Peutz-Jeghers syndrome
| Peutz-Jeghers syndrome | |
 | |
|---|---|
| ICD-10 | Q85.8 |
| ICD-9 | 759.6 |
| OMIM | 175200 |
| DiseasesDB | 9905 |
| MeSH | D010580 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
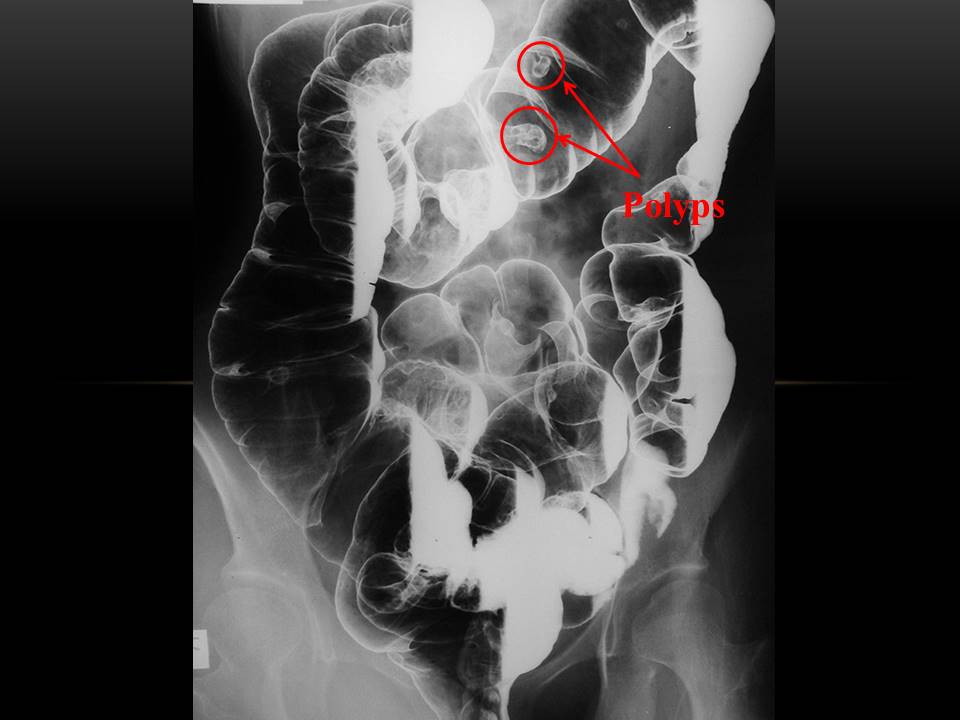
Peutz-Jeghers, also known as Hereditary Intestinal Polyposis Syndrome, is an autosomal dominant genetic disease characterized by the development of benign hamartomatous polyps in the gastrointestinal tract.
Diagnosis
The three main criteria for diagnosis are:
- Family history
- Mucocutaneous lesions causing patches of hyperpigmentation in the mouth and on the hands and feet. The oral pigmentations are the first on the body to appear, and thus play an important part in early diagnosis. Intraorally, they are most frequently seen on the gingiva, hard palate and inside of the cheek. The mucosa of the lower lip is almost invariably involved as well.
- Hamartomatous polyps in the gastrointestinal tract. These are benign polyps with a extraordinarily low potential for malignancy.
Having 2 of the 3 listed criteria indicates a positive diagnosis. The oral findings are consistent with other conditions, such as Addison's disease and McCune-Albright syndrome, and these should be included in the differential diagnosis. Definitive diagnosis requires a histological sample of a polyp.
Causes of Peutz-Jeghers syndrome
Genetics
In 1998, a gene was found to be associated with the mutation. On chromosome 19, the gene known as STK11 (LKB1)[1] is a possible tumor suppressor gene. It is inherited in an Autosomal Dominant pattern (see Mendelian inheritance) which means that anyone who has PJS has a 50% chance of passing it onto their children.
History & Symptoms
The risks associated with this syndrome include a strong tendency of developing cancer in multiple sites[2]. While the harmartomatous polyps themselves do not have malignant potential, patients with the syndrome have an increased risk of developing carcinomas of the pancreas, liver, lungs, breast, ovaries, uterus and testicles.
The average age of first diagnosis is 23, but the lesions can be identified at birth by an astute pediatrician. Prior to puberty, the mucocutaneous lesions can be found on the palms and soles. Often the first presentation is as a bowel obstruction from an intussusception which is a common cause of mortality; an intussusception is a telescoping of one loop of bowel into another segment.
Most of the data regarding this disorder are from selected family lines and thus the risks endured by those families regarding outcomes may not translate completely to the patient without a familial history.
Natural history, Complications, and Prognosis
Almost half of Peutz-Jeghers patients die from cancer by age 57 years, and the cumulative risk of developing a form of cancer associated with Peutz-Jeghers syndrome between ages 15-64 is 93%.[3]
Screening
Screening includes upper GI endoscopy, enteroclysis, and colonoscopy to check for the locations of the hamartomas. To check for cancerous lesions, endoscopic ultrasound, testicular ultrasound and imaging studies of the liver and the pancreas are indicated because of the risk of pancreatic cancer as well as gallbladder polyps and cancer. These imaging studies may include ultrasonography as well as CT with pancreatic details or magnetic resonance cholangiopancreatography (MRCP).
In addition, an annual physical examination that includes evaluation of the breasts, abdomen, pelvis, and testes should be done by a physician. An annual complete blood count to check for anemia should be done. If bleeding is found, removal of hemorrhagic or large polyps (>5 mm) by endoscopic polypectomy should be performed.
Some suggestions for surveillance for cancer include the following: Small intestine with small bowel radiography every 2 years, Esophagogastroduodenoscopy and colonoscopy every 2 years, Ultrasound of the pancreas yearly, Ultrasound of the pelvis (women) and testes (men) yearly, Mammography (women) at ages 25, 30, 35, and 38 years, then every 2 years until age 50 years, then annually, and Papanicolaou (Pap) test every year
Follow-up care should be supervised by a gastroenterologist familiar with Peutz-Jeghers syndrome. Genetic consultation and counseling as well as urological and gynecological consultations are required in the management of these patients.
References
- ↑ "UniProtKB/Swiss-Prot entry Q15831 [STK11_HUMAN] Serine/threonine-protein kinase 11". Retrieved 2007-07-21.
- ↑ Boardman LA, Thibodeau SN, Schaid DJ; et al. (1998). "Increased risk for cancer in patients with the Peutz-Jeghers syndrome". Ann. Intern. Med. 128 (11): 896–9. PMID 9634427.
- ↑ "eMedicine - Peutz-Jeghers Syndrome : Article by Andrea Duchini, MD". Retrieved 2007-07-21.
Template:Digestive system neoplasia
de:Peutz-Jeghers-Syndrom
it:Sindrome di Peutz-Jeghers
nl:Syndroom van Peutz-Jeghers