21-hydroxylase deficiency pathophysiology: Difference between revisions
| Line 13: | Line 13: | ||
Since 21-hydroxylase activity is not involved in synthesis of [[androgen]]s, a substantial fraction of the large amounts of 17-hydroxypregnenolone is diverted to synthesis of dehydroepiandrostenedione ([[DHEA]]), [[androstenedione]], and [[testosterone]] beginning in the third month of fetal life in both sexes. | Since 21-hydroxylase activity is not involved in synthesis of [[androgen]]s, a substantial fraction of the large amounts of 17-hydroxypregnenolone is diverted to synthesis of dehydroepiandrostenedione ([[DHEA]]), [[androstenedione]], and [[testosterone]] beginning in the third month of fetal life in both sexes. | ||
Synthesis of [[aldosterone]] is also dependent on 21-hydroxylase activity. Although fetal production is impaired, it causes no prenatal effects, as the [[placenta]]l connection allows maternal blood to "dialyze" the fetus and maintain both [[electrolyte]] balance and blood volume. | Synthesis of [[aldosterone]] is also dependent on 21-hydroxylase activity. Although fetal production is impaired, it causes no prenatal effects, as the [[placenta]]l connection allows maternal blood to "dialyze" the fetus and maintain both [[electrolyte]] balance and blood volume. | ||
===Genetics=== | ===Genetics=== | ||
The ''CYP21'' gene for the [[P450]]c21 enzyme (also known as 21-hydroxylase) is at 6p21.3, amid genes ''HLA B'' and ''HLA DR'' coding for the major human histocompatibility loci ([[HLA]]). ''CYP21'' is paired with a nonfunctional [[pseudogene]] ''CYP21A''. Scores of abnormal [[allele]]s of CYP21 have been documented, mostly arising from [[recombination]]s of homologous regions of ''CYP21'' and ''CYP21A''. Differences in residual enzyme activity of the various alleles account for the various degrees of severity of the disease. The inheritance of all forms of congenital adrenal hyperplasia due to 21-hydroxylase deficiency is [[autosomal recessive]]. | The ''CYP21'' gene for the [[P450]]c21 enzyme (also known as 21-hydroxylase) is at 6p21.3, amid genes ''HLA B'' and ''HLA DR'' coding for the major human histocompatibility loci ([[HLA]]). ''CYP21'' is paired with a nonfunctional [[pseudogene]] ''CYP21A''. Scores of abnormal [[allele]]s of CYP21 have been documented, mostly arising from [[recombination]]s of homologous regions of ''CYP21'' and ''CYP21A''. Differences in residual enzyme activity of the various alleles account for the various degrees of severity of the disease. The inheritance of all forms of congenital adrenal hyperplasia due to 21-hydroxylase deficiency is [[autosomal recessive]]. | ||
Persons affected by any forms of the disease have two abnormal alleles, and both parents are usually carriers ([[heterozygote]]s). When parents both carry an abnormal allele, each child has a 25% chance of having the disease, a 50% chance of being an [[asymptomatic carrier]] like parents, and a 25% chance of having two normal genes. | Persons affected by any forms of the disease have two abnormal alleles, and both parents are usually carriers ([[heterozygote]]s). When parents both carry an abnormal allele, each child has a 25% chance of having the disease, a 50% chance of being an [[asymptomatic carrier]] like parents, and a 25% chance of having two normal genes. | ||
It is now possible to test for [[heterozygote|heterozygosity]] by measuring 17-hydroxyprogesterone elevation after [[ACTH]] stimulation, or more recently by direct gene sequencing. | It is now possible to test for [[heterozygote|heterozygosity]] by measuring 17-hydroxyprogesterone elevation after [[ACTH]] stimulation, or more recently by direct gene sequencing.<ref name="pmid19228439">{{cite journal| author=Trakakis E, Loghis C, Kassanos D| title=Congenital adrenal hyperplasia because of 21-hydroxylase deficiency. A genetic disorder of interest to obstetricians and gynecologists. | journal=Obstet Gynecol Surv | year= 2009 | volume= 64 | issue= 3 | pages= 177-89 | pmid=19228439 | doi=10.1097/OGX.0b013e318193301b | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19228439 }} </ref> | ||
__NOTOC__ | |||
{{Congenital adrenal hyperplasia}} | |||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | |||
==Overview== | |||
== Pathophysiology == | |||
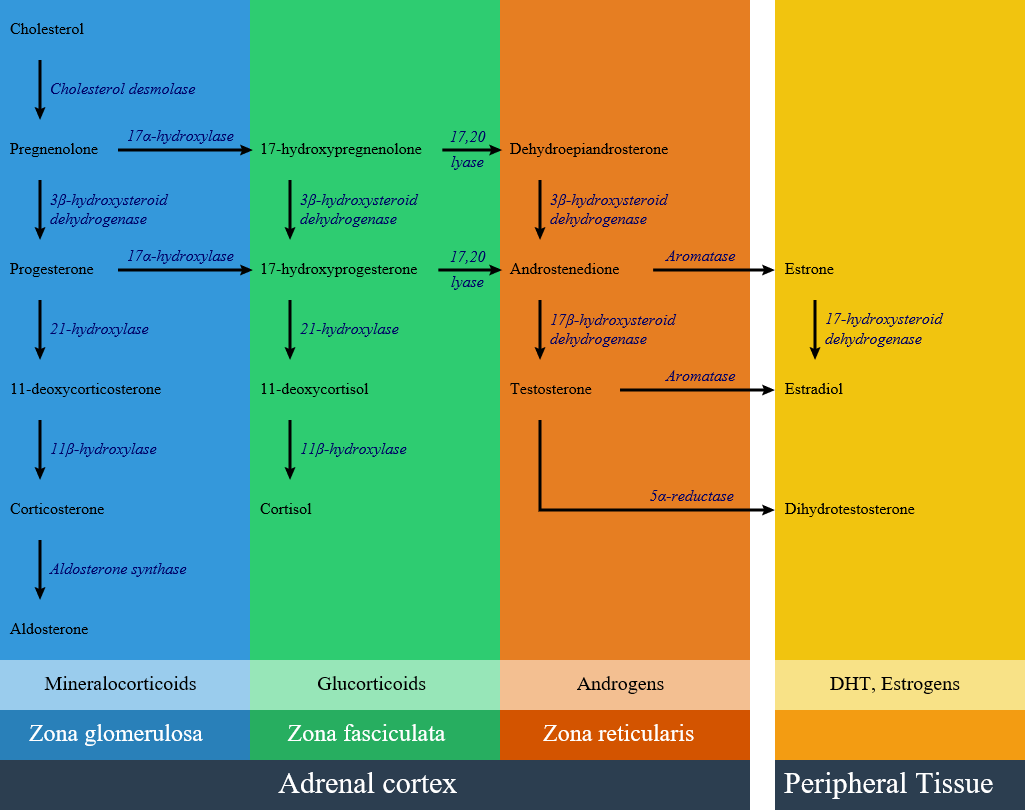
In patients with 21-hydroxylase deficiency, there is a defective conversion of 17-hydroxyprogesterone to 11-deoxycortisol which results in decreased cortisol synthesis and therefore increased corticotropin (ACTH) secretion and as a consequence of rising ACTH there is an increased production of androgens.<ref name="pmid10857554">{{cite journal |vauthors=White PC, Speiser PW |title=Congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=Endocr. Rev. |volume=21 |issue=3 |pages=245–91 |year=2000 |pmid=10857554 |doi=10.1210/edrv.21.3.0398 |url=}}</ref> | |||
[[image:Adrenal Steroids.png|600px]] | |||
More than 95% of all cases of CAH are caused by 21-hydroxylase deficiency (21-OHD); | |||
The clinical manifestation of congenital adrenal hyperplasia is closely related to the type and severity of impairment. | |||
== Genetics == | |||
* Congenital adrenal hyperplasia subtypes are all autosomal recessive and monogenetic. The disease manifestation follows the allele that results in a more functional enzyme, and generally correlation between genotype and phenotype is good.<ref name="pmid20926536">{{cite journal |vauthors=Finkielstain GP, Chen W, Mehta SP, Fujimura FK, Hanna RM, Van Ryzin C, McDonnell NB, Merke DP |title=Comprehensive genetic analysis of 182 unrelated families with congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=J. Clin. Endocrinol. Metab. |volume=96 |issue=1 |pages=E161–72 |year=2011 |pmid=20926536 |pmc=3038490 |doi=10.1210/jc.2010-0319 |url=}}</ref><ref name="pmid23359698">{{cite journal |vauthors=New MI, Abraham M, Gonzalez B, Dumic M, Razzaghy-Azar M, Chitayat D, Sun L, Zaidi M, Wilson RC, Yuen T |title=Genotype-phenotype correlation in 1,507 families with congenital adrenal hyperplasia owing to 21-hydroxylase deficiency |journal=Proc. Natl. Acad. Sci. U.S.A. |volume=110 |issue=7 |pages=2611–6 |year=2013 |pmid=23359698 |pmc=3574953 |doi=10.1073/pnas.1300057110 |url=}}</ref><ref name="pmid20926536">{{cite journal |vauthors=Finkielstain GP, Chen W, Mehta SP, Fujimura FK, Hanna RM, Van Ryzin C, McDonnell NB, Merke DP |title=Comprehensive genetic analysis of 182 unrelated families with congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=J. Clin. Endocrinol. Metab. |volume=96 |issue=1 |pages=E161–72 |year=2011 |pmid=20926536 |pmc=3038490 |doi=10.1210/jc.2010-0319 |url=}}</ref> | |||
* Responsible gene for 21 OH deficiency is CYP21A. This gene is located within the [[Human leukocyte antigen|human leucocyte antigen]] class III region of chromosome 6. CYP21A gene has two types: | |||
*# An active gene called CYP21A2, which encodes 21-hydroxylase, a cytochrome P450 type II enzyme of 495 amino acids. | |||
*# The other gene is a non-functional pseudogene named CYP21A1 or CYP21P. This pseudogene produces an enzyme with no activity because it lacks eight bases from codons 110-112, which results in a stop codon<ref name="pmid3487786">{{cite journal |vauthors=White PC, New MI, Dupont B |title=Structure of human steroid 21-hydroxylase genes |journal=Proc. Natl. Acad. Sci. U.S.A. |volume=83 |issue=14 |pages=5111–5 |year=1986 |pmid=3487786 |pmc=323900 |doi= |url=}}</ref> | |||
* Meiotic recombination events occurs in this genomic region as a result of the high degree of sequence homology between CYP21A2 and its pseudogene CYP21A1. | |||
** Approximately 70% of CYP21A2 disease is due to gene conversion and micro-deletions in CYP21A1 gen. | |||
** Approximately 25% to 30% are chimeric genes due to large deletions. | |||
** Approximately 1% to 2% of cases are due to de novo mutations because of high variability of the CYP21A2 locus. | |||
** Chromosome 6 uniparental disomy is rare cause of 21-hydroxylase deficiency with an unknown prevalence. | |||
Conventionally, classic 21OH deficiency is subclassified into salt wasting and simple virilising forms, which reflect the severity of aldosterone deficiency. Mutations that completely inactivate ''CYP21A2'' result in the salt-wasting phenotype, which, without neonatal screening, presents in the first 2 weeks of life with a life-threatening adrenal crisis ( table 2).<sup>23</sup> Patients with classic simple virilising congenital adrenal hyperplasia have mutations that retain 1–2% of 21OH activity and minimal aldosterone production prevents a neonatal crisis.<sup>40</sup> Excess fetal adrenal androgen exposure results in virilisation of external genitalia of 46,XX patients with classic 21OH deficiency (salt wasting and simple virilising; figure 3A). Without neonatal screening, male toddlers with the simple virilising form of the disorder are diagnosed with signs and symptoms of androgen excess. Postnatal excess androgen presence leads to premature growth of pubic hair and rapid skeletal growth in children. Patients with the non-classic form retain up to 50% of enzyme activity and mostly do not have adrenal insufficiency, but might have partial glucocorticoid deficiency, and female patients have normal genitalia.<sup>41</sup> Patients might present with mild androgen excess or have few or no symptoms. In fact, the term cryptic congenital adrenal hyperplasia was created to define patients with non-classic congenital adrenal hyperplasia who are identified by family genetic studies, but are otherwise asymptomatic.<sup>42</sup> | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Disease]] | |||
[[Category:Pediatrics]] | |||
[[Category:Endocrinology]] | |||
[[Category:Genetic disorders]] | |||
[[Category:Intersexuality]] | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
==References== | ==References== | ||
Revision as of 13:52, 12 July 2017
|
Congenital adrenal hyperplasia due to 21-hydroxylase deficiency Microchapters |
|
Differentiating Congenital adrenal hyperplasia due to 21-hydroxylase deficiency from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
21-hydroxylase deficiency pathophysiology On the Web |
|
American Roentgen Ray Society Images of 21-hydroxylase deficiency pathophysiology |
|
Directions to Hospitals Treating Congenital adrenal hyperplasia due to 21-hydroxylase deficiency |
|
Risk calculators and risk factors for 21-hydroxylase deficiency pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ahmad Al Maradni, M.D. [2]
Overview
Development of congenital adrenal hyperplasia due to 21-hydroxylase deficiency is the result of a defective P450c21 enzyme. Genes involved in the pathogenesis of congenital adrenal hyperplasia due to 21-hydroxylase deficiency include the CYP21 gene.
Pathophysiology
The defective enzyme P450c21, commonly referred to as 21-hydroxylase (21-OH), is embedded in the smooth endoplasmic reticulum of the cells of the adrenal cortex. It catalyzes hydroxylation of 17-hydroxyprogesterone to 11-deoxycortisol in the glucocorticoid pathway from pregnenolone to cortisol. It also catalyzes the hydroxylation of progesterone to 11-deoxycorticosterone (DOC) in the mineralocorticoid pathway from pregnenolone to aldosterone. Deficient activity of this enzyme reduces the efficiency of cortisol synthesis, with consequent elevation of adrenocorticotropic hormone (ACTH) levels and hyperplasia of the adrenal cortex. ACTH stimulates uptake of cholesterol and synthesis of pregnenolone. Steroid precursors up to and including progesterone, 17-hydroxypregnenolone, and especially 17-hydroxyprogesterone (17OHP) accumulate in the adrenal cortex and in circulating blood. Blood levels of 17OHP can reach 10-1000 times the normal concentration.
Since 21-hydroxylase activity is not involved in synthesis of androgens, a substantial fraction of the large amounts of 17-hydroxypregnenolone is diverted to synthesis of dehydroepiandrostenedione (DHEA), androstenedione, and testosterone beginning in the third month of fetal life in both sexes.
Synthesis of aldosterone is also dependent on 21-hydroxylase activity. Although fetal production is impaired, it causes no prenatal effects, as the placental connection allows maternal blood to "dialyze" the fetus and maintain both electrolyte balance and blood volume.
Genetics
The CYP21 gene for the P450c21 enzyme (also known as 21-hydroxylase) is at 6p21.3, amid genes HLA B and HLA DR coding for the major human histocompatibility loci (HLA). CYP21 is paired with a nonfunctional pseudogene CYP21A. Scores of abnormal alleles of CYP21 have been documented, mostly arising from recombinations of homologous regions of CYP21 and CYP21A. Differences in residual enzyme activity of the various alleles account for the various degrees of severity of the disease. The inheritance of all forms of congenital adrenal hyperplasia due to 21-hydroxylase deficiency is autosomal recessive.
Persons affected by any forms of the disease have two abnormal alleles, and both parents are usually carriers (heterozygotes). When parents both carry an abnormal allele, each child has a 25% chance of having the disease, a 50% chance of being an asymptomatic carrier like parents, and a 25% chance of having two normal genes.
It is now possible to test for heterozygosity by measuring 17-hydroxyprogesterone elevation after ACTH stimulation, or more recently by direct gene sequencing.[1]
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [4]
Overview
Pathophysiology
In patients with 21-hydroxylase deficiency, there is a defective conversion of 17-hydroxyprogesterone to 11-deoxycortisol which results in decreased cortisol synthesis and therefore increased corticotropin (ACTH) secretion and as a consequence of rising ACTH there is an increased production of androgens.[2]
More than 95% of all cases of CAH are caused by 21-hydroxylase deficiency (21-OHD);
The clinical manifestation of congenital adrenal hyperplasia is closely related to the type and severity of impairment.
Genetics
- Congenital adrenal hyperplasia subtypes are all autosomal recessive and monogenetic. The disease manifestation follows the allele that results in a more functional enzyme, and generally correlation between genotype and phenotype is good.[3][4][3]
- Responsible gene for 21 OH deficiency is CYP21A. This gene is located within the human leucocyte antigen class III region of chromosome 6. CYP21A gene has two types:
- An active gene called CYP21A2, which encodes 21-hydroxylase, a cytochrome P450 type II enzyme of 495 amino acids.
- The other gene is a non-functional pseudogene named CYP21A1 or CYP21P. This pseudogene produces an enzyme with no activity because it lacks eight bases from codons 110-112, which results in a stop codon[5]
- Meiotic recombination events occurs in this genomic region as a result of the high degree of sequence homology between CYP21A2 and its pseudogene CYP21A1.
- Approximately 70% of CYP21A2 disease is due to gene conversion and micro-deletions in CYP21A1 gen.
- Approximately 25% to 30% are chimeric genes due to large deletions.
- Approximately 1% to 2% of cases are due to de novo mutations because of high variability of the CYP21A2 locus.
- Chromosome 6 uniparental disomy is rare cause of 21-hydroxylase deficiency with an unknown prevalence.
Conventionally, classic 21OH deficiency is subclassified into salt wasting and simple virilising forms, which reflect the severity of aldosterone deficiency. Mutations that completely inactivate CYP21A2 result in the salt-wasting phenotype, which, without neonatal screening, presents in the first 2 weeks of life with a life-threatening adrenal crisis ( table 2).23 Patients with classic simple virilising congenital adrenal hyperplasia have mutations that retain 1–2% of 21OH activity and minimal aldosterone production prevents a neonatal crisis.40 Excess fetal adrenal androgen exposure results in virilisation of external genitalia of 46,XX patients with classic 21OH deficiency (salt wasting and simple virilising; figure 3A). Without neonatal screening, male toddlers with the simple virilising form of the disorder are diagnosed with signs and symptoms of androgen excess. Postnatal excess androgen presence leads to premature growth of pubic hair and rapid skeletal growth in children. Patients with the non-classic form retain up to 50% of enzyme activity and mostly do not have adrenal insufficiency, but might have partial glucocorticoid deficiency, and female patients have normal genitalia.41 Patients might present with mild androgen excess or have few or no symptoms. In fact, the term cryptic congenital adrenal hyperplasia was created to define patients with non-classic congenital adrenal hyperplasia who are identified by family genetic studies, but are otherwise asymptomatic.42
References
- ↑ Trakakis E, Loghis C, Kassanos D (2009). "Congenital adrenal hyperplasia because of 21-hydroxylase deficiency. A genetic disorder of interest to obstetricians and gynecologists". Obstet Gynecol Surv. 64 (3): 177–89. doi:10.1097/OGX.0b013e318193301b. PMID 19228439.
- ↑ White PC, Speiser PW (2000). "Congenital adrenal hyperplasia due to 21-hydroxylase deficiency". Endocr. Rev. 21 (3): 245–91. doi:10.1210/edrv.21.3.0398. PMID 10857554.
- ↑ 3.0 3.1 Finkielstain GP, Chen W, Mehta SP, Fujimura FK, Hanna RM, Van Ryzin C, McDonnell NB, Merke DP (2011). "Comprehensive genetic analysis of 182 unrelated families with congenital adrenal hyperplasia due to 21-hydroxylase deficiency". J. Clin. Endocrinol. Metab. 96 (1): E161–72. doi:10.1210/jc.2010-0319. PMC 3038490. PMID 20926536.
- ↑ New MI, Abraham M, Gonzalez B, Dumic M, Razzaghy-Azar M, Chitayat D, Sun L, Zaidi M, Wilson RC, Yuen T (2013). "Genotype-phenotype correlation in 1,507 families with congenital adrenal hyperplasia owing to 21-hydroxylase deficiency". Proc. Natl. Acad. Sci. U.S.A. 110 (7): 2611–6. doi:10.1073/pnas.1300057110. PMC 3574953. PMID 23359698.
- ↑ White PC, New MI, Dupont B (1986). "Structure of human steroid 21-hydroxylase genes". Proc. Natl. Acad. Sci. U.S.A. 83 (14): 5111–5. PMC 323900. PMID 3487786.