Acute pancreatitis CT: Difference between revisions
No edit summary |
|||
| (15 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Acute pancreatitis}} | {{Acute pancreatitis}} | ||
{{CMG}}; {{AE}} {{RT}} | {{CMG}}; {{AE}} {{RT}} | ||
==Overview== | ==Overview== | ||
Although [[ultrasound imaging]] and [[CT scanning]] of the [[abdomen]] can be used to confirm the diagnosis of pancreatitis, neither is usually necessary as a primary diagnostic modality<ref name="pmid12792243">{{cite journal |author=Fleszler F, Friedenberg F, Krevsky B, Friedel D, Braitman L |title=Abdominal computed tomography prolongs length of stay and is frequently unnecessary in the evaluation of acute pancreatitis |journal=Am J Med Sci |volume=325 |issue=5 |pages=251-5 |year=2003 |id=PMID 12792243}}</ref> | |||
. In addition, CT contrast may exacerbate pancreatitis,<ref name="pmid8678000">{{cite journal |author=McMenamin D, Gates L |title=A retrospective analysis of the effect of contrast-enhanced CT on the outcome of acute pancreatitis |journal=Am J Gastroenterol |volume=91|issue=7 |pages=1384-7 |year=1996 |id=PMID 8678000}}</ref> although this is disputed.<ref name="pmid10722029">{{cite journal|author=Hwang T, Chang K, Ho Y |title=Contrast-enhanced dynamic computed tomography does not aggravate the clinical severity of patients with severe acute pancreatitis: reevaluation of the effect of intravenous contrast medium on the severity of acute pancreatitis|journal=Arch Surg |volume=135 |issue=3 |pages=287-90 |year=2000 |id=PMID 10722029}}</ref><ref name="acutepancreatitis">{{cite journal | |||
| last = Forsmark | |||
| first = Chris E. | |||
| last2 = Vege | |||
| first2 = Santhi Swaroop | |||
| last3 = Wilcox | |||
| first3 = Mel | |||
| date = November 17,2016 | |||
| title = Acute Pancreatitis | |||
| url = http://www.nejm.org/doi/full/10.1056/NEJMra1505202 | |||
| journal = The New England Journal of Medicine | |||
| volume = | |||
| issue = | |||
| pages = 1972 - 1981 | |||
| doi = 10.1056/NEJMra1505202 | |||
| pmc = | |||
| pmid = | |||
| access-date = November 25,2016 | |||
| name-list-format = vanc | |||
}}</ref> | |||
==CT== | |||
== | |||
Regarding the need for [[computed tomography]], practice guidelines state: | Regarding the need for [[computed tomography]], practice guidelines state: | ||
: 2006: "Many patients with acute pancreatitis do not require a [[CT scan]] at admission or at any time during the [[hospitalization]]. For example, a [[CT scan]] is usually not essential in patients with recurrent mild pancreatitis caused by alcohol. A reasonable indication for a [[CT scan]] at admission (but not necessarily a [[CT]] with IV contrast) is to distinguish acute pancreatitis from another serious intra-abdominal condition, such as a [[perforated ulcer]]." <ref name="pmid17032204">{{cite journal |author=Banks P, Freeman M |title=Practice guidelines in acute pancreatitis |journal=Am J Gastroenterol |volume=101 |issue=10 |pages=2379-400 |year=2006 |id=PMID 17032204 | doi=10.1111/j.1572-0241.2006.00856.x}}</ref><ref name="acutepancreatitis">{{cite journal | |||
| last = Forsmark | |||
| first = Chris E. | |||
| last2 = Vege | |||
| first2 = Santhi Swaroop | |||
| last3 = Wilcox | |||
| first3 = Mel | |||
| date = November 17,2016 | |||
| title = Acute Pancreatitis | |||
| url = http://www.nejm.org/doi/full/10.1056/NEJMra1505202 | |||
| journal = The New England Journal of Medicine | |||
| volume = | |||
| issue = | |||
| pages = 1972 - 1981 | |||
| doi = 10.1056/NEJMra1505202 | |||
| pmc = | |||
| pmid = | |||
| access-date = November 25,2016 | |||
| name-list-format = vanc | |||
}}</ref> | |||
: 2005: "Patients with persisting organ failure, signs of [[sepsis]], or deterioration in clinical status 6–10 days after admission will require [[CT]] (recommendation grade B)."<ref name="pmid15831893">{{cite journal |author=UK Working Party on Acute Pancreatitis |title=UK guidelines for the management of acute pancreatitis |journal=Gut |volume=54 Suppl 3 |issue= |pages=iii1-9 |year=2005 |id=PMID 15831893 | doi=10.1136/gut.2004.057026 | url=http://gut.bmj.com/cgi/content/full/54/suppl_3/iii1}}</ref> | |||
: 2005: "Patients with persisting organ failure, signs of sepsis, or deterioration in clinical status 6–10 days after admission will require CT (recommendation grade B)."<ref name="pmid15831893">{{cite journal |author=UK Working Party on Acute Pancreatitis |title=UK guidelines for the management of acute pancreatitis |journal=Gut |volume=54 Suppl 3 |issue= |pages=iii1-9 |year=2005 |id=PMID 15831893 | doi=10.1136/gut.2004.057026 | url=http://gut.bmj.com/cgi/content/full/54/suppl_3/iii1}}</ref | |||
CT abdomen should not be performed before the 1st 48 hours of onset of symptoms as early [[CT]] (<48 h) may result in equivocal or normal findings. | |||
[ | CT findings can be classified into the following categories for easy recall : | ||
*Intrapancreatic - diffuse or segmental enlargement, [[edema]], gas bubbles, [[Pancreatic pseudocyst|pancreatic pseudocysts]] and phlegmons/[[abscesses]] (which present 4 to 6 weeks after initial onset) | |||
*Peripancreatic / extrapancreatic - irregular pancreatic outline, obliterated peripancreatic fat, [[retroperitoneal]] [[edema]], fluid in the lesser sac, fluid in the left [[anterior]] pararenal space | |||
*Locoregional - [[Gerota's fascia]] sign (thickening of inflamed [[Gerota's fascia]], which becomes visible), pancreatic [[ascites]], [[pleural effusion]] (seen on basal cuts of the [[pleural cavity]]), [[adynamic ileus]], | |||
===Balthazar Scoring=== | |||
Balthazar Scoring for the grading of acute pancreatitis: | |||
* The [[Computed tomography|CT]] severity score is the sum of the CT Grade and Necrosis Grade Scores. | |||
Balthazar Scoring for the | |||
The CT | |||
===== CT Grade Score: ===== | |||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 80: | Line 89: | ||
|} | |} | ||
Necrosis score | ===== Necrosis score: ===== | ||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 99: | Line 107: | ||
|} | |} | ||
[[Image:Acute-pancreatitis-8.jpg|500 px|thumb|center|Case courtesy of Dr Rahmoun Fateh, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/18850">rID: 18850</a>]] | |||
[[Image:Acute-pancreatitis.jpg|500 px|thumb|center|Case courtesy of <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/11163">rID: 11163</a>]] | |||
[[Image:Acute-pancreatitis-14 (1).jpg|500 px|thumb|center|Case courtesy of David Puyó, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/22434">rID: 22434</a>]] | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Gastroenterology]] | |||
[[Category:Surgery]] | |||
[[Category:Emergency medicine]] | |||
{{WS}} | |||
{{WH}} | {{WH}} | ||
Latest revision as of 18:59, 21 December 2017
|
Acute pancreatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acute pancreatitis CT On the Web |
|
American Roentgen Ray Society Images of Acute pancreatitis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Overview
Although ultrasound imaging and CT scanning of the abdomen can be used to confirm the diagnosis of pancreatitis, neither is usually necessary as a primary diagnostic modality[1] . In addition, CT contrast may exacerbate pancreatitis,[2] although this is disputed.[3][4]
CT
Regarding the need for computed tomography, practice guidelines state:
- 2006: "Many patients with acute pancreatitis do not require a CT scan at admission or at any time during the hospitalization. For example, a CT scan is usually not essential in patients with recurrent mild pancreatitis caused by alcohol. A reasonable indication for a CT scan at admission (but not necessarily a CT with IV contrast) is to distinguish acute pancreatitis from another serious intra-abdominal condition, such as a perforated ulcer." [5][4]
- 2005: "Patients with persisting organ failure, signs of sepsis, or deterioration in clinical status 6–10 days after admission will require CT (recommendation grade B)."[6]
CT abdomen should not be performed before the 1st 48 hours of onset of symptoms as early CT (<48 h) may result in equivocal or normal findings.
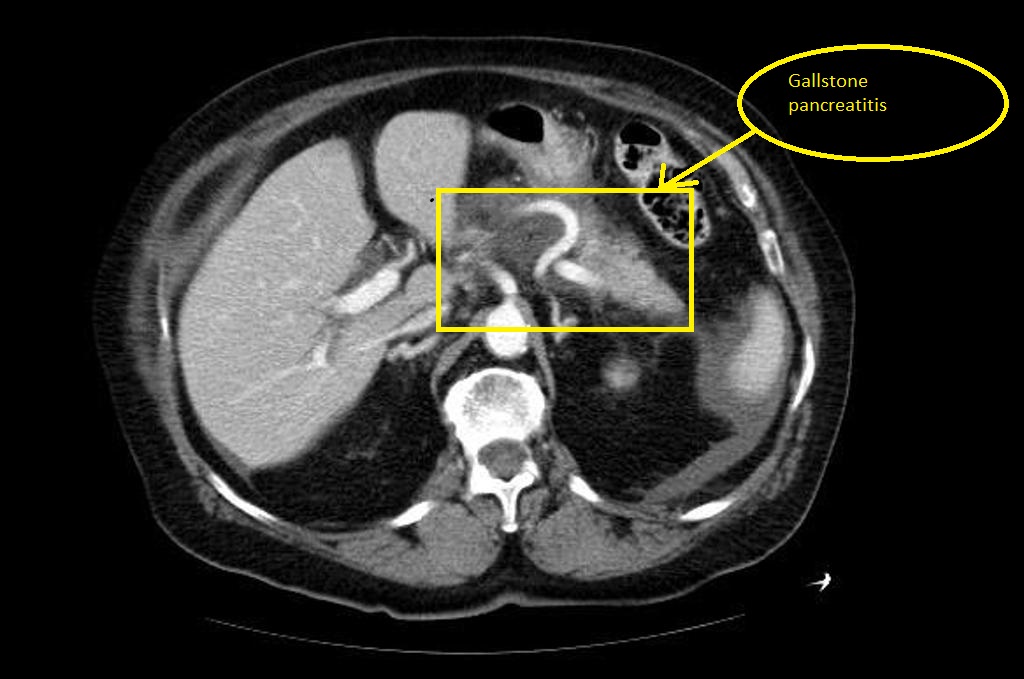
CT findings can be classified into the following categories for easy recall :
- Intrapancreatic - diffuse or segmental enlargement, edema, gas bubbles, pancreatic pseudocysts and phlegmons/abscesses (which present 4 to 6 weeks after initial onset)
- Peripancreatic / extrapancreatic - irregular pancreatic outline, obliterated peripancreatic fat, retroperitoneal edema, fluid in the lesser sac, fluid in the left anterior pararenal space
- Locoregional - Gerota's fascia sign (thickening of inflamed Gerota's fascia, which becomes visible), pancreatic ascites, pleural effusion (seen on basal cuts of the pleural cavity), adynamic ileus,
Balthazar Scoring
Balthazar Scoring for the grading of acute pancreatitis:
- The CT severity score is the sum of the CT Grade and Necrosis Grade Scores.
CT Grade Score:
| CT Grade | Appearance on CT | CT Grade Points |
|---|---|---|
| Grade A | Normal CT | 0 points |
| Grade B | Focal or diffuse enlargement of the pancreas | 1 point |
| Grade C | Pancreatic gland abnormalities and peripancreatic inflammation | 2 points |
| Grade D | Fluid collection in a single location | 3 points |
| Grade E | Two or more fluid collections and / or gas bubbles in or adjacent to pancreas | 4 points |
Necrosis score:
| Necrosis Percentage | Points |
|---|---|
| No necrosis | 0 points |
| 0 to 30% necrosis | 2 points |
| 30 to 50% necrosis | 4 points |
| Over 50% necrosis | 6 points |


References
- ↑ Fleszler F, Friedenberg F, Krevsky B, Friedel D, Braitman L (2003). "Abdominal computed tomography prolongs length of stay and is frequently unnecessary in the evaluation of acute pancreatitis". Am J Med Sci. 325 (5): 251–5. PMID 12792243.
- ↑ McMenamin D, Gates L (1996). "A retrospective analysis of the effect of contrast-enhanced CT on the outcome of acute pancreatitis". Am J Gastroenterol. 91 (7): 1384–7. PMID 8678000.
- ↑ Hwang T, Chang K, Ho Y (2000). "Contrast-enhanced dynamic computed tomography does not aggravate the clinical severity of patients with severe acute pancreatitis: reevaluation of the effect of intravenous contrast medium on the severity of acute pancreatitis". Arch Surg. 135 (3): 287–90. PMID 10722029.
- ↑ 4.0 4.1 Forsmark CE, Vege SS, Wilcox M (November 17,2016). "Acute Pancreatitis". The New England Journal of Medicine: 1972–1981. doi:10.1056/NEJMra1505202. Retrieved November 25,2016. Check date values in:
|access-date=, |date=(help) - ↑ Banks P, Freeman M (2006). "Practice guidelines in acute pancreatitis". Am J Gastroenterol. 101 (10): 2379–400. doi:10.1111/j.1572-0241.2006.00856.x. PMID 17032204.
- ↑ UK Working Party on Acute Pancreatitis (2005). "UK guidelines for the management of acute pancreatitis". Gut. 54 Suppl 3: iii1–9. doi:10.1136/gut.2004.057026. PMID 15831893.