observed in human and animal studies with another endothelin receptor antagonist and in animal fertility studies with ambrisentan. Letairis may have an adverse effect on spermatogenesis. Counsel patients about potential effects on fertility.
Hematological Changes
- Decreases in hemoglobin concentration and hematocrit have followed administration of other endothelin receptor antagonists and were observed in clinical studies with Letairis. These decreases were observed within the first few weeks of treatment with Letairis, and stabilized thereafter. The mean decrease in hemoglobin from baseline to end of treatment for those patients receiving Letairis in the 12-week placebo-controlled studies was 0.8 g/dL.
- Marked decreases in hemoglobin (>15% decrease from baseline resulting in a value below the lower limit of normal) were observed in 7% of all patients receiving Letairis (and 10% of patients receiving 10 mg) compared to 4% of patients receiving placebo. The cause of the decrease in hemoglobin is unknown, but it does not appear to result from hemorrhage or hemolysis.
- In the long-term open-label extension of the two pivotal clinical studies, mean decreases from baseline (ranging from 0.9 to 1.2 g/dL) in hemoglobin concentrations persisted for up to 4 years of treatment.
- There have been postmarketing reports of decreases in hemoglobin concentration and hematocrit that have resulted in anemia requiring transfusion.
- Measure hemoglobin prior to initiation of Letairis, at one month, and periodically thereafter. Initiation of Letairis therapy is not recommended for patients with clinically significant anemia. If a clinically significant decrease in hemoglobin is observed and other causes have been excluded, consider discontinuing Letairis.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Safety data for Letairis were obtained from two 12-week, placebo-controlled studies in patients with pulmonary arterial hypertension (PAH) (ARIES-1 and ARIES-2) and four nonplacebo-controlled studies in 483 patients with PAH who were treated with doses of 1, 2.5, 5, or 10 mg once daily. The exposure to Letairis in these studies ranged from 1 day to 4 years (N = 418 for at least 6 months and N = 343 for at least 1 year).
- In ARIES-1 and ARIES-2, a total of 261 patients received Letairis at doses of 2.5, 5, or 10 mg once daily and 132 patients received placebo. The adverse reactions that occurred in >3% more patients receiving Letairis than receiving placebo are shown in Table 1.
- Most adverse drug reactions were mild to moderate and only nasal congestion was dose-dependent.
- Few notable differences in the incidence of adverse reactions were observed for patients by age or sex. Peripheral edema was similar in younger patients (<65 years) receiving Letairis (14%; 29/205) or placebo (13%; 13/104), and was greater in elderly patients (≥65 years) receiving Letairis (29%; 16/56) compared to placebo (4%; 1/28). The results of such subgroup analyses must be interpreted cautiously.
- The incidence of treatment discontinuations due to adverse events other than those related to PAH during the clinical trials in patients with PAH was similar for Letairis (2%; 5/261 patients) and placebo (2%; 3/132 patients). The incidence of patients with serious adverse events other than those related to PAH during the clinical trials in patients with PAH was similar for placebo (7%; 9/132 patients) and for Letairis (5%; 13/261 patients).
- During 12-week controlled clinical trials, the incidence of aminotransferase elevations >3 × upper limit of normal (ULN) were 0% on Letairis and 2.3% on placebo. In practice, cases of hepatic injury should be carefully evaluated for cause.
Use in Patients with Prior Endothelin Receptor Antagonist (ERA) Related Serum Liver Enzyme Abnormalities
- In an uncontrolled, open-label study, 36 patients who had previously discontinued endothelin receptor antagonists (ERAs: bosentan, an investigational drug, or both) due to aminotransferase elevations >3 × ULN were treated with Letairis. Prior elevations were predominantly moderate, with 64% of the ALT elevations <5 × ULN, but 9 patients had elevations >8 × ULN. Eight patients had been re-challenged with bosentan and/or the investigational ERA and all eight had a recurrence of aminotransferase abnormalities that required discontinuation of ERA therapy. All patients had to have normal aminotransferase levels on entry to this study. Twenty-five of the 36 patients were also receiving prostanoid and/or phosphodiesterase type 5 (PDE5) inhibitor therapy. Two patients discontinued early (including one of the patients with a prior 8 × ULN elevation). Of the remaining 34 patients, one patient experienced a mild aminotransferase elevation at 12 weeks on Letairis 5 mg that resolved with decreasing the dosage to 2.5 mg, and that did not recur with later escalations to 10 mg. With a median follow-up of 13 months and with 50% of patients increasing the dose of Letairis to 10 mg, no patients were discontinued for aminotransferase elevations. While the uncontrolled study design does not provide information about what would have occurred with re-administration of previously used ERAs or show that Letairis led to fewer aminotransferase elevations than would have been seen with those drugs, the study indicates that Letairis may be tried in patients who have experienced asymptomatic aminotransferase elevations on other ERAs after aminotransferase levels have returned to normal.
Postmarketing Experience
- The following adverse reactions were identified during postapproval use of Letairis. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to estimate reliably the frequency or to establish a causal relationship to drug exposure: anemia, heart failure (associated with fluid retention), hypersensitivity (eg, angioedema, rash), nausea, and vomiting.
- Elevations of liver aminotransferases (ALT, AST) have been reported with Letairis use; in most cases alternative causes of the liver injury could be identified (heart failure, hepatic congestion, hepatitis, alcohol use, hepatotoxic medications). Other endothelin receptor antagonists have been associated with elevations of aminotransferases, hepatotoxicity, and cases of liver failure.
Drug Interactions
- Multiple dose coadministration of ambrisentan and cyclosporine resulted in an approximately 2-fold increase in ambrisentan exposure in healthy volunteers; therefore, limit the dose of ambrisentan to 5 mg once daily when coadministered with cyclosporine.
In Vitro Studies
- Studies with human liver tissue indicate that ambrisentan is metabolized by CYP3A, CYP2C19, and uridine 5'-diphosphate glucuronosyltransferases (UGTs) 1A9S, 2B7S, and 1A3S. In vitro studies suggest that ambrisentan is a substrate of the Organic Anion Transporting Polypeptides OATP1B1 and OATP1B3, and P-glycoprotein (P-gp). Drug interactions might be expected because of these factors; however, a clinically relevant interaction has been demonstrated only with cyclosporine. In vitro studies found ambrisentan to have little to no inhibition of human hepatic transporters. Ambrisentan demonstrated weak dose-dependent inhibition of OATP1B1, OATP1B3, and NTCP (IC50 of 47 µM, 45 µM, and approximately 100 µM, respectively) and no transporter-specific inhibition of BSEP, BRCP, P-gp, or MRP2. Ambrisentan does not inhibit or induce drug metabolizing enzymes at clinically relevant concentrations.
In Vivo Studies
- The effects of other drugs on ambrisentan pharmacokinetics and the effects of ambrisentan on the exposure to other drugs are shown in Figure 2 and Figure 3, respectively.
Use in Specific Populations
Pregnancy
- Pregnancy Category X
- Risk Summary
- Letairis may cause fetal harm when administered to a pregnant woman and is contraindicated during pregnancy. Letairis was teratogenic in rats and rabbits at doses which resulted in exposures of 3.5 and 1.7 times, respectively, the human dose of 10 mg per day. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, advise the patient of the potential hazard to a fetus.
- Animal Data
- Letairis was teratogenic at oral doses of ≥ 15 mg/kg/day (AUC 51.7 h•µg/mL) in rats and ≥ 7 mg/kg/day (24.7 h•µg/mL) in rabbits; it was not studied at lower doses. These doses are of 3.5 and 1.7 times, respectively, the human dose of 10 mg per day (14.8 h•µg/mL) based on AUC. In both species, there were abnormalities of the lower jaw and hard and soft palate, malformation of the heart and great vessels, and failure of formation of the thymus and thyroid.
- A preclinical study in rats has shown decreased survival of newborn pups (mid and high doses) and effects on testicle size and fertility of pups (high dose) following maternal treatment with ambrisentan from late gestation through weaning. Doses tested were 17 ×, 51 ×, and 170 × (on a mg/kg:mg/m2 basis) the maximum oral human dose of 10 mg and an average adult body weight of 70 kg.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ambrisentan in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Ambrisentan during labor and delivery.
Nursing Mothers
- It is not known whether ambrisentan is present in human milk. Because many drugs are present in human milk and because of the potential for serious adverse reactions in nursing infants from Letairis, a decision should be made whether to discontinue nursing or discontinue Letairis, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness of Letairis in pediatric patients have not been established.
Geriatic Use
- In the two placebo-controlled clinical studies of Letairis, 21% of patients were ≥65 years old and 5% were ≥75 years old. The elderly (age ≥65 years) showed less improvement in walk distances with Letairis than younger patients did, but the results of such subgroup analyses must be interpreted cautiously. Peripheral edema was more common in the elderly than in younger patients.
Gender
There is no FDA guidance on the use of Ambrisentan with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ambrisentan with respect to specific racial populations.
Renal Impairment
- The impact of renal impairment on the pharmacokinetics of ambrisentan has been examined using a population pharmacokinetic approach in PAH patients with creatinine clearances ranging between 20 and 150 mL/min. There was no significant impact of mild or moderate renal impairment on exposure to ambrisentan. Dose adjustment of Letairis in patients with mild or moderate renal impairment is therefore not required. There is no information on the exposure to ambrisentan in patients with severe renal impairment.
- The impact of hemodialysis on the disposition of ambrisentan has not been investigated.
Hepatic Impairment
- Pre-existing Hepatic Impairment
- The influence of pre-existing hepatic impairment on the pharmacokinetics of ambrisentan has not been evaluated. Because there is in vitro and in vivo evidence of significant metabolic and biliary contribution to the elimination of ambrisentan, hepatic impairment might be expected to have significant effects on the pharmacokinetics of ambrisentan. Letairis is not recommended in patients with moderate or severe hepatic impairment. There is no information on the use of Letairis in patients with mild pre-existing impaired liver function; however, exposure to ambrisentan may be increased in these patients.
- Elevation of Liver Transaminases
- Other endothelin receptor antagonists (ERAs) have been associated with aminotransferase (AST, ALT) elevations, hepatotoxicity, and cases of liver failure. In patients who develop hepatic impairment after Letairis initiation, the cause of liver injury should be fully investigated. Discontinue Letairis if elevations of liver aminotransferases are >5 × ULN or if elevations are accompanied by bilirubin >2 × ULN, or by signs or symptoms of liver dysfunction and other causes are excluded.
Females of Reproductive Potential and Males
- Pregnancy Testing
- Female patients of reproductive potential must have a negative pregnancy test prior to initiation of treatment, monthly pregnancy test during treatment, and 1 month after stopping treatment with Letairis. Advise patients to contact their healthcare provider if they become pregnant or suspect they may be pregnant. Perform a pregnancy test if pregnancy is suspected for any reason. For positive pregnancy tests, counsel patient on the potential risk to the fetus and patient options.
- Contraception
- Female patients of reproductive potential must use acceptable methods of contraception during treatment with Letairis and for 1 month after stopping treatment with Letairis. Patients may choose one highly effective form of contraception (intrauterine device (IUD), contraceptive implant, or tubal sterilization) or a combination of methods (hormone method with a barrier method or two barrier methods). If a partner's vasectomy is the chosen method of contraception, a hormone or barrier method must be used along with this method. Counsel patients on pregnancy planning and prevention, including emergency contraception, or designate counseling by another healthcare provider trained in contraceptive counseling.
- Infertility in Males
- In a 6-month study of another endothelin receptor antagonist, bosentan, 25 male patients with WHO functional class III and IV PAH and normal baseline sperm count were evaluated for effects on testicular function. There was a decline in sperm count of at least 50% in 25% of the patients after 3 or 6 months of treatment with bosentan. One patient developed marked oligospermia at 3 months, and the sperm count remained low with 2 follow-up measurements over the subsequent 6 weeks. Bosentan was discontinued and after 2 months the sperm count had returned to baseline levels. In 22 patients who completed 6 months of treatment, sperm count remained within the normal range and no changes in sperm morphology, sperm motility, or hormone levels were observed. Based on these findings and preclinical data from endothelin receptor antagonists, it cannot be excluded that endothelin receptor antagonists such as Letairis have an adverse effect on spermatogenesis. Counsel patients about the potential effects on fertility.
Immunocompromised Patients
There is no FDA guidance one the use of Ambrisentan in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Ambrisentan in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Ambrisentan in the drug label.
Overdosage
Acute Overdose
- There is no experience with overdosage of Letairis. The highest single dose of Letairis administered to healthy volunteers was 100 mg, and the highest daily dose administered to patients with PAH was 10 mg once daily. In healthy volunteers, single doses of 50 mg and 100 mg (5 to 10 times the maximum recommended dose) were associated with headache, flushing, dizziness, nausea, and nasal congestion. Massive overdosage could potentially result in hypotension that may require intervention.
Chronic Overdose
There is limited information regarding Chronic Overdose of Ambrisentan in the drug label.
Pharmacology
| |
Ambrisentan
| |
| Systematic (IUPAC) name | |
| (2S)-2-[(4,6-dimethylpyrimidin-2-yl)oxy]-3-methoxy- 3,3-diphenylpropanoic acid | |
| Identifiers | |
| CAS number | |
| ATC code | C02 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 378.421 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | Undetermined |
| Protein binding | 99% |
| Metabolism | ? |
| Half life | 15 hours (terminal) |
| Excretion | ? |
| Therapeutic considerations | |
| Licence data |
, |
| Pregnancy cat. | |
| Legal status |
Prescription Only (S4)(AU) ?(CA) POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral |
Mechanism of Action
- Endothelin-1 (ET-1) is a potent autocrine and paracrine peptide. Two receptor subtypes, ETA and ETB, mediate the effects of ET-1 in the vascular smooth muscle and endothelium. The primary actions of ETA are vasoconstriction and cell proliferation, while the predominant actions of ETB are vasodilation, antiproliferation, and ET-1 clearance.
- In patients with PAH, plasma ET-1 concentrations are increased as much as 10-fold and correlate with increased mean right atrial pressure and disease severity. ET-1 and ET-1 mRNA concentrations are increased as much as 9-fold in the lung tissue of patients with PAH, primarily in the endothelium of pulmonary arteries. These findings suggest that ET-1 may play a critical role in the pathogenesis and progression of PAH.
- Ambrisentan is a high-affinity (Ki=0.011 nM) ETA receptor antagonist with a high selectivity for the ETA versus ETB receptor (>4000-fold). The clinical impact of high selectivity for ETA is not known.
Structure
- Letairis is the brand name for ambrisentan, an endothelin receptor antagonist that is selective for the endothelin type-A (ETA) receptor. The chemical name of ambrisentan is (+)-(2S)-2-[(4,6-dimethylpyrimidin-2-yl)oxy]-3-methoxy-3,3-diphenylpropanoic acid. It has a molecular formula of C22H22N2O4 and a molecular weight of 378.42. It contains a single chiral center determined to be the (S) configuration and has the following structural formula:
- Ambrisentan is a white to off-white, crystalline solid. It is a carboxylic acid with a pKa of 4.0. Ambrisentan is practically insoluble in water and in aqueous solutions at low pH. Solubility increases in aqueous solutions at higher pH. In the solid state ambrisentan is very stable, is not hygroscopic, and is not light sensitive.
- Letairis is available as 5 mg and 10 mg film-coated tablets for once daily oral administration. The tablets include the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate and microcrystalline cellulose. The tablets are film-coated with a coating material containing FD&C Red #40 aluminum lake, lecithin, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide. Each square, pale pink Letairis tablet contains 5 mg of ambrisentan. Each oval, deep pink Letairis tablet contains 10 mg of ambrisentan. Letairis tablets are unscored.
Pharmacodynamics
- Cardiac Electrophysiology
- In a randomized, positive- and placebo-controlled, parallel-group study, healthy subjects received either Letairis 10 mg daily followed by a single dose of 40 mg, placebo followed by a single dose of moxifloxacin 400 mg, or placebo alone. Letairis 10 mg daily had no significant effect on the QTc interval. The 40 mg dose of Letairis increased mean QTc at tmax by 5 ms with an upper 95% confidence limit of 9 ms. For patients receiving Letairis 5–10 mg daily and not taking metabolic inhibitors, no significant QT prolongation is expected.
Pharmacokinetics
- The pharmacokinetics of ambrisentan (S-ambrisentan) in healthy subjects is dose proportional. The absolute bioavailability of ambrisentan is not known. Ambrisentan is absorbed with peak concentrations occurring approximately 2 hours after oral administration in healthy subjects and PAH patients. Food does not affect its bioavailability. In vitro studies indicate that ambrisentan is a substrate of P-gp. Ambrisentan is highly bound to plasma proteins (99%). The elimination of ambrisentan is predominantly by non-renal pathways, but the relative contributions of metabolism and biliary elimination have not been well characterized. In plasma, the AUC of 4-hydroxymethyl ambrisentan accounts for approximately 4% relative to parent ambrisentan AUC. The in vivo inversion of S-ambrisentan to R-ambrisentan is negligible. The mean oral clearance of ambrisentan is 38 mL/min and 19 mL/min in healthy subjects and in PAH patients, respectively. Although ambrisentan has a 15-hour terminal half-life, the mean trough concentration of ambrisentan at steady-state is about 15% of the mean peak concentration and the accumulation factor is about 1.2 after long-term daily dosing, indicating that the effective half-life of ambrisentan is about 9 hours.
Nonclinical Toxicology
- Carcinogenesis, Mutagenesis, Impairment of Fertility
- Oral carcinogenicity studies of up to two years duration were conducted at starting doses of 10, 30, and 60 mg/kg/day in rats (8 to 48 times the maximum recommended human dose [MRHD] on a mg/m2 basis) and at 50, 150, and 250 mg/kg/day in mice (28 to 140 times the MRHD). In the rat study, the high- and mid-dose male and female groups had their doses lowered to 40 and 20 mg/kg/day, respectively, in week 51 because of effects on survival. The high-dose males and females were taken off drug completely in weeks 69 and 93, respectively. The only evidence of ambrisentan-related carcinogenicity was a positive trend in male rats, for the combined incidence of benign basal cell tumor and basal cell carcinoma of skin/subcutis in the mid-dose group (high-dose group excluded from analysis), and the occurrence of mammary fibroadenomas in males in the high-dose group. In the mouse study, high-dose male and female groups had their doses lowered to 150 mg/kg/day in week 39 and were taken off drug completely in week 96 (males) or week 76 (females). In mice, ambrisentan was not associated with excess tumors in any dosed group.
- Positive findings of clastogenicity were detected, at drug concentrations producing moderate to high toxicity, in the chromosome aberration assay in cultured human lymphocytes. There was no evidence for genetic toxicity of ambrisentan when tested in vitro in bacteria (Ames test) or in vivo in rats (micronucleus assay, unscheduled DNA synthesis assay).
- The development of testicular tubular atrophy and impaired fertility has been linked to the chronic administration of endothelin receptor antagonists in rodents. Testicular tubular degeneration was observed in rats treated with ambrisentan for two years at doses ≥10 mg/kg/day (8-fold MRHD). Increased incidences of testicular findings were also observed in mice treated for two years at doses ≥50 mg/kg/day (28-fold MRHD). Effects on sperm count, sperm morphology, mating performance, and fertility were observed in fertility studies in which male rats were treated with ambrisentan at oral doses of 300 mg/kg/day (236-fold MRHD). At doses of ≥10 mg/kg/day, observations of testicular histopathology in the absence of fertility and sperm effects were also present.
Clinical Studies
Pulmonary Arterial Hypertension (PAH)
- Two 12-week, randomized, double-blind, placebo-controlled, multicenter studies were conducted in 393 patients with PAH (WHO Group 1). The two studies were identical in design except for the doses of Letairis and the geographic region of the investigational sites. ARIES-1 compared once-daily doses of 5 mg and 10 mg Letairis to placebo, while ARIES-2 compared once-daily doses of 2.5 mg and 5 mg Letairis to placebo. In both studies, Letairis or placebo was added to current therapy, which could have included a combination of anticoagulants, diuretics, calcium channel blockers, or digoxin, but not epoprostenol, treprostinil, iloprost, bosentan, or sildenafil. The primary study endpoint was 6-minute walk distance. In addition, clinical worsening, WHO functional class, dyspnea, and SF-36® Health Survey were assessed.
- Patients had idiopathic or heritable PAH (64%) or PAH associated with connective tissue diseases (32%), HIV infection (3%), or anorexigen use (1%). There were no patients with PAH associated with congenital heart disease.
- Patients had WHO functional class I (2%), II (38%), III (55%), or IV (5%) symptoms at baseline. The mean age of patients was 50 years, 79% of patients were female, and 77% were Caucasian.
Submaximal Exercise Ability
- Results of the 6-minute walk distance at 12 weeks for the ARIES-1 and ARIES-2 studies are shown in Table 2 and Figure 4.

This image is provided by the National Library of Medicine. 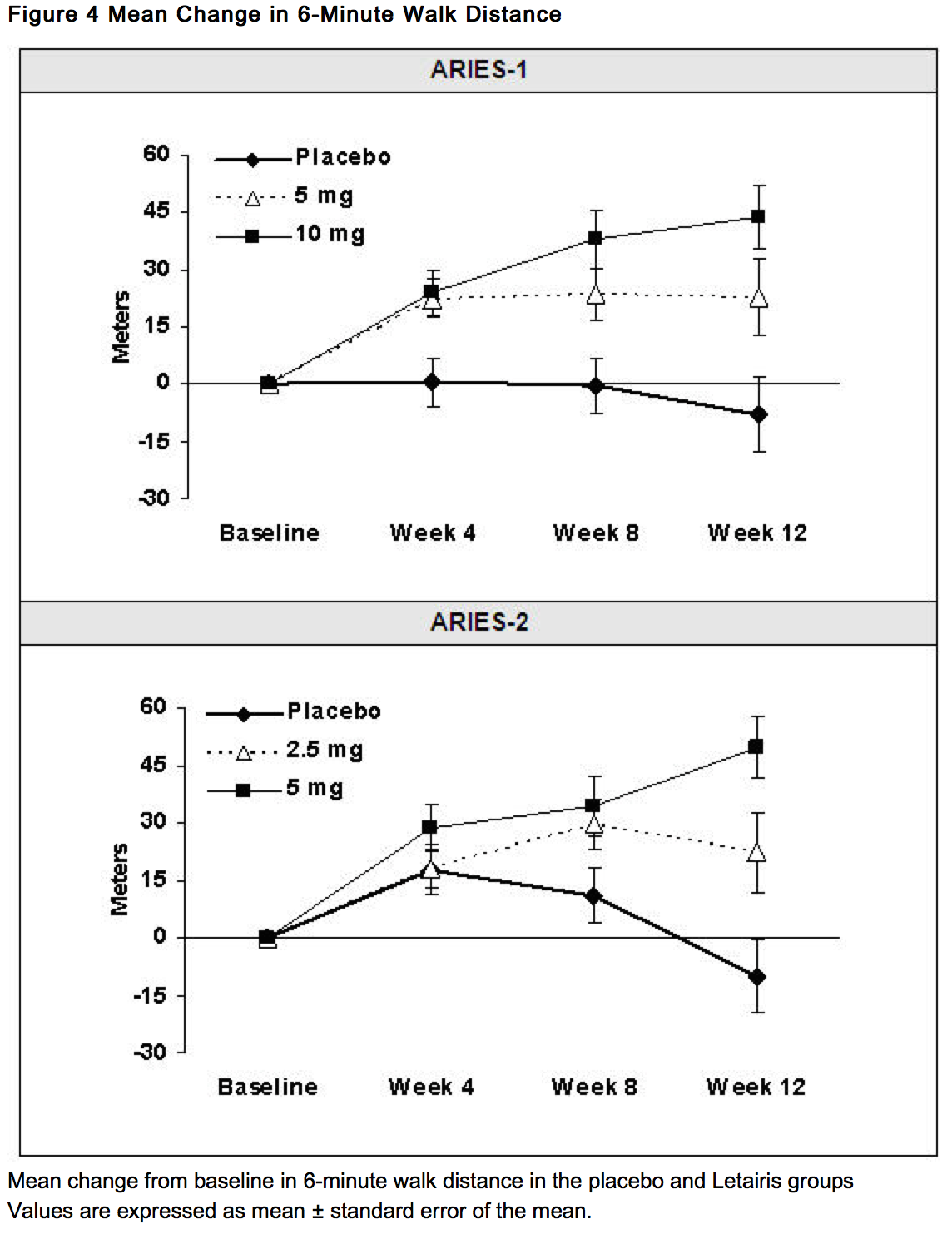
This image is provided by the National Library of Medicine.
- In both studies, treatment with Letairis resulted in a significant improvement in 6-minute walk distance for each dose of Letairis and the improvements increased with dose. An increase in 6-minute walk distance was observed after 4 weeks of treatment with Letairis, with a dose-response observed after 12 weeks of treatment. Improvements in walk distance with Letairis were smaller for elderly patients (age ≥65) than younger patients and for patients with secondary PAH than for patients with idiopathic or heritable PAH. The results of such subgroup analyses must be interpreted cautiously.
- The effects of Letairis on walk distances at trough drug levels are not known. Because only once-daily dosing was studied in the clinical trials, the efficacy and safety of more frequent dosing regimens for Letairis are not known. If exercise ability is not sustained throughout the day in a patient, consider other PAH treatments that have been studied with more-frequent dosing regimens.
Clinical Worsening
- Time to clinical worsening of PAH was defined as the first occurrence of death, lung transplantation, hospitalization for PAH, atrial septostomy, study withdrawal due to the addition of other PAH therapeutic agents, or study withdrawal due to early escape. Early escape was defined as meeting two or more of the following criteria: a 20% decrease in the 6-minute walk distance; an increase in WHO functional class; worsening right ventricular failure; rapidly progressing cardiogenic, hepatic, or renal failure; or refractory systolic hypotension. The clinical worsening events during the 12-week treatment period of the Letairis clinical trials are shown in Table 3 and Figure 5.
- There was a significant delay in the time to clinical worsening for patients receiving Letairis compared to placebo. Results in subgroups such as the elderly were also favorable.
Long-term Treatment of PAH
- In long-term follow-up of patients who were treated with Letairis (2.5 mg, 5 mg, or 10 mg once daily) in the two pivotal studies and their open-label extension (N = 383), Kaplan-Meier estimates of survival at 1, 2, and 3 years were 93%, 85%, and 79%, respectively. Of the patients who remained on Letairis for up to 3 years, the majority received no other treatment for PAH. These uncontrolled observations do not allow comparison with a group not given Letairis and cannot be used to determine the long-term effect of Letairis on mortality.
Adverse Effects in Idiopathic Pulmonary Fibrosis (IPF)
- A randomized controlled study in patients with IPF, with or without pulmonary hypertension (WHO Group 3), compared Letairis (N = 329) to placebo (N = 163). The study was terminated after 34 weeks for lack of efficacy, and was found to demonstrate a greater risk of disease progression or death on Letairis. More patients taking Letairis died (8% vs. 4%), had a respiratory hospitalization (13% vs. 6%), and had a decrease in FVC/DLCO (17% vs. 12%).
How Supplied
- Letairis film-coated tablets are supplied as follows:
- Store at 25° C (77° F); excursions permitted to 15–30° C (59–86° F).
- Store Letairis in its original packaging.
Storage
There is limited information regarding Ambrisentan Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Ambrisentan |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Ambrisentan |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
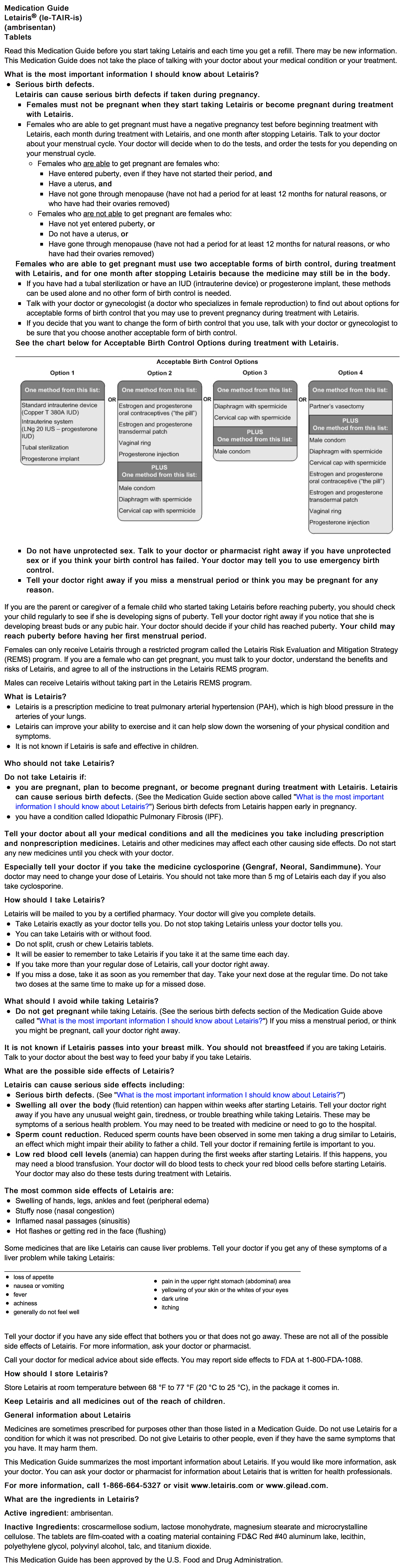
Precautions with Alcohol
- Alcohol-Ambrisentan interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Letairis®[1]
Look-Alike Drug Names
- Letairis® — Letaris®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "LETAIRIS (ambrisentan) tablet, film coated".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Ambrisentan |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Ambrisentan |Label Name=Ambrisentan10.png
}}
{{#subobject:
|Label Page=Ambrisentan |Label Name=Ambrisentan11.png
}}
{{#subobject:
|Label Page=Ambrisentan |Label Name=Ambrisentan12.png
}}