Colonoscopy
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Template:Interventions infobox
|
WikiDoc Resources for Colonoscopy |
|
Articles |
|---|
|
Most recent articles on Colonoscopy Most cited articles on Colonoscopy |
|
Media |
|
Powerpoint slides on Colonoscopy |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Colonoscopy at Clinical Trials.gov Clinical Trials on Colonoscopy at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Colonoscopy
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Colonoscopy Discussion groups on Colonoscopy Patient Handouts on Colonoscopy Directions to Hospitals Treating Colonoscopy Risk calculators and risk factors for Colonoscopy
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Colonoscopy |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Colonoscopy is the endoscopic examination of the large colon and the distal part of the small bowel with a CCD camera or a fiber optic camera on a flexible tube passed through the anus. It may provide a visual diagnosis (e.g. ulceration, polyps) and grants the opportunity for biopsy or removal of suspected lesions. Virtual colonoscopy, which uses 2D and 3D imagery reconstructed from computed tomography (CT) scans or from nuclear magnetic resonance (MR) scans, is also possible, as a totally non-invasive medical test, although it is not standard and still under investigation regarding its diagnostic abilities. Furthermore, virtual colonoscopy does not allow for therapeutic maneuvers such as polyp/tumor removal or biopsy nor visualization of lesions smaller than 5 millimeters. If a growth or polyp is detected using CT colonography, a standard colonoscopy would still need to be performed. Colonoscopy can remove polyps smaller than one millimeter. Once polyps are removed, they can be studied with the aid of a microscope to determine if they are precancerous or not. Colonoscopy is similar but not the same as sigmoidoscopy. The difference between colonoscopy and sigmoidoscopy is related to which parts of the colon each can examine. Sigmoidoscopy allows doctors to view only the final two feet of the colon, while colonoscopy allows an examination of the entire colon, which measures four to five feet in length. Often a sigmoidoscopy is used as a screening procedure for a full colonoscopy.
Uses
Indications for colonoscopy include gastrointestinal hemorrhage, unexplained changes in bowel habit or suspicion of malignancy. Colonoscopies are often used to diagnose colon cancer, but are also frequently used to diagnose inflammatory bowel disease. In older patients (sometimes even younger ones) an unexplained drop in hematocrit (one sign of anemia) is an indication to do a colonoscopy, usually along with an EGD (esophagoastroduodenoscopy), even if no obvious blood has been seen in the stool (feces).
Fecal occult blood is a quick test which can be done to test for microscopic traces of blood in the stool. A positive test is almost always an indication to do a colonoscopy. In most cases the positive result is just due to hemorrhoids; however, it can also be due to diverticulosis, inflammatory bowel disease (Crohn's disease, ulcerative colitis), colon cancer, or polyps. However--since its development by Dr. Hiromi Shinya in the 1960's--polypectomy has become a routine part of colonoscopy, allowing for quick and simple removal of polyps without invasive surgery.[1]
Due to the high mortality associated with colon cancer and the high effectivity and low risks associated with colonoscopy, it is now also becoming a routine screening test for people 50 years of age or older. Subsequent rescreenings are then scheduled based on the initial results found, with a five- or ten-year recall being common for colonoscopies that produce normal results.
Procedure
Preparation
The patient may be asked to skip aspirin and aspirin products such as salicylate for up to ten days before the procedure to avoid the risk of bleeding if a polypectomy is performed during the procedure. Often a blood test is performed before the procedure and upon a low platelet count, a clot time test may be done. A clotting time greater than ten minutes may contraindicate polyp removal. Many laboratories are not performing bleeding times any more, as platelet function tests are replacing it.[2][3]
The colon must be free of solid matter for the test to be performed properly. For one to three days, the patient is required to follow a low fibre or clear-fluid only diet. Examples of clear fluids are apple juice, bouillon, artificially flavored lemon-lime soda or sports drink, and of course water. As orange juice, prune juice, and milk contain fibre, they are banned from the list, as are liquids dyed red, orange, purple, or brown, such as cola or coffee. On the day before the colonoscopy, the patient is either given a laxative preparation (such as Bisacodyl, phospho soda, sodium picosulfate, or sodium phosphate and/or magnesium citrate) and large quantities of fluid or whole bowel irrigation is performed using a solution of polyethylene glycol and electrolytes.
The most effective bowel preparation is split dose of polyethylene glycol.[4][5]
The investigation
During the procedure the patient is often given sedation intravenously, employing agents such as midazolam or fentanyl. Although meperidine (Demerol) may be used as an alternative to fentanyl, the concern of seizures has relegated this agent to second choice for sedation behind the combination of midazolam and fentanyl. The average person will receive a combination of these two drugs, usually between 1-4 mg iv midazolam, and 25 to 100 µg iv fentanyl. Sedation practices vary between practitioners and nations; in some clinics in Norway, sedation is rarely administered.[6][7] Some endocoscopists are experimenting with, or routinely use, alternative or additional methods such as nitrous oxide[8][9] and propofol[10], which have advantages and disadvantages relating to recovery time (particularly the duration of amnesia after the procedure is complete), patient experience, and the degree of supervision needed for safe administration. This sedation is called "twilight anesthesia" and for some patients it doesn't take and they are indeed awake for the procedure and watch the inside of their colon on the color monitor.
The first step is usually a digital rectal examination, to examine the tone of the sphincter and to determine if preparation has been adequate. The endoscope is then passed though the anus up the rectum, the colon (sigmoid, descending, transverse and ascending colon, the cecum), and ultimately the terminal ileum. The endoscope has a movable tip and multiple channels for instrumentation, air, suction and light. The bowel is occasionally insufflated with air to maximize visibility. Biopsies are frequently taken for histology.
In most experienced hands, the endoscope is advanced to the junction of where the colon and small bowel join up (cecum) in under 10 minutes in 95% of cases. Due to tight turns and redundancy in areas of the colon that are not "fixed", loops may form in which advancement of the endoscope creates a "bowing" effect that causes the tip to actually retract. These loops often result in discomfort due to stretching of the colon and its associated mesentery. Maneuvers to "reduce" or remove the loop include pulling the endoscope backwards while torquing the instrument. Alternatively, body position changes and abdominal support from external hand pressure can often "straighten" the endoscope to allow the scope to move forward. In a minority of patients, looping is often cited as a cause for an incomplete examination. Usage of alternative instruments leading to completion of the examination has been investigated, including use of pediatric colonscope, push enteroscope and upper GI endoscope variants.[11]
For screening purposes, a closer visual inspection is then often performed upon withdrawal of the endoscope over the course of 20 to 25 minutes. Lawsuits over missed cancerous lesions have prompted recent institutions to better document withdrawal time as rapid withdrawal times may be a source of potential medical legal liability.[12] This is often a real concern in private practice settings where high throughput of cases have been postulated as a financial incentive to complete colonoscopies as quickly as possible.
Suspicious lesions may be cauterized, treated with laser light or cut with an electric wire for purposes of biopsy or complete removal polypectomy. Medication can be injected, e.g. to control bleeding lesions. On average, the procedure takes 20-30 minutes, depending on the indication and findings. With multiple polypectomies or biopsies, procedure times may be longer. As mentioned above, anatomic considerations may also affect procedure times.
After the procedure, some recovery time is usually allowed to let the sedative wear off. Most facilities require that patients have a person with them to help them home afterwards (again, depending on the sedation method used).
One very common aftereffect from the procedure is a bout of flatulence and minor wind pain caused by air insufflation into the colon during the procedure.
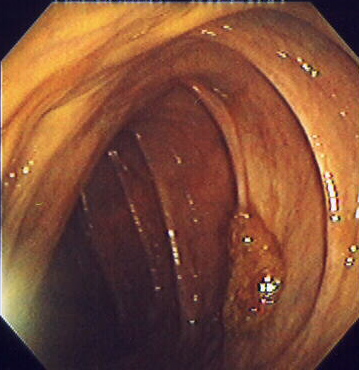
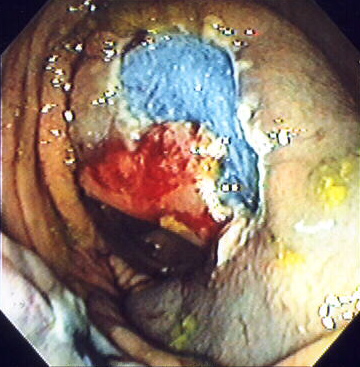
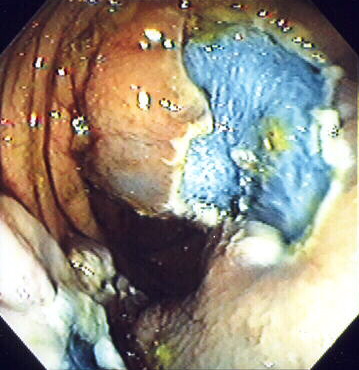
An advantage of colonoscopy over x-ray imaging or other, less invasive tests, is the ability to perform therapeutic interventions during the test. If a polyp is found, for example, it can be removed by one of several techniques. A snare can be placed around a polyp for removal. Even if the polyp is flat on the surface it can often be removed. For example, the following show a polyp removed in stages.
1. Polyp is identified.
2. A sterile solution is injected under the polyp to lift it away from deeper tissues.

3. A portion of the polyp is now removed.
4. The polyp is fully removed.
Risks
This procedure has a low (0.2%) risk of serious complications.
The most serious complication is a tear or hole in the lining of the colon called a gastrointestinal perforation, which is life-threatening and requires immediate major surgery for repair; however, the rate of perforation is less than 1 in 2000 colonoscopies.
Bleeding complications may be treated immediately during the procedure by cauterization via the instrument. Delayed bleeding may also occur at the site of polyp removal up to a week after the procedure and a repeat procedure can then be performed to treat the bleeding site. Even more rarely, splenic rupture can occur after colonoscopy because of adhesions between the colon and the spleen.
As with any procedure involving anaesthesia, other complications would include cardiopulmonary complications such as temporary drop in blood pressure and oxygen saturation, usually the result of overmedication and easily reversed. In rare cases, more serious cardiopulmonary events such as a heart attack, stroke, or even death may occur; these are extremely rare except in critically ill patients with multiple risk factors.
References
- ↑ Sivak, Jr., Michael V. (2004-12). "Polypectomy: Looking Back". Gastrointestinal Endoscopy. 60 (6): 977–982. ISSN 1097-6779. Check date values in:
|date=(help) - ↑ Decker, Joe (15 November 2006). "Preparation: Diet" (Blog). Colonoscopy Blog. Blogger.com. Retrieved 2007-06-12.
- ↑ "Colyte/Trilyte Colonoscopy Preparation" (PDF). Palo Alto Medical Foundation. 2006. Retrieved 2007-06-12. Unknown parameter
|month=ignored (help) - ↑ Kilgore TW, Abdinoor AA, Szary NM, Schowengerdt SW, Yust JB, Choudhary A; et al. (2011). "Bowel preparation with split-dose polyethylene glycol before colonoscopy: a meta-analysis of randomized controlled trials". Gastrointest Endosc. 73 (6): 1240–5. doi:10.1016/j.gie.2011.02.007. PMID 21628016.
- ↑ American Society of Colon and Rectal Surgeons (ASCRS). American Society for Gastrointestinal Endoscopy (ASGE). Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Wexner SD, Beck DE, Baron TH; et al. (2006). "A consensus document on bowel preparation before colonoscopy: prepared by a Task Force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES)". Surg Endosc. 20 (7): 1161. doi:10.1007/s00464-006-3037-1. PMID 16799744.
- ↑ Bretthauer, M (20 May 2004). "[Systematic quality control programme for colonoscopy in an endoscopy centre in Norway]". Tidsskrift for den Norske laegeforening (Abstract)
|format=requires|url=(help) (in Norwegian). 124 (10): 1402&ndash, 1405. ISSN 0029-2001. PMID 15195182. Unknown parameter|coauthors=ignored (help);|access-date=requires|url=(help) - ↑ The article PMID 20514160 was cited here, but this UID appears to be incorrect.
- ↑ Rikshospitalet University Hospital (2006). "Clinical Trial: Nitrous Oxide for Analgesia During Colonoscopy". ClinicalTrials.gov. Retrieved 2007-06-12. Unknown parameter
|month=ignored (help) - ↑ Forbes, GM (2000). "Nitrous oxide for colonoscopy: a randomized controlled study". Gastrointestinal Endoscopy. 51 (3): 271&ndash, 277. PMID 10699770. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help);|access-date=requires|url=(help) - ↑ Clarke, Anthony C (18 February 2002). "Sedation for endoscopy: the safe use of propofol by general practitioner sedationists". Medical Journal of Australia. 176 (4): 158&ndash, 161. PMID 11913915. Retrieved 2007-06-12. Unknown parameter
|coauthors=ignored (help) - ↑ Lichtenstein, Gary R. (18 August 1998). "Use of a Push Enteroscope Improves Ability to Perform Total Colonoscopy in Previously Unsuccessful Attempts at Colonoscopy in Adult Patients". The American Journal of Gastroenterology. 94 (1): 187. PMID 9934753. Unknown parameter
|coauthors=ignored (help);|access-date=requires|url=(help) Note:Single use PDF copy provided free by Blackwell Publishing for purposes of Wikipedia content enrichment. - ↑ Barclay RL, Vicari JJ, Doughty AS; et al. (2006). "Colonoscopic withdrawal times and adenoma detection during screening colonoscopy". 355 (24): 2533&ndash, 41.
See also
External links
- Colonoscopy. Based on public-domain NIH Publication No. 02-4331, dated February 2002.
- Patient Education Brochures. American Society for Gastrointestinal Endoscopy information
Template:Digestive system surgical procedures
de:Koloskopie it:Colonscopia he:קולונוסקופיה sv:Koloskopi yi:קאלאנסקאפי
- CS1 errors: dates
- Pages with citations using unsupported parameters
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- Pages using citations with format and no URL
- Pages using citations with accessdate and no URL
- CS1 maint: Unrecognized language
- Diagnostic gastroenterology
- Medical tests