ACC AHA guideline on the primary prevention of hypercholestrolemia: Difference between revisions
Jump to navigation
Jump to search
Gerald Chi (talk | contribs) mNo edit summary |
Gerald Chi (talk | contribs) mNo edit summary |
||
| Line 42: | Line 42: | ||
<font size="-3">''Clinical ASCVD is defined as acute coronary syndromes or history of MI, stable or unstable angina, coronary revascularization, stroke, or TIA presumed to be of atherosclerotic origin, and peripheral arterial disease or revascularization.''</font> | <font size="-3">''Clinical ASCVD is defined as acute coronary syndromes or history of MI, stable or unstable angina, coronary revascularization, stroke, or TIA presumed to be of atherosclerotic origin, and peripheral arterial disease or revascularization.''</font> | ||
==Risk Assessment in Primary Prevention== | |||
{| {{table}} | |||
| align="center" style="background:#f0f0f0;"|'''Rationale for the Expert Panel Approach to Primary Prevention Guidelines<ref name="circ.ahajournals.org">{{Cite web |last = | first = | title = 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults | url =http://circ.ahajournals.org/content/early/2013/11/11/01.cir.0000437738.63853.7a.full.pdf+html | publisher = | date = | accessdate = 13 November 2013 }}</ref>''' | |||
|- | |||
| 1. Cholesterol-lowering medications, particularly statins, are efficacious and effective for reducing risk for initial cardiovascular events. | |||
|- | |||
| 2. Statins are associated with similar relative-risk reductions for cardiovascular events across the majority of primary-prevention patient groups studied.* | |||
|- | |||
| 3. The extent of relative-risk reductions for ASCVD is proportional to the degree of LDL–C lowering observed on statin therapy. Therefore, more intensive statin therapy could reduce risk more than moderate- or lower-intensity statin therapy. | |||
|- | |||
| 4. According to consistent findings, the absolute benefit in ASCVD risk reduction is proportional to the baseline risk of the patient group or individual, and to the intensity of statin therapy. | |||
|- | |||
| 5. Patients or groups at higher baseline absolute risk, therefore, will derive greater absolute benefit from initiation of statin therapy over a period of 5 to 10 years. | |||
|- | |||
| 6. The absolute risk for adverse outcomes, including a small excess in cases of newly diagnosed diabetes, also appears to be proportional to the intensity of statin therapy. However, the adverse outcome of incident (or earlier diagnosis of) diabetes must be weighed in the context of the potentially fatal or debilitating occurrence of MI or stroke that could be prevented by statin therapy. | |||
|- | |||
| 7. The Expert Panel emphasizes that the occurrence of a major CVD event (MI or stroke) represents a much greater harm to health status than does an increase in blood glucose leading to a diagnosis of diabetes. The net absolute benefit of statin therapy may be considered as a comparison of the absolute risk reduction for CVD compared with the absolute excess risks including that for diabetes. Benefit also could be understood as a comparison of the number of statin-treated patients that would result in the prevention of 1 case of major ASCVD (NNT) with the number of statin-treated patients that would result in 1 excess case of diabetes (NNH). | |||
|- | |||
| 8. Because the absolute benefit in terms of CVD risk reduction depends on the baseline absolute risk for CVD, the absolute benefit from initiation of statin therapy is lower and would approach the risk for adverse effects in patients with lower baseline levels of predicted CVD risk. | |||
|- | |||
| 9. Available RCT evidence indicates a clear net absolute benefit of initiation of moderate-to-intensive statin therapy at a baseline estimated 10-year ASCVD risk of ≥7.5%. | |||
|- | |||
| 10. Available RCT evidence indicates that when baseline ASCVD risk is 5.0% to <7.5%, there is still net absolute benefit with moderate-intensity statin therapy. However, the tradeoffs between the ASCVD risk reduction benefit and adverse effects are less clear. Thus, a risk-benefit discussion is even more important for individuals with this range of ASCVD risk. The net benefit of high-intensity statin therapy appears to be marginal in such individuals. | |||
|- | |||
| '''Conclusion''' <BR> On the basis of the above tenets and its review of the evidence, this guideline recommends initiation of moderate or intensive statin therapy for patients who are eligible for primary CVD prevention and have a predicted 10-year “hard” ASCVD risk of ≥7.5%. This guideline recommends that initiation of moderate-intensity statin therapy be considered for patients with predicted 10-year “hard” ASCVD risk of 5.0% to <7.5%.or intensive statin therapy for patients who are eligible for primary CVD prevention and have a predicted 10-year “hard” ASCVD risk of ≥7.5%. This guideline recommends that initiation of moderate-intensity statin therapy be considered for patients with predicted 10-year “hard” ASCVD risk of 5.0% to <7.5%. | |||
|- | |||
|} | |||
==References== | ==References== | ||
Revision as of 21:33, 13 November 2013
Template:Hypercholesterolemia Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Primary Prevention in Adult ≥21 Years With LDL–C ≥190 mg/dL
- Adults ≥21 years of age with primary, severe elevations of LDL–C (≥190 mg/dL) have a high lifetime risk for ASCVD events and require even more substantial reductions in their LDL–C levels and intensive management of other risk factors to reduce their ASCVD event. It is reasonable to use high-intensity statin therapy to achieve at least a 50% reduction. In addition to a maximally tolerated dose of statin, nonstatin cholesterol-lowering medications are often needed to lower LDL–C to acceptable levels in these individuals.
- Because the hypercholesterolemia in these high-risk individuals is often genetically determined, family screening is especially important in this group to identify additional family members who would benefit from assessment and early treatment.
- Secondary causes of severe elevations of LDL–C ≥190 mg/dL and triglycerides ≥500 mg/dL often contribute to the magnitude of the hyperlipidemia and should be evaluated and treated appropriately. The most frequently encountered secondary conditions were excessive alcohol intake, uncontrolled diabetes mellitus and overt albuminuria.
| Secondary Cause | Elevated LDL–C | Elevated Triglycerides |
| Diet | Saturated or trans fats, weight gain, anorexia | Weight gain, very low-fat diets, high intake of refined carbohydrates, excessive alcohol intake |
| Drugs | Diuretics, cyclosporine, glucocorticoids, amiodarone | Oral estrogens, glucocorticoids, bile acid sequestrants, protease inhibitors, retinoic acid, anabolic steroids, sirolimus, raloxifene, tamoxifen, beta blockers (not carvedilol), thiazides |
| Diseases | Biliary obstruction, nephrotic syndrome | Nephrotic syndrome, chronic renal failure, lipodystrophies |
| Disorders and altered states of metabolism | Hypothyroidism, obesity, pregnancy* | Diabetes (poorly controlled), hypothyroidism, obesity; pregnancy* |
* Cholesterol and triglycerides rise progressively throughout pregnancy (81); treatment with statins, niacin, and ezetimibe are contraindicated during pregnancy and lactation.
Primary Prevention in Individuals With Diabetes
- The use of moderate-intensity statin therapy should be considered in individuals with diabetes that are 40 to 75 years of age since they are at substantially increased lifetime risk for ASCVD events and death. Moreover, individuals with diabetes experience greater morbidity and worse survival following the onset of clinical ASCVD.
- In persons with diabetes <40 or >75 years of age, statin therapy should be individualized based on considerations of ASCVD risk reduction benefits, the potential for adverse effects and drug-drug interactions, and patient preferences.
Primary Prevention in Individuals Without Diabetes and With LDL–C 70 to 189 mg/dL
- In individuals 40 to 75 years of age with LDL–C 70 to 189 mg/dL who are without clinical ASCVD or diabetes, initiation of statin therapy based on estimated 10-year ASCVD risk is recommended, regardless of sex, race or ethnicity.
- In individuals 40 to 75 years of age, who are not already candidates for statin therapy based on the presence of clinical ASCVD, diabetes, or LDL–C ≥190 mg/dL, it is recommended to receive statin therapy if they have a ≥7.5% estimated 10-year risk for ASCVD and LDL–C 70 to 189 mg/dL.
- Before initiating statin therapy, the clinician and patient discussion should include consideration of the potential for ASCVD risk reduction benefits, adverse effects, and drug-drug interactions. Additional factors may also be considered to inform treatment decision making in selected individuals. Factors that may contribute to assessment of ASCVD risk include primary LDL–C >160 mg/dL or other evidence of genetic hyperlipidemias, family history of premature ASCVD with onset <55 years of age in a first degree male relative or <65 years of age in a first degree female relative, high- sensitivity C-reactive protein >2 mg/L, coronary artery calcium score ≥300 Agatston units or ≥75 percentile for age, sex, and ethnicity, ankle brachial index <0.9, or elevated lifetime risk of ASCVD.
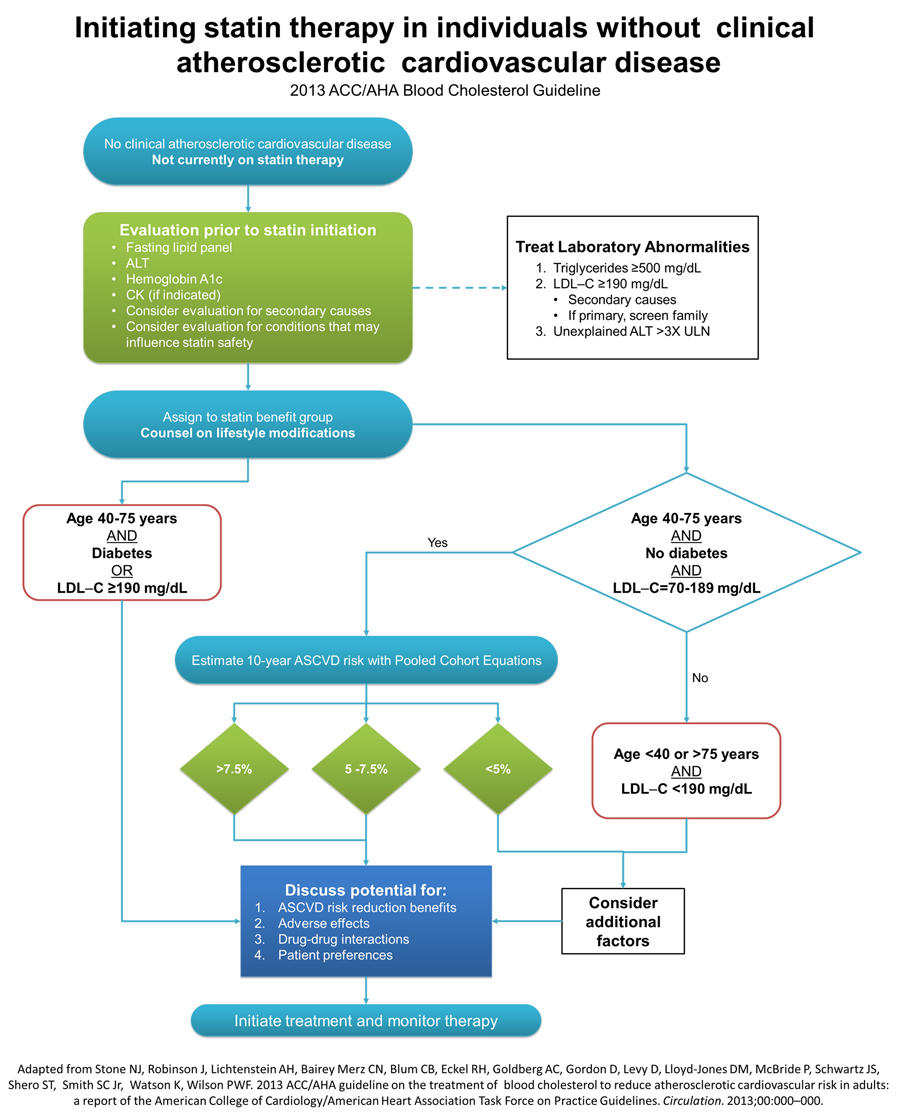
Initiating and Management of Statin Therapy in Individuals Without Clinical ASCVD
Clinical ASCVD is defined as acute coronary syndromes or history of MI, stable or unstable angina, coronary revascularization, stroke, or TIA presumed to be of atherosclerotic origin, and peripheral arterial disease or revascularization.
Risk Assessment in Primary Prevention
| Rationale for the Expert Panel Approach to Primary Prevention Guidelines[1] |
| 1. Cholesterol-lowering medications, particularly statins, are efficacious and effective for reducing risk for initial cardiovascular events. |
| 2. Statins are associated with similar relative-risk reductions for cardiovascular events across the majority of primary-prevention patient groups studied.* |
| 3. The extent of relative-risk reductions for ASCVD is proportional to the degree of LDL–C lowering observed on statin therapy. Therefore, more intensive statin therapy could reduce risk more than moderate- or lower-intensity statin therapy. |
| 4. According to consistent findings, the absolute benefit in ASCVD risk reduction is proportional to the baseline risk of the patient group or individual, and to the intensity of statin therapy. |
| 5. Patients or groups at higher baseline absolute risk, therefore, will derive greater absolute benefit from initiation of statin therapy over a period of 5 to 10 years. |
| 6. The absolute risk for adverse outcomes, including a small excess in cases of newly diagnosed diabetes, also appears to be proportional to the intensity of statin therapy. However, the adverse outcome of incident (or earlier diagnosis of) diabetes must be weighed in the context of the potentially fatal or debilitating occurrence of MI or stroke that could be prevented by statin therapy. |
| 7. The Expert Panel emphasizes that the occurrence of a major CVD event (MI or stroke) represents a much greater harm to health status than does an increase in blood glucose leading to a diagnosis of diabetes. The net absolute benefit of statin therapy may be considered as a comparison of the absolute risk reduction for CVD compared with the absolute excess risks including that for diabetes. Benefit also could be understood as a comparison of the number of statin-treated patients that would result in the prevention of 1 case of major ASCVD (NNT) with the number of statin-treated patients that would result in 1 excess case of diabetes (NNH). |
| 8. Because the absolute benefit in terms of CVD risk reduction depends on the baseline absolute risk for CVD, the absolute benefit from initiation of statin therapy is lower and would approach the risk for adverse effects in patients with lower baseline levels of predicted CVD risk. |
| 9. Available RCT evidence indicates a clear net absolute benefit of initiation of moderate-to-intensive statin therapy at a baseline estimated 10-year ASCVD risk of ≥7.5%. |
| 10. Available RCT evidence indicates that when baseline ASCVD risk is 5.0% to <7.5%, there is still net absolute benefit with moderate-intensity statin therapy. However, the tradeoffs between the ASCVD risk reduction benefit and adverse effects are less clear. Thus, a risk-benefit discussion is even more important for individuals with this range of ASCVD risk. The net benefit of high-intensity statin therapy appears to be marginal in such individuals. |
| Conclusion On the basis of the above tenets and its review of the evidence, this guideline recommends initiation of moderate or intensive statin therapy for patients who are eligible for primary CVD prevention and have a predicted 10-year “hard” ASCVD risk of ≥7.5%. This guideline recommends that initiation of moderate-intensity statin therapy be considered for patients with predicted 10-year “hard” ASCVD risk of 5.0% to <7.5%.or intensive statin therapy for patients who are eligible for primary CVD prevention and have a predicted 10-year “hard” ASCVD risk of ≥7.5%. This guideline recommends that initiation of moderate-intensity statin therapy be considered for patients with predicted 10-year “hard” ASCVD risk of 5.0% to <7.5%. |
References
- ↑ "2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults". Retrieved 13 November 2013.